Abstract
The Taylor spatial frame (TSF) has been used commonly in children and young adults. Its use in the tibia is more extensively studied and applied than in the femur. We asked whether normal alignment can be achieved with accuracy during correction of femoral deformities while avoiding major complications in children and young adults. We retrospectively reviewed the clinical and radiographic records of 20 patients (22 limbs), ages 5.9 to 24.6 years, who underwent a TSF for femoral deformity. Etiology included a number of diagnoses of the pediatric age. Minimum followup was 4.5 months (mean, 15.7 months; range, 4.5–35 months). The mean time in frame was 6.2 months (range, 2.6–19 months). Frontal and sagittal plane deformities were corrected to within normal values. A mean limb lengthening of 4.9 cm (range, 1.5–9 cm) was performed in eight femora in seven of which the limb length discrepancy was a secondary concern. External fixation index in the lengthening subgroup was 2.2 months/cm. The 15 complications in 13 limbs included pin tract infection, knee stiffness, delayed union, skin irritation, and posterior knee subluxation. No complications occurred in nine limbs. Computer-assisted femoral deformity correction with six-axis deformity analysis and the TSF is an accurate and safe technique in children and young adults.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The Taylor spatial frame (TSF) applies the basic principles of a six-axis platform and is commonly used in clinical practice for the correction of multiplanar deformities in the pediatric and adult populations. The TSF has the ability to correct any deformity in six axes in all three planes (frontal, sagittal, and axial) with the aid of computer-based software readily available online [20]. The femoral deformities that can be treated individually or in any combination with the TSF are frontal plane angulation (varus/valgus), frontal plane translation (medial/lateral), sagittal plane angulation (procurvatum/recurvatum), sagittal plane translation (anterior/posterior), axial plane angulation (internal rotation [anteversion]/external rotation [retroversion]), and axial plane translation (short/long).
The limited studies available involving the TSF concentrate on its tibial use [1, 2, 5–7]. With the use of TSF, fractures were all reduced anatomically [1, 2] and normal alignment was achieved in all deformities involving the tibia [5–7].
The purposes of this study were to gather data on the time spent in the frame, the mean followup time, the additionally performed surgeries, the accuracy of correction in various lower extremity deformities (ie, genu valgum, genu varum, and sagittal plane deformities), the amount of limb lengthening that was obtained, and the safety of the use of the TSF by reviewing the complications. We also described the treatment modalities in femoral deformities in children and young adults.
Materials and Methods
We retrospectively reviewed the records of all 20 patients (22 femurs) treated with a femoral TSF (Smith & Nephew, Inc., Memphis, TN) between July 1999 and December 2006. No patients were specifically recalled for this chart review. Twelve were left and 10 were right. The 12 female and eight male patients had a mean age of 13.9 years (range, 5.9–24.6 years) at the time of surgery. Eighteen patients were younger than 18 years old and two were in their early 20s. The etiologies of the femoral deformities were seven traumatic, six developmental (idiopathic), two multiple enchondromatosis, two rickets, two congenital femoral deficiency, one spondyloepiphyseal dysplasia, one congenital pseudohypoparathyroidism, and one multifocal osteomyelitis. The primary femoral deformities were eight valgus, six varus, three anterolateral bowing, one anteromedial bowing, one posteromedial bowing, one recurvatum, one procurvatum, and one shortened limb. The secondary deformities were two external rotations (retroversion), two internal rotations (anteversion), and seven limb-length inequalities (shortened limb). Every deformity was analyzed for translation and/or angulation in the frontal, sagittal, and axial planes, resulting in a total of six axes. Both preoperative and latest followup radiographs were available for 17 of the 22 limbs. We obtained prior IRB approval for the study.
Key variables included the mechanical lateral distal femoral angle (mLDFA) and posterior distal femoral angle (PDFA) measured from standing radiographs of the knee to include the femur, according to Paley’s method [15]. Accuracy was measured with the radiographic angles either being brought to the normal range or not. The amount of limb lengthening was calculated. Complications were reviewed from medical charts. Safety was considered according to whether there were major complications that needed a secondary surgery. A CT version study of the femur was performed in cases with clinically obvious deformity to measure the amount of axial angulation (internal/external rotation of the femur). This is a simple method to evaluate the correct rotational profile objectively. It involves taking serial computed tomography cuts through the femoral neck and femoral condyles while the limb is held in position. The angle between femoral neck and the transverse axis of femoral condyles gives the correct rotation of femur. Distal referencing was utilized in the chronic operative mode. “Chronic operative mode” gave the ability to prebuild the frame before the surgery according to the preoperative radiograph planning, as opposed to other modes such as Total Residual where the frame could be applied in a “rings-first method.” It is a preference of the surgeon, not necessarily meaning one is better than the other. Two 2/3 rings were selected and applied with the opening of the frame facing posteriorly in the distal frame and medially in the proximal frame. Deformity parameters were measured and entered in the software program. Rotary frame angle of the reference (distal) frame was set as 60° externally rotated. The frame was applied to the leg with 6-mm hydroxyapatite-coated pins and a total residual program was run after the surgery.
