Abstract
Advances in medical and rehabilitative care have increased interest in studying how different factors may affect the health-related quality of life (HRQOL) of individuals with spinal cord injury (SCI). There has been a large increase in the number of studies assessing HRQOL among persons with SCI. However, despite these advances, numerous issues remain unanswered because these studies have used a variety of methodologic approaches and assessment tools to examine how different factors have a role in predicting HRQOL in SCI populations. Therefore, standardized instruments should be used as part of this process. The Medical Outcomes Study Short Form (SF-36) was developed in order to survey health status of the general population. However, the available data on the HRQOL of individuals with SCI are currently limited. In addition, there is little information currently available on the factors that are associated with HRQOL in the SCI population and this issue remains controversial. The findings from several individual studies that used the SF-36 to assess the HRQOL of patients suffering from SCI were reviewed, and the results were interpreted with disability in mind. This review article aims to summarize the data regarding the HRQOL of individuals with SCI by using the SF-36.
Keywords: Spinal cord injury, quality of life, questionnaires, Short Form-36
INTRODUCTION
As healthcare has improved, the average life expectancy following a spinal cord injury (SCI) has increased. Living with a disability has become a life-long process for many injured persons, with a different set of problems presenting themselves at different stages throughout their lifetime. Extended life spans and the need for life-long follow-up make it important to expand the outcome parameters of medical care in order to better understand and promote physical, psychological, and social well-being after an SCI. Thus, advances in medical and rehabilitative care have increased interest in studying how several factors may affect the health-related quality of life (HRQOL) of individuals with SCI.
There has been a large increase in the number of studies that assess HRQOL among persons with SCI. HRQOL measures provide a meaningful way to document an individual's progress and response to treatment without the limitations of the more traditional measures of mortality and morbidity. These studies have used a variety of methodological approaches and assessment tools in order to examine the different factors that are used in predicting HRQOL in SCI populations.1-8 Differences in the conclusions drawn by some researchers, such as in the relationship of HRQOL to the severity of the individual's impairment, may at least be in part a function of the instruments used to assess HRQOL.2,9-14 Part of the difficulty in implementing and adopting good and reliable measures of HRQOL is due to the confusion caused by defining this concept.
Generic measures of HRQOL are recommended to be used for the assessment of the general quality of healthcare being provided and are also used to monitor the health of large populations. Thus, generic HRQOL assessments may be preferred in research covering the entire age spectrum of adults. The Medical Outcomes Study Short Form (SF-36) was developed in order to survey the health status in the United States.15 Experience to date suggests that the SF-36 can be adapted for use in other countries with relatively minor changes to the content of the form, providing support for the use of these translations in multinational clinical trials and other studies.16
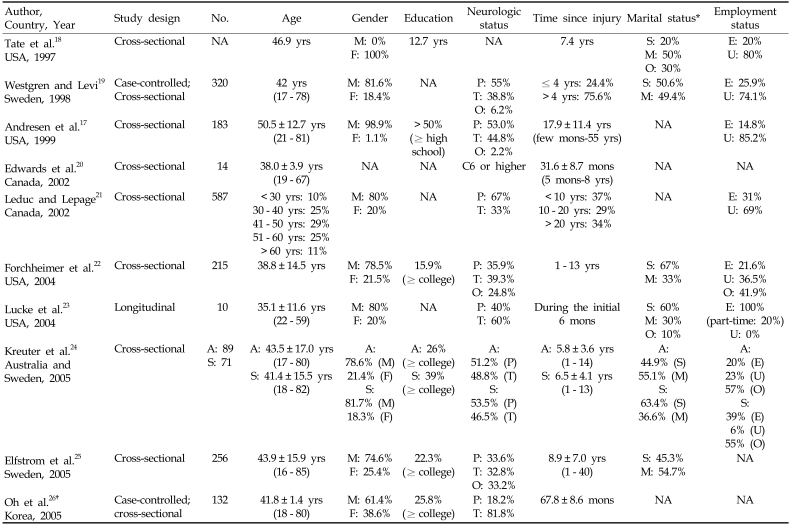
While generic outcomes instruments are designed for use in any population, their validity and reliability in a particular disease should be verified in order to ensure their appropriateness for use in that disease. The ability of generic instruments to assess HRQOL of impairment-specific populations is likely to vary depending on the characteristics of the different groups. For example, floor effects or compressed scale ranges may be more common in patients with SCI than in other more general populations because generic instruments might not distinguish among individuals with morbidity limitations caused by the SCI. However, although the SF-36 scales demonstrated some problems with scale extremes, the SF-36 summary measures, due to the scaling transformation process, were free of floor and ceiling effects.17 The findings from several individual studies that used the SF-36 to assess HRQOL of patients suffering from SCI were reviewed and interpreted in light of the concept of being disabled (Table 1).17-26
Table 1.
