Abstract
Purpose
To investigate the correlation between gadolinium enhanced magnetic resonance image (MRI) results and surgical findings of facial nerves in Bell's palsy and Ramsay Hunt syndrome.
Materials and Methods
From 1995 to 2004, MRI was performed on 13 patients with Bell's palsy or Ramsay Hunt syndrome, who were offered with surgical decompression of the facial nerve through the middle cranial fossa approach. Gadolinium enhanced MRI was performed on all patients and the enhancement of the facial nerve was evaluated by radiology specialists. Operative findings including the degree of the facial nerve segment swelling were examined. Furthermore, the time interval from the onset of palsy to surgery was evaluated.
Results
Swelling of facial nerve segments was found in patients with enhanced facial nerves from MRI. The swelling of the facial nerve in the labyrinthine segment in particular was identified in all patients with enhanced labyrinthine segments in MRI. The intraoperative swelling of geniculate ganglion of facial nerve was found in 78% of patients with enhanced facial segment in MRI (p = 0.01). The intraoperative swelling of tympanic segment was observed from fourth to ninth weeks after the onset of palsy.
Conclusion
MRI enhancement of facial nerves in Bell's palsy and Ramsay Hunt syndrome is associated with the extent of intratemporal lesions of facial nerves, especially in the labyrinthine segment.
Keywords: Bell's palsy, herpes zoster oticus, MRI, facial nerve
INTRODUCTION
Bell's palsy accounts for 80% of all peripheral facial palsies diagnosed annually and it is known to occur in 20 - 30 people per 100,000 per year. The facial palsy in Bell's palsy and Ramsay Hunt syndrome is thought to be due to the activity of latent viruses which cause neural degeneration.1,2 Bell's palsy is attributed to inflammation of facial nerves due to Herpes simplex virus (HSV) infection. Herpes zoster oticus, caused by varicella zoster virus (VZV) in the geniculate ganglion (Hunt, 1907), yields more severe symptoms of facial palsy and higher risk of complete nerve degeneration.
If first developed in the geniculate ganglion, inflammation proceeds proximally and distally, causing facial palsy due to the physical pressure on the narrow facial canal. There have been attempts to identify these nerve changes in MRI, a technology known for visualization of soft tissue lesions. Contrast enhancement in MRI can be seen in the neural degeneration cases due to destruction of the blood-peripheral barrier. There is no consensus regarding the correlation of the image findings with the prognosis of facial palsy, with some authors reporting correlation with bad prognosis, while others believe there is no correlation.3-6 However, most of these reports analyzed only the frequency and site of enhancement in Bell's palsy and Ramsay Hunt syndrome and compared the findings with clinical progress. There has been a report on the correlation between T2 weighted three dimensional fast spin echo MRI and intraoperative findings for facial nerves in peripheral facial nerve palsy.7
The purpose of this study was to investigate the correlation between the swelling of the facial nerve and visualization of an enhanced segment by MRI. Furthermore, we investigated the swelling of the facial nerve in accordance with time after symptom onset.
MATERIALS AND METHODS
We retrospectively analyzed the medical charts of 13 patients who were diagnosed with either Bell's palsy or Ramsay Hunt syndrome from 1995 to 2004 and their MRI scan upon the diagnosis. MRI scan was taken in all patients to exclude other pathology. The male-to-female ratio was 7:6 and the average age was 47 years old. There were 5 cases of right side palsy and 8 cases with the left side. Seven patients were diagnosed with Bell's palsy and 6 patients with Ramsay Hunt syndrome. All patients underwent facial nerve decompression via the middle cranial fossa approach (MCFA) with any of following conditions; no symptomatic improvement despite medical treatment, degeneration ratio more than 90% by electroneuronography (ENoG), or no evidence of recovery upon facial electromyography. On cases with partial paralysis of House-Brackmann (H-B) grade IV, surgical decompression was done when they showed no evidence of recovery. For medical treatment, steroids and anti-viral agents were used.
Age, sex, the degree of facial palsy on admission, the time interval between the symptom onset and the MRI scan, the enhanced facial nerve on MRI, the time interval between the symptom onset and the surgery and intraoperative finding of the facial nerve were analyzed in all patients. During surgery, the surgeon determined the swelling of facial nerve under operating microscope. The intraoperative swelling of facial nerve was determined by the extension of swelling beyond facial canal or the degree of bulging through the incision in the nerve sheath.
