Abstract
Purpose
The da Vinci® robot system has been used to perform complex reconstructive procedures in a minimally invasive fashion. Robot-assisted laparoscopic radical prostatectomy has recently established as one of the standard cares. Based on experience with the robotic prostatectomy, its use is naturally expanding into other urologic surgeries. We examine our practical pattern and application of da Vinci® robot system in urologic field.
Patients and Methods
Robotic urologic surgery has been performed during a period from July 2005 to August 2008 in a total of 708 cases. Surgery was performed by 7 operators. In our series, radical prostatectomy was performed in 623 cases, partial nephrectomy in 43 cases, radical cystectomy in 11 cases, nephroureterectomy in 18 cases and other surgeries in 15 cases.
Results
In the first year, robotic urologic surgery was performed in 43 cases. However, in the second year, it was performed in 164 cases, and it was performed in 407 cases in the third year. In the first year, only prostatectomy was performed. In the second year, partial nephrectomy (2 cases), nephroureterectomy (3 cases) and cystectomy (1 case) were performed. In the third year, other urologic surgeries than prostatectomy were performed in 64 cases. The first robotic surgery was performed with long operative time. For instance, the operative time of prostatectomy, partial nephrectomy, cystectomy and nephroureterectomy was 418, 222, 340 and 320 minutes, respectively. Overall, the mean operative time of prostatectomy, partial nephrectomy, cystectomy and nephrourectectomy was 179, 173, 309, and 206 minutes, respectively.
Conclusion
Based on our experience at a single-institution, robot system can be used both safely and efficiently in many areas of urologic surgeries including prostatectomy. Once this system is familiar to surgeons, it will be used in a wide range of urologic surgery.
Keywords: Robotics, prostatectomy, urology
INTRODUCTION
With recent introduction of robot in surgery, prostatectomy has frequently been performed worldwide in the field of urology. The da Vinci® robot system (Intuitive Surgical, Sunnyvale, CA, USA) has been used to perform complex reconstructive procedures in a minimally invasive fashion. The da Vinci® robot system has such advantages as seven degrees of freedom including the operator's grip, a 3-dimensional vision, intuitive motion and the filtration of unwanted physiologic tremors and it allows ease of intracorporeal dissection and suturing secondary to the wristed and articulating instrumentation. However, the da Vinci® robot system has some disadvantages; it is still expensive, requires training for the robot system, and is devoid of tactile feedback. Nevertheless, the introduction of robots has been expanding in the field of clinical medicine. With accumulated experience of robot-assisted laparoscopic radical prostatectomy, robot systems have been used for other urologic surgeries. In addition to prostatectomy, many surgeries, in the field of urology including pyeloplasty, radical nephrectomy, donor nephrectomy, and partial nephrectomy, are performed using robot systems.1-3 In Korea, robot-assisted laparoscopic radical prostatectomy was first performed in 2005. It has also been used for partial nephrectomy, nephrectomy, cystectomy, nephroureterectomy and pyeloplasty.4-6
We analyzed robotic urologic surgery which has been performed in a single-institution setting. We also present how the scope of application of robotic urologic surgery has been extended to date since it was first introduced.
PATIENTS AND METHODS
Robotic urologic surgery has performed during a period from July 2005 to August 2008 in a total of 708 cases. Surgery was performed by 7 operators, and 3 of them were responsible for the surgery in only 6 cases, and the remaining 4 surgeons performed all 702 cases. The surgical period ran from July 2005 to May 2007 using 1 unit da Vinci® robot, and from May 2007 to the present using 4 units da Vinci® S (Fig. 1). Mean age was 58.7 ± 10.6 years, and the number of male patients was 661 (93.7%). In our clinical series, radical prostatectomy was performed in 623 cases, partial nephrectomy in 41 cases, radical cystectomy in 11 cases, nephroureterectomy in 18 cases and other surgeries in 15 cases. We presented perioperative clinical course and a short-term surgical outcome through a retrospective analysis of medical records.
Fig. 1.
The da Vinci® surgical system.
RESULTS
A comparison was made based on a 12-month interval during a period from July 2005 to the present. This revealed clear changes in the pattern by which robotic urologic surgery was performed. During the first 1-year period, robotic urologic surgery was performed in 43 cases, it was performed in 164 cases during the second 1-year period, and it was performed in 407 cases during the third 1-year period. 94 were performed during the last 2 months. During the first 1-year period, only prostatectomy was performed. During the second 1-year period, however, partial nephrectomy (2 cases), nephroureterectomy (3 cases), and cystectomy (1 case) were performed. During a recent 1-year period, urologic surgeries other than prostatectomy were also performed in 64 cases. Furthermore, various urologic surgeries such as cystectomy, nephroureterectomy, pyeloplasty, partial nephrectomy, and donor nephrectomy were also performed.