In most cases, the patient was discharged between postoperative days 3 and 5 with instructions to start deformity correction on postoperative Day 7. Patients were allowed to either partially or fully weight bear using walking aids such as crutches and/or a walker. Physical therapy was initiated as an inpatient to teach range-of-motion exercises and was also continued in the outpatient setting 3 to 5 days a week as range-of-motion exercises initially and then to be followed by stretching and strengthening exercises.
Followup visits were scheduled weekly during the first month and then approximately every 2 weeks until correction was achieved. When tricortical consolidation was observed on anteroposterior and lateral radiographs, the frame was dynamized for 2 weeks. Fixator was removed and foot-flat weight bearing was allowed with assistive devices such as a walker and/or crutches.
Outcome measures in this study included time spent in frame (external fixation time), followup time, additional surgeries performed, mean length obtained during correction, complications, and mLDFA and PDFA radiographic angles. All outcome measures were collected from the medical charts and xrays of the patients obtained in the clinic or the office. The data were collected, the radiographs were measured, and the angles were recorded by two investigators (SM, JG) who were not primarily involved in the patients’ care.
Results
The mean time in the frame was 6.2 months (range, 2.6–19 months). The minimum length of followup from the date of initial surgery was 4.5 months (mean, 15.7 months; range, 4.5–35 months). Additional surgeries included three iliotibial band releases, one tibial TSF and tibial/fibular osteotomy, and one distal femoral epiphysiodesis to maintain the achieved correction in a 12-year-old with procurvatum after a motor vehicle injury. The frame was extended across the knee in three preoperatively unstable knees and one preoperatively stable knee that subluxated during the correction of an 8.5-cm limb-length inequality and a 40° valgus deformity. Peroneal nerve decompression was performed prophylactically in two limbs (one with 33° of valgus and 60° of procurvatum, and the other with 8.5-cm limb-length inequality and 40° of valgus).
For genu valgum, complete sets of radiographs were available for seven of the 10 limbs. The mean mLDFA was 73° (range, 48–84°) preoperatively and 88.9° (range, 85–95°) at latest followup. Given the normal value for mLDFA of 88° (range, 85–90°) [14], the amount of deformity (absolute difference from the normal mean mLDFA) was reduced from a mean of 15° (range, 4–40°) preoperatively to 2.1° (range, 1–7°) at latest followup (Table 1). One patient, who was lost to followup with the frame in place prior to correction, returned with a deformity with an mLDFA of 95°. When this patient was excluded, the followup mean mLDFA became 87.8° and the mLDFA for the remaining patients was within the normal range of 85° to 90°.
Table 1.
Preoperative and followup radiographic measurements
| Category | Preoperative | Latest followup |
|---|---|---|
| Mean (range) | Mean (range) | |
| Valgus (n = 7) | ||
| mLDFA | 73° (48–84°) | 88.9° (85–95°) |
| Amount of deformity* | 15° (4–40°) | 2.1° (1–7°) |
| Varus (n = 8) | ||
| mLDFA | 99.8° (91–112°) | 88.3° (87–90°) |
| Amount of deformity* | 11.9° (3–23°) | 1.5° (0–3°) |
| Procurvatum (n = 5) | ||
| PDFA | 60° (50–70°) | 83.8° (83–84°) |
| Amount of deformity† | 23° (13–33°) | 0.8° (0–1°) |
*Absolute difference from 88° as the mean normal mLDFA; †absolute difference from 83° as the mean normal PDFA.
For genu varum, complete sets of radiographs were available for eight of the nine limbs. The mean mLDFA was 99.8° (range, 91–112°) preoperatively and 88.3° (range, 87–90°) at latest followup. Given the normal value for mLDFA of 88° (range, 85–90°) [14], the amount of deformity (absolute difference from the normal mean mLDFA) was reduced from a mean of 11.9° (range, 3–23°) preoperatively to 1.5° (range, 0–3°) at latest followup (Table 1). Thus, all limbs with genu varum were corrected to within the normal range.
