Abstract
Distraction osteogenesis is an effective method for lengthening, deformity correction, and treatment of nonunions and bone defects. The classic method uses an external fixator for both distraction and consolidation leading to lengthy times in frames and there is a risk of refracture after frame removal. We suggest a new technique: lengthening and then nailing (LATN) technique in which the frame is used for gradual distraction and then a reamed intramedullary nail inserted to support the bone during the consolidation phase, allowing early removal of the external fixator. We performed a retrospective case-matched comparison of patients lengthened with LATN (39 limbs in 27 patients) technique versus the classic (34 limbs in 27 patients). The LATN group wore the external fixator for less time than the classic group (12 versus 29 weeks). The LATN group had a lower external fixation index (0.5 versus 1.9) and a lower bone healing index (0.8 versus 1.9) than the classic group. LATN confers advantages over the classic method including shorter times needed in external fixation, quicker bone healing, and protection against refracture. There are also advantages over the lengthening over a nail and internal lengthening nail techniques.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Distraction osteogenesis by the Ilizarov method is a widely used technique for leg lengthening, deformity correction [14, 15, 30, 31, 34], and reconstruction of nonunions and bone defects [11, 21, 24, 29, 33, 35]. The overall process is comprised of two stages, distraction and consolidation, which take place successively [14, 15]. External fixation has generally been considered necessary for both stages. In the adult patient, the consolidation phase can take a long time, leading to frame times of up to 2 months per cm of lengthening [9]. This prolonged time in a frame confers several disadvantages. First, there is a greater chance of health-related complications including pin tract infection and decreased range of motion in the surrounding joints. Second, the process can affect the patient psychologically, increasing frustration and decreasing compliance. Finally, when the frame is removed, there is a risk for fracture of the regenerated bone due to the lack of any internal stabilization. O’Carrigan et al. [26] reported an 8% fracture rate after frame removal in a review of 650 patients with 986 lengthening segments. Danziger et al. [8] reported refracture of the femur in 6 of 18 patients after frame removal. Simpson and Kenwright [37] reported a fracture rate of 9.4% in a series of 180 lengthening segments.
Other methods of lengthening that minimize or eliminate time in external fixation include lengthening over a nail [18, 28, 39, 42] and use of a fully implantable limb lengthening nail [5, 13]. These methods also have limitations noted in the literature [20] and in our own experience including infection [28, 39], need for acute deformity correction when a deformity is present [28], inability to control rate of lengthening resulting in nonunion and inability to distract the bone and achieve the desired lengthening [20].
We introduce a novel technique called lengthening and then nailing (LATN). External fixation is used for lengthening during the distraction phase. The external fixator is applied so that an intramedullary nail can be inserted while the frame is in place, however, without contact between the internal fixation and the external fixation pins and wires (Fig. 1). Once length has been achieved, a reamed locked intramedullary nail is inserted across the regenerate bone and the frame is removed. The intramedullary nail supports the bone during the consolidation phase allowing removal of the external fixator after the distraction phase of lengthening. Our goal was to decrease the time needed in external fixation and protect the bone from deformation and refracture.
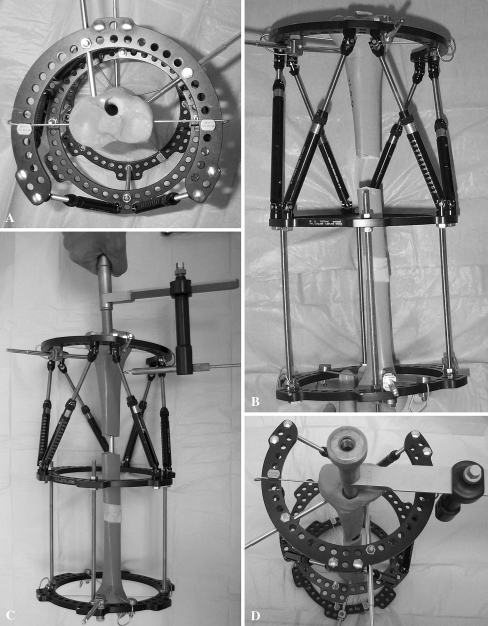
Fig. 1A–D.
This is a sawbone model illustrating LATN technique. (A) An axial view shows proximal fixation placed peripherally to avoid contact with future intramedullary nail. (B) This is a front view after 4-cm lengthening; note absent fixation on the middle ring. (C) Insertion of intramedullary nail is shown; note the targeting jig (EBI, Biomet Trauma, Parsippany, NJ) is not blocked by frame. (D) A Front axial view shows the proximal pin configuration and that the intramedullary nail is not blocked by the external fixation.
We asked the following questions: Does the LATN technique necessitate less time in an external fixator, result in faster bone healing, and have a lower rate of refracture compared to the classic method of limb lengthening? Is there a greater risk of deep infection with LATN compared to the classic method?