Patient characteristics of studies using the Short-Form 36-item questionnaire
NA, not available; M, male; F, female; S, single; M, Married; O, others; E, employed; U, unemployed; P, paraplegia; T, tetraplegia; A, Australia; S, Sweden.
*Divorced and widowed persons were included in 'single' and those with stable partner were included in 'married'.
†Patients using clean intermittent catheterization.
SHORT-FORM 36-ITEM HEALTH SURVEY
The SF-36 assesses eight health phenomena: (a) limitations of physical functioning because of health problems (PF); (b) limitations in usual activities because of physical health problems (role-physical: RP); (c) bodily pain (BP); (d) general health perception (GH); (e) vitality (energy and fatigue: VT); (f) limitations on social functioning because of physical or emotional problems (SF); (g) limitations on usual activities because of emotional problems (role-emotional: RE); and (h) general mental health (psychological distress and well-being: MH). A norm-based scoring, which are derived from these standard scores, can also be used. The mean scores within the general population are 50 and the standard deviations are 10 for all eight domains. The eight domains are collapsed in order to create two global components, a physical component score (PCS) and a mental component score (MCS). The PCS is associated with high scores on the PF, RP, BP and GH scales and low scores on the RE and MH scales. Conversely, for the MCS, positive weights are placed on the MH, RE, SF, and VT scales, whereas substantial negative scores are placed on the PF and RP scales.
To date, experience with the SF-36 has been documented in more than a thousand publications. The usefulness of using the SF-36 to estimate disease burden has been described for more than 130 diseases and conditions. Translation of the SF-36 is the subject of 148 publications, and one or more articles compare results from the SF-36 with those of 225 other generic and disease-specific instruments.27 The SF-36 is a generic measure of health status as opposed to one that targets a specific age, disease, or treatment group. Accordingly, the SF-36 has proven useful in comparing general and specific populations, estimating the relative burden of different diseases, differentiating the health benefits produced by a wide range of different treatments, and screening individual patients.28
It has been correctly stated that the conventional translation strategies, including duplicating the originals as closely as possible, for translating the HRQOL questionnaires are limited because they preserve the efficiencies of the original questionnaire and do not permit modifications that reflect differences in cultures and values.29 Differences exist among cultures in the levels of literacy, taboo subjects, and social desirability effects. Furthermore, certain features of the English language, such as idioms, are very difficult to translate and would make little sense when given in a different cultural context. The ability to define and assess HRQOL across ethnic groups requires the development of outcome measures in non-English languages that are culturally appropriate for cross-ethnic studies. Experience to date suggests that the SF-36 can be adapted for use in other countries with relatively minor changes to the contents of the form and thus provides support for the use of these translations in multinational clinical trials and other studies.16
The SF-36 has provided a good overall validity with regard to the health status of SCI individuals.21 However, the rehabilitation community has raised one concern about the SF-36 in regard to its inclusion of three questions that refer to walking and two others that concern climbing stairs.22 These questions related to walking and climbing stairs in the PF domain may pose a problem for individuals who use wheelchairs.17 Furthermore, the maximum level of difficulty is defined as "limited a lot," which does not clearly distinguish the different impairment levels that are relevant to those suffering from partial SCI.17
HEALTH-RELATED QUALITY OF LIFE IN PATIENTS WITH SPINAL CORD INJURY
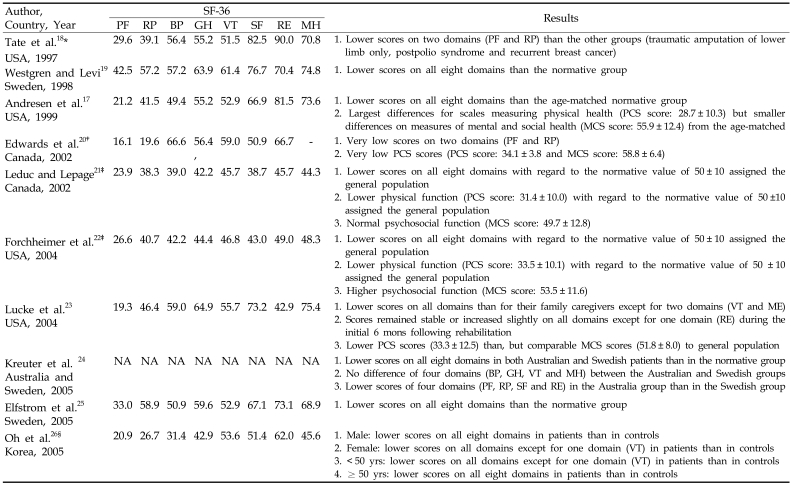
Norms have already been established for patient populations with chronic conditions. However, very little work has been done to investigate the use of the SF-36 with individuals with SCI. Of the few studies that have looked at possible correlates or predictors of HRQOL among persons with disabilities, most suggest that the subjective well-being of persons with physical disabilities is on average less than that of the general population. Table 2 summarizes the results of HRQOL of the SCI population.17-26
Table 2.
