Abstract
Circular fixators have been used successfully to correct multiplanar deformities but are often cumbersome and may be difficult to apply. We determined whether a monolateral fixator, which allows for correction of angular deformity and displacement in three planes, can correct lower extremity deformities to within normal radiographic means (anatomic lateral distal femoral angle, anatomic medial proximal tibial angle, and tibial femoral angle). We retrospectively reviewed the clinical records and radiographs of 22 consecutive patients (25 limbs) who underwent deformity correction using a new multiaxial monolateral external fixator. The patients were 4 to 16 years of age. We had a minimum 1.2-year followup (mean, 2.14 years; range, 1.2–3.1 years). Those with primary femoral and tibial deformities had improvements in the mean deviation from normal of the anatomic lateral distal femoral angle, anatomic medial proximal tibial angle and tibial femoral angle. Patients with Blount’s disease had improvements in the mean anatomic medial proximal tibial angle from 59.9º to 87.8º. Five patients had complications (two pin site infections, one premature consolidation, one knee flexion contracture, one recurrence of varus). Six patients developed secondary deformities, all of which were corrected using the primary or secondary hinge. We conclude this fixator can produce satisfactory results with relatively few complications.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
External fixation is a powerful tool for treating extremity deformities. It allows for complex deformity correction with minimal soft tissue disruption and can be performed gradually, minimizing the risk of neurovascular injury and allowing for exact deformity correction. Various types of external fixators have been used for deformity correction and lengthening [1–5, 7, 9, 10]. In general, there are two types of fixators: ring-type fixators, which allow for lengthening and deformity correction, and monolateral fixators, which are excellent for lengthening and easier to apply but have limited deformity correction capabilities.
A new external fixator system for deformity correction and lengthening is applied as a monolateral external fixator but allows for correction of displacement and angulation in all three planes. It consists of a core block that has primary and secondary hinges and accompanying translation blocks oriented orthogonally to each other that allow for angulation and translation in the sagittal and coronal planes. Rotation arcs and compression/distraction components are added to correct rotation and allow for lengthening. The theoretical advantage of this device is it can be applied as simply as a monolateral fixator but allows for correction and adjustment of displacement and angulation in all three planes, including correction of residual or secondary deformities that occur during lengthening.
Other devices have been used to provide correction in more than one plane such as the Heidelberg fixator, which is a linear device that is placed in an anatomically safe zone so correction of some deformities can be difficult such as placement on the humerus and forearm or near the metaphyseal deformities. Because the multiaxial correction (MAC) is a component system, the hinge can usually be placed directly on the deformity (center of rotational angulation [CORA]). Placement of bone screws into safe zones, although not always in the plane of the CORA or perpendicular to the CORA, can be safely reached with arcs, even if the MAC hinges are placed near the joints.
The limitations of the MAC device include bones in which the available length for screws is less than 9 cm for three screws at each fragment or 6 cm for two screws at each fragment. It is not designed for small bones such as the metacarpals or metatarsals. Rotation correction is limited to 90°, the angulation with the primary hinge is 80°, and that of the secondary hinge is 35° to 45°; translation for the adult MAC is 3 cm in two planes and for the extra small MAC 2 cm in two planes. The extra small MAC is recommended for a maximum of 80 pounds weightbearing in legs but can be used in the adult upper extremity. Ring fixators would be better suited than the MAC in long bones in which two or more deformities must be treated individually but the deformities are closer than 6 cm.
We determined whether the MAC device could correct lower extremity deformities in three groups of patients (lengthening with or without deformity correction, Blount’s disease, and tibial deformities other than Blount’s disease) to within normal means as measured by the anatomic lateral distal femoral angle (aLDFA), anatomic medial proximal tibial angle (aMPTA), and degree of deformity as measured radiographically.
Materials and Methods
We retrospectively reviewed the medical records and radiographs of all 22 patients (25 limbs) who underwent deformity correction using the `Multi-Axial Correcting (MAC) Monolateral External Fixation System (EBI/Biomet Trauma, Parsippany, NJ) from 2002 to 2005. There were 11 boys and 11 girls with an average age of 11.6 years (range, 4.5–16.3 years) who underwent correction of angular deformities. Preoperative diagnosis included Blount’s disease in 11 patients, congenital femoral deficiency in five, and one patient each with tibial hemimelia, fibular hemimelia, rickets, trauma, malunion, and knee flexion contracture secondary to arthrogryposis. We had prior Institutional Review Board approval.
