Abstract
Purpose
Most patients diagnosed with right-sided colonic diverticulitis complain of right lower quadrant pain, which is frequently confused for appendicitis and therefore may result in unnecessary emergency surgery. In this paper we intend to differentiate between right-sided colonic diverticulitis and appendicitis by initial presentation in the emergency department.
Materials and Methods
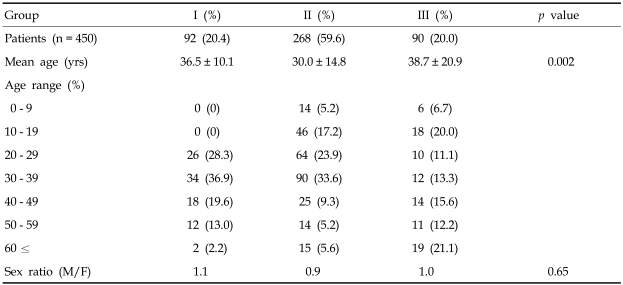
We retrospectively reviewed the medical records of 450 patients between January 1997 and July 2003. Among these patients, 92 with right-sided colonic diverticulitis were classified as group I; 268 patients with simple appendicitis were classified as group II; and 90 patients with perforated appendicitis were classified as group III.
Results
Prodromal symptoms were less common in group I (p < 0.05) than in the other groups. In comparing the location of maximal tenderness among groups, 19.6% of group I patients complained of maximal tenderness at a point lateral to McBurney's point, a greater percentage than those in groups II and III (p = 0.002). Group I experienced less leukocytosis (10,913.8/mm3) than did groups II (13,238.3/mm3) and III (15,589.3/mm3). The percentage of segmented forms in the differential counts was also smaller in group I (73.6%) than in groups II (79.1%) and III (81.8%). In addition, the proportion of lymphocytes was larger in group I (17.7%) than in groups II (13.9%) and III (9.3%).
Conclusion
Among patients complaining of right lower quadrant pain in an emergency setting, right-sided colonic diverticulitis must be considered in the following conditions to avoid unnecessary emergency operations: lack of prodromal symptoms, tenderness at a point lateral to McBurney's point, and absent or mild leukocytosis with a low fraction of segmented forms and a high fraction of lymphocytes in the CBC.
Keywords: Right-sided colonic diverticulitis, appendicitis, clinical features
INTRODUCTION
Right lower quadrant abdominal pain is one of the most common reasons for surgical consultation by emergency department physicians. In many cases, acute appendicitis is the cause of this pain. However, several other diseases present with similar symptoms and require differential diagnoses.
Colonic diverticulitis is one of many diseases that can present with right lower quadrant pain. Although, in the West, colonic diverticulitis is commonly left-sided, in the East the incidence is low and the process tends to develop in the cecum and ascending colon.1-3 Right-sided colonic diverticulitis generally occurs in patients who are 20 to 40 years of age. This younger age at presentation is in stark contrast to the typically older patients that develop left- sided colonic diverticulitis.
Acute appendicitis is also commonly found in relatively young patients with right lower quadrant pain. Therefore, in the East, it is often difficult to differentiate between right-sided colonic diverticulitis and acute appendicitis.4 For these reasons, 80% of patients with right-sided colonic diverticulitis are misdiagnosed on pre-op evaluation with acute appendicitis. Only 3-6% of these patients are diagnosed correctly before surgery.5
The optimal treatment for patients accurately diagnosed with right-sided colonic diverticulitis is a topic of controversy. Some insist that it is better to follow a conservative approach and treat patients with antibiotics alone, while others argue that it is better to treat the condition surgically.1,4,5-10 The aim of this study is to analyze the clinical differences between the two conditions and to enhance diagnostic accuracy in right-sided colonic diverticulitis.