Health-related quality of life in patients with spinal cord injury
SF, short-form; PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health; PCS, Physical Component Summary; MCS, Mental Component Summary; NA, not available.
*Women only.
†Score of VT is a sum of vitality (4 items) plus mental health (5 items) and score of GH is general health (5 items) and Health change (1 item).
‡Calculating a score with the norm-based scoring method.
§Patients using clean intermittent catheterization.
United States
Tate et al.18 assessed HRQOL among women with physical disabilities, including SCI and breast cancer, from a medical center in the Midwest. Women with traumatic conditions reported a significantly lower score of both physical functioning and physical well-being than did women with nontraumatic conditions.
Andresen et al.17 evaluated HRQOL among 183 veterans with SCI who were randomly selected from those who received care at a regional veterans' SCI program. The SF-36 scores of the SCI groups were compared with age-matched normative data from the 1990 National Survey of Functional Health Status (NSFHS). Forchheimer et al.22 explored the applicability of using the SF-36 on 215 persons with SCI. Subjects included in this study were members of a model SCI Care System at a university hospital in the Midwest (University of Michigan). Lucke et al.23 evaluated the HRQOL among 10 individuals with SCI who were recruited from two rehabilitation hospitals located in southwestern Pennsylvania during the initial six months following rehabilitation. These studies demonstrated that the PCS scores for the SCI patients were lower than that for the general population, while their MCS scores were comparable with those of the general population.
Canada
Edwards et al.20 assessed HRQOL among 14 patients from The Spinal Program at the Toronto Western Hospital, which is a part of the University Health Network. Ludec and Lepage21 assessed HRQOL among 587 subjects with SCI who were listed in the data bank of the Quebec Paraplegic Association (QPA). They suggested that physical health seemed particularly more affected than mental health, especially for the aging SCI population because they are more vulnerable to medical complications.
Sweden
Westgren and Levi19 surveyed HRQOL among 320 individuals with SCI in the greater Stockholm area as a part of the Stockholm Spinal Cord Injury Study (SSCIS). Elfstrom et al.25 studied 256 patients with SCI who were treated and/or followed-up at the Gothenburg Spinal Injuries Unit. The SCI group scored significantly lower than the normative group on all domains in both studies.
Australia and Sweden
Kreuter et al.24 compared HRQOL in Australian and Swedish people with SCI. The Australian group consisted of 89 SCI patients who were randomly selected from the records at the Austin Health located in Melbourne. The Swedish group consisted of 71 consecutive SCI patients who were treated at the spinal unit in Gothenburg. Although the scores of BP, GH, VT and MH were not different between the two groups, the limitations in RF, RP, SF and RE were more pronounced among the Australian SCI patients.
South Korea
Oh et al.26 evaluated 132 SCI patients using a clean intermittent catheterization for those with a neurogenic bladder. The SCI patients had lower scores for most of the domains than did the controls, regardless of sex and age.
FACTORS INFLUENCING HEALTH-RELATED QUALITY OF LIFE IN PATIENTS WITH SPINAL CORD INJURY
A number of SCI studies have focused on predicting HRQOL from sociodemographic variables, disability-related variables, medical problems, and psychosocial variables. However, little information regarding factors associated with HRQOL in persons with SCI is currently available. In addition, since these factors have not been consistently found to have the same effects on HRQOL, this issue remains controversial.