We used gradual correction in 23 limbs and acute correction in the operating room in two. For study purposes, patients were divided into three groups. Group I consisted of six patients (six limbs) in whom the MAC was placed on the femur for deformity correction and/or lengthening; the mean age was 13 years with two girls and four boys and a mean followup of 2 years. Four were diagnosed with congenital femoral deficiency and one each with trauma and malunion. Group II consisted of 11 patients (13 limbs) who underwent MAC placement to the tibia for Blount’s disease. The mean age was 10 years; there were six girls and five boys with a mean followup of 2 years. Group III consisted of five patients (six limbs) in which the MAC was applied to the tibia for angular correction or lengthening for a disorder other than Blount’s disease. One each was diagnosed with congenital femoral deficiency, fibular hemimelia, tibial hemimelia, arthrogryposis, and rickets. In this group, the surgical indications included (1) angular deformity of the tibia and/or femur; (2) leg length discrepancy more than 4 cm with or without associated angular deformity; and (3) knee flexion contracture. The mean angular deformity was 20º. The mean age was 11 years; there were three girls and two boys with a mean followup of 2.3 years. For all patient groups, the minimum followup was 1.2 years (mean, 2.14 years; range 1.2–3.1 years).
Patients and their families were educated regarding the surgical technique, hospital stay, pain management, postoperative care of the fixator, fixator adjustment, and rehabilitation protocol.
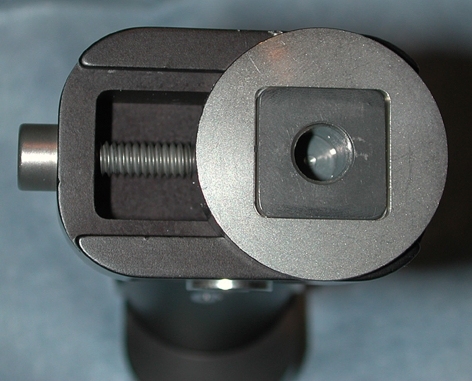
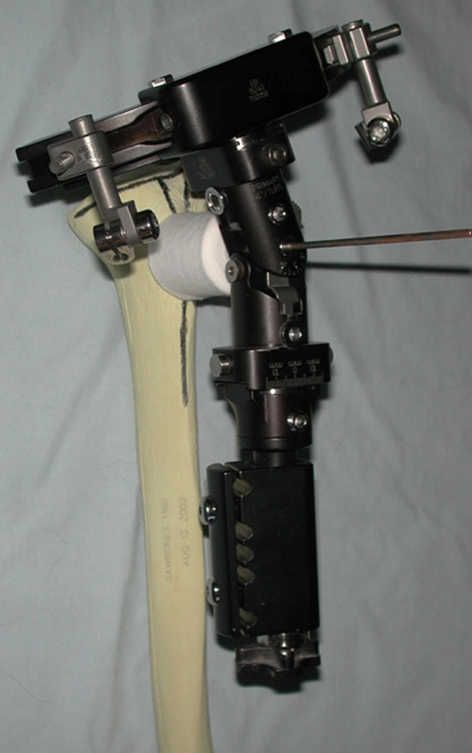
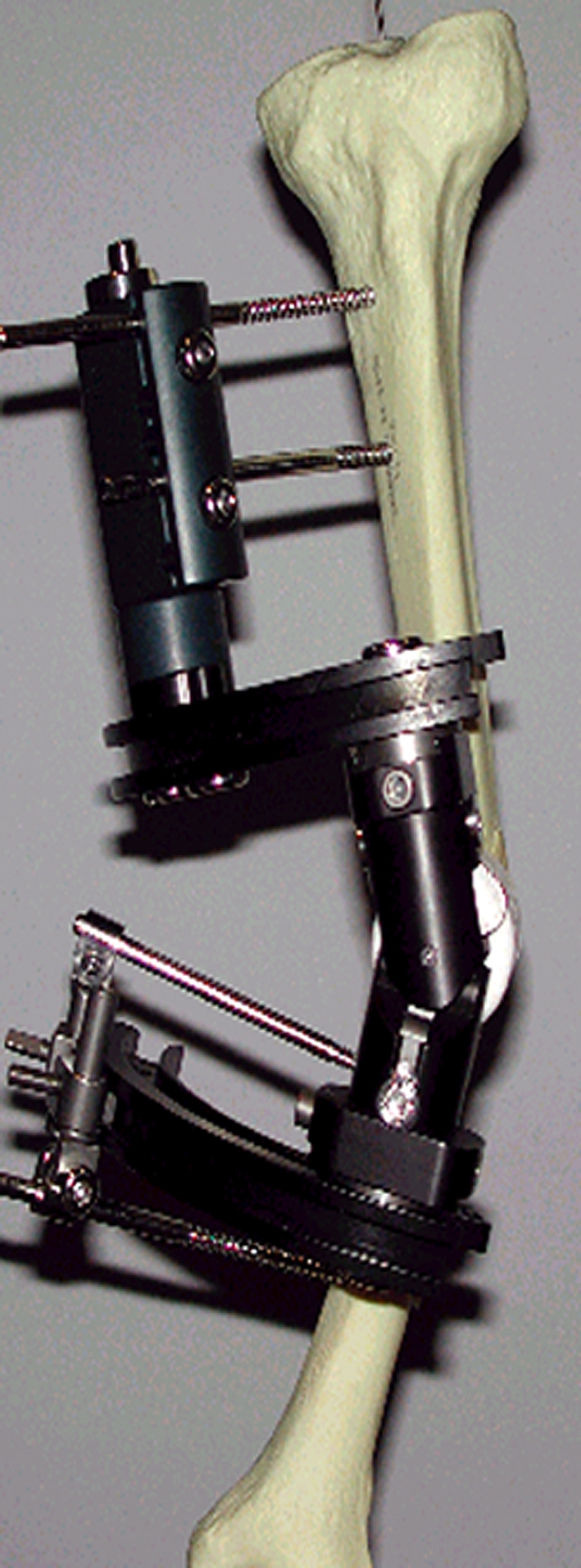
The MAC system is a Food and Drug Administration-approved monolateral fixator that allows for correction of angular deformity and displacement, including rotation and lengthening, in all three planes. The MAC system consists of a central component with a primary and secondary hinge capable of 80° and 35° to 55° of angulation, respectively, in two planes (Fig. 1). There is a translation screw at either end mounted at 90° to each other, and each is capable of 3 cm of translation (Fig. 2). Each end of the MAC device permits the attachment of a variety of components, including compression/distraction bone screw blocks, rails, arcs, rings, or rotation arcs, to allow positioning of