MRI scans were taken with a 3 mm thickness image on an intera 1.5T instrument (Phillips Medical Systems, Best, The Netherlands). Gadolinium-diethylenetriamine pentacetic acid (Gd-DTPA) was used as a contrast medium with a dosage of 0.1 mmol/kg given intravenously. The film was read by a radiology specialist who was unaware of the lesion. The degree of facial palsy was graded according to the House-Brackmann classification. The analysis of time versus degree of nervous swelling and its correlation to other factors was done with a Fisher's exact test.
RESULTS
All 13 patients showed at least a H-B grade IV facial palsy upon admission, within which there were 10 cases with grade V and 1 case with grade VI. The time interval from the symptom onset to MRI scan ranged from 5 to 53 days with an average of 19 days. All patients underwent facial nerve decompression via MCFA within an average of 37 days (range 8 to 75 days) after symptom onset (Table 1).
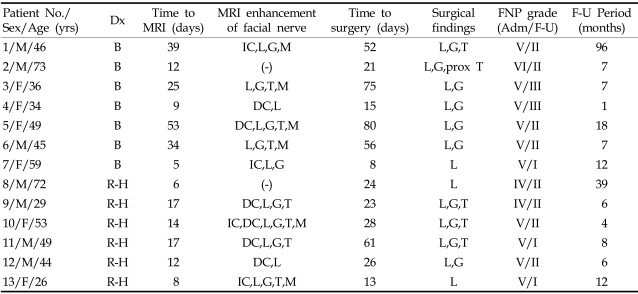
Table 1.
Baseline Clinical Data (Clinical Characteristics of Patients with Bell's Palsy or Ramsay-Hunt Syndrome)
Dx, diagnosis; B, Bell's palsy; R-H, Ramsay Hunt syndrome; (-), No enhancement; IC, intracanalicular segment; DC, distal intracanalicular segment; L, labyrinthine segment; G, geniculate ganglion; T, tympanic segment; M, mastoid segment; Prox T, proximal tympanic segment of facial nerve; Surgical finding, swelling segment of facial nerve in surgical field; FNP grade, facial nerve palsy with House-Brackmann grade; Adm/F-U, admission/last follow up.
Except for the two cases, all patients showed enhancement in the labyrinthine segment in MRI scan. Enhancement of the intracanalicular and geniculate ganglion were seen in 9 cases, and enhancement in the tympanic segment, and mastoid segment were also noted (Table 2). Of the cases that showed intracanalicular enhancement, there were 5 patients with enhancement of the distal intracanalicular segment and 4 patients with enhancement of the entire intracanalicular segment, although all cases were labeled as intracanalicular segment enhancement.
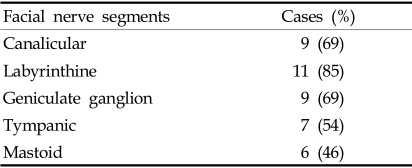
Table 2.
MRI-Enhanced Segments of the Facial Nerve (n = 13)
Intraoperative findings of the facial nerve change demonstrated edema of the labyrinthine segment in all patients with enhanced facial nerve in MRI and hemorrhage in one case of Ramsay Hunt syndrome. The frequency of occurrence for edema decreased toward the geniculate ganglion and distal portion of the tympanic segment (Table 3).
Table 3.