Sociodemographic variables
Age
Aging with SCI has recently gained attention in the literature, as has its relationship with HRQOL. Edwards et al.20 found that the age of patients was negatively correlated with SF scores, although not significantly (r = -0.43, p = 0.12). Oh et al.26 also reported that patients younger than 50 years had higher scores in the VT domain than those who were 50 years old or older (46.8 ± 2.1 versus 34.9 ± 3.5). These studies show a correlation between being young and a perceived higher HRQOL in some domains. However, Kreuter et al.24 found that age was not significantly correlated with global HRQOL. Furthermore, Leduc and Lepage21 demonstrated that HRQOL scores were negatively correlated with age. All eight SF-36 domains showed differences between the five age subgroups in both the PCS and MCS. A previous study carried out on SCI individuals suggested that the HRQOL begins to decline in individuals between the age of 45 and 50 years old.1 Therefore, only tentative conclusions can be drawn, and these must be made cautiously.
Gender
Gender differences in the broad scope of health and illness have been the subject of extensive investigation and are also currently gaining more attention in medicine. Women and men emphasize different aspects of their lives when evaluating their level of HRQOL and life satisfaction. Women with SCI are overrepresented in the group suffering from psychiatric ill health. Westgren and Levi19 reported gender differences in both VT and MH, where women scored lower than men. Leduc and Lepage21 also found differences in the PF, VT and MH scores. However, Oh et al.26 revealed that the scores of patients using clean intermittent catheterization did not show any significant differences between men and women.
Education level
A low level of education is typically connected with work that is physically demanding, which would be difficult to manage after an SCI. A number of studies have shown that a higher education is associated with higher employment rates among SCI individuals.30 Kreuter et al.24 found that a higher level of education was associated with higher HRQOL ratings in the Australian SCI group, whereas the level of education was not significantly correlated with global HRQOL in the Swedish group. Oh et al.26 revealed that when patients using clean intermittent catheterization were subdivided into three groups according to their educational levels, no significant differences were found in the SF-36 scores.
Employment status
Employment is considered an important indicator for good HRQOL, although this variable is strongly influenced by economic and social opportunities, as well as age and education level. However, a previous study indicated that at the social level, the level of employment of SCI individuals remains well below that of the general population.31 This is due to a number of reasons but is mainly related to medical issues, insufficient training, and lack of integration measures; in addition, sometimes the disablement benefits can act as a deterrent. Westgren and Levi19 reported significantly lower scores in all eight domains in atients in the SCI group who worked less than full time or were not employed than in patients in the SCI group who worked full-time. In this study, there was no difference in the reported HRQOL of the employed SCI group that worked full-time and the normative group. Leduc and Lepage21 also found that employed subjects reported significantly higher scores for all eight of the SF-36 domains, as well as the PCS and MCS, when compared to the non-employed subjects.. However, Kreuter et al.24 revealed that occupation was not significantly correlated with global HRQOL in both the Australian and Swedish groups. Interestingly, unemployment was significantly more common in the Australian group. These results indicate that occupation alone has no significant impact on the perceived HRQOL.
Monthly income
Oh et al.26 reported that when patients using clean intermittent catheterization were subdivided into three groups according to their monthly income, no significant differences were found in their SF-36 scores.
Marital status
At the social level, the divorce rate of SCI individuals is greater than that of the general population.32 Marriage has proven to be a powerful ally in maintaining a high degree of life satisfaction in both SCI and nondisabled populations,5 and may have an important and positive impact on HRQOL after SCI. Westgren and Levi19 demonstrated that when evaluating the impact of marital status on HRQOL, single individuals scored significantly lower on VT, RE, and MH when compared with the married/cohabitating group. However, marital status was not significantly correlated with global HRQOL in the study performed by Kreuter et al.24
Disability-related variables
Age at injury
Being older at the time of injury is associated with a reduced capacity to cope with the injury and thus may have a negative impact on recovery. Westgren and Levi19 compared two age groups, a group that was 20 years or younger at the time of injury and a group older than 20 years at the time of injury. They found that the younger individuals scored highest with respect to PF, RP, BP, GH, and SF. In another study,25 those who were young at the time of the lesion also scored better in some domains, where the strongest associations were in the dual-role functioning scales. However, Kreuter et al.24 reported that the age at the time of the injury was not significantly correlated with global HRQOL.
