Abstract
Schwannomas, also known as neurinomas or neurilemmomas, are generally benign, slow-growing neoplasms originating in any nerve that has a Schwann cell sheath. These neoplasms are rare among the spindle cell mesenchymal tumors of the gastrointestinal tract, but develop most commonly in the stomach representing 0.2% of all gastric tumors. We present the case of a 57-year-old female patient with a large schwannoma in the stomach that was palpable in the abdomen. She underwent subtotal gastrectomy under suspicion of gastrointestinal stromal tumor (GIST), but post-operative histopathological and immunohistochemical findings showed a fascicular arrangement of spindle cell with pallisading nuclei, and positive for S-100 protein with negative smooth muscle actin (SMA). These results confirmed schwannoma as the diagnosis.
Keywords: Schwannoma, stomach, submucosal tumor, S-100 protein
INTRODUCTION
Schwannomas also known as neurinomas or neurilemmomas, are tumors originating from any nerve that has a Schwann cell sheath. These rarely develop in the gastrointestinal tract, and the most common site along the GI tract is the stomach. Schwannomas make-up 0.2% of all gastric neoplasm.1 The tumors are usually benign, slow-growing, and asymptomatic, but in some cases, bleeding or a palpable mass is present. Gastrointestinal endoscopy is the principal diagnostic tool. However, when the tumor has the characteristics of an exophytic mass from the gastric wall to the abdominal cavity, the differentiation of a schwannoma from other submucosal tumors is very difficult on pre-operative examination. The diagnostic determination of schwannomas requires histological testing to be positive for the S-100 protein and vimentin but negative for both smooth muscle actin and c-KIT. Because most schwannomas have an excellent prognosis, surgical removal is sufficient for treatment.
Here we present a 57-year-old woman with a gastric schwannoma manifesting as a palpable mass in the abdomen, which was confirmed pathologically after surgery.
CASE REPORT
A 57-year-old woman with diabetic nephropathy, hypertension, and angina was referred to our institution for an incidentally-detected abdominal mass detected by sonography. She did not have any other clinical complaints. Physical examination revealed a palpated golf ball-sized mass in the epigastric area without tenderness or rebound tenderness.
Gastrointestinal endoscopy was not performed due to her medical history of angina. Instead, an upper gastrointestinal barium study showed a large submucosal mass in the gastric angle (Fig. 1).
Fig. 1.
Barium upper gastrointestinal study shows a large submucosal tumor noted in gastric angle without mucosal ulceration (black arrows).
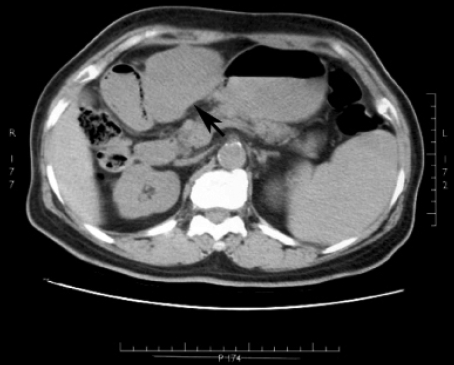
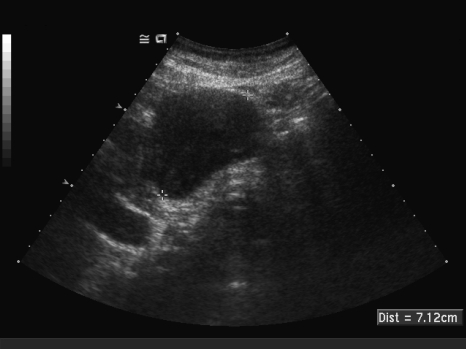
Computed tomography of the abdomen revealed an ovoid and homogenous 7 × 5 × 4 cm soft tissue mass at the lesser curvature in the lower body of the stomach (Fig. 2). Aside from splenomegaly, there was no evidence of metastasis. To facilitate visualization of the mass, we performed a sonography, which depicted an ill-defined round mass neighboring the antrum. The mass was approximately 6 × 5 × 4 cm in diameter and had a homogenous internal echo (Fig. 3).
Fig. 2.
Abdomen computed tomography reveals a large soft tissue mass lesion along lesser curvature side of stomach (black arrow).
Fig. 3.
Abdomen sonography reveals a homogeneous, hypoechoic and kidney bean shaped mass.
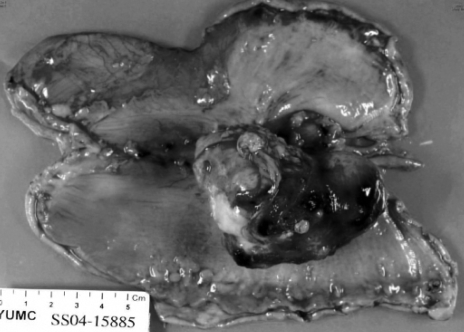
The patient underwent a subtotal gastrectomy. On gross inspection, the tumor was an exophytic, intramural, fungating, nodular, solid mass measuring 6 × 5.5 × 4 cm with whirling trabeculation seen in cross section (Fig. 4).
Fig. 4.
Surgical specimen is seen a intramural fungating nodular solid mass.
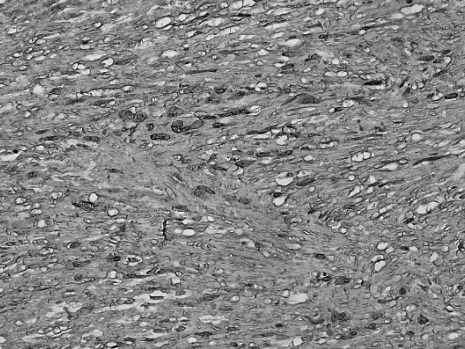
Immunohistochemically, the tumor was positive for S-100 protein, while desmin and smooth muscle actin were negative. These morphologic features were identical to those of previously reported digestive tract schwannomas (Fig. 5).