Methods
We performed a retrospective matched-case comparison with patients lengthened using LATN and the classic Ilizarov method. We used LATN to treat 39 limbs (35 tibiae and four femora) in 27 selected patients between 2001 and 2006. All patients who underwent LATN were included in the study. We selected patients for LATN according to the following criteria: there was an absence of active or history of infection at the site of bone lengthening and area of subsequent nailing; the intramedullary canal was of suitable shape and size to accommodate an intramedullary nail; there were no open growth plates that would be damaged by an intramedullary nail. The Ilizarov/Taylor Spatial Frame (TSF) (Smith & Nephew, Inc., Memphis, TN) or EBI/ Biomet (Parsippany, NJ) monolateral rail frames were used in the tibia and femur, respectively, for the distraction phase along with pin/wire placement to allow for subsequent intramedullary nailing. At the end of distraction, reamed intramedullary nails were inserted and the frames were removed. We identified 27 patients who underwent lengthening using the classic Ilizarov method and individually matched these to the LATN patients. The criteria for matching included amount of lengthening, etiology of the problem, and age of the patient. The method used resembled that used by Paley et al. [28] in their comparison study between femoral lengthening using the classic method versus lengthening over a nail. All patients in both groups underwent surgery by the senior author (SRR). There were no differences between the groups regarding etiology (Table 1), age, surgery site, amount of lengthening (Table 2), and followup. The minimum followup for the LATN group was 11.4 months (mean, 40 months; range, 11.4 to 71.1 months). The minimum followup for the classic group was 12.1 months (mean, 41 months; range, 12.1 to 88.8 months). This was an IRB-approved retrospective case-matched series taken from our IRB-approved limb lengthening database.
Table 1.
Etiology in both patient groups
| Etiology | LATN | Classic |
|---|---|---|
| Bilateral (short stature, deformity) | 12 | 7 |
| Malunion | 6 | 7 |
| Nonunion | 3 | 4 |
| Congenital | 2 | 3 |
| Polio | 1 | 1 |
| Growth arrest | 1 | 5 |
| Fibrous dysplasia | 2 | 0 |
LATN = lengthening and then nailing group.
Table 2.
Patient demographics
| Variable | LATN | Classic |
|---|---|---|
| Age in years (range) | 35 (22–55) | 30 (11–57) |
| Lengthening (cm) | 5.4 (1.5–10) | 3.9 (1.2–7.5) |
| Number of patients | 27 | 27 |
| Number of tibiae | 35 | 31 |
| Number of femurs | 4 | 3 |
| Tibia lengthening (cm) | 5.6 (2.4–10) | 4 (1.2–7.5) |
| Femur lengthening (cm) | 5.3 (2.6–7) | 3 (2–4) |
An external fixator index (EFI) [9] was defined as the time in external fixation in months divided by the amount of lengthening in centimeters. A bone healing index (BHI) [9] was defined as the time until bony union in months divided by the amount of lengthening in centimeters.
We performed a fibular osteotomy under tourniquet control. A 3-cm incision was made on the lateral aspect of the middle leg and the fibula was approached in the interval between the lateral and posterior compartment. The fibula osteotomy was then performed using a multiple-drill-hole technique with a 1.8-mm wire and then completed with an osteotome. The tourniquet is not used for the remainder of the surgery. A three-ring TSF was applied using a rings-first method [32]. The proximal ring was stabilized with a 1.8-mm tensioned transverse wire, a 1.8-mm tibia-fibula wire, an anteromedial half pin, and an anterolateral half pin. The configuration of this proximal ring fixation is unique in that the bone fixation is placed peripherally within the proximal tibia to allow future insertion of an intramedullary nail avoiding any contact with the external fixation pins. The 1.8-mm wires were placed more posterior in the tibia than is typical. We placed the half pins using a cannulated wire technique for precision. The anteromedial half pin was peripheral and ran in an anterior to posterior direction. The anterolateral half pin was peripheral and ran in an anterolateral to posterior central direction (Fig. 1). The proximal ring was the reference ring and TSF mounting parameters were measured in relation to this ring [32]. The origin was placed at the level of deformity within the diaphysis. When there was no deformity, we assigned the origin to the center of the bone at the level of osteotomy 10 to 12 cm distal to the knee joint. Next, a ring block consisting of two rings connected with four rods was applied to the mid-distal tibia orthogonal to the tibial diaphysis. The distal ring was stabilized with a transverse 1.8-mm wire 1.5 cm proximal to the ankle, a-1.8 mm tibia-fibula wire 2 cm proximal to the ankle, and an anteromedial to posterolateral 6-mm half-pin. The middle ring was left with no fixation. The proximal and middle rings were then connected with six TSF struts whose lengths were recorded. The struts were then removed for the tibial osteotomy.
The tibial osteotomy was performed in a percutaneous fashion using a multiple-drill-hole technique. The osteotomy was then stabilized in a nondisplaced position by reattaching the struts. Distraction was started on postoperative day 7–10. The distraction schedule was made using the TSF internet based software using the total residual method (Smith and Nephew Inc, Memphis, TN). Care was taken to correct all deformity at the osteotomy site prior to nail insertion (Fig. 2).