Time since injury
Studies that focus on the effect of recovery time after the injury are contradictory, and little consensus has been reached about the impact that recovery time may have on HRQOL. Some of the previous studies found that the time since the injury occurred was not significantly correlated to HRQOL, whereas other studies concluded a positive correlation. Furthermore, early findings suggest that over the long term, HRQOL may hold steady at first but decline in later years.5 Westgren and Levi19 reported that an individual with SCI is more likely to report a good HRQOL the longer they have had the injury. This was illustrated by significantly lower scores on both the PF and RE, as well as SF, in the group who had been injured within 4 years than the group injured between 18 to 44 years ago. There was also a weak positive correlation between the time after injury and the emotional health of the patient (r = 0.56, p < 0.05) in the study performed by Edwards et al.20 In this study, a patient's reported physical (PCS: r = 0.43, p = 0.12) and mental health (MCS: r = 0.47, p = 0.08) improved over time after the injury initially occurred. Kreuter et al.24 also reported that the time since the lesion was first diagnosed in the Swedish group of SCI patients was correlated to HRQOL ratings, such that the longer the duration the better the ratings. The adaptive process seems to operate over a long time, despite the fact that as the time after an injury increases, the cumulated percentage of most complications increases successively. These studies indicate that at least a patient's emotional and mental health improved with time after their injury. However, Leduc and Lepage21 revealed that there were no differences observed from the amount of time since the injury. Furthermore, Elfstrom et al.25 showed that individuals with shorter durations of disability reported somewhat better HRQOL results in some of the domains. Several studies describe the duration of time since the injury as a significant predictor of HRQOL, whereas others fail to find a relationship to HRQOL. Therefore, it is difficult to compare the different studies in this respect due to differences in the sociodemographic variables.
Neurologic status (injury level and completeness of lesion)
The cost of rehabilitation for SCI patients can vary significantly depending on the level of neurologic impairment,33 with higher costs associated with higher levels of injury. In contrast, the relationship between the level or extent of the impairment and HRQOL is not well understood. A meta-analysis of 32 reports, dating from 1983 to 1992, suggested that the severity of the injury correlated negatively with HRQOL, but concluded that definitive conclusions could not be drawn from these studies due to the limited rigor of research design and the poor validity of the measurements.2 Another review also found no significant differences between groups based on the level of their injury and severity of impairment.5
Westgren and Levi19 did not find a significant difference in HRQOL between subgroups of SCI (tetraplegia (n = 124) versus paraplegia (n = 176)) in the Swedish subgroup, with the exception of a lower score in the RF domain with more extensive neurologic deficits. Similarly, Andresen et al.17 found no significant difference in injury levels in any of the domains. The HRQOL scores had few differences in the SF-36 scales when the self-reported paraplegia and quadriplegia groupings were used. In fact, for the measure of BP, those with quadriplegia had significantly higher scores (mean scale scores 55.0 versus 44.8). Underscoring this finding, all of the SF-36 scores showed only a minimal, if any, trend of decreasing health across the categories of SCI lesion levels.
However, in a 2002 study, Leduc and Lepage21 found that both the PF and PCS domains showed significant differences between paraplegics and tetraplegic subjects. Forchheimer et al.22 also found that there was a significant relationship between impairment severity and PCS scores, although no significant difference was observed with MCS scores. Elfstrom et al.25 indicated that among the disability-related variables, individuals that were more neurologically disabled reported more injury-related problems, as well as limitations in physical and social functioning. Oh et al.26 reported that patients with noncervical injuries had higher scores in the PF domain than those with cervical injuries (58.8 ± 4.4 versus 8.5 ± 1.7). In a cross-cultural comparison study,24 the level of lesion was associated with the persons' perceived HRQOL in the Australian SCI group, where the higher the lesion the lower the HRQOL ratings, whereas this was not the case for the Swedish group. Completeness of injury was not significantly correlated with global HRQOL in both groups.
Medical problems
Medical problems
Medical problems related to SCI and their associations to HRQOL have not been studied in a structured manner. However, the medical problems associated with SCI may negatively affect HRQOL. In one study,19 individuals with medical problems, neurogenic pain, problematic spasticity, and bladder problems, were associated with lower HRQOL in all eight domains, with the exception of RF for neurogenic pain. The presence of pressure sores was associated with a lower HRQOL in both the PF and SF domains. Problems with bowel function were associated with a lower HRQOL in all domains but the RP. Sexual dysfunction was associated with a lower HRQOL in both the GH and SF domains.
