Abstract
Histoplasmosis is a very rare disease in Korea. Clinical manifestations are very similar to those of tuberculosis. This is the first case report of combined disseminated histoplasmosis and tuberculosis in a patient with HIV infection in Korea. A 42-year-old Korean with Acquired Immunodeficiency Syndrome (AIDS) was diagnosed with tuberculosis. He had lived in Guatemala for the past five years. Upon diagnosis of disseminated tuberculosis with HIV infection, he was treated with anti-tuberculosis medications and anti-retroviral agents. Fever, weakness, hepatosplenomegaly and pancytopenia were persistent despite treatment. The patient's history of living in Guatemala caused us to seek opportunistic infectious organisms other than tuberculosis. Bone marrow aspiration and biopsy were performed and the result revealed numerous intracellular organisms consistent with Histoplasma capsulatum; therefore, the diagnosis of disseminated histoplasmosis was made.
Keywords: Histoplasmosis, HIV infections, AIDS, tuberculosis
INTRODUCTION
The clinical features of disseminated histoplasmosis are similar to those of disseminated tuberculosis.1 Fever, cachexia, hepatosplenomegaly, lymphadenopathy, abnormal liver function tests, anemia, leukopenia, and thrombocytopenia are common symptoms of both disseminated tuberculosis and histoplasmosis. These similarities can cause a delay in diagnosing histoplasmosis in an AIDS patient with confirmed tuberculosis.
Histoplasmosis is prevalent in the Midwestern United States along the Mississippi river bed, parts of the Caribbean Islands, and in South and Central America.2 In endemic areas, the incidence of histoplasmosis among patients with AIDS is 5% to 20%.2 In areas where histoplasmosis is not endemic, it is often neglected in the differential diagnosis of opportunistic infections associated with AIDS. Since more people are spending time abroad, physicians should consider other opportunistic infections in addition to common organisms.
We report a case of disseminated histoplasmosis and tuberculosis in a patient with Human Immunodeficiency Virus (HIV) infection in Korea. This case confirms the importance of considering histoplasmosis as a possible diagnosis in AIDS patients with confirmed tuberculosis and the importance of taking a patient's residence history.
CASE REPORT
The patient, a 42-year old man, presented to the infectious diseases clinic at the Korea University Anam (KU) Hospital with symptoms of generalized weakness and fever. Generalized weakness, fever and cough developed 3 months prior to presentation. The patient had experienced a 12-kg weight loss.
The patient had been living in Guatemala for five years and had sought medical attention there. He was told that the serum HIV-antibody test done by enzyme-linked immunosorbent assay (ELISA) and sputum AFB smear were positive. Immediately after the diagnosis of AIDS, he came home to Seoul, South Korea.
An HIV-1 Western blot test was done at a separate hospital to confirm the diagnosis and the result was positive. The CD4 cell count was 10/µL and the HIV RNA titer was 18,000 copies/mL. Anti-tuberculosis medications (isoniazid, rifampin, ethambutol, pyrazinamide) were started and continued for 40 days. Fluconazole and trimethoprim/sulfamethoxazole were given as prophylaxis because of the low CD4 cell count.
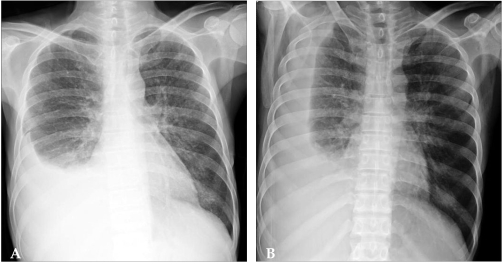
Despite the treatment, his generalized weakness and fever continued. He was then transferred to KU hospital. Upon admission, his body temperature was 37.6℃. He had oral thrush and hepatosplenomegaly with ascites. Laboratory results on the day of admission were as follows: hemoglobin 10.6g/dL, white blood cell 2,700/µL, platelet 58,000/µL, total bilirubin 2.4mg/dL, AST/ALT 131/48IU/L, ALP 114IU/L, GGT133 IU/L. Chest X-ray showed costophrenic angle blunting and fluid shifting in the right hemithorax and mild pneumonic infiltration in left lung (Fig. 1).
Fig. 1.
Chest X-ray. (A) Chest PA, (B) Chest right decubitus view- Right side pleural effusion and mild peribronchial infiltrations are seen.