the device where needed and safe placement of fixation screws. This component system permits application virtually anywhere along either the upper or lower extremity. The MAC device can be mounted in a CORA centric or a CORA perpendicular fashion. The CORA centric method is similar in planning and application to routine Ilizarov planning. The primary hinge is placed over the center of rotational angulation, and the frame is built around this to allow for safe pin placement (Figs. 3, 4).
Fig. 1.
The multiaxial correction system consists of a central component with a primary and secondary hinge capable of 80° and 35° to 55° of angulation, respectively, in two planes.
Fig. 2.
There is a translation screw at either end mounted 90° to one another and each is capable of 3 cm of translation.
Fig. 3.

In the center of rotational angulation centric method, the first step is to place the primary hinge over the center of rotational angulation.
Fig. 4.
The second step of the center of rotational angulation centric method is to build the frame around this to allow for safe pin placement.
The CORA perpendicular method is similar in planning and application to a hinged monolateral fixator with the primary hinge perpendicular to the CORA (along the bisector of the CORA) (Fig. 5) with the hinge on the bisector of the primary hinge. Application with the CORA perpendicular method is often easier, especially for femoral deformities, but must incorporate the lengthening or shortening that accompanies the angular correction. We typically used this method if lengthening was desired. Both methods allow for simultaneous correction of unrecognized or secondary deformities, including displacement and out-of-plane angular deformities, which may occur during surgery or while lengthening. Correction of deformity was attained through rotation of an L-shaped Allen wrench in the appropriate location. This can be performed acutely in the operating room, if small corrections are needed, or, more commonly, it was performed gradually at home by the patient or their family members. The rate of correction depends on the amount of lengthening for the structure at risk and can be determined by the rule of triangles or the angulation rate guide.
Fig. 5.
The center of rotational angulation (CORA) perpendicular method places the primary hinge perpendicular to the CORA with the hinge on the bisector of the primary hinge.