Hospital stay
Ludec and Lepage21 reported that, with the exception of PF, all of the other domains of the SF-36, PCS and MCS, showed a significant difference between a hospital stay in the past year and no hospital stay.
Ability to perform self-catheterization
The introduction of clean intermittent catheterization has reduced the morbidity and mortality in patients with neurogenic bladders,34 and has other beneficial effects, such as improved body image and self-esteem, and may guarantee a good HRQOL.35 Oh et al.26 demonstrated that patients who were able to perform self-catheterization had higher scores in the PF domain than those who were unable to perform self-catheterization (29.9 ± 3.3 versus 7.2 ± 2.9). However, there has been no study to date that has compared patients with SCI according to bladder management methods using the SF-36 questionnaire.
Psychosocial variables
Coping strategies
Coping strategies have been shown to be more important than social support in affecting HRQOL, in terms of psychosocial role performance and numerous aspects of well-being, in other populations with severe chronic conditions, such as multiple sclerosis.36 Elfstrom et al.25 indicated that coping strategies were also clear correlates of HRQOL in individuals with SCI when sociodemographic, disability-related, and social support variables were studied.
Psychological parameters
Mood (depressive feelings), physical and social dysfunction, and perceived loss of independence (problems regarding injury) were significantly correlated to global HRQOL ratings in both groups consisting of Australian and Swedish SCI patients.24
Patients' interest in areas of SCI
Edward et al.20 assessed the interest and accessibility of patients with SCI to information in different areas of SCI. Results from the SF-36 showed that interest in support groups was negatively correlated with SF (r = -0.67, p = 0.01) and interest in therapy was negatively correlated with the patient's general health perception (r = -0.60, p = 0.02), meaning that those with poor physical health are very interested in physical and occupational therapy.
CONCLUSIONS
HRQOL is partly a reflection of the individual's ability to cope and adapt to his or her new life situation. Addressing HRQOL issues in the SCI population is imperative as the majority survives their initial injury and their longevity now approaches that of the general population. While the physical and practical restrictions caused by SCI impairments are evident in SCI individuals, their personal roles and social activities can often be maintained. However, much remains to be discovered about the health of SCI individuals in terms of their functional health and well-being, the relative burden of disease, and the relative benefits of alternative treatments. The reasons for the lack of literature on comprehensive HRQOL issues for patients with SCI are: 1) The lack of practical measurement tools that are appropriate for widespread use across diverse populations. 2) Most of the studies were cross-sectional with limited study populations. The cross-sectional study design precludes any conclusions about causations. 3) Previous studies on SCI and HRQOL have varied considerably with respect to the methods used to measure and analyze the results. 4) Selected hospital groups have often been surveyed by mailed assessment packages, which results in biased samples and low response rates.
The effect of physical disability or illness cannot be fully understood without taking into consideration both the specific areas of functioning affected by one's physical conditions and the aspects of HRQOL that are of particular importance to the individual.18 The case-control and/or cross-sectional studies that used the SF-36 were employed in order to elucidate the potential determinants of factors associated with HRQOL in SCI individuals. However, the results of the majority of these studies may be considered preliminary, because of the small sample sizes or lack of generality. Nonetheless, these studies suggest hypotheses that will require further evaluation in well-designed population-based studies. Factors that may influence the HRQOL of SCI individuals from different countries should be considered in future studies, such as religion, culture, customs, environment, and climates to name a few,. In addition, family support, the ability to adjust and cope, productivity, self-esteem, and financial stability should also be taken into account. Potentially, the identification and characterization of the factors that are related to HRQOL in the SCI population may accelerate the development of preventive, diagnostic, and therapeutic strategies for the improvement of the HRQOL in this targeted population.