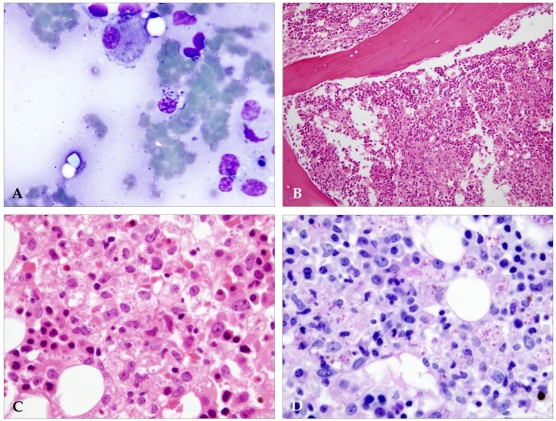
Disseminated tuberculosis was suspected. As Mycobacterium tuberculosis was identified from his sputum cultured at another hospital in Seoul, anti-tuberculosis medication was continued even though the sputum AFB smear done at the time of admission to KU hospital was negative. Anti-retroviral agents (zidovudine, lamivudine, efavirenz) were started on admission day 1. The severity of the pancytopenia progressed rapidly; the laboratory tests showed a hemoglobin of 7.4g/dL, a white blood cell count of 1,070/µL and a platelet count of 13,000/µL. Rifampin, zidovudine, and trimethoprim/sulfamethoxazole were discontinued due to possible bone marrow suppression associated with these medications. However, pancytopenia persisted. On day 5, the patient developed new pulmonary infiltrates and septic shock; empirical antibiotic therapy with piperacillin/tazobactam was started. On day 6, the patient was transferred to the intensive care unit for mechanical ventilator support. Gram stain and ordinary culture from sputum and blood revealed no pathologic organisms. Despite treatment, the pancytopenia, pneumonia, and hepatosplenomegaly did not improve. A bone marrow aspiration and biopsy were performed on day 9. However, the patient died on day 10 as a result of refractory septic shock and hypoxia. The results of the bone marrow aspiration smears and biopsy revealed numerous intra-cytoplasmic organisms identified as Histoplasma capsulatum (Fig. 2); this patient was confirmed to have concomitant disseminated histoplasmosis.
Fig. 2.
Bone marrow aspirates and biopsies. (A) Bone marrow aspirate, Wright-Giemsa stain × 1000. Numerous intracellular Histoplasma capsulatum are seen in several histiocytes. (B) Bone marrow biopsy, H & E stain × 100. The bone marrow is hypercellular and is packed with macrophages and eosinophils. The number of normal hematopoietic elements is markedly decreased. (C) Bone marrow biopsy, H & E stain × 1000. At high magnification, the infiltrate consists of macrophages which contain small, oval yeasts within their cytoplasm. A single nuclear mass can be seen in most yeast cells. (D) Bone narrow biopsy, PAS stain × 1000. The small yeasts are well demonstrated by PAS stain, which highlights the single nuclear body. The intracellular location of the yeast is clarified by clustering.
DISCUSSION
The prevalence of tuberculosis in Korea is high. It affects about 1% of the total population. Tuberculosis is one of the major opportunistic infections in Korean HIV-infected patients,3 but histoplasmosis is very rare. It is prevalent in the mid-western United States along the Mississippi river bed, the Caribbean Islands, and parts of South and Central America.2 In such areas, the incidence of histoplasmosis among patients with AIDS is 5% to 20%.2 The development of histoplasmosis can be due to a primary infection, reinfection, or reactivation.4,5 Primary infections are either asymptomatic or mild influenza-like illnesses with fever, headache, nonproductive cough and chest discomfort.6 Most symptoms resolve spontaneously after a few days. In endemic areas, people who are reexposed to a large inoculum of histoplasma may show reinfection with fever, cough and myalgia that are usually milder than the symptoms of primary infection. Infected individuals remain hosts for many years. The dormant organisms can be active when the individual becomes immunosuppressed. Because of severe immunosuppression, most of the reports of histoplasmosis in AIDS patients are of disseminated cases.7
Histoplasmosis was not considered in the initial evaluation of this patient because the clinical features were consistent with tuberculosis and there was consistent evidence of tuberculosis. When we reviewed the literature, we did find a few cases of histoplasmosis misdiagnosed as tuberculosis in Europe and Malaysia.8,9 In those cases, the similarity of clinical symptoms between tuberculosis and histoplasmosis may have delayed the diagnosis of histoplasmosis.
