Abstract
It generally is accepted that fractures of the tibia located in the proximal and distal thirds tend to angulate more than midshaft fractures when treated with intramedullary nails. We therefore compared the angular deformities and final shortening of 434 closed fractures located in the middle third of the tibia treated with a functional brace with those in fractures in the proximal and distal thirds treated in the same manner. Ninety-seven percent in the middle third healed with 8° or less angulation in the mediolateral plane, which was a higher percentage than we had experienced in distal and proximal third fractures treated with this method. Nonunions occurred in four (0.9%) fractures. We found correlations between initial shortening, final shortening, initial displacement, final displacement, and time to brace with initial angulation and final angulation in the mediolateral and anteroposterior planes. The overall mean final shortening of the fractures located in the middle third was 4.3 mm. These experiences suggest satisfactory results can be obtained in most instances using a functional brace for management of closed fractures of the middle third of the tibia.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Distal and proximal fractures of the tibia with an intact fibula tend to angulate into varus whether treated with intramedullary nails or functional braces [1, 2, 5, 7–9, 11–16, 20, 21, 23–25, 33, 34, 37–39, 41, 45, 46, 48–50, 52–55]. Proximal fractures of the tibia tend to angulate into anterior bowing when fixed with intramedullary nails [1, 3, 4, 12–14, 19, 22–25, 32, 38, 52, 53] and into varus if the fibula is intact and stabilized in a functional brace [15, 26, 28, 39, 41, 42, 44, 45, 48]. It has been suggested this may occur because of the poor leverage [49]. Shortening with functional bracing has been associated with the degree of soft tissue damage and initial shortening at the time of injury, but no correlation has been tested by level of fracture [26, 36, 39–48]. It generally is accepted that fractures of the tibia located in the proximal and distal thirds tend to angulate more than midshaft fractures when treated with intramedullary nails [4, 12–14, 19–21, 23, 24, 34, 38, 49, 53].
We therefore questioned whether midshaft closed fractures of the tibia, treated without surgery and early weightbearing in a functional brace would similarly experience a lower incidence of angulation in all planes and less shortening after healing than fractures treated with the same method but located in the proximal [28] or distal third [46] of the tibial diaphysis. We also asked if initial shortening was related to final shortening, or if initial angulation in each plane was related to final angulation in that plane, or if time to bracing correlated with final shortening or angulation. As we earlier found an increase in angulation of proximal and distal tibial fractures treated by this method if the fibula was not fractured [41, 44–46, 48], we thought it would be important to see if that also held true for middle-third tibial fractures. The purpose was to seek parameters that could be recognized early in the treatment that might influence the final anatomic outcome, and might serve to identify patients appropriate for nonoperative treatment and prevent angulation or shortening.
Materials and Methods
From a prospective study of 2384 closed diaphyseal fractures of the tibia treated with functional braces between June 1978 and June 1992, we previously reported on 973 patients with 992 fractures (108 in the proximal third [28], 450 in the distal third [46]) who were followed until completion of treatment, that is, documented healing or nonunion. The remaining 434 patients (434 fractures) constitute the material of this study [48]. The remaining 1372 patients with 1392 fractures (58%) were lost to followup or had inadequate radiographs. From the prospective series, we performed a retrospective review of the radiographs. Eighty patients (18%) were female and 354 (82%) were male. Their ages ranged from 14 to 86 years (average, 31.5 ± 12.7 years; median, 27 years; mode, 26 years). One hundred forty-three (32.9%) fractures were comminuted, 112 (25.8%) were oblique, 38 (8.7%) were spiral, 125 (28.8%) were transverse, and 16 (3.7%) were segmental. Three hundred twelve fractures (71.9%) had associated fibular fractures and 122 (28.1%) had intact fibulae. From the group of 312 tibial fractures with associated fibular fractures, 239 (76.6%) fibula fractures were located in the middle third, 51 (16.3%) in the proximal third, and 22 (7.1%) in the distal third. The minimum followup was 1.5 months (mean, 4.3 months; range, 1.5–14.3 months).