Swollen Segments of the Facial Nerve (n=13)
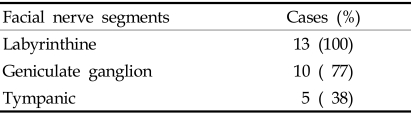
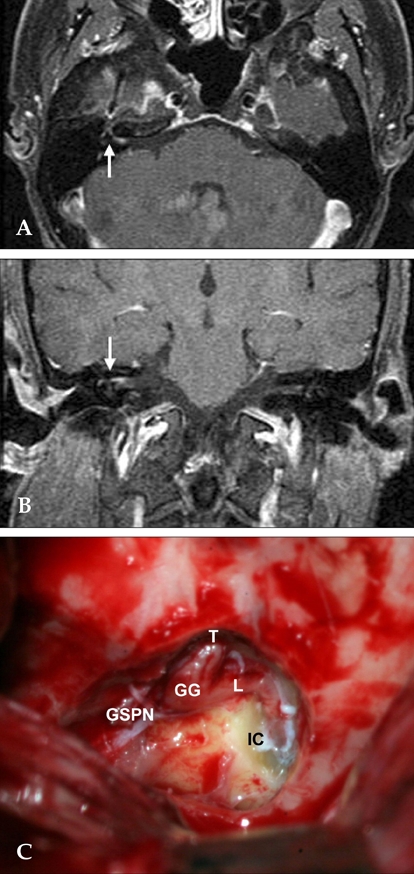
Fig. 1 shows the MRI and operative findings in a patient with Ramsay Hunt syndrome. The enhanced area of facial nerve correlated with the swollen area during surgery. The relationship between the MRI findings and the degree of intraoperative facial nerve edema was that all patients with enhancement of the labyrinthine segment in MRI had intraoperative edema at the labyrinthine segment of the facial nerve except for the two cases that did not show enhancement of facial nerve in MRI. Facial nerve edema was also seen in the two patients without enhancement on MRI. Of the 9 cases that had enhanced MRI of the geniculate ganglion, the edema of the facial nerve was actually seen in 7 patients. Of the 7 cases that had enhanced MRI of tympanic segment, the edema of the facial nerve was seen in only 3 patients. Thus, there was a statistically significant correlation between the enhancement of the facial nerve and the actual site of nerve edema with Fisher's exact test (p = 0.01) (Fig. 2).
Fig. 1.
MRI and operative findings in a patient with Ramsay Hunt syndrome (right). (A) Axial contrast enhanced T1 image demonstrates enhancement from the lateral canalicular to the proximal tympanic segment of right facial nerve (arrow). (B) Coronal T1 weighted Gd-MRI shows enhancement of right facial nerve (arrow). (C) Photograph shows edematous swelling along the decompressed segment of facial nerve in MRI enhanced areas. IC, intracanalicular segment; L, labyrinthine segment; GG, geniculate ganglion; T, tympanic segment; GSPN, greater superficial petrosal nerve.
Fig. 2.
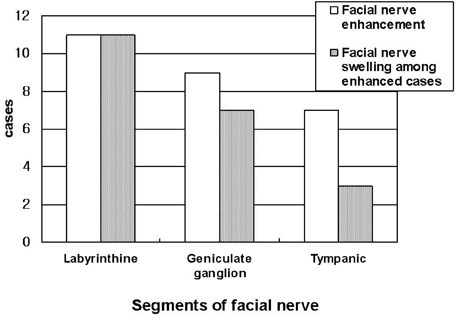
Correlation between MR enhancement and swelling of facial nerve (p = 0.01).
The time interval between the symptom onset and surgery illustrates that the labyrinthine segment swelling was mainly seen in cases where the surgery was performed within 3 weeks, while change of the labyrinthine, geniculate ganglion and tympanic segment were in cases in which surgery was performed 3 to 9 weeks after the symptom onset. In the patients whose surgery was performed 9 weeks after symptom onset, changes in the labyrinthine segment and geniculate ganglion only were observed (Fig. 3).
Fig. 3.
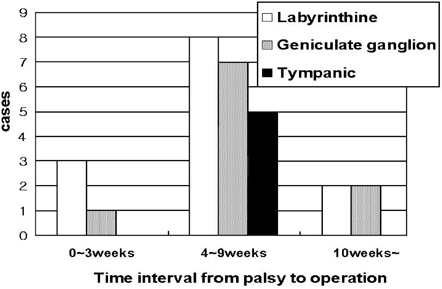
Facial nerve swelling in accordance with the time interval from the palsy onset to the surgery (p = 0.66).