MATERIALS AND METHODS
We performed a retrospective chart review of patients evaluated between January of 1997 and July of 2003 in the emergency department of Kangbuk Samsung Hospital. During this period, 1435 patients presented with right lower quadrant abdominal pain. Of these, 450 were diagnosed with and admitted for treatment of either acute appendicitis or right-sided colonic diverticulitis. Cases with right lower quadrant pain due to other processes were excluded. In addition, patients diagnosed with acute appendicitis or right-sided colonic diverticulitis were excluded if they were found to have peritonitis without pain in the right lower quadrant or if a palpable abdominal mass representing phlegmon formation was noted. Of the 450 patients, 92 patients were diagnosed with cecal or ascending colonic diverticulitis and were assigned to group I. The remaining 358 patients who were diagnosed with acute appendicitis were classified into two groups. Group II included 268 patients with simple appendicitis and group III included 90 patients with perforated appendicitis. Patient data included age, gender, prodromal symptoms, findings of the initial physical examination, and laboratory results. In our statistical analysis, the chi-square test, ANOVA, and the least significant difference test were employed. A p value less than 0.05 was considered significant.
RESULTS
Patient characteristics (Table 1)
Table 1.
Patient Characteristics
Group I Right sided colonic diverticulitis.
Group II Simple appendicitis.
Group III Perforated appendicitis.
The mean age of group I (36.5 ± 10.1 year) was not significantly different from that of group III (38.7 ± 20.9 years). In group I, 84.8% (78pts) were between the ages of 20 and 40. The mean age of group II (30.7 ± 14.8 years) was significantly less than both groups I and III. No difference in gender was observed among the three groups. There was also an equal prevalence of cecal or right-sided colonic diverticulitis in men and women (1.1:1).
Prodromal symptoms (Table 2)
Table 2.
Distribution of Prodromal Signs and Symptoms
*Statistical significance could not be assessed because of an insufficient number of medical records.
Fever and chills were experienced by 9 patients (9.8%) from group I, 29 patients (10.8%) from group II, and 30 patients (33.3%) from group III. The incidence of fever and chills in group I was similar to that of group II, but differed significantly from that of group III (p = 0.017).
The incidence of nausea and vomiting in group I (15pts, 16.3%) was significantly less than that in group II (86pts, 32.0%) and group III (30pts, 33.3%) (p = 0.028).
Characteristics of pain (Table 3)
Table 3.
Characteristics of Pain
*Statistical significance could not be assessed because of an insufficient number of medical records.
In group I, 32 (34.8%) patients complained of pain without rebound tenderness. In contrast, the incidence of rebound tenderness was relatively high in the cohort of patients with acute appendicitis. In terms of the location of maximal tenderness among the three groups, 18 patients (19.6%) from group I complained of maximal tenderness at a point lateral to McBurney's point, a percentage significantly higher than that of groups II and III (p = 0.002).
Laboratory results (Table 4)
Table 4.
Laboratory Results
The mean WBC count was significantly lower in group I (10,913/mm3) than in groups II (13,238.3/mm2) and III (15,589.3/mm2)(p = 0.003). The percentage of segmented cells in the differential counts was also lower in group I (73.6%) (p = 0.018). However, the percentage of lymphocytes was higher in group I (17.7%) than in the other two groups (p = 0.026).