To compare consistency of the groups, we documented the mechanism of injury, which might influence final alignment of the fractures with this method of treatment. We considered fractures as low energy if they were the result of direct blows, falls to the ground, falls from a bicycle, or a kick in the leg. Fractures were considered high energy if they occurred during a motorcycle or motor vehicle accident, or involved a bicycle and an automobile, or a pedestrian being hit by a motor vehicle. Two hundred one (46.4%) were considered low energy fractures and 232 (53.6%) were high energy fractures (one had no recorded mechanism of injury). One hundred one (23.0%) occurred in motor vehicle accidents, 88 (20.2%) in pedestrian/vehicle accidents, 43 (9.9%) in motorcycle accidents, 121 (27.9%) in falls, 76 by a direct blow (17.6%), four from a kick (0.9%), and one through an unknown mechanism. The incidence of high-energy and low-energy injuries was similar between the groups according to fracture level, or between groups that ended with angulations greater than 8 or shortening greater than 12 mm. Therefore, we found no reason to use energy of injury as a criterion for exclusion or inclusion for this method of treatment.
We instituted functional brace treatment if the patient was not polytraumatized and did not have other major fractures, the fracture was closed, initial shortening was 12 mm or less, and the angular deformity, once corrected by manipulation, was 6° or less. The initial method of stabilization consisted of an above-knee cast that held the knee in 10° or less flexion and the ankle in a neutral position. Alignment of the fracture was performed with the patient under sedation or anesthesia. Only patients with transverse/displaced fractures received anesthesia. All other fractures (oblique, spiral, comminuted) were usually treated with the patient under conscious sedation consisting of intravenous Demerol (Sanofi-Aventis U.S., LLC, Bridgewater, NJ). No forceful attempt was made to regain length in these fractures because we were aware of the fact that whatever length was gained by traction is lost when patients resume function [26, 36, 39, 42–45, 47, 48].
If angular deformity exceeding 5° was recognized after application of the initial above-knee cast, the angulation was corrected at that time. If angulation was recognized later when the functional brace was applied, we attempted to improve it by gentle pressure at the apex of the fracture and appropriate corresponding counterpressure either proximally or distally to the fracture site. We have no data regarding the number of casts or modification of casts made to improve alignment of the fractures. The fractures were not manipulated forcefully, but the injured limb was allowed to hang over the side of the table and be subjected to gravity forces while gentle molding was used to provide alignment. Patients were admitted to the hospital overnight whenever the treating resident believed in-hospital observation of the muscle compartments of the leg was desirable. Weightbearing as tolerated was encouraged from the outset.
Application of the brace, accomplished when the acute symptoms had subsided, occurred an average of 26.3 ± 20.2 days after the injury (median, 20 days; mode, 14 days). Details of the steps to treat patients with functional braces have been described [39, 42, 44, 45, 47, 48]. The brace was prefabricated, consisting of two shells of polypropylene fastened together with Velcro straps (Fig. 1). We encouraged weightbearing as tolerated with external support. Frequent tightening of the straps was encouraged to maintain the desirable snugness of the brace as swelling subsided. Neither the brace nor the accompanying shoe was to be removed. At the 1-week followup, the brace was removed temporarily and the leg was inspected. If discomfort and swelling were minimal, the patient was instructed regarding the appropriate way of donning and doffing the brace for hygienic purposes. The next appointment usually was 4 weeks later. Subsequent followups were at 4-week intervals.
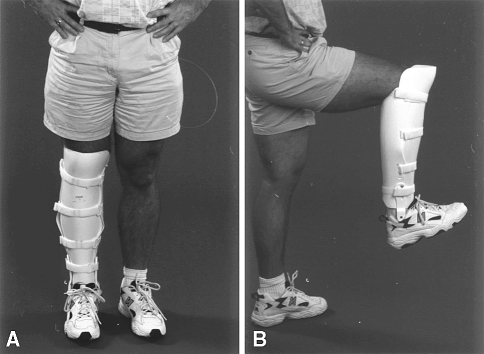
Fig. 1A–B.
(A) A photograph of a functional brace shows full flexion of the knee that the brace permits. (B) This lateral-view photograph shows the functional brace permits unencumbered motion of the knee and ankle.
Under the supervision of attending staff, residents recorded data on specially designed forms for initial angulation, displacement, presence of and level of fibular fractures, and shortening as observed on radiographs obtained before treatment. From the clinical charts, we obtained the age, gender, date of injury, date of bracing, date of healing, and complications. We considered a fracture united when radiographs showed mature callus bridging the major fragments on at least one radiographic projection and the patient was walking without pain or external support. Time to healing did not differ from analyses of the distal and proximal fractures of the tibia [28, 50].