The MAC device can be simply applied (Fig. 6). Anteroposterior and lateral radiographs demonstrate 22° of metaphyseal deformity. The CORA is identified at approximately 1.5 cm distal to the physis. Tibial torsion (internal rotation) of 30° is identified. An appropriate-sized guide pin is placed in the axis of the CORA with care to align the wire in the frontal and sagittal planes with the long axis of the leg. A two-fingerbreadth spacer of padding is placed on the skin at the guide pin. The guide hole through the primary hinge of the MAC device is placed over the guide pin and aligned so the angle of the primary hinge matches the deformity. Two to three bone screws are inserted into the upper tibia from anteromedial to posterolateral and anterolateral to posteromedial avoiding the joint (note the proximal tibia slopes posteriorly) and the physis (if it is still open). The distal screws are placed in the distal tibial diaphysis, and the osteotomy is performed at a safe location in the proximal tibial. If rotational correction is needed, a rotation arc is chosen for the proximal component. Otherwise, a solid arc is chosen. Distally, a compression/distraction bone screw block is chosen and assembled to the MAC device through a male adaptor.
Fig. 6.
The guide hole through the primary hinge of the multiaxial correction device is placed over the guide pin and aligned so that the angle of the primary hinge matches the deformity.
We typically performed an osteotomy percutaneously with a Gigli saw in the tibia and with drill holes and an osteotomy in the femur. Anterior and lateral fasciotomies were performed for tibial corrections.
After 5 to 7 days, the compression/distraction device was used to lengthen ¼ mm (a 90° turn four times each day) for 1 week. This created a space allowing the flat osteotomy to slide along the arc defined by the MAC’s hinge. Then the angle was corrected with the hinge. Once the mechanical axis was restored, rotation could be corrected. If the MAC device was not properly aligned with the CORA, then secondary corrections could be made with the secondary hinge or translation screws without altering the device, returning to the operating room or using a computer to analyze the deformity or correction. Because the MAC device is based on a coordinate system, only anteroposterior and lateral radiographs need to be taken to define the alignment at each weekly visit.
The rate of correction was calculated to correct angular deformities at 4° per day or lengthen the bone at 1 mm per day. Lengthenings were performed four times each day by the patient or their parents or caretakers at home. The amount of rotation and the appropriate location on the fixator was determined by the surgeon (RSD, JJIM) using the basic trigonometric principles or from precalculated tables provided by the manufacturer (EBI/Biomet Trauma).
We reviewed charts for preoperative demographic data and to identify complications. Rotational deformity of the tibia had been assessed by clinically measuring the thigh-foot angle with the patient in a prone position. Weightbearing anteroposterior radiographs had been made for both lower extremities and lateral radiographs of affected limb segments to determine angular deformities and length discrepancy. One of us (AR) reviewed all radiographs to assess limb deformity and lengthening. Standard radiographic measurements were made, including the aLDFA for femoral deformities (Group I), the aMPTA for proximal tibial deformities (Group II), the tibiofemoral angle (TFA) to assess overall alignment (Group III), and limb length inequality [6].
Differences in the preoperative aLDFA and the postoperative aLDFA, the preoperative aMPTA and the postoperative aMPTA, and the preoperative TFA and the postoperative TFA were determined by the paired t test. The deviation from the normal measurements were determined in Groups I and III for the aLDFA and TFA, respectively. The preoperative aLDFA deviation from normal and the postoperative aLDFA deviation from normal as well as the preoperative TFA deviation from normal and the postoperative TFA deviation from normal were also compared using the paired t test.
Results
In Group I (femoral deformity or limb length inequality), the mean preoperative aLDFA was 83.3º and did not change (p = 0.46) postoperatively. We also observed no difference (p = 0.11) in the mean TFA (from 11.7º of valgus to 5.7º. Because these measurements are a summation of varus and valgus deformities, the mean changed little despite the fact that the deviation from normal improved. The mean deviation from normal of the aLDFA decreased (p = 0.054) from 7.5° to 4.2º, and the deviation of the TFA from normal (considered to be 6° of valgus) decreased (p = 0.041) from 9.3° to 2.7°. The mean length gain was 7.5 cm for the four patients who underwent lengthening, and the average time spent in the fixator was 9.6 months. The healing index for this group was 38 days/cm.
In Group II (Blount’s disease), the mean preoperative mean aMPTA was 59.9º preoperatively, which improved (p < 0.0069) to a mean of 87.8º postoperatively; the preoperative TFA was 25.2º of varus, which improved (p < 0.0004) to 4.8º of valgus postoperatively. One patient (one limb) had a recurrence of the varus deformity to 13° of varus at followup (from 28° preoperatively). The average time spent in the fixator for this group was 3.3 months.