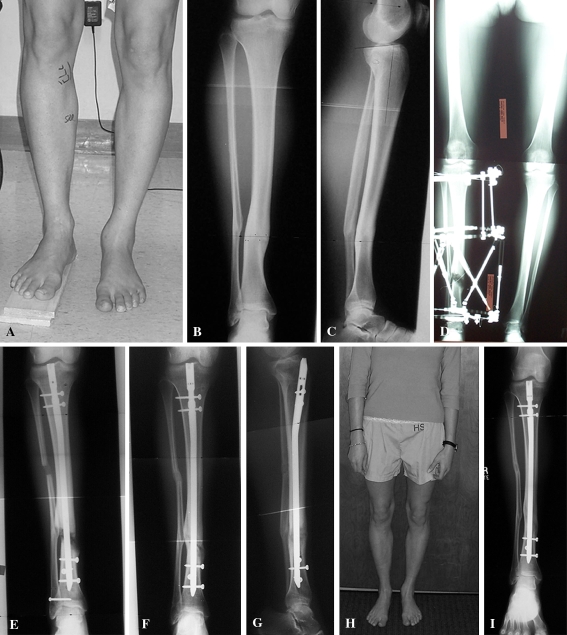
Fig. 2A–I.
This is an example of a 23-year-old woman who underwent correction of varus, recurvatum, external rotation malunion, and 2.5 cm lengthening. (A) A preoperative front view shows deformity and shortening. (B) This is a preoperative AP radiograph. (C) This is a preoperative lateral radiograph. (D) This is an erect leg radiograph at end of distraction showing equal leg lengths and correction of deformity. (E) This is an AP radiograph 2 weeks after insertion of intramedullary nail. (F) This is an AP radiograph 3 months after insertion of intramedullary nail. (G) This is a lateral radiograph 3 months after insertion of intramedullary nail. (H) This is a front view 2 years after surgery. (I) This is an AP radiograph 2 years after surgery.
Once length and deformity correction were achieved, the second-stage surgery was scheduled with minimal delay. We avoided surgery if there was an active pin tract infection. We used no tourniquet. The external fixator was sprayed with a Betadine solution and prepped into the surgical field. Betadine-soaked sponges were placed around all pin sites. The frame was covered with sterile towels and contact with it was avoided as much as possible. To prevent proximal migration of the fibula, we inserted a 4.5-mm solid syndesmosis screw 1 cm proximal to the distal tibia pin fixation. The screw was placed in an oblique fashion engaging two cortices of the fibula and two cortices of the tibia. We templated the nail diameter and length prior to surgery and had a custom interlocking hole made so that two interlocking screws could be inserted into the proximal segment without using the standard proximal interlocking screw hole. The standard proximal hole was typically at the same level as the previously placed external fixation pins and this would lead to contamination (Fig. 3). We used a minimal incision technique for IM nail insertion. IM nails used were manufactured by Synthes (Paoli, PA) and EBI/ Biomet (Parsippany, NJ). With the knee flexed, a percutaneously placed Steinmann pin was used to localize the optimal location for nail entry in the proximal tibia. This was performed with biplanar fluoroscopy and care was taken to avoid contact with previously placed external fixator pins. A 2-cm incision was made and the patella tendon incised longitudinally. A 10-mm cannulated drill was used to open the IM canal. The guide wire was passed across the regenerate and into the distal fragment ending at the syndesmosis screw. Serial reaming was performed until cortical chatter was achieved and a nail 1 mm smaller inserted. We ensured the maximum amount of reaming particles was retained within the tibia. We did not open the regenerate site and we did not remove any reaming particles. One proximal interlocking screw was inserted using a special jig that allowed clearance of the proximal ring (Fig. 1C–D). The second proximal interlocking screw and the two distal interlocking screws were placed using a freehand technique. Surgical wounds were irrigated and closed and covered with betadine sponges. The external fixator was then removed without risk of tibial displacement or shortening. The pin sites were irrigated but not curettaged and not closed. The surgical wounds and pin sites were covered with a dry sterile dressing. When gastrocnemius recession was done, it was performed after frame removal.
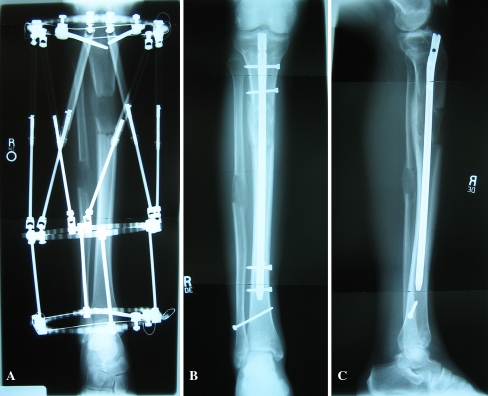
Fig. 3A–C.