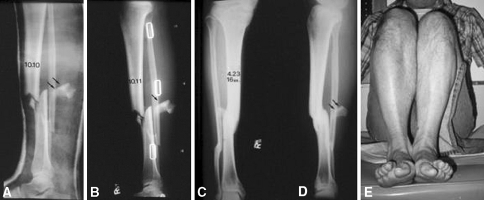
The radiographs of all 434 patients were analyzed for initial shortening and angulation in the anteroposterior (AP) and mediolateral (ML) planes, final shortening and angulation in the AP and ML planes, and initial and final displacement. Shortening was measured from radiographs by identifying specific points of the fracture on the proximal and distal fragments where they would fit together (Fig. 2). No correction was made for magnification, so the measured shortening was greater than the actual shortening. The radiographic data initially were recorded by residents in the outpatient clinic under the supervision of the senior author. Subsequently, numerous senior residents reviewed the films again before submission of various manuscripts.
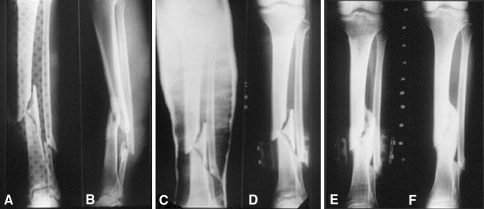
Fig. 2A–F.
(A) Anteriorposterior and (B) lateral radiographs show comminuted fractures of the tibia and fibula with severe recurvatum deformity but acceptable shortening. Radiographs were obtained after application of the original above-knee cast (C) and functional brace (D), respectively, with no attempts having been made to regain length. (E) Healing at the time of brace removal shows complete radiographic healing. (F) At final follow up solid radiographic healing is evident.
We correlated initial angulation in the AP and ML planes, initial shortening with final angulation in both planes, and final shortening using ANOVA multivariate analysis with Bonferroni correction for multiple comparisons. We made comparisons of all other continuous variables with the Student’s t test using the Bonferroni post hoc correction for multiple comparisons. Using a chi square analysis we compared the number of patients who had a final angulation greater than 8° in the ML plane between the patients with fractures in the current study and patients with proximal fractures [28] and distal fractures [46] of the tibia treated with the same protocol. Systat (Systat, Inc, Point Richmond, CA) was used for all analyses.
Results
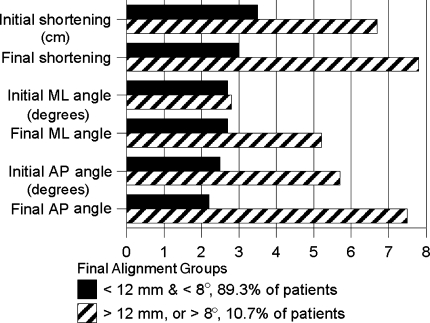
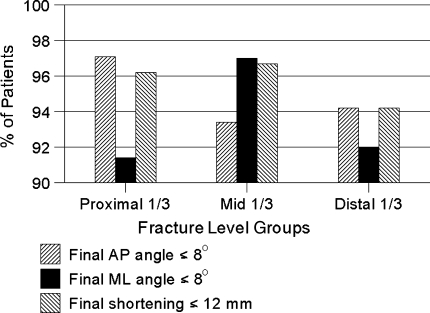
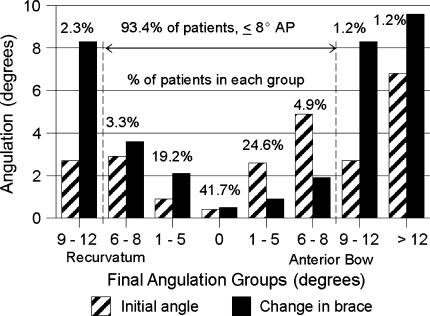
In the ML plane, 421 (97.0%) fractures healed with 8° or less angulation, three (0.7%) fractures had varus angulation greater than 12°, and 10 (2.3%) fractures had 9° to 12° varus (Figs. 3, 4). This left 13 of 434 fractures with angulation greater than 8° which was less (p < 0.003) than the incidence in the proximal fractures (nine of 108 [28]) and the distal fractures (36 of 450 [46]) (Fig. 5). In the AP plane, 399 (93.4%) fractures healed with 8° or less angulation, 10 (2.3%) fractures had greater than 8° anterior bowing, and 18 (4.3%) fractures had greater than 8° recurvatum (Figs. 3, 6), all percentages similar to those with proximal or distal fractures. The percentages of fractures with final shortening greater than 12 mm were also similar in all three groups.
