Abstract
Hepatocyte growth factor (HGF) was initially identified in cultured hepatocytes and subsequently reported to induce angiogenic, morphogenic, and antiapoptotic activity in various tissues. These properties suggest a potential influence of HGF on bone healing. We asked if gene transfer of human HGF (hHGF) into an osteotomy gap with a hemagglutinating virus of Japan-envelope (HVJ-E) vector promotes bone healing in rabbits. HVJ-E that contained either hHGF or control plasmid was percutaneously injected into the osteotomy gap of rabbit tibias on Day 14. The osteotomy gap was evaluated by radiography, pQCT, mechanical tests, and histology at Week 8. The expression of hHGF was evaluated by reverse transcriptase–polymerase chain reaction and immunohistochemistry at Week 3. Radiography, pQCT, and histology suggested the hHGF group had faster fracture healing. Mechanical tests demonstrated the hHGF group had greater mechanical strength. The injected tissues at 3 weeks expressed hHGF mRNA by reverse transcriptase–polymerase chain reaction. hHGF-positive immunohistochemical staining was observed in various cells at the osteotomy gap at Week 3. The data suggest delivery of hHGF plasmid into the osteotomy gap promotes fracture repair, and HGF could become a novel agent for fracture treatment.
Introduction
The treatment of fractures has advanced rapidly in recent years. Various implants for treating fractures have been developed [3, 20]. However, complex fractures remain a challenge and often require prolonged fixation. External fixation is the method preferred by many surgeons to stabilize such fractures. However, external fixators are associated with nonunions, pin track infections, and contracture of adjacent joints, some of which relate to the length of the required immobilization.
More rapid bone repair within the fracture gap could minimize the complications that result from prolonged immobilization. Moreover, Einhorn [16] concluded enhancement of the fracture repair process would ensure rapid restoration of function. The ability of injured patients to return earlier to daily life would not only have a substantial economic impact on society, but would also improve the overall physical and mental well-being of the patients. Therefore, a compelling need still exists for a safe and effective way to enhance bone repair.
Many studies report enhancement of fracture healing with hormones or growth factors such as IGF-I [30], BMP [17, 29, 51], FGF-2 [4, 10, 42], VEGF [13], and PTH [2]. Recent reports suggest another growth factor, hepatocyte growth factor (HGF), functions as a powerful and versatile factors, such as angiogenetic, mitogenic, morphogenic, and antiapoptotic activity. HGF was originally identified from plasma and serum as a molecule that simulated DNA synthesis in rat and human hepatocytes in 1989 [36, 37]. Multiple studies subsequently confirmed the role of HGF in enhancing hepatocyte function [21, 25, 27, 28, 39, 45, 47, 49, 50, 52]. Given that many growth factors influence various tissues, the question arises as to whether HGF influences bone healing.
We therefore hypothesized gene transfer of human HGF (hHGF) directly into osteotomy gaps using the hemagglutinating virus of Japan-envelope (HVJ-E) vector would promote tibia fracture healing on radiographs, computer tomography, mechanical tests, and histology in rabbits. Furthermore, we tested the mRNA and protein expression of hHGF to prove the effect of the injected gene.
Materials and Methods
In a preliminary study, we delivered high hHGF concentrations percutaneously and therefore less invasively than an open method to rabbit tibia osteotomy gaps. We used a novel, nonviral vector, the HVJ-E, to deliver hHGF genes to osteotomy gaps. The HVJ-E vector is effective for gene transfer both in vitro and in vivo [26]. Fractures were simulated by an osteotomy with a gap in 50 mature female Japanese white rabbits weighing 2.5 to 3 kg. The rabbits were equally divided into two groups of 25 rabbits each, the hHGF group and the control vector group. Human HGF cDNA (2.2 kb) was inserted between the EcoRI and NotI gaps of the pUC-Sr expression vector plasmid to produce an hHGF expression vector. A pcDNA 3.1(-) plasmid DNA vector (Invitrogen, San Diego, CA) with the same structure, but lacking the hHGF cDNA, was used as a control vector. On Day 7 after injection of HVJ-E, three rabbits in each group were assessed for hHGF mRNA. At 3 and 8 weeks postoperatively, two animals from each group were euthanized for immunohistochemistry. At 8 weeks, the remaining 40 animals were euthanized and equal numbers used for histologic and mechanical testing. The experimental protocol was approved by the Committee on the Ethics of Animal Experiments of Kanazawa University.