DISCUSSION
A colonic diverticulum is an abnormal sac or pouch that is formed when the intestinal mucosa is either pulled or prolapsed through the surrounding muscular layers. The causes of this process are not completely understood. However, the incidence has increased as society has become more industrialized.4 According to Burkitt and Painter,11 industrialization promotes the intake of canned food, refined sugar, fat and protein, and reduces the intake of fiber. This diet causes a reduction in the volume of feces and increases the transit time of feces through the colon. These factors lead to an increase in the intensity of colonic muscular tone and colonic pressure which presents a higher risk of forming diverticula and subsequently developing diverticulitis.11,12 Differences exist between the features of diverticulitis in the East and the West. In the West, colonic diverticulitis is considered a common disease and occurs most often in the sigmoid and descending colon. The majority of cases originate with pseudodiverticula. These pseudodiverticula form as a result of the aforementioned degenerative process and their prevalence increases with age.13,14 Cecal and right-sided colonic diverticulitis, which are found mainly in Eastern society, including South Korea, were first reported by Poiter in 1912.14 In Korea, right-sided colonic diverticulitis was first reported by Kim et al in 1968.15 In most cases, diverticulitis arises from true diverticula and therefore represents a type of congenital diverticula. Seventy-eight percent of these diverticula are found between 1cm proximal to and 2cm distal from the ileocecal junction. Complications from these lesions typically arise in younger people. The incidence of right-sided diverticulitis is increasing as a result of the westernization of eating habits in Korea and Japan.2 Right lower quadrant abdominal pain is a common symptom both in patients with right-sided colonic diverticulitis and in patients with appendicitis. Park et al report that among 1,137 patients who underwent surgery for presumed appendicitis, 2.7% were later found to have diverticultis.16 Over the 6 years covered by this study, 1,343 patients were initially diagnosed with acute appendicitis and 92 of those patients (6.8%) were eventually found to have cecal or right-sided colonic diverticulitis.
The mean age of those with right-sided diverticulitis was 36.5 years, which is similar to the mean age of 36.8 years reported by Park, Sung et al. and 37.5 years by Park, Kim et al.16,17 A significant difference was observed in the mean age of group I as compared to that of group II (the simple appendicitis group), i.e. 36.5 vs. 30.7 years, respectively, while little difference was observed between groups I and III (the perforated appendicitis group), i.e., 36.5 vs. 38.7 years, respectively. The mean age of group I was relatively young with 84.8% of the patients ranging from 20 to 40 years old. In contrast, group III had a broader age range with peak incidences in patients younger than 10 years of age (26.6%), and older than 50 years of age (31.4%). It was found that for those patients in their 20's to 40's, the incidence of right-sided colonic diverticulitis expressed as a percentage of appendicitis was 8.9%.
Cho et al. reported that prodromal symptoms such as nausea and vomiting are less common in patients with cecal and right-sided colonic diverticulitis (26.7%) than in those with appendicitis (51%).18 Such findings indicate that prodromal symptoms, such as nausea and vomiting, occur less frequently in patients with right-sided colonic diverticulitis than in those with appendicitis. This was also confirmed by our present study in which only 15 of 92 patients (16.3%) with right-sided colonic diverticulitis complained of nausea and vomiting.
Painter stated that it is difficult to diagnose colonic diverticulitis before surgery. In addition, Kim et al. reported discovering cecal diverticulitis in 73% of patients with presumed acute appendicitis during surgery.19,20 Lee et al. pointed out that prior to surgery 80% of patients with cecal diverticulitis had been misdiagnosed with acute appendicitis.5 They also found that only 3-6% of patients were diagnosed correctly with diverticulitis prior to surgery. In most cases, when patients complain of right lower quadrant abdominal pain they are presumed to have appendicitis. In the present study, only patients with right lower quadrant abdominal pain were selected among all patients with presumed acute diverticulitis. In this study we analyzed the physical examination results of these selected patients. However, patients were excluded if: a) pain extended over the entire abdomen: and b) an easily palpable abdominal mass was present. Patients with classical appendicitis usually complain of pain and rebound tenderness at McBurney's point. Lauridsen noted that in diverticulitis complaints of pain and rebound tenderness are not clearly localized.21 However, it is difficult to find empirical studies that support the notion that abdominal pain characteristics can clearly differentiate right-sided diverticulitis from acute appendicitis. In the present study, the incidence of lower right quadrant pain without rebound tenderness was higher in group I (34.8%) than in groups II (17.5%) or III (11.1%). Suh et al. more accurately documented the area of maximal tenderness and found that in 58% of patients with cecal diverticulitis the point of maximum tenderness was lateral to McBurney's point.22 In this study, the maximum point of tenderness was found lateral to McBurney's point in 19.6% of cases in group I. Though this percentage is much lower than the results reported by Suh et al., it is still an appreciably higher percentage than found in groups II (0.8%) and III (2.2%). The possibility of right-sided colonic diverticulitis should be considered when patients complaining of right lower quadrant pain express maximum tenderness at a point lateral to McBurney's point.