Fig. 3.
High energy injuries accounted for 61.5% of all the fractures with greater than 8° varus or valgus, whereas 53.3% of the 414 patients with 8° or less varus or valgus had high energy injuries. The initial angulation in the 13 fractures that healed with greater than 8° varus or valgus was 3.2° ± 3.2° compared with fractures that healed in the 8° or less group, which was 2.7° ± 2.9°. There was no major difference in the initial angulation in these groups, but there was a difference (p < 0.0005) in the change in angulation during treatment: 2.7° ± 2.8° versus 11.8° ± 7.5°. AP = anteroposterior; ML = mediolateral.
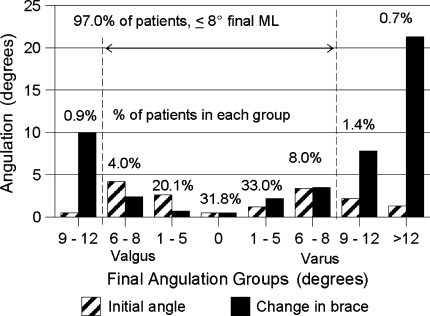
Fig. 4.
Coronal angular deformity at the initial visit and changes during functional treatment are displayed by the final angulation groups. ML = mediolateral.
Fig. 5.
The odds for obtaining final alignment with angulation in all planes of 8° or less and shortening 12 mm or less was better than 90% for all fracture levels, but the odds for maintaining 8° or less in the ML plane was considerably better for the mid-shaft fractures. AP = anteroposterior; ML = mediolateral.
Fig. 6.
Sagittal angular deformity at the initial visit and changes during functional treatment are displayed by the final angulation groups. AP = anteroposterior.
Final angulation in the ML plane correlated with initial angulation in that plane and final angulation in the AP plane correlated with initial angulation in that plane. Final shortening also correlated with initial shortening (Fig. 3). Initial and final angulation in both planes correlated (all p values at least < 0.001) with time to brace application. Therefore, it was not the severity of the injury, but the initial position of the bone fragments that influenced the final length and alignment of the limb (Fig. 7). The percentage of fractures with greater than 8° AP angulation was similar in isolated tibial fractures and those with associated fibula fractures.
Fig. 7A–E.
(A) The radiograph shows high energy-produced comminuted fractures of the tibia and fibula. A free fragment is evident posteriorly. The shortening was accepted because the patient was elderly and had diabetes. (B) This radiograph shows the fracture as seen through the brace. (C) The anterioposterior radiograph shows the healed fractures without additional shortening or angulation, also evident (D) in the lateral view. (E) The photograph of the patient’s leg shows mild shortening of the fractured leg, which was compensated with a shoe lift.
Discussion
We sought to find measurable parameters to help guide surgeons in choosing patients for nonoperative treatment of tibial diaphyseal fractures.
There are numerous limitations to this study. Although the data were collected prospectively, the patients were selected for this treatment; only patients with closed fractures with initial shortening less than 15 mm were included. The data were collected by numerous residents. At the time of this study, intramedullary nailing was the preferred treatment method for axially unstable fractures with initial shortening greater than 15 mm. We have no information regarding the number of fractures treated surgically during the same period at the same institution. The data we report cannot be applied to fractures with initial shortening greater than 15 mm or to open fractures of the tibia. Many patients were lost to followup. The minimum followup was 1.5 months. The considerable number of patients from the original group with closed tibial fractures treated with functional braces who were lost to followup was thought to be the result of their low socioeconomic level. For various reasons, they frequently chose to remove the stabilizing braces once they were pain-free and able to walk without support. This pattern precluded an objective evaluation regarding the outcome of many fractures. We did not evaluate rotary deformities in this study. Such deformities, we believe, were rare with functional bracing, and their presence is the result of failure to correct it at the time of initial reduction of the fracture [48].
Treatment modalities for closed diaphyseal tibial fractures seem to be limited to intramedullary nailing, plating, casting, or bracing. We recognize the place for functional bracing in open fractures is limited; therefore, our subsequent experience with the method was exclusively with closed diaphyseal fractures [48]. However, in previous studies, it was reported that initial shortening of closed tibial fractures did not increase beyond that observed immediately after the initial insult [26, 36, 39, 42, 47]. Therefore, if bracing is limited to closed fractures that have acceptable initial shortening, final shortening is not a problem.