From the seven sagittal plane deformities, complete sets of radiographs were available for five limbs with procurvatum. The mean PDFA was 60° (range, 50–70°) preoperatively and 83.8° (range, 83–84°) at latest followup. The amount of procurvatum deformity (absolute difference from the normal PDFA value of 83°) was reduced from a mean of 23° (range, 13–33°) to 0.8° (range, 0–1°) (Table 1). Therefore, procurvatum was also corrected to within the normal range in these limbs.
Although it was noted that the radiographs were adequate for a subset of patients in a certain deformity group such as genu valgum, genu varum, or sagittal deformities, clinical information was collected in all. The complications presented in this study included those that occurred during the treatment of the patients even if they had inadequate radiographs.
A mean limb lengthening of 4.9 cm (range, 1.5–9 cm) was accomplished in eight femurs in seven of which the limb length discrepancy was a secondary concern. External fixation index for these limbs was 2.2 months/cm (range, 0.5–3.6 months/cm).
Complications included six pin tract infections (one required IV antibiotics and the others responded to oral antibiotics), four stiff knees that resolved with physical therapy, two delayed unions that underwent bone grafting, and one skin irritation. Two knees, which were stable preoperatively, had posterior subluxations. One was successfully treated by extending the frame to the tibia along with iliotibial band and hamstring releases, and the other by stopping the correction and providing physical therapy. No complications occurred in nine limbs of eight patients.
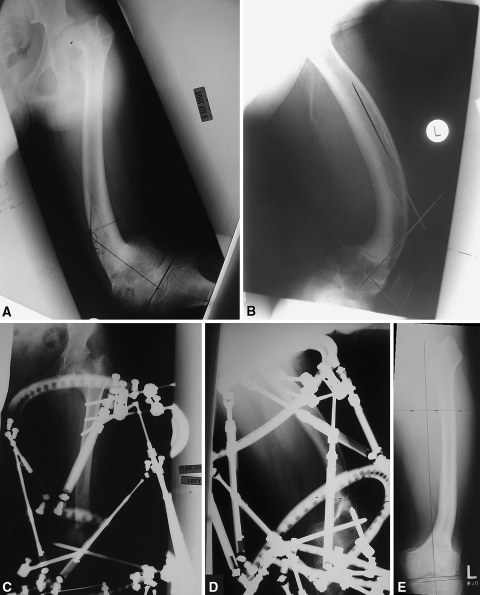
Successful correction of severe deformities was achieved gradually with the accuracy of the Taylor spatial frame using computer software. Preoperative front-to-back (Fig. 1A) and side-to-side (Fig. 1B) clinical views of a 16-year-old girl with severe genu valgum and procurvatum of the left distal femur were included along with a postoperative front-to-back clinical view (Fig. 1C) showing the alignment of lower extremities. Radiographically, an anteroposterior (Fig. 2A) and a lateral view (Fig. 2B) illustrate the deformity before the surgery. An anteroposterior (Fig. 2C) and a lateral radiograph view (Fig. 2D) show the correction phase after the application of external fixator. The final anteroposterior radiograph demonstrates the mechanical axis of the femur and the mLDFA angle being 90°, which is the normal angle (Fig. 2E).
Fig. 1A–C.
(A) Shown preoperatively here, a 16-year-old girl with congenital pseudohypoparathyroidism had an anteromedial bow of the left femur corrected with TSF. (B) The same patient is seen while standing (B) preoperatively and (C) at latest followup.
Fig. 2A–E.
(A) An AP radiograph of the left femur is shown preoperatively in the same patient. (B) A lateral radiograph of the left femur is presented preoperatively in the same patient. (C) An AP radiograph of the left femur shows the frame on the femur during correction in the same patient. (D) A lateral radiograph of the left femur shows the frame configuration during correction in the same patient. (E) An AP radiograph of the left femur reveals the correction of the mechanical axis at latest followup in the same patient.
Discussion
The Taylor spatial frame (TSF) has been used commonly in children and young adults, but more extensively in the tibia than in the femur. We investigated the use of the Taylor spatial frame for femoral deformity correction in children and young adults. The purposes of this study were (1) to gather the descriptive data on time spent in frame, mean followup time, and to describe the additionally performed surgeries; (2) to determine the accuracy of correction in different deformities (ie, genu valgum, genu varum, and sagittal plane deformities) by evaluating radiological outcome comparing the preoperative and postoperative measurements; (3) to assess how much limb lengthening was performed; (4) to determine the safety of the use of the TSF by reviewing the complications; and (5) to describe treatment modalities in femoral deformities in children and young adults.