In Group III (other tibial deformities), like patients in Group I, there was little improvement in the mean aMPTA or TFA resulting from the combination of varus and valgus deformities. The mean preoperative aMPTA was 84º and increased (p = 0.28) to 88º postoperatively. The TFA did not change (from 6.4º to 8.5º of valgus) in Group III. The mean deviation from normal of the aMPTA decreased (p = 0.05) from 7.3º to 2º, and the deviation of the TFA from normal (considered to be 6° of valgus) decreased (p = 0.0058) from 12.8º to 4.4º. The patient with knee flexion contracture of 45° was corrected to 10°. The mean length gain was 4.6 cm for the three patients who underwent tibial lengthening, and the time in the fixator (for these three patients) was 7 months with a healing index of 46 days/cm.
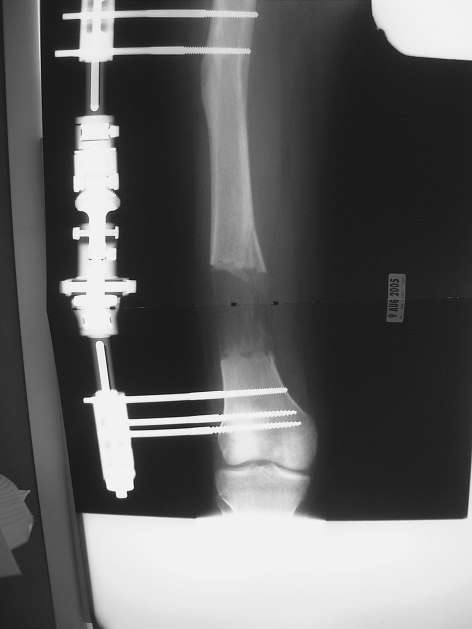
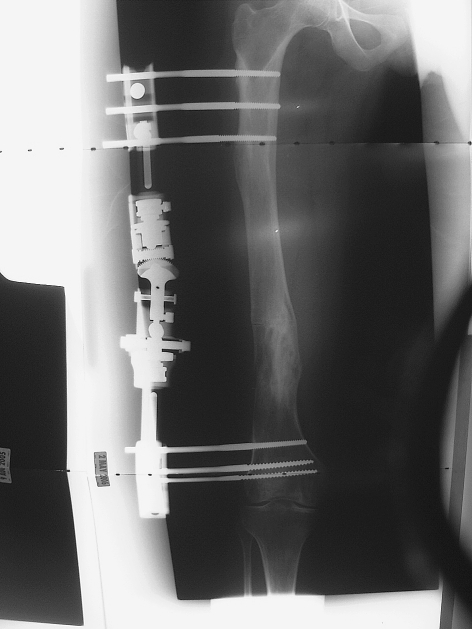
Five of the 25 procedures (20%) had complications. Two patients with pin site infection required admission for intravenous antibiotics. Other complications included premature consolidation of regenerate in one, development of knee flexion contracture in one, and recurrence of varus deformity of the tibia in one. There were no neurovascular complications. During the course of treatment, six patients developed secondary deformities as a consequence of a fall in three and secondary to lengthening in the rest. All of these deformities were corrected using the primary or secondary hinge. Except for one patient, these deformities had no impact on the final result. An example was a patient who underwent femoral lengthening with a secondary varus deformity after lengthening that was corrected by adjustment of the hinge on the MAC. They are shown immediately after lengthening (Fig. 7) and after lengthening and correction of the deformity (Fig. 8).
Fig. 7.
An example is shown of a patient who underwent femoral lengthening with a secondary varus deformity after lengthening.
Fig. 8.
Ten months later, the varus has been corrected and interval consolidation has occurred.
Discussion
Deformity correction in children can be achieved by various methods. The use of external fixation offers advantages of postoperative adjustment and simultaneous lengthening when indicated. Various types of external fixation devices have been used. External fixation, particularly with the ring fixators, can be cumbersome for patients and laborious for surgeons. We asked whether a monolateral fixator that allows for correction of angular deformity and displacement in three planes (MAC device), can correct lower extremity deformities to within normal radiographically mean measurements. The device has the advantages of a monolateral fixator but allows for correction of angulation and displacement in all three planes, and its use does not require a computer-generated program to adjust corrections.