This is an example of a 45-year-old man who underwent 5 cm lengthening. (A) This is an anteroposterior (AP) radiograph at the end of distraction. (B) This is an AP radiograph 8 weeks after insertion of the intramedullary nail. (C) This is a lateral radiograph 8 weeks after insertion of the intramedullary nail.
Postoperatively a cast or splint was not used. Twenty-pound partial weight bearing was allowed after surgery in unilateral cases. In bilateral cases, protected weight bearing with crutches was allowed for transfers and walking less than 10 steps at a time for a maximum of 50 steps per day. Prophylactic intravenous antibiotics were administered for 48 hours after surgery.
Descriptive statistics were obtained on all variables. We used T-tests to compare normally distributed data such as age, and Mann-Whitney analysis was used to compare the other variables such as LLD between the two lengthening groups. The usual reason for failing the test for a Gaussian distribution was a truncated tail due to a large standard deviation. There were occasional missing values. The alpha was set at 0.05. However, the cases where we identified difference all had probability values below the 0.001 level and therefore would likely be significant even after a Bonferroni correction. We used Systat v10.2 (Systat Software Inc. Richmond CA) for all analyses.
Results
The LATN group wore the external fixator for less time than the group treated with the classic method (Table 3). We found lower EFI in the LATN group. The BHI was lower in the LATN group (Table 3). The joint-orientation angles around the knee (lateral distal femoral angle (LDFA) and the medial proximal tibial angle (MPTA) measurements for both subgroups) remained or were slightly restored to within their normal ranges (Table 4). The ankle and knee range of motion did not change with treatment in both groups (Table 5).
Table 3.
Clinical results
| Variable | LATN | Classic | p value |
|---|---|---|---|
| Followup (months) | 40 (8–74) | 41 (12–88) | 0.9 |
| Time in frame (weeks) | 12 (3–27) | 29 (14–55) | <0.001 |
| ED to frame removal (days) | 9.6 (0–35) | 130 (45–278) | <0.001 |
| EFI (months/cm) | 0.5 (0.3–1.1) | 1.9 (1–4) | <0.001 |
| BHI (months/cm) | 0.8 (0.4–1.3) | 1.9 (1–4) | <0.001 |
ED = end distraction; EFI = external fixation index; BHI = bone healing index.
All results expressed as mean (range).
Table 4.
Radiographic results
| Variable | LATN | Classic | p Value |
|---|---|---|---|
| LLD preoperative (cm) | 4.9 (1.1–12.9) | 3 (0.5–8) | 0.6 |
| LLD postoperative | 0.8 (0–5.5) | 0.5 (0–5) | 0.1 |
| LDFA preoperative | 88 (83–95) | 88.2 (82–93) | 0.7 |
| LDFA postoperative | 87.5 (81–91) | 87.7 (81–93) | 0.8 |
| MPTA preoperative | 86.5 (72–121) | 85.3 (72–95) | 0.4 |
| MPTA postoperative | 87.2 (83–105) | 87.4 (80–98) | 0.8 |
LLD = leg length discrepancy; LDFA = lateral distal femoral angle; MPTA = medial proximal tibial angle.
Table 5.
Knee and ankle range of motion
| Range of motion type | LATN (degrees) | Classic (degrees) |
|---|---|---|
| Preoperative knee | Ext: 0.6 (−15–5) | Ext: −1.6 (−15–5) |
| Flex: 129 (90–140) | Flex: 131.2 (125–140) | |
| Postoperative knee | Ext: −0.4 (−5–10) | Ext: −0.5 (−10–0) |
| Flex: 126.3 (90–140) | Flex: 129.5 (110–145) | |
| Preoperative ankle | DF: 11.4 (−25–20) | DF: 13.9 (−10–25) |
| PF: 42.6 (20–70) | PF: 44.5 (20–70) | |
| Postoperative ankle | DF: 7.3 (−15–20) | DF: 12.1 (0–20) |
| PF: 38.2 (25–50) | PF: 42.2 (25–70) |
Values are expressed as mean (range). Ext = extension; Flex = flexion; DF = dorsiflexion; PF = plantar flexion.
We observed some complications in the LATN group. One patient with a femoral lengthening had a sciatic nerve palsy that resolved without any further intervention. One patient had skin breakdown over a prominent proximal tibial interlocking screw and deep infection occurred after complete bone healing. This was treated successfully with removal of the intramedullary nail and administration of six weeks of intravenous antibiotics. There were two patients with premature consolidation of the fibula that required repeat fibula osteotomy. Joint contractures were successfully addressed with gastrocnemius recessions in 17 limbs of 10 patients, gradual correction of ankle equines contracture in one patient, quadricepsplasty in one patient, and gradual correction of knee flexion contracture in one patient. Additional procedures included planned ankle fusion (Fig. 4) in two patients and removal of intramedullary nails in 11 limbs for symptoms of painful hardware in 10 patients and deep infection in one patient. Complications in the classic lengthening group included joint contractures treated successfully with quadricepsplasty in three patients and gastrocnemius recession in two limbs of one patient. There was one deep pin infection that was treated with removal, curettage, and administration of six weeks of intravenous antibiotics. There were no nonunions or refractures in either group. There were no differences in rate of deep infection between the two groups.