DISCUSSION
Facial palsy develops from various causes and the prognosis ranges from full recovery to permanent conditions. The etiology of facial palsy includes trauma, unknown causes, Human Immunodeficiency Virus infection,8 iatrogenic causes, tumor, congenital causes, and particularly in Bell's palsy and Ramsay Hunt syndrome, viral infection. The cause of Bell's palsy was previously thought to be unknown, but Murakami et al. found HSV-1 DNA in the perineural fluid of a patient who underwent facial nerve decompression during the acute stage of Bell's palsy.9 Additionally, the Iowa group revealed the presence of HSV-1 DNA in the temporal bone of a patient who died 6 days after developing Bell's palsy.10 Moreover, Bell's palsy was induced by injecting HSV into the auricle or tongue in an animal model.11 Adding antiviral agents to the treatment protocol was more effective than steroid treatment alone in double blind steroid trials.12 Taken together, these studies support the etiology of Bell's palsy being the virus. In contrast, other authors reported that adding antiviral agents to the treatment protocol was not statistically better than steroid treatment alone.13
Through such viral activity, inflammation occurs in the geniculate ganglion of the facial nerve and progresses distally or proximally. The meatal foramen, which connects the internal auditory canal to the facial canal, is the narrowest portion of the facial nerve and as such is subject to high pressure, even if the degree of inflammation change is the same. As a result, decompression of this portion of the facial nerve is mandatory when performing facial nerve decompression.14 Therefore, in cases where surgical decompression is needed, decompression via MCFA is more effective than the transmastoid approach commonly performed during the early stages. For this reason, we performed facial nerve decompression via MCFA in all patients with surgical needs. In all patients, edema and swelling was observed in the labyrinthine segment of the facial nerve.
The change in the nerve decreased towards the geniculate ganglion or distal portion of the tympanic segment. Yanagihara et al. observed changes in the facial nerve in Bell's palsy and Ramsay Hunt syndrome patients over time.15,16 They reported that facial nerve edema lasted longer and was more severe in Ramsay Hunt syndrome than in Bell's palsy, but in all patients, the edema proceeded from the geniculate ganglion towards the peripheral area as time progressed and the facial nerve edema decreased. As for the intraoperative finding according to symptom onset, the edema of the labyrinthine segment was mainly observed, and the tympanic segment edema was seen in the subacute phase, 3 to 9 weeks after symptom onset. However, as time progressed, the edema remained only in the labyrinthine and geniculate ganglion.
Enhancement is noted in the case of nerve degeneration due to the destruction of the blood-peripheral nerve barrier. There have been many reports on contrast enhancement seen in Bell's palsy and Ramsay Hunt syndrome, but it is difficult to distinguish between the two conditions from the enhancement patterns.17 Gebarski et al. reported that the labyrinthine, the internal auditory canal segment of facial nerve, which is most easily enhanced due to poor AVP vascularity, was never enhanced in normal facial nerve. But they found the geniculate ganglion, the proximal greater superficial petrosal nerve, and tympanic segment was enhanced in 76%. The facial nerve may normally be enhanced anterior and posterior to the rich arterio-venous plexus around the geniculate ganglion, particularly in the tympanic and mastoid segments.18
In facial palsy, contrast enhancement reports differ depending on the investigator. Some authors report that enhancement is seen most frequently seen in the geniculate ganglion of symptomatic facial nerves.19 Kinoshita, etc. reported that the contrast enhancement of the distal intrameatal and labyrinthine segments was respectively found in 67% and 43% of the 125 patients with Bell's palsy and the contrast enhancement of the geniculate ganglion or the tympanic-mastoid segments was found in 91% of patients with Bell's palsy.20 Yanagida, etc. reported that the contrast enhancement of the distal intrameatal or labyrinthine segments was respectively found in 64% of the 14 patients with Ramsay Hunt syndrome.21
Some authors reported a correlation between enhancement and prognosis,3,4 while others reported the opposite.5,6 Absence of contrast enhancement can also be observed, and in our study, contrast enhancement could not be seen in 2 cases. This is thought to be due to the progression of swelling of the nerve, which disturbs the circulation around the nerve, which in turn decreases the diffusion of the contrast around the nerve.