References
- 1.Eisenberg MG, Saltz CC. Quality of life among aging spinal cord injured persons: long term rehabilitation outcomes. Paraplegia. 1991;29:514–520. doi: 10.1038/sc.1991.74. [DOI] [PubMed] [Google Scholar]
- 2.Evans RL, Hendricks RD, Connis RT, Haselkorn JK, Ries KR, Mennet TE. Quality of life after spinal cord injury: a literature critique and meta-analysis (1983-1992) J Am Paraplegia Soc. 1994;17:60–66. doi: 10.1080/01952307.1994.11735918. [DOI] [PubMed] [Google Scholar]
- 3.Hallin P, Sullivan M, Kreuter M. Spinal cord injury and quality of life measures: a review of instrument psychometric quality. Spinal Cord. 2000;38:509–523. doi: 10.1038/sj.sc.3101054. [DOI] [PubMed] [Google Scholar]
- 4.Wood-Dauphinee S, Exner G, Bostanci B, Exner G, Glass C, Jochheim KA, et al. Quality of life in patients with spinal cord injury--basic issues, assessment, and recommendations. Restor Neurol Neurosci. 2002;20:135–149. [PubMed] [Google Scholar]
- 5.Tate DG, Kalpakjian CZ, Forchheimer MB. Quality of life issues in individuals with spinal cord injury. Arch Phys Med Rehabil. 2002;83(12 Suppl 2):S18–S25. doi: 10.1053/apmr.2002.36835. [DOI] [PubMed] [Google Scholar]
- 6.Hammell KW. Exploring quality of life following high spinal cord injury: a review and critique. Spinal Cord. 2004;42:491–502. doi: 10.1038/sj.sc.3101636. [DOI] [PubMed] [Google Scholar]
- 7.Dijkers MP. Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement, and research findings. J Rehabil Res Dev. 2005;42(3 Suppl 1):87–110. doi: 10.1682/jrrd.2004.08.0100. [DOI] [PubMed] [Google Scholar]
- 8.Post M, Noreau L. Quality of life after spinal cord injury. J Neurol Phys Ther. 2005;29:139–146. doi: 10.1097/01.npt.0000282246.08288.67. [DOI] [PubMed] [Google Scholar]
- 9.Decker SD, Schulz R. Correlates of life satisfaction and depression in middle-aged and elderly spinal cord-injured persons. Am J Occup Ther. 1985;39:740–745. doi: 10.5014/ajot.39.11.740. [DOI] [PubMed] [Google Scholar]
- 10.Siosteen A, Lundqvist C, Blomstrand C, Sullivan L, Sullivan M. The quality of life of three functional spinal cord injury subgroups in a Swedish community. Paraplegia. 1990;28:476–488. doi: 10.1038/sc.1990.64. [DOI] [PubMed] [Google Scholar]
- 11.Dunnum L. Life satisfaction and spinal cord injury: the patient perspective. J Neurosci Nurs. 1990;22:43–47. doi: 10.1097/01376517-199002000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Fuhrer MJ, Rintala DH, Hart KA, Clearman R, Young ME. Relationship of life satisfaction to impairment, disability, and handicap among persons with spinal cord injury living in the community. Arch Phys Med Rehabil. 1992;73:552–557. [PubMed] [Google Scholar]
- 13.Clayton KS, Chubon RA. Factors associated with the quality of life of long-term spinal cord injured persons. Arch Phys Med Rehabil. 1994;75:633–638. doi: 10.1016/0003-9993(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 14.Ville I, Ravaud JF Tetrafigap Group. Subjective well-being and severe motor impairments: the Tetrafigap survey on the long-term outcome of tetraplegic spinal cord injured persons. Soc Sci Med. 2001;52:369–384. doi: 10.1016/s0277-9536(00)00140-4. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 16.Bullinger M, Alonso J, Apolone G, Leplege A, Sullivan M, Wood-Dauphinee S, et al. Translating health status questionnaires and evaluating their quality: the IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:913–923. doi: 10.1016/s0895-4356(98)00082-1. [DOI] [PubMed] [Google Scholar]
- 17.Andresen EM, Fouts BS, Romeis JC, Brownson CA. Performance of health-related quality-of-life instruments in a spinal cord injured population. Arch Phys Med Rehabil. 1999;80:877–884. doi: 10.1016/s0003-9993(99)90077-1. [DOI] [PubMed] [Google Scholar]
- 18.Tate DG, Riley BB, Perna R, Roller S. Quality of life issues among women with physical disabilities or breast cancer. Arch Phys Med Rehabil. 1997;78(12 Suppl 5):S18–S25. doi: 10.1016/s0003-9993(97)90217-3. [DOI] [PubMed] [Google Scholar]