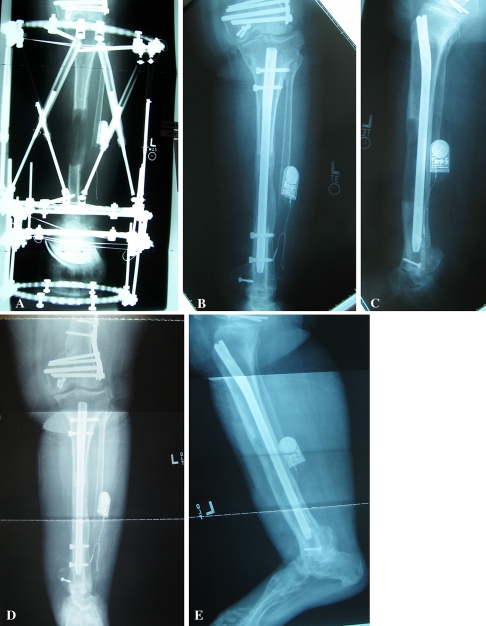
Fig. 4A–E.
This is an example of a 55-year-old woman who underwent ankle fusion and 10 cm lengthening for a segmental bone defect. (A) This is an AP radiograph at end of 10 cm distraction; the ankle fusion is stabilized more distally. (B) This is an AP radiograph 4 months after insertion of the intramedullary nail. (C) This is a lateral radiograph 4 months after insertion of the intramedullary nail. (D) This is an AP radiograph 9 months after insertion of the intramedullary nail. (E) This is a lateral radiograph 9 months after insertion of the intramedullary nail.
Discussion
LATN was developed to decrease the time needed in the frame, speed bone healing, and protect the lengthened limb against refracture. We reviewed our experience with a consecutive group of 39 limbs in 27 patients. To evaluate our outcomes and evaluate if indeed LATN had these advantages, we compared our group to a matched cohort of our patients who underwent tibial lengthening with the classic method.
The major limitation of our study is that it is retrospective without concurrent controls matched in all aspects. However, the patients of the case-matched comparison cohort were chosen by amount of lengthening, age, and etiology. In our practice, we had many more patients who underwent tibia lengthening with the classic method than those who underwent LATN. None of the patients chosen in the classic group had experienced a fracture, despite the fact that this is a documented problem [8, 26, 37] after frame removal in classic lengthenings. There were no fractures in either group in the current study. Another limitation is the difficulty of assigning a point of bony union. We do not believe this jeopardized our conclusions since we used consistent practical time points for healing. For the classic group, we chose the time of frame removal which corresponded to the patient’s ability to bear full weight on the leg with the frame and bridging of three of four cortices on radiographs. For the LATN group, we chose ability to bear full weight on the leg with the intramedullary nail and also bridging of three of four cortices on radiographs. The number of patients in the study is too small to demonstrate differences in low-frequency complications such as fracture or infection. It is possible that with large numbers of patients, we would be able to demonstrate such differences. However, the number of patients in each group was appropriate to demonstrate notable differences in EFI and BHI.
We demonstrated a very low EFI and BHI in the LATN group. The LATN patients wore the frame about ¼ the time of the classic group and bony union occurred in less than half the time of the classic group. The low EFI is related to the ability to remove the frame immediately after the distraction phase of lengthening. The bone is supported by the intramedullary nail during the consolidation phase. The classic group’s time to bone healing was in line with that reported by Fischgrund et al. [9]. Bone healing in the LATN group was substantially quicker than that seen in the classic group.
We speculate the reaming through the regenerate enhances and speeds bone healing. In our patient group, bone healing was sufficient to allow full weight bearing without pain within 6 to 8 weeks in most patients. We have observed extraordinary radiographic healing during the first several weeks after IM nailing. This is in comparison to our 8-year clinical experience [24, 29–31, 33–35] observing bone healing after conventional distraction osteogenesis. In our study, the BHI was lower in the LATN group (0.8 versus 1.9). This phenomenon may be compared to exchange nailing for nonunions of the femur and tibia. Several reports document rates of union [3, 12, 23, 40, 43, 44] ranging from 78% to 96%. The biological effects of exchange nailing are likely similar to that seen in the current series. Reaming of the medullary canal increases periosteal blood flow and stimulates periosteal new bone formation [7]. Blood flow in the cortex returns to normal and even supernormal levels within days after medullary reaming. The periosteum reacts to the increased blood flow by forming new bone [7]. Some have suggested the products of reaming, which contain osteoblasts and multipotent stem cells, serve as local bone graft that stimulates medullary healing [3]. Utvag et al. [41] demonstrated increased bone mineral content and density in the callus segment compared to controls after intramedullary nailing in a rat femur model. They suggested increased mineralization of the callus was the mechanism of enhanced healing. An osteoinductive effect of reaming particles and intense new bone formation is observed around reaming dust, if it is surrounded by vital tissue [16].