These various opinions are bounded by the clinical limitations of MRI, but in this study, enhancement of the labyrinthine segment was seen in all patients but two. Comparing the MRI findings with the actual intra-operative findings, the edema of labyrinthine segment of the facial nerve was seen in all patients with enhancement of the labyrinthine segment. As for the geniculate ganglion, edema was seen in 78% of the patients with enhanced MRI. However, edema was actually seen in only 43% of the patients showing enhancement of the tympanic segment in MRI. Thus, there is less correlation between the MRI findings and actual nerve edema in tympanic segment. One possible explanation is that the tympanic segment has a greater amount of normal arterio-venous plexus than the labyrinthine or geniculate ganglion, so that even without the presence of nerve edema, enhancement can be observed. Considering the etiologies of Bell's palsy and Ramsay Hunt syndrome, the labyrinthine segment is influenced the most because it is located at the meatal foramen which is the narrowest part, and therefore enhancement is easily found in MRI and edema noted. However, as the time interval between MRI scan and the diagnosis varies along with the time interval from the diagnosis to the surgery, these differences may effect the changes in the lesion. In general, the continuation of contrast enhancement lasts longer than the clinical recovery, which is a limitation of the study.22 In addition, steroids can affect contrast enhancement but we did not control the role of steroid therapy. The small population in this study warrants a larger work to confirm our results.
Despite these limitations, we were able to identify the enhanced nerve segment on temporal MRI scans in Bell's palsy and Ramsay Hunt syndrome and compared it with the actual injured facial nerve segment observed upon performing facial nerve decompression via the middle cranial fossa approach. Cases of Bell's palsy and Ramsay Hunt syndrome treated with facial nerve decompression showed frequent enhancement of the labyrinthine segment on MRI scans. In all cases with enhancement in MRI, the edema of the actual labyrinthine segment of the facial nerve was observed. Subsequently, we believe that MRI scan is feasible in demonstrating the changes of the facial nerve, and the decompression of the labyrinthine segment during surgery is essential.
References
- 1.Adour KK, Bell DN, Hilsinger RG., Jr Herpes simplex virus in idiopathic facial paralysis (Bell's palsy) JAMA. 1975;233:527–530. [PubMed] [Google Scholar]
- 2.Giannoni E, Corbacelli A. Virological findings and their correlation with immunological findings in Bell's paralysis. Boll Soc Ital Biol Sper. 1975;51:139–143. [PubMed] [Google Scholar]
- 3.Engström M, Thuomas KA, Naeser P, Stålberg E, Jonsson L. Facial nerve enhancement in Bell's palsy demonstrated by different gadolinium-enhanced magnetic resonance imaging techniques. Arch Otolaryngol Head Neck Surg. 1993;119:221–225. doi: 10.1001/archotol.1993.01880140111017. [DOI] [PubMed] [Google Scholar]
- 4.Murphy TP. MRI of the facial nerve during paralysis. Otolaryngol Head Neck Surg. 1991;104:47–51. doi: 10.1177/019459989110400110. [DOI] [PubMed] [Google Scholar]
- 5.Brändle P, Satoretti-Schefer S, Böhmer A, Wichmann W, Fisch U. Correlation of MRI, clinical, and electroneuronographic findings in acute facial nerve palsy. Am J Otol. 1996;17:154–161. [PubMed] [Google Scholar]
- 6.Kohsyu H, Aoyagi M, Tojima H, Tada Y, Inamura H, Ikarashi T, et al. Facial nerve enhancement in Gd-MRI in patients with Bell's palsy. Acta Otolaryngol Suppl. 1994;511:165–169. doi: 10.3109/00016489409128325. [DOI] [PubMed] [Google Scholar]