Leukocytosis can be associated with appendicitis. Wagner et al. state that in their reviews the presence of only a moderate elevation in the white blood cell count is a factor that helps establish the diagnosis of diverticulitis prior to surgery.6,23,24 Suh et al. found that leukocytosis was present in 58% of patients with cecal diverticulitis and in 90% of patients with appendicitis.22 In addition, Chen et al. found statistical differences between the level of leukocytosis in diverticulitis (11,581.9/ mm3) and appendicitis (14,620.0/mm3)(p < 0.01).25 On the other hand, Cho et al. reported that the WBC count could not help to differentiate between diverticulitis and acute appendicitis.19 In our study, the median white blood cell count in group I was 10,918.3/mm3 and this was significantly lower than that of groups II (13,238.3/mm3) and III (15,589.3/mm3 (p = 0.003). Additionally, comparing the differential white blood cell counts, the percentage of segmented forms in group 1 was 73.6%, which was lower than that of groups II (79%) and III (81.8%)(p = 0.018). In addition, the percentage of lymphocytes in the differential counts was higher in group I (17.7%) than in groups II and III (13.9% and 9.3%, respectively) (p = 0.026).
In this study, we analyzed clinical features to aid in the differential diagnosis of patients presenting with acute right lower quadrant abdominal pain. Our results suggest that it is essential to include cecal or right-sided colonic diverticulitis within the differential diagnosis when there are either unclear or lacking prodromal symptoms such as nausea and vomiting; when a patient complains of tenderness without rebound signs at a point lateral to McBurney's point; and when the white blood cell differential count shows a near- normal percentage of segmented cells and an elevated proportion of lymphocytes.
References
- 1.Almy TP, Howell DA. Medical Progress. Diverticular disease of the colon. N Engl J Med. 1980;302:324–331. doi: 10.1056/NEJM198002073020605. [DOI] [PubMed] [Google Scholar]
- 2.Sugihara K, Muto T, Morioka Y, Asano A, Yamamoto T. Diverticular disease of the colon in Japan. A review of 615 cases. Dis Colon Rectum. 1984;27:531–537. doi: 10.1007/BF02555517. [DOI] [PubMed] [Google Scholar]
- 3.Kim JS, Cha SG, Kim YT, Yoon YB, Song IS, Choi KW, et al. The prevalence and clinical features of Diverticular disease of the colon. Korean J Gastroenterol. 1993;25:305–314. [Google Scholar]
- 4.Graham SM, Ballantyne GH. Cecal diverticulitis. A review of the American experience. Dis Colon Rectum. 1987;30:821–826. doi: 10.1007/BF02554637. [DOI] [PubMed] [Google Scholar]
- 5.Lee KJ, Hyun TI. Clinical evaluation of colonic diverticular disease. J Korean Surg Soc. 1995;11:100–106. [Google Scholar]
- 6.Arrington P, Judd CS., Jr Cecal diverticulitis. Am J Surg. 1981;142:56–59. doi: 10.1016/s0002-9610(81)80012-8. [DOI] [PubMed] [Google Scholar]
- 7.Vignati PV, Welch JP, Cohen JL. Long term management of diverticulitis in young patients. Dis Colon Rectum. 1995;38:627–629. doi: 10.1007/BF02054123. [DOI] [PubMed] [Google Scholar]