Other possible mechanisms by which reaming stimulates healing include activation of growth factors [1, 3], induction of an inflammatory response [1, 3, 10, 38], and attenuation of immune system reactivity [3, 38]. Messenger RNA expression for a variety of angiogenic factors, extracellular matrix proteins, and bone morphogenic proteins (BMPs) are maximal during the distraction phase of lengthening [4, 27]. These factors are early mediators produced by distraction that contribute toward the processes that promote bone formation. We presume reaming through the regenerate may stimulate a second surge in growth factors in addition to providing local bone graft to the regenerate bone.
Intramedullary nail insertion after external fixation is generally avoided because of concern regarding deep infection. Insertion of an intramedullary nail after external fixation has been reported previously in setting of complicated fractures [2, 6, 17, 22, 25, 36] and complications after distraction osteogenesis. There is understandably a risk of infection when inserting an intramedullary nail after previous external fixation. Pin sites may become colonized with bacteria. This has been best documented when an intramedullary nail is inserted after initial use of external fixation for high-energy and open tibial fractures. Rates of infection in this situation have ranged between 1.7% and 21% and bony union rates were high [2, 6, 17, 22, 25, 36]. These were cases of high-energy open fractures that are initially treated with external fixation. The interval between removal of the fixator and insertion of intramedullary nail varied from immediate to a delay of few weeks. Maurer et al. [22] reported the high incidence in their series and noted five of the seven infections were in cases with documented pin tract infections. They concluded a pin tract infection was a contraindication. Siebenrock et al. [36] reported an infection rate of 4.1% and bony union rate of 96%. They concluded sequential nailing can be performed without the necessity of a safety interval between removal of external fixation and insertion of intramedullary nail. Our rate of infection was 2.5%. The main differences in our patient group were a healthy, well-vascularized bone and planned absence of contact between internal fixation and external fixation pin tracts.
Lai et al. [19] reported the use of locked intramedullary nails in the treatment of complications after distraction osteogenesis including nonunion at lengthening and docking sites. They achieved 100% bony union in 27 patients and had a deep infection rate of 7%. There are differences from our patient group including long times in external fixation prior to removal and pins placed in the intramedullary canal not intended to avoid contact with an intramedullary nail.
Another technique, known as lengthening over a nail, [18, 28, 39, 42] was introduced in an attempt to eliminate the disadvantages of the classic Ilizarov method. During this process, an intramedullary nail is inserted after an osteotomy is performed. A frame is then applied during the same surgery to lengthen over the nail. At the end of distraction, the nail is locked and the frame is removed. Time spent in an external fixator is reduced while still providing support for the bone with an intramedullary nail during the consolidation phase. However, the total bone healing time does not appear less than that of the classic method [42]. This technique has certain limitations, however, mainly inherent in the concurrent use of internal and external fixation [18, 39]. Song et al. reported a 14% rate of deep infection after lengthening over a nail [39].
There may be several advantages of the LATN over the lengthening over a nail technique, including the ability to insert a full-length large-diameter nail for more stability. In the lengthening over a nail technique a small-diameter nail is used so the bone can slide over the nail. In addition the nail is pulled out of the distal fragment with lengthening leading to suboptimal stability; also, distraction over a nail can sometimes be difficult and mechanical binding from nail impingement can prevent lengthening [18]. This problem is avoided with the LATN technique. With the LATN technique, there is no concomitant use of internal and external fixation, and this should lower the risk of infection. In the lengthening over a nail procedure, if a pin tract infection occurs during the distraction phase, the presence of the nail increases the chances that the infection will spread to become a deep infection. If a pin tract infection develops during the LATN technique, it can be treated with antibiotics or with pin removal prior to IM nail insertion. Additionally, the timing of intramedullary nail insertion can be adjusted if need be. Like the classic method, LATN affords the ability to gradually correct diaphyseal deformity and lengthen prior to nail insertion. Lengthening over a nail or use of an internal lengthening nail requires an acute deformity correction which compromises bone healing potential during subsequent lengthening. A distal third tibial deformity could not be treated with lengthening over a nail since the IM nail would be pulled out of the distal segment during lengthening.
There were more joint contractures in the LATN group. This may be attributed to larger lengthening in the LATN and the fact that foot was more often included in the frame in the classic group. In addition, the tibial osteotomy of the LATN group was typically 10 cm from the knee compared to 5 cm in the classic group, possibly leading to more soleus muscle stretch.
LATN is an effective technique that decreases time needed in external fixation, speeds bone healing, and protects against refracture. While infection is a risk, it is minimal because of planned absent contact between internal and external fixation and use of the technique on healthy, well-vascularized bone. If a deep infection does occur, we recommend immediate removal of the intramedullary nail and treatment with six weeks of culture-specific intravenous antibiotics. If the bone is healed, then no additional stabilization is needed as was the case in the one deep infection in the present series. If bony union is not complete, then we recommend repeat application of a circular frame until bone healing is complete.