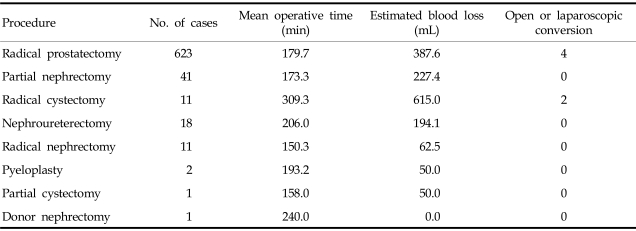
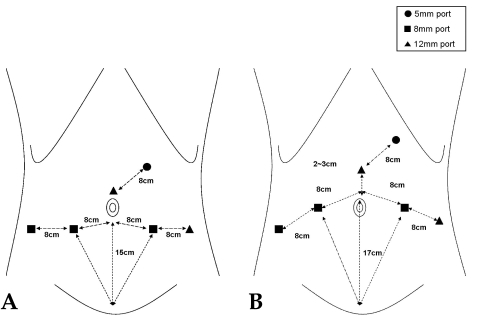
The first robotic surgery was performed with long operative time. For instance, the operative time of prostatectomy, partial nephrectomy, cystectomy, and nephroureterectomy was 418, 222, 340, and 320 minutes, respectively. When the operator was accustomed to setting up or manipulating robot system, the operator felt comfortable and operative time was shortened. Overall, the mean operative time of prostatectomy, partial nephrectomy, cystectomy, and nephrourectectomy was 179, 173, 309, and 206 minutes, respectively. Types and initial outcomes of robotic surgery are represented in Table 1. After we overcame the initial learning curve for robotic surgery, we had no difficulty in applying it to other urologic surgeries. We modified the port placement of prostatectomy and applied it to other surgeries (Fig. 2). Also in the first surgery, the surgical time was relatively shorter.
Table 1.
Perioperative Data of 614 Robotic Urologic Surgeries
Fig. 2.
Port placement for robot-assisted laparoscopic radical prostatectomy (A) and cystectomy (B).
Conversion to open or laparoscopic surgery was seen in a total of 6 cases, which was noted in 4 cases of prostatectomy and 2 cases of cystectomy. A switch to open or laparoscopic surgery was done due to severe adhesion in 2 cases and mechanical defect of robot system in 2 cases in which prostatectomy was performed. It was done due to severe adhesion in all 2 cases, and cystectomy was performed.
DISCUSSION
In recent years, urologic surgery has been advanced toward the direction of less-invasive surgery while the principle of the open surgery is still observed. In most of the surgical treatment for benign prostate hyperplasia, the open surgery was replaced by transurethral surgery. In the treatment of simple renal cyst or adrenal tumor, the laparoscopic surgery is favored over the open surgery, which can be shown as a good example. In the field of urology, the laparoscopic surgery shows no significant differences in the safety and efficiency compared to the open surgery, which has been demonstrated in various institutions and actively performed. Laparoscopic surgeries have several advantages, including shorter length of hospital stay due to faster recovery, cosmetic factors and lower risk of developing postoperative complications. Consequently, the laparoscopic surgery has substituted for the open surgery. Nevertheless, the difficulty in obtaining technical expertise and prolonged operative time has been considered to be inherent with laparoscopic surgery. In most of the surgical modalities, operators must spend a lot of time and efforts in getting accustomed to novel surgeries. Until recently, in cases of the laparoscopic prostatectomy which has commonly been performed for the surgical treatment of prostate cancer. Guillonneau et al.,7 reported that approximately 40 cases of surgeries are needed for surgeons to obtain average level of skill.
In 1994, Kavoussi et al.8 first reported an initial surgery with robot system, using AESOP camera and laparoscopic instruments. Several years later, Cadiere et al.9 reported 146 cases of surgeries using da Vinci® system. Until then, however, most of surgeries have been performed in the field of surgeries. Of total 146 cases, urologic surgeries accounted for 2 cases of prostatectomy and one case of varicocelectomy. According to Talamini et al.,10 of total 211 cases of surgeries done by using the da Vinci® system, 15 cases of donor nephrectomy and 6 cases of adrenalectomy were performed. In the field of urology, the robotic surgery was first initiated with prostatectomy. In recent years, it has been applied to a broad range of areas including pyeloplasty, partial nephrectomy, cystectomy, and donor nephrectomy.1-3 Good surgical vision, prevention of tremors and accurate mobility are advantages of robotic surgery compared to laparoscopic surgery, nevertheless the easiness-to-learn is attractive to the operator. Chang et al.11 reported that surgical technique was persistently improved following the training with the use of robotic surgery, and Ahlering et al.12 noted that results improved in proportion to the accumulation of operator's experience. Our own experience showed that robotic surgery overcame the learning curve relatively in the earlier stage unlike the laparoscopic surgery. Therefore, it appears that it can be extensively applied to other areas. We first performed robot-assisted laparoscopic radical prostatectomy in 2005. Thereafter, we have expanded it's scope to partial nephrectomy, cystectomy, nephroureterectomy and pyeloplasty.4-6 Following approximately 40 cases of prostatectomy, we performed partial nephrectomy. After more than 100 cases performed, we had no difficulty in carrying out cystectomy and nephroureterectomy. In addition, after more than 100 cases, we successfully performed the first robotic surgery without any difficulties within an average surgical time. Conversion to the open or the laparoscopic surgery was done in 6 cases (1.0%); it was done due to severe adhesion in 4 cases where the lesions remained until recently, and mechanical defects of robot system in 2 cases where the causes were identified in the early stage. With accumulated experiences of robot system, most of the mechanical defects are presently checked preoperatively and then resolved. In cases where such defects occur, we are capable of resolving them within the shortest time. Thanks to this, there have been no cases, where conversion has to be done because of robot system.