Potential weaknesses of this study are the heterogeneous nature of the limb deformities in this patient group, the relatively small numbers of patients in each group, and the lack of a control group. To account for the heterogeneous group of patients, we divided the limb deformities into three groups clustering primary femoral deformities, Blount’s disease, and other tibial deformities into Groups I, II, and III, respectively. This allowed for in-group comparisons. Our study population was similar to many of those described in the literature, but still relatively small. We believed it was important to assess the first group of consecutive patients treated at our institution in a critical fashion, and larger controlled studies are currently underway. Our study is similar to the vast majority of those in the literature that report their results without a control group [2–5, 7, 9, 10]. We chose to use each patient as their own control and attempt to determine if surgery brought the deformity within the normal means of limb alignment.
Our data demonstrate a correction toward the normal alignment. Moreover, there was the ability to correct secondary deformities, whether residual or unrecognized by gradual angulation, across the primary or secondary hinge or displacement in either the sagittal or coronal planes. This process is much like the “residual correction on the Taylor special frame” but requires no computer assistance [3–5].
Our complication rate (20%, five complications in 25 limbs) is similar or less than the complication rate reported in other studies [2–5, 7, 9, 10]. This number also represents our learning curve for the application of new fixator, even though the complication rate was relatively low, implying this device is not particularly difficult to use for a surgeon with training in limb deformity. The healing index for those patients lengthened (Groups I and III) was 42 days/cm, which compares to the literature of approximately 40 to 50 days/cm with a longer healing index for tibial lengthenings than femoral [9, 11]. Like all fixators, both ring and monolateral, the fixator can interfere with radiographic evaluation either by directly obscuring the osteotomy site or secondary to patient positioning errors (such as knee flexion), which may lead to errors in angular or length measurements [8]. Care must be taken in accounting for these errors and oblique radiographs may need to be used to better visualize the osteotomy site.
We believe MAC is a good addition to the existing tools for pediatric deformity correction; it allows for correction of displacement and angulation in the sagittal and coronal planes and has the option of adding lengthening and rotational components. The time to construct the fixator is much less than with traditional Ilizarov devices and because it is applied as a monolateral device, it tends to be less cumbersome for the patient. Adjustments can be made intuitively without the need for a computer program.
Footnotes
One or more of the authors (JJM, RSD) has received funding from EBI/Biomet. The institution of the authors (Shriners Hospitals for Children) has received funding from EBI/Biomet.
Each author certifies that his or her institution has approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Birch JG, Samchukov ML. Use of the Ilizarov method to correct lower limb deformities in children and adolescents. J Am Acad Orthop Surg. 2004;12:144–154. [DOI] [PubMed]
- 2.Coogan PG, Fox JA, Fitch RD. Treatment of adolescent Blount disease with circular external fixation device and distraction osteogenesis. J Pediatr Orthop. 1996;16:450–454. [DOI] [PubMed]
- 3.Eidelman M, Bialik V, Katzman A. Correction of deformities in children using the Taylor spatial frame. J Pediatr Orthop B. 2006;15:387–395. [DOI] [PubMed]
- 4.Fadel M, Hosny G. The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop. 2005;29:125–129. [DOI] [PMC free article] [PubMed]
- 5.Feldman DS, Madan SS, Koval KJ, van Bosse HJ, Bazzi J, Lehman WB. Correction of tibia vara with six-axis deformity analysis and Taylor spatial frame. J Pediatr Orthop. 2003;23:387–391. [DOI] [PubMed]
- 6.Paley D, ed. Principles of Deformity Correction. Berlin, Germany: Springer-Verlag; 2002:61–89.
- 7.Price CT, Scott DS, Greenberg DA. Dynamic axial fixation in the surgical treatment of tibia vara. J Pediatr Orthop. 1995;15:236–243. [PubMed]
- 8.Sabharwal S, Badarudeen S, McClemens E, Choung E. The effect of circular fixation on limb alignment. J Pediatr Orthop. 2008;28:314–319. [DOI] [PubMed]
- 9.Sluga M, Pfeiffer M, Kotz R, Nehrer S. Lower limb deformities in children: two-stage correction using the Taylor spatial frame. J Pediatr Orthop B. 2003;12:123–128. [DOI] [PubMed]
- 10.Stanitski DF, Srivastava P, Stanitski CL. Correction of proximal tibial deformities in adolescents with the T-Garches external fixator. J Pediatr Orthop. 1998;18:512–517. [DOI] [PubMed]
- 11.Tsuchiya H, Uehara K, Abdel-Wanis ME, Sakurakichi K, Kabata T, Tomita K. Deformity correction followed by lengthening with the Ilizarov method. Clin Orthop Relat Res. 2002;402:176–183. [DOI] [PubMed]