When a trauma surgeon chooses a method to care for a patient with a closed tibial fracture, numerous variables contribute to the decision. Some of those variables are addressed in this study. The measured differences in the selected groups in this study were not large mainly because the incidence of clinically important malalignment is small. However, because of the sample sizes in this series (almost 1000 fractures), we found statistical differences. Thus, the surgeon must weigh the clinical importance of these anatomic differences with other important clinical variables. Healing time and cost of treatment are important variables that we did not address in this study, but others have [10, 48].
Plating, intramedullary nailing, and external fixation are other methods of treatment. However, nailing currently seems the preferred treatment. Therefore, we compared our results only with published results for nailing. Intramedullary nailing does not consistently result in perfect alignment. Freedman and Johnson, using criteria in which a fracture was considered malaligned if 5° or greater angulation in any plane was measured, reported malalignment in 7% of fractures located in the middle third of the tibia, 58% in fractures located in the proximal third, and 8% in the distal third [12]. The angular deformities measured in patients in our study were acceptable cosmetically in most instances, because 405 (90.0%) patients had 8° or less angular deformity. These figures are comparable with those reported for intramedullary nailing [1–3, 5, 8, 12, 14, 20, 23–25, 34, 38, 50, 53, 55]. Others also have reported a considerable incidence of angulations greater than 5° [9, 11–13, 20, 23–25, 34, 38, 53–55] and some greater than 10° [55] when treating distal fractures with intramedullary nails. Proximal fractures also reportedly have a considerable incidence of angulations [12–14, 20, 34, 54, 55]. Most of these problems seem to have been alleviated by the use of blocking screws [4, 19, 21, 23, 38, 49]. The short fragments also tend to angulate more in the ML plane with functional bracing and early weightbearing (Fig. 8) with an incidence of angulations greater than 8° less than the incidence reported for fractures treated with intramedullary nailing greater than 5° that did not use blocking screws. This is not a direct comparison but is similar.
Fig. 8A–G.
(A) The anteriorposterior and (B) lateral radiographs show oblique, slightly comminuted fractures of the tibia and fibula. There is initial valgus deformity but minimal shortening. (C) Radiographs were obtained after initial stabilization with the patient wearing an above-knee cast and then (D) a brace, respectively. The initial shortening was accepted. (E) The anteriorposterior and (F) lateral radiographs show the healed fractures with a mild varus angular deformity. (G) A photograph of the patient’s legs show some residual atrophy of the musculature. The cosmetic appearance of the fractured extremity was satisfactory.
Chronic knee pain after intramedullary nailing remains a troublesome complication regardless of the surgical approach used, ranging from 5% to 86%. Removal of the nail failed to eliminate the pain, which according to some persisted in as many as 69% at an average of 1.5 years [6, 17, 18, 20, 35, 51, 53].
As angulatory deformities are likely to occur with intramedullary nailing and functional bracing, one must understand their clinical importance. Puno et al. reported some instances in which they linked arthritic changes to angular deformities [37]. However, there is strong suggestive evidence that angular deformities resulting from diaphyseal tibial fractures are rarely responsible for late degenerative arthritis in the adjacent joints. Merchant and Dietz, based on a review of 37 patients with tibial fractures who had a followup of nearly 29 years, concluded 10° to 15° angular deformities were well tolerated and the deformity was not related to functional deficit [31]. They stated the clinical and radiographic results were unaffected by the amount of anterior or posterior and varus or valgus angulation and the level of the fracture [31]. Milner et al. reported their findings from 164 patients with followups ranging between 30 and 43 years [33]. Seventeen (15%) patients had overall alignment of the lower limb, defined as a hip-knee-ankle angle outside the normal range of 6.25° varus to 4.75° valgus. “Most of the subjects” in whom osteoarthritis was observed had normal overall alignment of the normal limb [33]. Other factors such as severe cartilage impaction at the time of the injury may be more important in causing osteoarthritis [40]. Kristensen et al. observed no osteoarthritis of the ankle 20 years after malaligned tibial fractures and reported ankle stiffness and associated pain correlated with the length of immobilization [22]. It can be extrapolated that early mobilization of all joints made possible by the functional brace minimizes temporary stiffness. We and others have studied the effect of angular deformities on adjacent joints and have found minor deformities do not alter pressure distribution on the articular cartilage in adjacent joints in a major way [27, 29, 30].