- 8.Harada RN, Whelan TJ., Jr Surgical management of cecal diverticulitis. Am J Surg. 1993;166:666–671. doi: 10.1016/s0002-9610(05)80676-2. [DOI] [PubMed] [Google Scholar]
- 9.Chung YL, Kin WC. Acute diverticulitis of the right colon. Am J Surg. 1996;171:244–246. doi: 10.1016/S0002-9610(97)89559-1. [DOI] [PubMed] [Google Scholar]
- 10.Ngoi SS, Chia J, Goh MY, Sim E, Rauff A. Surgical management of right colon diverticulitis. Dis Colon Rectum. 1992;35:799–802. doi: 10.1007/BF02050332. [DOI] [PubMed] [Google Scholar]
- 11.Burkitt DP, Walker AR, Painter NS. Dietary fiber and disease. JAMA. 1974;229:1068–1074. [PubMed] [Google Scholar]
- 12.Burkitt DP, Walker AR, Painter NS. Effect of dietary fibre on stools and the transit-times, and its role in the causation of disease. Lancet. 1972;2:1408–1412. doi: 10.1016/s0140-6736(72)92974-1. [DOI] [PubMed] [Google Scholar]
- 13.Hackford AW, Schoetz DJ, Jr, Coller JA, Veidenheimer MC. Surgical management of the complicated diverticulitis. The Lahey Clinic experience, 1967 to 1982. Dis Colon Rectum. 1985;28:317–321. doi: 10.1007/BF02560431. [DOI] [PubMed] [Google Scholar]
- 14.Poiter F. Diverticulite et appendicite. Bull Mem Soc Anat (Paris) 1912;137:29–33. (Cited from A.M.A Arch Surg 1961;83:436) [Google Scholar]
- 15.Kim KY, Kim HS, Kim IH, Chun EC. Cecal diverticulitis. J Korean Surg Soc. 1968;10:249–252. [Google Scholar]
- 16.Park CW, Kim BG, Kim KS, Byun YH, Cho KH, Byun SH, et al. Surgical management of cecal diverticulitis detected during appendectomy. J Korean Soc Coloproctol. 2001;17:15–19. [Google Scholar]
- 17.Park JK, Sung JK, Choi SH, Yun SS, Lee S. Clinical analysis of right colon diverticulitis. J Korean Surg Soc. 2003;64:44–48. [Google Scholar]
- 18.Cho HJ, Cho SY, Oh JH. Clinical analysis of right colonic diverticulitis that was operated under the impression of acute appendicitis. J Korean Soc Coloproctol. 2000;16:18–24. [Google Scholar]
- 19.Painter NS. The cause of diverticular disease of the colon, its symptoms and its complication. Review and hypothesis. J R Coll Surg Edinb. 1985;30:118–122. [PubMed] [Google Scholar]
- 20.Kim W, Lee DS, Suh YJ, Cho WI, Oh ST, Jin HM, et al. Cecal diverticulitis. J Korean Surg Soc. 1996;50:116–123. [Google Scholar]
- 21.Lauridsen J, Ross FP. Acute diverticulitis of the cecum; a report of four cases and review of one hundred fifty-three surgical cases. AMA Arch Surg. 1952;64:320–330. [PubMed] [Google Scholar]
- 22.Suh KW, Suh YJ, Choi JS, Yoo CH, Kim JH. Clinically differential diagnosis of cecal diverticulitis from appendicitis. J Korean Surg Soc. 1996;12:94–98. [Google Scholar]
- 23.Sasso RD, Hanna EA, Moore DL. Leukocytic and neutrophilic counts in acute appendicitis. Am J Surg. 1970;120:563–566. doi: 10.1016/s0002-9610(70)80168-4. [DOI] [PubMed] [Google Scholar]
- 24.Wagner DE, Zollinger RW. Diverticulitis of the cecum and ascending colon. Arch Surg. 1961;83:436–443. doi: 10.1001/archsurg.1961.01300150110014. [DOI] [PubMed] [Google Scholar]
- 25.Chen SC, Chang KJ, Wei TC, Yu SC, Wang SM. Can cecal diverticulitis be differentiated from acute appendicitis? J Formos Med Assoc. 1994;93:263–265. [PubMed] [Google Scholar]