Acknowledgments
We thank Dr. Margaret Peterson for her assistance with the statistical analysis.
Footnotes
The institution of the authors has received funding from Smith and Nephew, Inc (Memphis, TN) and EBI, Biomet (Parsippany, NJ).
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bhandari M, Schemitsch EH. Bone formation following intramedullary femoral reaming is decreased by indomethacin and antibodies to insulin-like growth factors. J Orthop Trauma. 2002;16:717–722. [DOI] [PubMed]
- 2.Blachut PA, Meek RN, O’Brien PJ. External fixation and delayed intramedullary nailing of open fractures of the tibial shaft. A sequential protocol. J Bone Joint Surg Am. 1990;72:729–735. [PubMed]
- 3.Brinker MR, O’Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am. 2007;89:177–188. [DOI] [PubMed]
- 4.Carvalho RS, Einhorn TA, Lehmann W, Edgar C, Al-Yamani A, Apazidis A, Pacicca D, Clemens TL, Gerstenfeld LC. The role of angiogenesis in a murine tibial model of distraction osteogenesis. Bone. 2004;34:849–861. [DOI] [PubMed]
- 5.Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C. The intramedullary skeletal kinetic distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury. 2001;32(4):SD129–SD139. [DOI] [PubMed]
- 6.Cosco F, Risi M, Pompili M, Boriani S. External fixation and sequential nailing in the treatment of open diaphyseal fractures of the tibia. Chir OrganiMov. 2001;86:191–197. [PubMed]
- 7.Danckwardt-Lilliestrom G. Reaming of the medullary cavity and its effect on diaphyseal bone. A fluorochromic, microangiographic and histologic study on the rabbit tibia and dog femur. Acta Orthop Scand Suppl. 1969;128:1–153. [DOI] [PubMed]
- 8.Danziger MB, Kumar A, DeWeese J. Fractures after femoral lengthening using the Ilizarov method. J Pediatr Orthop. 1995;15:220–223. [PubMed]
- 9.Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res. 1994;301:31–37. [PubMed]
- 10.Giannoudis PV, Smith RM, Bellamy MC, Morrison JF, Dickson RA, Guillou PJ. Stimulation of the inflammatory system by reamed and unreamed nailing of femoral fractures. An analysis of the second hit. J Bone Joint Surg Br. 1999;81:356–361. [DOI] [PubMed]
- 11.Green SA, Garland DE, Moore TJ, Barad SJ. External fixation for the uninfected angulated nonunion of the tibia. Clin Orthop Relat Res. 1984;190:204–211. [PubMed]
- 12.Hak DJ, Lee SS, Goulet JA. Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma. 2000;14:178–182. [DOI] [PubMed]
- 13.Hankemeier S, Gosling T, Pape HC, Wiebking U, Krettek C. Limb lengthening with the Intramedullary Skeletal Kinetic Distractor (ISKD). Oper Orthop Traumatol. 2005;17:79–101. [DOI] [PubMed]
- 14.Ilizarov GA. Tranosseous Osteosynthesis. 1st ed. Berlin, Germany: Springer-Verlag; 1992.
- 15.Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8–26. [PubMed]
- 16.Kessler SB, Hallfeldt KK, Perren SM, Schweiberer L. The effects of reaming and intramedullary nailing on fracture healing. Clin Orthop Relat Res. 1986;212:18–25. [PubMed]
- 17.Klezl Z, Rennirt G, Seligson D. Secondary intramedullary nailing of complicated fractures of lower extremities. Acta Chir Orthop Traumatol Cech. 1993;60:88–92. [PubMed]
- 18.Kocaoglu M, Eralp L, Kilicoglu O, Burc H, Cakmak M. Complications encountered during lengthening over an intramedullary nail. J Bone Joint Surg Am. 2004;86:2406–2411. [DOI] [PubMed]
- 19.Lai KA, Lin CJ, Chen JH. Application of locked intramedullary nails in the treatment of complications after distraction osteogenesis. J Bone Joint Surg Br. 2002;84:1145–1149. [DOI] [PubMed]
- 20.Leidinger B, Winkelmann W, Roedl R. Limb lengthening with a fully implantable mechanical distraction intramedullary nail [in German]. Z Orthop Ihre Grenzgeb. 2006;144:419–426. [DOI] [PubMed]
- 21.Lowenberg DW, Feibel RJ, Louie KW, Eshima I. Combined muscle flap and Ilizarov reconstruction for bone and soft tissue defects. Clin Orthop Relat Res. 1996;332:37–51. [DOI] [PubMed]
- 22.Maurer DJ, Merkow RL, Gustilo RB. Infection after intramedullary nailing of severe open tibial fractures initially treated with external fixation. J Bone Joint Surg Am. 1989;71:835–838. [PubMed]
- 23.Mercado EM, Lim EV, Stern PJ, Aquino NJ. Exchange nailing for failure of initially rodded tibial shaft fractures. Orthopedics. 2001;24:757–762. [DOI] [PubMed]
- 24.Nho SJ, Helfet DL, Rozbruch SR. Temporary intentional leg shortening and deformation to facilitate wound closure using the Ilizarov/Taylor spatial frame. J Orthop Trauma. 2006;20:419–424. [DOI] [PubMed]
- 25.Nowotarski PJ, Turen CH, Brumback RJ, Scarboro JM. Conversion of external fixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J Bone Joint Surg Am. 2000;82:781–788. [DOI] [PubMed]
- 26.O’Carrigan T, Paley D, Herzenberg JE. Obstacles in limb lengthening: fractures. In: Rozbruch SR, Ilizarov S, eds. Limb Lengthening and Reconstruction Surgery. New York, NY: Informa Healthcare; 2007:675–679.