Bone and Johnson [2] reported shortening after intramedullary nailing was 10 mm in 5% patients, and Hooper et al. [15] reported shortening of 3.4% in 21 patients. In our study, the mean shortening was 3.5 mm.
The absence of complications that may accompany surgical treatment of tibial fractures further provides serious consideration to the value of closed functional bracing as a therapeutic modality in a high percentage of fractures. Although functional bracing appears to render good results in the care of closed axially unstable fractures that initially have 12 mm or less shortening and a corrected angular deformity of 8° or less, and in reduced, made-stable closed transverse fractures, at this time the role of bracing should not be extended to fractures that initially have greater than 12 mm shortening and angular deformity greater than 8°.
In our protocol, the amount of weightbearing is dictated by the degree of symptoms, which in most instances rapidly decreases in intensity, allowing full weightbearing within the first few weeks after injury. This factor contradicts the widely accepted perception that nailing, in all instances, permits earlier full weightbearing ambulation [39, 41, 42, 46, 48].
Acknowledgments
We thank the residents in the Department of Orthopaedics at the University of Southern California for treatment and subsequent followup of the patients and recording of computerized data, particularly Phillip Sobol MD, Larry Gersten MD, James Shankwiler MD, and especially Frances Sharpe MD and Edward Ebramzadeh PhD, for their contributions in compilation of the statistical data.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Alho A, Ekeland A, Stromsoe K, Folleras G, Thoresen BO. Locked intramedullary nailing for displaced tibial shaft fractures. (Erratum in J Bone Joint Surg Br. 1991;73:181.) J Bone Joint Surg Br. 1990;72:805–809. [DOI] [PubMed]
- 2.Bone LB, Johnson KD. Treatment of tibial fractures by reaming and intramedullary nailing. J Bone Joint Surg Am. 1986;68:877–887. [PubMed]
- 3.Bonnevialle P, Bellumore Y, Foucras L, Hézard L, Mansat M. Tibial fracture with intact fibula treated with reamed nailing.] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2000;86:29–37. [PubMed]
- 4.Buehler KC, Green J, Woll TS, Duwelius PJ. A technique for intramedullary nailing of proximal third tibia fractures. J Orthop Trauma. 1997;11:218–223. [DOI] [PubMed]
- 5.Court-Brown CM, Christie J, McQueen MM. Closed intramedullary tibial nailing: its use in closed and type I open fractures. J Bone Joint Surg Br. 1990;72:605–611. [DOI] [PubMed]
- 6.Court-Brown CM, Gustilo T, Shaw AD. Knee pain after intramedullary nailing: its incidence, etiology, and outcome. J Orthop Trauma. 1997;11:103–105. [DOI] [PubMed]
- 7.Court-Brown CM, Will E, Christie J, McQueen MM. Reamed or unreamed nailing for closed tibial fractures: a prospective study in Tscherne C1 fractures. J Bone Joint Surg Br. 1996;78:580–583. [PubMed]
- 8.De Smet K, Mostert AK, De Witte J, De Brauwer V, Verdonk R. Closed intramedullary tibial nailing using the Marchetti-Vicenzi nail. Injury. 2000;31:597–603. [DOI] [PubMed]
- 9.Dogra AS, Ruiz AL, Thompson NS, Nolan PC. Dia-methaphyseal distal tibial fractures: treatment with a shortened intramedullary nail: a review of 15 cases. Injury. 2000;31:799–804. [DOI] [PubMed]
- 10.Downing ND, Griffin DR, Davis TR. A comparison of the relative costs of cast treatment and intramedullary nailing for tibial diaphyseal fractures in the UK. Injury. 1997;28:373–375. [DOI] [PubMed]
- 11.Finkemeier CG, Schmidt AH, Kyle RF, Templeman DC, Varecka TF. A prospective, randomized study of intramedullary nails inserted with and without reaming for the treatment of open and closed fractures of the tibial shaft. J Orthop Trauma. 2000;14:187–193. [DOI] [PubMed]
- 12.Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res. 1995;315:25–33. [PubMed]
- 13.Gregory P, Sanders R. The treatment of closed, unstable tibial shaft fractures with unreamed interlocking nails. Clin Orthop Relat Res. 1995;315:48–55. [PubMed]
- 14.Habernek H, Kwansy O, Schmid L, Ortner F. Complications of interlocking nailing for lower leg fractures: a 3-year follow up of 102 cases. J Trauma. 1992;33:863–869. [DOI] [PubMed]
- 15.Hooper GJ, Keddell RG, Penny ID. Conservative management or closed nailing for tibial shaft fractures: a randomised prospective trial. J Bone Joint Surg Br. 1991;73:83–85. [DOI] [PubMed]
- 16.Hutson JJ, Zych GA, Cole JD, Johnson KD, Ostermann P, Milne EL, Latta L. Mechanical failures of intramedullary tibia nails applied without reaming. Clin Orthop Relat Res. 1995;315:129–137. [PubMed]
- 17.Katsoulis E, Court-Brown C, Giannoudis PV. Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br. 2006;88:576–580. [DOI] [PubMed]
- 18.Keating JF, Orfaly R, O’Brien PJ. Knee pain after tibial nailing. J Orthop Trauma. 1997;11:10–13. [DOI] [PubMed]
- 19.Kim JJ, Noh KM, Cho WS, Kim YT, Kim KY. A technique for intramedullary nailing of proximal third tibia fractures. J Korean Fracture Soc. 1998; 11:456–463.