- 7.Sartoretti-Schefer S, Kollias S, Wichmann W, Valavanis A. T2-weighted three-dimensional fast spin-echo MR in inflammatory peripheral facial nerve palsy. AJNR Am J Neuroradiol. 1998;19:491–495. [PMC free article] [PubMed] [Google Scholar]
- 8.Kim MS, Yoon HJ, Kim HJ, Nam JS, Choi SH, Kim JM, et al. Bilateral peripheral facial palsy in a patient with Human Immunodeficiency Virus (HIV) infection. Yonsei Med J. 2006;47:745–747. doi: 10.3349/ymj.2006.47.5.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murakami S, Mizobuchi M, Nakashiro Y, Doi T, Hato N, Yanagihara N. Bell's palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med. 1996;124:27–30. doi: 10.7326/0003-4819-124-1_part_1-199601010-00005. [DOI] [PubMed] [Google Scholar]
- 10.Burgess RC, Michaels L, Bales JF, Jr, Smith RJ. Polymerase chain reaction amplification of herpes simplex viral DNA from the geniculate ganglion of a patient with Bell's palsy. Ann Otol Rhinol Laryngol. 1994;103:775–779. doi: 10.1177/000348949410301006. [DOI] [PubMed] [Google Scholar]
- 11.Sugita T, Murakami S, Yanagihara N, Fujiwara Y, Hirata Y, Kurata T. Facial nerve paralysis induced by herpes simplex virus in mice: an animal model of acute and transient facial paralysis. Ann Otol Rhinol Laryngol. 1995;104:574–581. doi: 10.1177/000348949510400713. [DOI] [PubMed] [Google Scholar]
- 12.Adour KK, Ruboyianes JM, Von Doereten PG, Byl FM, Trent CS, Quesenberry CP, Jr, et al. Bell's palsy treatment with acyclovir and prednisone compared with prednisone alone: a double-blind, randomized, controlled trial. Ann Otol Rhinol Laryngol. 1996;105:371–378. doi: 10.1177/000348949610500508. [DOI] [PubMed] [Google Scholar]
- 13.Furuta Y, Ohtani F, Chida E, Mesuda Y, Fukuda S, Inuyama Y. Herpes simplex virus type 1 reactivation and antiviral therapy in patients with acute peripheral facial palsy. Auris Nasus Larynx. 2001;28(Suppl):S13–S17. doi: 10.1016/s0385-8146(00)00105-x. [DOI] [PubMed] [Google Scholar]
- 14.Fisch U, Esslen E. Total intratemporal exposure of the facial nerve. Pathologic findings in Bell's palsy. Arch Otolaryngol. 1972;95:335–341. doi: 10.1001/archotol.1972.00770080529008. [DOI] [PubMed] [Google Scholar]
- 15.Yanagihara N, Honda N, Hato N, Murakami S. Edematous swelling of the facial nerve in Bell's palsy. Acta Otolaryngol. 2000;120:667–671. doi: 10.1080/000164800750000522. [DOI] [PubMed] [Google Scholar]
- 16.Honda N, Yanagihara N, Hato N, Kisak H, Murakami S, Gyo K. Swelling of the intratemporal facial nerve in Ramsay Hunt syndrome. Acta Otolaryngol. 2002;122:348–352. doi: 10.1080/000164802753648295. [DOI] [PubMed] [Google Scholar]
- 17.Tada Y, Aoyagi M, Tojima H, Inamura H, Saito O, Maeyama H, et al. Gd-DTPA enhanced MRI in Ramsay Hunt syndrome. Acta Otolaryngol Suppl. 1994;511:170–174. doi: 10.3109/00016489409128326. [DOI] [PubMed] [Google Scholar]
- 18.Gebarski SS, Telian SA, Niparko JK. Enhancement along the normal facial nerve in the facial canal: MR imaging and anatomic correlation. Radiology. 1992;183:391–394. doi: 10.1148/radiology.183.2.1561339. [DOI] [PubMed] [Google Scholar]
- 19.Saatci I, Sahintürk F, Sennaroğlu L, Boyvat F, Gürsel B, Besim A. MRI of the facial nerve in idiopathic facial palsy. Eur Radiol. 1996;6:631–636. doi: 10.1007/BF00187662. [DOI] [PubMed] [Google Scholar]
- 20.Kinoshita T, Ishii K, Okitsu T, Okudera T, Ogawa T. Facial nerve palsy: evaluation by contrast-enhanced MR imaging. Clin Radiol. 2001;56:926–932. doi: 10.1053/crad.2001.0730. [DOI] [PubMed] [Google Scholar]
- 21.Yanagida M, Ushiro K, Yamashita T, Kumazawa T, Katoh T. Enhanced MRI in patients with Ramsay-Hunt's syndrome. Acta Otolaryngol Suppl. 1993;500:58–61. doi: 10.3109/00016489309126181. [DOI] [PubMed] [Google Scholar]
- 22.Tien R, Dillon WP, Jackler RK. Contrast-enhanced MR imaging of the facial nerve in 11 patients with Bell's palsy. AJNR Am J Neuroradiol. 1990;11:735–741. [PMC free article] [PubMed] [Google Scholar]