There are some disadvantage of robotic surgery such as requirement of long docking time and the expensiveness of robotic assistance. When the operation team gets accustomed to setting up or manipulating robot system, the docking time can be shortened. But cost issues regarding the expense of robotic system should also be discussed.13
A present, robot system has been performed almost in all clinical fields. In near future, it will be the elemental factor for medical environment such as operation room or hospitalization room. For a robot system to be applied in a wide range of areas, the operator must first be accustomed to using it. All the surgical personnel must fully understand the mechanisms by which robot system is manipulated. In addition, all the personnel who participated in robotic surgery must be accustomed to it as a team.
Based on our experience at a single-institution, robot system can be used both safely and efficiently in many areas of urologic surgeries including prostatectomy. Once this system is familiar to surgeons, it will be used in a wide range of urologic surgery.
References
- 1.Sung GT, Gill IS, Hsu TH. Robotic-assisted laparoscopic pyeloplasty: a pilot study. Urology. 1999;53:1099–1103. doi: 10.1016/s0090-4295(99)00030-8. [DOI] [PubMed] [Google Scholar]
- 2.Abbou CC, Hoznek A, Salomon L, Olsson LE, Lobontiu A, Saint F, et al. Laparoscopic radical prostatectomy with a remote controlled robot. J Urol. 2001;165:1964–1966. doi: 10.1097/00005392-200106000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Guillonneau B, Jayet C, Tewari A, Vallancien G. Robot assisted laparoscopic nephrectomy. J Urol. 2001;166:200–201. [PubMed] [Google Scholar]
- 4.Lee YS, Han WK, Oh YT, Choi YD, Yang SC, Rha KH. Robot-assisted laparoscopic radical prostatectomy: four cases. Yonsei Med J. 2007;48:341–346. doi: 10.3349/ymj.2007.48.2.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park SY, Cho KS, Ham WS, Lee JH, Choi HM, Rha KH. Robot-assisted laparoscopic nephroureterectomy with a bladder cuff excision. Korean J Urol. 2008;49:373–375. [Google Scholar]
- 6.Park SY, Kim HJ, Seo JW, Cho KS, Ham WS, Rha KH. Robot-assisted laparoscopic partial nephrectomy. Korean J Urol. 2008;49:387–391. [Google Scholar]
- 7.Guillonneau B, Rozet F, Barret E, Cathelineau X, Vallancien G. Laparoscopic radical prostatectomy: assessment after 240 procedures. Urol Clin North Am. 2001;28:189–202. doi: 10.1016/s0094-0143(01)80021-5. [DOI] [PubMed] [Google Scholar]
- 8.Kavoussi LR, Moore RG, Partin AW, Bender JS, Zenilman ME, Satava RM. Telerobotic assisted laparoscopic surgery: initial laboratory and clinical experience. Urology. 1994;44:15–19. doi: 10.1016/s0090-4295(94)80003-0. [DOI] [PubMed] [Google Scholar]
- 9.Cadière GB, Himpens J, Germay O, Izizaw R, Degueldre M, Vandromme J, et al. Feasibility of robotic laparoscopic surgery: 146 cases. World J Surg. 2001;25:1467–1477. doi: 10.1007/s00268-001-0132-2. [DOI] [PubMed] [Google Scholar]
- 10.Talamini MA, Chapman S, Horgan S, Melvin WS The American Robotic Group. A prospective analysis of 211 robotic-assisted surgical procedures. Surg Endosc. 2003;17:1521–1524. doi: 10.1007/s00464-002-8853-3. [DOI] [PubMed] [Google Scholar]
- 11.Chang L, Satava RM, Pellegrini CA, Sinanan MN. Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc. 2003;17:1744–1748. doi: 10.1007/s00464-003-8813-6. [DOI] [PubMed] [Google Scholar]
- 12.Ahlering TE, Skarecky D, Lee D, Clayman RV. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: initial experience with laparoscopic radical prostatectomy. J Urol. 2003;170:1738–1741. doi: 10.1097/01.ju.0000092881.24608.5e. [DOI] [PubMed] [Google Scholar]
- 13.Burgess SV, Atug F, Castle EP, Davis R, Thomas R. Cost analysis of radical retropubic, perineal, and robotic prostatectomy. J Endourol. 2006;20:827–830. doi: 10.1089/end.2006.20.827. [DOI] [PubMed] [Google Scholar]