- 20.Koval KJ, Clapper MF, Brumback RJ, Ellison PS Jr, Poka A, Bathon GH, Burgess AR. Complications of reamed intramedullary nailing of the tibia. J Orthop Trauma. 1991;5:184–189. [DOI] [PubMed]
- 21.Krettek C, Miclau T, Schandelmaier P, Stephan C, Mohlmann U, Tscherne H. The mechanical effect of blocking screw (“Poller screws”) in stabilizing tibia fractures with short proximal or distal fragments after insertion of small-diameter intramedullary nails. J Orthop Trauma. 1999;13:550–553. [DOI] [PubMed]
- 22.Kristensen KD, Kiaer T, Blicher J. No arthrosis of the ankle 20 years after malaligned tibial-shaft fracture. Acta Orthop Scand. 1989;60:208–209. [DOI] [PubMed]
- 23.Laflamme GY, Heimlich D, Stephen D, Kreder HJ, Whyne CM: Proximal tibial fracture stability with intramedullary nail fixation using oblique interlocking screws. J Orthop Trauma. 2003;17:496–502. [DOI] [PubMed]
- 24.Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures: should they be nailed? Clin Orthop Relat Res. 1995;315:64–74. [PubMed]
- 25.Larsen LB, Madsen JE, Hoiness PR, Ovre S. Should insertion of intramedullary nails for tibial fractures be with or without reaming? A prospective, randomized study with 3.8 years’ follow-up. J Orthop Trauma. 2004;18:144–149. [DOI] [PubMed]
- 26.Latta LL, Sarmiento A, Zych G. Principles of nonoperative fracture management. In: Browner B, Jupiter J, Levine J, Trafton PWB, eds. Skeletal Trauma. 2nd Ed. Philadelphia, PA: WB Saunders; 2003:159–178.
- 27.Lovasz G, Llinas A, Benya P, Bodey B, McKellop HA, Luck JV Jr, Sarmiento A. Effects of valgus tibial angulation on cartilage degeneration in the rabbit knee. J Orthop Res. 1995;13:846–853. [DOI] [PubMed]
- 28.Martinez A, Sarmiento A, Latta LL. Closed fractures of the proximal tibia treated with a functional brace. Clin Orthop Relat Res. 2003;417:293–302. [DOI] [PubMed]
- 29.McKellop HA, Llinas A, Sarmiento A. Effects of tibial malalignment on the knee and ankle. Orthop Clin North Am. 1994;25:415–423. [PubMed]
- 30.McKellop HA, Sigholm G, Redfern F, Doyle B, Sarmiento A, Luck JV Sr. The effect of simulated fracture-angulations of the tibia on cartilage pressures in the knee joint. J Bone Joint Surg Am. 1991;73:1382–1391. [PubMed]
- 31.Merchant TC, Dietz FR. Long-term follow-up after fractures of the tibial and fibular shafts. J Bone Joint Surg Am. 1989;71:599–606. [PubMed]
- 32.Mertens P, Broos P, Reynders P, Deswart R. The unreamed locked intramedullary tibial nail: a follow-up study in 51 patients. Acta Orthop Belg. 1998;64:277–283. [PubMed]
- 33.Milner SA, Davis TR, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002;84:971–980. [DOI] [PubMed]
- 34.Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am. 2005;87:1213–1221. [DOI] [PubMed]
- 35.Orfaly R, Keating JE, O’Brien PJ. Knee pain after tibial nailing: does the entry point matter? J Bone Joint Surg Br. 1995;77:976–977. [PubMed]
- 36.Park SH, O’Connor K, McKellop H, Sarmiento A. The influence of active shear or compressive motion on fracture-healing. J Bone Joint Surg Am. 1998;80:868–878. [DOI] [PubMed]
- 37.Puno RM, Vaughan JJ, Stetten ML, Johnson JR. Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma. 1991;5:247–254. [DOI] [PubMed]