There are several limitations to this study. The study is comprised of patients operated by four different surgeons at two centers over 7 years. This is mainly a chart review and data collection from radiographs and no functional questionnaires were obtained pre- and postoperatively. Twenty-two limbs of 20 patients were included. Due to the inadequacy of the radiographs 17 limbs of 15 patients were enrolled. This is a descriptive study. No statistical analysis was performed. Even within these limitations, this study describes a series of femoral deformities corrected with a single method. We were able to determine the effectiveness of the TSF and the obstacles encountered.
Femoral deformities may be corrected by several methods, including an osteotomy and internal fixation or an osteotomy and external fixation. An acute or gradual correction could be obtained with either a monolateral or a circular fixator. Feldman et al. [6] reported that gradual correction was more accurate than acute correction in the treatment of tibia vara. The Ilizarov circular external fixator uses multiple components, each designed to address specific planar deformities (translation, rotation, or angulation) to gradually correct limb deformities, even complex ones [8]. The Ilizarov device, despite its capabilities, requires extensive planning for building a frame to correct angulation, translation, and rotation simultaneously. Additionally, building the frame and making revisions to correct residual deformities are often difficult and labor intensive. In attempts to overcome these limitations of the Ilizarov device, Lin et al. [10] employed a computer software program and Seide et al. [17, 18] developed a new hexapod configuration with six distractors and 12 ball joints. The TSF is an alternative circular external fixator with rings, bolts, nuts, and attachments similar to those of the Ilizarov, but uses a hexapod-like arrangement of six telescopic struts and special universal joints for attaching the two rings together. The accompanying computer software provides the TSF with the advantage of permitting the gradual correction of a multiaxial deformity across all planes simultaneously and correction of any residual deformity without changing the mounted frame. Despite the common use of the TSF in deformity correction today, current literature primarily involves the use of the TSF in the tibia [1, 2, 5–7]. Femoral deformity correction previously has only been described as part of general lower extremity correction [3, 4, 19] or in case reports of adults [11, 12].
Our study resulted in a mean external fixation time of 6.2 months (range, 2.6–19 months). Eidelman et al. [3] reported the mean time in the frame as 3.1 months (range, 2–5 months). Sluga et al. [19] reported the mean external fixation time as 9.4 months (range, 5.4–12.1 months).
Our radiographic evaluation demonstrated the successful correction of multiplanar femoral deformities in 16 of 17 limbs in 14 of 15 patients. The only unacceptable correction was in a patient who failed to return for followup and had a varus deformity develop at the site of a fracture through the regenerate, which occurred while still in the frame. With the exception of that one case, both femoral deformity parameters (mLDFA and PDFA) corrected to within 3° of their normal mean values. The amount of deformity (absolute difference from the normal mean mLDFA) was reduced from a mean of 15° (range, 4–40°) preoperatively to 2.1° (range, 1–7°) at latest followup in genu valgum, and from a mean of 11.9° (range, 3–23°) preoperatively to 1.5° (range, 0–3°) at latest followup in genu varum. The amount of procurvatum deformity (absolute difference from the normal PDFA value of 83°) was reduced from a mean of 23° (range, 13–33°) to 0.8° (range, 0–1°) Of the five children treated with the TSF by Sluga et al. [19], the four with femoral deformities had a mean valgus correction of 9.75°, lateral translation correction of 7.5 mm, and lengthening of 6.9 cm. They reported excellent results for two patients but noted the other two would require further lengthenings. Fadel and Hosny [4] used the TSF in 22 patients for the correction of lower-limb deformities including lengthening in three patients with congenitally short femurs, and deformity correction and lengthening in one with a posttraumatic femoral fracture. Although the findings from this small subgroup of patients could not be isolated, the overall results were 18 excellent, two good, and two fair. In another study, 13 of 44 TSFs were applied to the femurs of pediatric patients to address angular deformities and limb-length inequalities [3]. The authors reported good results in these complex cases. In a novel application of the TSF for distal femoral deformities, Rogers et al. [16] achieved acute intraoperative correction initially using the TSF, stabilized the correction with internal fixation, and then removed the TSF during the same operation. Their early experience in seven patients, aged 17 to 63 years, indicated that the TSF was a useful adjunct tool in the correction of complex deformities.