- 19.Westgren N, Levi R. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil. 1998;79:1433–1439. doi: 10.1016/s0003-9993(98)90240-4. [DOI] [PubMed] [Google Scholar]
- 20.Edwards L, Krassioukov A, Fehlings MG. Importance of access to research information among individuals with spinal cord injury: results of an evidenced-based questionnaire. Spinal Cord. 2002;40:529–535. doi: 10.1038/sj.sc.3101364. [DOI] [PubMed] [Google Scholar]
- 21.Leduc BE, Lepage Y. Health-related quality of life after spinal cord injury. Disabil Rehabil. 2002;24:196–202. doi: 10.1080/09638280110067603. [DOI] [PubMed] [Google Scholar]
- 22.Forchheimer M, McAweeney M, Tate DG. Use of the SF-36 among persons with spinal cord injury. Am J Phys Med Rehabil. 2004;83:390–395. doi: 10.1097/01.phm.0000124441.78275.c9. [DOI] [PubMed] [Google Scholar]
- 23.Lucke KT, Coccia H, Goode JS, Lucke JF. Quality of life in spinal cord injured individuals and their caregivers during the initial 6 months following rehabilitation. Qual Life Res. 2004;13:97–110. doi: 10.1023/B:QURE.0000015284.95515.17. [DOI] [PubMed] [Google Scholar]
- 24.Kreuter M, Siosteen A, Erkholm B, Bystrom U, Brown DJ. Health and quality of life of persons with spinal cord lesion in Australia and Sweden. Spinal Cord. 2005;43:123–129. doi: 10.1038/sj.sc.3101692. [DOI] [PubMed] [Google Scholar]
- 25.Elfstrom M, Ryden A, Kreuter M, Taft C, Sullivan M. Relations between coping strategies and health-related quality of life in patients with spinal cord lesion. J Rehabil Med. 2005;37:9–16. doi: 10.1080/16501970410034414. [DOI] [PubMed] [Google Scholar]
- 26.Oh SJ, Ku JH, Jeon HG, Shin HI, Paik NJ, Yoo T. Health-related quality of life of patients using clean intermittent catheterization for neurogenic bladder secondary to spinal cord injury. Urology. 2005;65:306–310. doi: 10.1016/j.urology.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE., Jr SF-36 health survey update. Spine. 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 28.Manocchia M, Bayliss MS, Connor J, Keller SD, Shiely JC, Tasai C, et al. SF-36 Health Survey Annotated Bibliography. Second Edition (1988-1996) Boston, MA: The Health Assessment Lab, New England Medical Center; 1998. [Google Scholar]
- 29.Guyatt GH. The philosophy of health-related quality of life translation. Qual Life Res. 1993;2:461–465. doi: 10.1007/BF00422220. [DOI] [PubMed] [Google Scholar]
- 30.Calman KC. Quality of life in cancer patients--an hypothesis. J Med Ethics. 1984;10:124–127. doi: 10.1136/jme.10.3.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Conroy L, McKenna K. Vocational outcome following spinal cord injury. Spinal Cord. 1999;37:624–633. doi: 10.1038/sj.sc.3100904. [DOI] [PubMed] [Google Scholar]
- 32.DeVivo MJ, Hawkins LN, Richards JS, Go BK. Outcomes of post-spinal cord injury marriages. Arch Phys Med Rehabil. 1995;76:130–138. doi: 10.1016/s0003-9993(95)80022-0. [DOI] [PubMed] [Google Scholar]
- 33.DeVivo MJ, Whiteneck GC, Charles ED. The economic impact of spinal cord injury. In: Stover SL, DeLisa JA, Whiteneck GC, editors. Spinal Cord Injury: Clinical Outcomes from the Model Systems. Gaithersburg, MD: Aspen Institute; 1995. pp. 242–269. [Google Scholar]
- 34.Lapides J, Diokno AC, Silber SJ, Lowe BS. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol. 1972;107:458–461. doi: 10.1016/s0022-5347(17)61055-3. [DOI] [PubMed] [Google Scholar]
- 35.Weld KJ, Dmochowski RR. Effect of bladder management on urological complications in spinal cord injured patients. J Urol. 2000;163:768–772. [PubMed] [Google Scholar]
- 36.Schwartz CE. Teaching coping skills enhances quality of life more than peer support: results of a randomized trial with multiple sclerosis patients. Health Psychol. 1999;18:211–220. doi: 10.1037//0278-6133.18.3.211. [DOI] [PubMed] [Google Scholar]