Fig. 5.
Immunochemistry stain shows the bundles of spindle cell with brown color, positive to S-100 protein (S-100 stain, × 200).
Three years after surgery, the patient is well and without evidence of recurrent disease.
DISCUSSION
The vast majority of spindle cell stromal tumors of the gastrointestinal tract were once considered to originate from smooth muscle. With the development of immunohistochemical staining and electron microscopy, various distinct origins have become apparent. These modalities allowed for a more precise classification among stromal tumors in the gastrointestinal system. For example, Daimaru et al. reported that 24 out of 306 diagnosed gastrointestinal spindle cell tumor cases were determined to be schwannomas by immunohistochemical methods. When these 24 cases were re-examined with hematoxylin-eosin, only 9 cases were diagnosed as schwannomas.2 This marked difference supports the high likelihood for misdiagnosing schwannoma as spindle cell tumors before the emergence of immunohistochemical staining.
Appelman et al. described a schwannoma as a benign neurogenic tumor under the name 'small intramuscular spindle cell nodule'.3 It is, in fact, a spindle cell mesenchymal tumor that is very rare in the gastrointestinal tract and originates in Schwann cells in the neural plexus.
The most common gastrointestinal site is the stomach, constituting 0.2% of all gastric neoplasms. Malignant transformation of a gastric schwannoma is very rare, and only one has been reported in children by Bee et al.4
The tumors are usually encased by intact mucosa and principally involve the submucosa and muscularis propria. Furthermore, they generally present asymptomatically or with abdominal discomfort.5 Bleeding may be present in the case of deep ulceration,6 and a mass may be palpated in the epigastric area when exophytic growth has occurred.
Although the definitive diagnosis of gastric schwannomas is determined by pathological examination, it may be helpful to gain limited information through gastrointestinal endoscopy, computed tomography, sonography, and magnetic resonance imaging.
On computed tomography, a gastric schwannoma tends to be homogenous, which distinguishes it from leiomyomas and leiomyosarcomas.7 Sonography with sufficient resolution power enables the determination of the tumor's layer of origin.8 In addition, magnetic resonance imaging is important to define the exact location and extent of the tumor with displacement of surrounding organs or vessels.9
In pathological tests, there are characteristics of fascicular arrangement or palisading nuclei with H&E stain. Immunohistochemically, positive staining for S-100 protein and vimentin and negative staining for smooth muscle actin, c-KIT, and CD34 supports the notion that the tumor originated from the Schwann cell. Because the tumor was benign, surgical resection of the tumor was sufficient.
In this case, a 57 year-old woman with a palpable abdominal mass was diagnosed with a pathologically confirmed gastric schwannoma after subtotal gastrectomy. The tumor size was 6 × 5.5 × 4 cm, and immunohistochemical staining was positive for S-100 protein but negative for desmin and smooth muscle actin, which supports the diagnosis of a schwannoma.
References
- 1.Melvin WS, Wilkinson MG. Gastric schwannoma. Clinical and pathologic considerations. Am Surg. 1993;59:293–296. [PubMed] [Google Scholar]
- 2.Daimaru Y, Kido H, Hashimoto H, Enjoji M. Benign schwannoma of the gastrointestinal tract: a clinicopathologic and immunohistochemical study. Hum Pathol. 1988;19:257–264. doi: 10.1016/s0046-8177(88)80518-5. [DOI] [PubMed] [Google Scholar]
- 3.Appelman HD. Smooth muscle tumors of the gastrointestinal tract. What we know now that Stout didn't know. Am J Surg Pathol. 1986;10 Suppl 1:83–89. [PubMed] [Google Scholar]
- 4.Bees NR, Ng CS, Dicks-Mireaux C, Kiely EM. Gastric malignant schwannoma in a child. Br J Radiol. 1997;70:952–955. doi: 10.1259/bjr.70.837.9486074. [DOI] [PubMed] [Google Scholar]
- 5.Prévot S, Bienvenu L, Vaillant JC, de Saint-Maur PP. Benign schwannoma of the digestive tract: a clinicopathologic and immunohistochemical study of five cases, including a case of esophageal tumor. Am J Surg Pathol. 1999;23:431–436. doi: 10.1097/00000478-199904000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Kim JY, An JY, Choi MG, Noh JH, Sohn TS, Kim S. A Case of giant gastric schwannoma accompanied with bleeding. J Korean Gastric Cancer Assoc. 2006;6:47–51. [Google Scholar]
- 7.Vinhais SN, Cabrera RA, Nobre-Leitão C, Cunha TM. Schwannoma of the esophagus: computed tomography and endosonographic findings of a special type of schwannoma. Acta Radiol. 2004;45:718–720. doi: 10.1080/02841850410008243. [DOI] [PubMed] [Google Scholar]
- 8.Fujii Y, Taniguchi N, Hosoya Y, Yoshizawa K, Yasuda Y, Nagai H, et al. Gastric schwannoma: sonographic findings. J Ultrasound Med. 2004;23:1527–1530. doi: 10.7863/jum.2004.23.11.1527. [DOI] [PubMed] [Google Scholar]
- 9.Karabulut N, Martin DR, Yang M. Case report: gastric schwannoma: MRI findings. Br J Radiol. 2002;75:624–626. doi: 10.1259/bjr.75.895.750624. [DOI] [PubMed] [Google Scholar]