A mean limb lengthening of 4.9 cm (range, 1.5–9 cm) was accomplished in eight femurs. External fixation index for these limbs was 2.2 months/cm (range, 0.5–3.6 months/cm). Eidelman et al. [3] reported in an angular deformity with shortening subgroup of their series a mean external fixation time of 14.1 weeks (range, 9–24 weeks) and a mean lengthening of 4 cm (range, 2.5–8 cm) with a resultant external fixation index of 0.9 month/cm.
In our series the most common complication was pin tract infection. All but one responded to oral antibiotics; one required intravenous antibiotics. Femoral application of an external fixator resulted in knee stiffness in four patients that resolved with physical therapy. The two patients with delayed unions underwent bone grafting, extending the external fixation time. The most significant complication was posterior subluxation of the knee joint in preoperatively stable knees. The two cases that had this complication were treated either with soft tissue releases and extending the frame to the tibia (one patient) or with just aggressive physical therapy (one patient). The potential risk for posterior subluxation of the knee exists with external fixators, and as we found, including the TSF. Although it is most often associated with the correction of a severe deformity, during a major lengthening, during simultaneous femoral and tibial lengthenings, and in inherently unstable knee joints, Jones and Moseley [9] reported posterior knee subluxations with as little as 2.5% of distraction. Additionally, subluxations can occur, as happened in two of our cases, in preoperatively stable knees. Close monitoring of the patients through frequent followup visits is the only way to avoid this complication. The main alerting symptoms are the insidious development of knee pain and loss of full knee extension, which should be evaluated with anteroposterior and lateral knee radiographs. If the knee is subluxated, one option is to stop the lengthening/correction and observe while providing physical therapy. Another option is to release the tethering musculature by releasing the hamstrings and iliotibial band. It is useful to cross the knee joint with the external fixators using rods attached to the partial/full ring and fix the proximal tibia through the ring using half pins/wires maintaining the reduced position of the knee joint. Eidelman et al. [3] reviewed their experience on the use of TSF in both tibia and femur. Complications included pin tract infections in two, fracture of the regenerated femur after frame removal in two, femoral fracture after a fall in one, delayed union in one, and residual femoral deformity in a patient with skeletal dysplasia. After experiencing three fractures, the authors suggested that removing the frame relying on radiographic evidence is inadequate for determining the extent of bone healing, and advocated dynamizing the frame to prevent fractures. One way of dynamizing a Taylor spatial frame is to replace the TSF struts with Ilizarov rods and loosen them to have dynamization. Another option could be either to back out the struts to obtain some compression or take out some wires and/or pins. The less wires/pins left in the bone, the more dynamized the frame would be. Another method could be to remove one of the struts, and allow the patient full weight-bearing on the frame. Since this will break the hexagonal construct and make the whole frame unstable, removing one or more struts of the TSF is subject to fractures if the bone is not healed enough. It does not act as the dynamization in Ilizarov devices or the monolateral external fixators which brace the regenerate while allowing the patient to fully weight bear. In our series we did not have any fractures related to early frame removal or dynamization. In the study by Sluga et al. [19], complications included pin tract infections, temporary knee stiffness, and pin breakage. Complications reported by Fadel and Hosny [4], not specific to the patients with femoral TSF, consisted of pin tract infections in all of the patients (12 required antibiotics), adjustment under anesthesia in six, frame loosening in three, early consolidation in three, fracture of the regenerate in two after premature removal of the fixator, and deep vein thrombosis in one. These authors additionally reported the patients had problems following the instructions of the TSF protocol.
Paley [13] described the problems, obstacles, and complications associated with the use of Ilizarov external fixators, especially during lengthening. Velazquez et al. [22] reviewed the complications they have experienced during deformity correction with Ilizarov external fixators and they have come to a conclusion that use of a circular transosseous fixation device did not appear to cause more complications compared to other methods. Theis et al. [21] also noted in their paper that the Ilizarov external fixator had a lower complication rate compared to the Wagner technique [23], which has an unacceptably high complication rate especially due to bone healing issues. Based on our results, we believe the TSF allows for the safe, gradual correction of the femoral deformity in children and young adults. It is accurate and well-tolerated, with a complication rate that is comparable to the Ilizarov external fixator. We now use the TSF as the first line of treatment of multiplanar femoral deformity in children and young adults.
Acknowledgments
We thank Jaime A. Gómez, MD, Matthew I. Stein, BS, and Harold J.P. van Bosse, MD, for their contributions to the study.
Footnotes
One of the authors (DSF) has received research support from Smith & Nephew, Inc. (Memphis, TN).