- 38.Ricci WM, O’Boyle M, Borrelli J, Bellabarba C, Sanders R. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma. 2001;15:264–270. [DOI] [PubMed]
- 39.Sarmiento A. On the behavior of closed tibial fractures: clinical/radiological correlations. J Orthop Trauma. 2000;14:199–205. [DOI] [PubMed]
- 40.Sarmiento A. Mechanism of injury may affect outcome after tibial shaft fracture. Comment on: J Bone Joint Surg Am. 2002;84:971–980. J Bone Joint Surg Am. 2003;85:571; author reply 571–572. [DOI] [PubMed]
- 41.Sarmiento A, Kinman PB, Latta LL, Eng P. Fractures of the proximal tibia and tibial condyles: a clinical and laboratory comparative study. Clin Orthop Relat Res. 1979;145:136–145. [PubMed]
- 42.Sarmiento A, Latta L. The evolution of functional bracing of fractures. J Bone Joint Surg Br. 2006;88:141–148. [DOI] [PubMed]
- 43.Sarmiento A, Latta L, Zilioli A, Sinclair W. The role of soft tissues in stabilization of tibial fractures. Clin Orthop Relat Res. 1974;105:116–129. [PubMed]
- 44.Sarmiento A, Latta LL. Fractures of the tibia, chapter 3. In: Closed Functional Treatment of Fractures. Berlin, Germany: Springer-Verlag; 1981:61–266.
- 45.Sarmiento A, Latta LL. Tibial fractures, chapter 2. In: Functional Fracture Bracing, Tibia, Humerus and Ulna. Heidelberg, Germany: Springer-Verlag; 1995:21–203.
- 46.Sarmiento A, Latta LL. 450 closed fractures of the distal third of the tibia treated with a functional brace. Clin Orthop Relat Res. 2004;428:261–271. [DOI] [PubMed]
- 47.Sarmiento A, McKellop HA, Llinas A, Park SH, Lu B, Stetson W, Rao R. Effect of loading and fracture motions on diaphyseal tibial fractures. J Orthop Res. 1996;14:80–84. [DOI] [PubMed]
- 48.Sarmiento A, Sharpe FE, Ebramzadeh E, Normand P, Shankwiler J. Factors influencing the outcome of closed tibial fractures treated with functional bracing. Clin Orthop Relat Res. 1995;315:8–24. [PubMed]
- 49.Stedtfeld HW, Mittlmeier T, Landgraf P, Ewert A. The logic and clinical applications of blocking screws. J Bone Joint Surg Am. 2004; 86(suppl 2):17–25. [DOI] [PubMed]
- 50.Toivanen JA, Honkonen SE, Koivisto AM, Jarvinen MJ. Treatment of low-energy tibial shaft fractures: plaster cast compared with intramedullary nailing. Int Orthop. 2001;25:110–113. [DOI] [PMC free article] [PubMed]
- 51.Toivanen JA, Vaisto O, Kannus P, Latvala K, Honkonen SE, Jarvinen MJ. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft: a prospective, randomized study comparing two different nail-insertion techniques. J Bone Joint Surg Am. 2002;84:580–585. [DOI] [PubMed]
- 52.Tornetta P 3rd, Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop Relat Res. 1996;328:185–189. [DOI] [PubMed]
- 53.Williams J, Gibbons M, Trundle H, Murray D, Worlock P. Complications of nailing in closed tibial fractures. J Orthop Trauma. 1995;9:476–481. [DOI] [PubMed]
- 54.Yang SW, Tzeng HM, Chou YJ, Teng HP, Liu HH, Wong CY. Treatment of distal tibial metaphyseal fractures: plating versus shortened intramedullary nailing. Injury. 2006;37:531–535. [DOI] [PubMed]
- 55.Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M; Evidence-Based Orthopaedic Trauma Working Group. Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma. 2006;20:76–79. [DOI] [PubMed]