- 27.Pacicca DM, Patel N, Lee C, Salisbury K, Lehmann W, Carvalho R, Gerstenfeld LC, Einhorn TA. Expression of angiogenic factors during distraction osteogenesis. Bone. 2003;33:889–898. [DOI] [PubMed]
- 28.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. [DOI] [PubMed]
- 29.Pugh K, Rozbruch SR. Nonunions and malunions. In: Baumgaertner MR, Tornetta P, eds. Orthopaedic Knowledge Update Trauma 3. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005:115–130.
- 30.Rozbruch SR. Post-traumatic reconstruction of the ankle using the Ilizarov method. J Hosp Special Surg. 2005;1:68–88. [DOI] [PMC free article] [PubMed]
- 31.Rozbruch SR, DiPaola M, Blyakher A. Fibula lengthening using a modified Ilizarov method. Orthopedics. 2002;25:1241–1244. [DOI] [PubMed]
- 32.Rozbruch SR, Fragomen AT, Ilizarov S. Correction of tibial deformity with use of the Ilizarov-Taylor spatial frame. J Bone Joint Surg Am. 2006;88(4):156–174. [DOI] [PubMed]
- 33.Rozbruch SR, Ilizarov S, Blyakher A. Knee arthrodesis with simultaneous lengthening using the Ilizarov method. J Orthop Trauma. 2005;19:171–179. [DOI] [PubMed]
- 34.Rozbruch SR, Paley D, Bhave A, Herzenberg JE. Ilizarov hip reconstruction for the late sequelae of infantile hip infection. J Bone Joint Surg Am. 2005;87:1007–1018. [DOI] [PubMed]
- 35.Rozbruch SR, Weitzman AM, Watson JT, Freudigman P, Katz HV, Ilizarov S. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma. 2006;20:197–205. [DOI] [PubMed]
- 36.Siebenrock KA, Schillig B, Jakob RP. Treatment of complex tibial shaft fractures. Arguments for early secondary intramedullary nailing. Clin Orthop Relat Res. 1993;290:269–274. [PubMed]
- 37.Simpson AH, Kenwright J. Fracture after distraction osteogenesis. J Bone Joint Surg Br. 2000;82:659–665. [DOI] [PubMed]
- 38.Smith RM, Giannoudis PV, Bellamy MC, Perry SL, Dickson RA, Guillou PJ. Interleukin-10 release and monocyte human leukocyte antigen-DR expression during femoral nailing. Clin Orthop Relat Res. 2000;373:233–240. [DOI] [PubMed]
- 39.Song HR, Oh CW, Mattoo R, Park BC, Kim SJ, Park IH, Jeon IH, Ihn JC. Femoral lengthening over an intramedullary nail using the external fixator: risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop. 2005;76:245–252. [DOI] [PubMed]
- 40.Templeman D, Thomas M, Varecka T, Kyle R. Exchange reamed intramedullary nailing for delayed union and nonunion of the tibia. Clin Orthop Relat Res. 1995;315:169–175. [PubMed]
- 41.Utvag SE, Grundnes O, Reikeras O. Graded exchange reaming and nailing of non-unions. Strength and mineralisation in rat femoral bone. Arch Orthop Trauma Surg. 1998;118:1–6. [DOI] [PubMed]
- 42.Watanabe K, Tsuchiya H, Sakurakichi K, Yamamoto N, Kabata T, Tomita K. Tibial lengthening over an intramedullary nail. J Orthop Sci. 2005;10:480–485. [DOI] [PubMed]
- 43.Wu CC, Shih CH, Chen WJ, Tai CL. High success rate with exchange nailing to treat a tibial shaft aseptic nonunion. J Orthop Trauma. 1999;13:33–38. [DOI] [PubMed]
- 44.Zelle BA, Gruen GS, Klatt B, Haemmerle MJ, Rosenblum WJ, Prayson MJ. Exchange reamed nailing for aseptic nonunion of the tibia. J Trauma. 2004;57:1053–1059. [DOI] [PubMed]