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with the ethical principles of research.
References
- 1.Al-Sayyad MJ. Taylor Spatial Frame in the treatment of pediatric and adolescent tibial shaft fractures. J Pediatr Orthop. 2006;26:164–170. [DOI] [PubMed]
- 2.Binski JC. Taylor Spatial Frame in acute fracture care. Techniques Orthop. 2002;17:173–184. [DOI]
- 3.Eidelman M, Bialik V, Katzman A. Correction of deformities in children using the Taylor Spatial Frame. J Pediatr Orthop B. 2006;15:387–395. [DOI] [PubMed]
- 4.Fadel M, Hosny G. The Taylor Spatial Frame for deformity correction in the lower limbs. Int Orthop. 2005;29:125–129. [DOI] [PMC free article] [PubMed]
- 5.Feldman DS, Madan SS, Koval KJ, van Bosse HJP, Bazzi J, Lehman WB. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop. 2003;23:387–391. [DOI] [PubMed]
- 6.Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop. 2006;26:794–798. [DOI] [PubMed]
- 7.Feldman DS, Shin SS, Madan S, Koval KJ. Correction of tibial malunion and nonunion with six-axis analysis deformity correction using the Taylor Spatial Frame. J Orthop Trauma. 2003;17:549–554. [DOI] [PubMed]
- 8.Ilizarov GA. The Apparatus: Components and Biomechanical Principles of Application. In: Transosseous Osteosynthesis. Berlin, Germany: Springer; 1992:63–120.
- 9.Jones DC, Moseley CF. Subluxation of the knee as a complication of femoral lengthening by the Wagner technique. J Bone Joint Surg Br. 1985;67:33–35. [DOI] [PubMed]
- 10.Lin H, Birch JG, Samchukov ML, Ashman RB. Computer assisted surgery planning for lower extremity deformity correction by the Ilizarov method. J Image Guid Surg. 1995;1:103–108. [DOI] [PubMed]
- 11.Nakase T, Ohzono K, Araki N, Hiroshima K. A case of Paget’s disease treated by distraction osteogenesis. Clin Orthop Relat Res. 2006;451:279–282. [DOI] [PubMed]
- 12.Nakase T, Ohzono K, Shimizu N, Yoshikawa H. Correction of severe post-traumatic deformities in the distal femur by distraction osteogenesis using Taylor Spatial Frame: a case report. Arch Orthop Trauma Surg. 2006;126:66–69. [DOI] [PubMed]
- 13.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed]
- 14.Paley D. Normal lower limb alignment and joint orientation. In: Paley D, ed. Principles of Deformity Correction. Berlin, Germany: Springer-Verlag; 2005:1.
- 15.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clinic North Am. 1994;25:425–465. [PubMed]
- 16.Rogers MJ, McFadyen I, Livingstone JA, Monsell F, Jackson M, Atkins RM. Computer hexapod assisted orthopaedic surgery (CHAOS) in the correction of long bone fracture and deformity. J Orthop Trauma. 2007;21:337–342. [DOI] [PubMed]
- 17.Seide K, Wolter D. Universal 3-dimensional correction and reposition with the ring fixator using the hexapod configuration [in German]. Unfallchirurg. 1996;99:422–424. [PubMed]
- 18.Seide K, Wolter D, Kortmann HR. Fracture reduction and deformity correction with the hexapod Ilizarov fixator. Clin Orthop Relat Res. 1999;363:186–195. [DOI] [PubMed]
- 19.Sluga M, Pfeiffer M, Kotz R, Nehrer S. Lower limb deformities in children: two-stage correction using the Taylor Spatial Frame. J Pediatr Orthop B. 2003;12:123–128. [DOI] [PubMed]
- 20.Spatialframe.com, Version 3.1™. Taylor Spatial Frame Web site. Available at: http://www.spatialframe.com. Accessed June 12, 2007.
- 21.Theis JC, Simpson H, Kenwright J. Correction of complex lower limb deformities by the Ilizarov technique: An audit of complications. J Orthop Surg (Hong Kong). 2000;8:67–71. [DOI] [PubMed]
- 22.Velazquez RJ, Bell DF, Armstrong PF, Babyn P, Tibshirani R. Complications of use of the Ilizarov technique in the correction of limb deformities in children. J Bone Joint Surg Am. 1993;75:1148–1156. [DOI] [PubMed]
- 23.Wagner H. Operative lengthening in the femur. Clin Orthop Relat Res. 1978;136:125–142. [PubMed]