There have been two reported cases of histoplasmosis in Korea. A newborn was diagnosed based on a peripheral blood smear.10 The second case was a foreign worker diagnosed with histoplasma peritonitis based on a laparoscopic biopsy.11 The evaluation of these two patients did not include complete immunological work-ups, nor was there a medical history to reveal possible exposure to HIV. There was no follow-up information available for these patients. Due to our patient's recent travel abroad, it is presumed that he acquired histoplasma in Guatemala.
Studying lung samples obtained by bronchoscopy, it has been documented that AIDS patients with pulmonary manifestations have rates as high as 90% histoplasma-positive cultures.6 Reports have also shown that bone marrow and blood cultures are positive in up to 50% of disseminated histoplasmosis patients.12 In our case, the fungal culture of sputum showed no organisms. A fungal culture of the peripheral blood and bone marrow was performed only after further diagnostic investigation.
Since work ups for the possible drug-resistant tuberculosis were not done in the previous two hospitals, one in Guatemala and the other in Seoul, the possibility of resistance to antituberculous agents in this patient cannot be ruled out. Since this patient's sputum AFB smear and culture showed negative conversion after antituberculous medication, it is unlikely that the cause of death of the patient was uncontrolled tuberculosis.
In addition to common tuberculosis, physicians need to be aware of histoplasmosis as a possible infection in immunocompromised patients because disseminated histoplasmosis and tuberculosis have similar clinical manifestations.
References
- 1.Raviglione MC, O'Brien RJ. Tuberculosis. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Principles of Internal Medicine. 15th ed. vol. 1. New York: McGraw-Hill; 2005. pp. 953–966. [Google Scholar]
- 2.Wheat LJ, Kauffman CA. Histoplasmosis. Infect Dis Clin North Am. 2003;17:1–19, vii. doi: 10.1016/s0891-5520(02)00039-9. [DOI] [PubMed] [Google Scholar]
- 3.Han YC. Tuberculosis in the past, present and future. In: Hong YP, KIM SJ, editors. Tuberculosis. 4th ed. Seoul: The Korean National Tuberculosis Association; 2000. pp. 1–8. [Google Scholar]
- 4.Wheat J. Histoplasmosis. Experience during outbreaks in Indianapolis and review of the literature. Medicine (Baltimore) 1997;76:339–354. doi: 10.1097/00005792-199709000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hajjeh RA. Disseminated histoplasmosis in persons infected with human immunodeficiency virus. Clin Infect Dis. 1995;21(Suppl 1):S108–S110. doi: 10.1093/clinids/21.supplement_1.s108. [DOI] [PubMed] [Google Scholar]
- 6.Deepe GS., Jr . Histoplasma capsulatum. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 6th ed. vol. 2. Philadelphia: Elsevier Churchill Livingstone; 2005. pp. 3012–3026. [Google Scholar]
- 7.Wheat LJ, Connolly-Stringfield PA, Baker RL, Curfman MF, Eads ME, Israel KS, et al. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore) 1990;69:361–374. doi: 10.1097/00005792-199011000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Pometta R, Trovato C, Vivani MA, Masini T, Conte D. Chronic pulmonary histoplasmosis in a patient with a recent history of tuberculosis and persistent round lung lesions. Eur J Clin Microbiol Infect Dis. 1999;18:229–231. doi: 10.1007/s100960050267. [DOI] [PubMed] [Google Scholar]
- 9.Chan KS, Looi LM, Chan SP. Disseminated histoplasmosis mimicking miliary tuberculosis: a case report. Malays J Pathol. 1993;15:155–158. [PubMed] [Google Scholar]
- 10.Jeon DS, Kim JR, Chun HJ, Hong YA, Kim WT. A case of histoplasmosis diagnosed on peripheral blood smear. Korean J Hematol. 1991;26:391–396. [Google Scholar]
- 11.Kim HS, Kim KA, Kwon KS, Cho HK, Kim BS, Lee DH. A Case of histoplasma peritonitis. Inha Med J. 1999;6:135–141. [Google Scholar]
- 12.Wheat LJ. Laboratory diagnosis of histoplasmosis: update 2000. Semin Respir Infect. 2001;16:131–140. doi: 10.1053/srin.2001.24243. [DOI] [PubMed] [Google Scholar]