HVJ (also known as Sendai virus) envelope vector was prepared as described previously [26]. Briefly, the virus was purified by centrifugation and inactivated by ultraviolet irradiation, which disabled the replication capacity of the virus completely without affecting the cell membrane fusing capability of the envelope. HVJ envelope (5 AU) was mixed with 50 μg of either HGF or pcDNA3.1(-) plasmid DNA and 0.3% Triton-X 100. The suspension was then washed with balanced salt solution (137 mM NaCl, 5.4 mM KCl, 10 mM Tris-HCl; pH 7.6) and centrifuged (10,000 g, 10 minutes) at 4°C, and the pellet was resuspended in a final volume of 100 μL balanced salt solution for subcutaneous injection. The suspension was stored at 4°C until use. HVJ-E vector is commercially available from Ishihara Sangyo Co Ltd (Osaka, Japan).
The rabbits were anesthetized with a subcutaneous injection of ketamine hydrochloride (35 mg/kg body weight; Sankyo Pharmaceutical, Tokyo, Japan), xylazine (5 mg/kg body weight; Bayer, Tokyo, Japan), and an intravenous injection of pentobarbital sodium (40–50 mg/kg body weight; Abbott Laboratories, North Chicago, IL). A longitudinal skin incision was made on the anteromedial aspect of the right tibia, and the periosteum was carefully stripped of the surrounding soft tissue and fascia. Four half pins 2 mm in diameter (Stryker, Geneva, Switzerland) were inserted into the medial aspect of the tibia, perpendicular to its axis, and a unilateral external fixator of our design was applied. To simulate a fracture of the rabbit tibia [33, 40, 41], we created a 3-mm gap between the bone fragments with a bone saw.
At postoperative Week 2, after induction of anesthesia with ketamine and xylazine, HVJ-E (100 μL) containing either hHGF or pcDNA 3.1(-) plasmid DNA (n = 25 for each group) was percutaneously injected into the osteotomy gap with a 29-gauge needle (Terumo, Atsugi, Japan) under an image intensifier. The reason we chose postoperative Week 2 was that many new cells existed at the osteotomy gap. Injected gene could be introduced into them.
On Day 7 after percutaneous injection of HVJ-E containing either hHGF or pcDNA 3.1 (-) plasmid DNA (n = 3 for each group), the rabbits were euthanized and the tissue at the osteotomy gap and the surrounding muscle was harvested and prepared for reverse transcription–polymerase chain reaction (RT-PCR) to detect hHGF mRNA. The reason why we chose 7 days after delivery was the maximum amount of mRNA from the introduced gene peaked at 5 to 7 days after the injection. Total RNA was isolated using acid guanidinium thiocyanate-phenol-chloroform and ethanol precipitation. RT-PCR was performed using an amplification reagent kit (TaqMan EZRT-PCR kit; Applied Biosystems, Alameda, CA) with primers specific for hHGF and rabbit GAPDH. The primer pairs for hHGF (sense primer, 5′-ACCCAAGCTGGCTAGCGT-3′; antisense primer, 5′-AGTGCTGGATCTATTTTGATTAGG-3′) and rabbit GAPDH (sense primer, 5′-GCGCCTGGTCACCAGGGCTGCTT-3′; antisense primer, 5′-TGCCGAAGTGGTCGTGGATGACCT-3′) [44] were used to amplify hHGF and rabbit GAPDH. PCR reactions of 40 cycles with annealing temperature of 62°C for 1 minute for hHGF and 26 cycles with annealing temperature 63°C for 1 minute for rabbit GAPDH were performed. The PCR products (hHGF, 260 bp; GAPDH, 465 bp) were separated by electrophoresis in a 3% agarose gel and stained with ethidium bromide.
At postoperative Weeks 3 (for the confirmation of the protein expression) and 8 (for the period of the protein expression), two tibias, respectively, from each group were used for immunohistochemistry. Paraffin sections were treated with anti-hHGF monoclonal antibody (R&D Systems Inc, Minneapolis, MN; dilution 1:100), and peroxidase-conjugated goat antimouse immunoglobulin (EnVision; DAKO, Carpinteria, CA) was used as the secondary antibody. To develop the color, a DAB kit (EnVision; DAKO) was used. The sections were counterstained with Mayer’s hematoxylin.
To monitor bone formation, we compared the various parameters of healing of osteotomy gaps of the hHGF group with those of the control vector group by radiography at each postoperative time point (Fig. 1A–B). The osteotomy gap was evaluated by comparing bone density of the hHGF and control groups (n = 20 for each group) on anteroposterior and medial-lateral radiographs with an aluminum step wedge (10 steps, 1 mm/step) on the same film. Radiographs were obtained weekly under anesthesia for 8 weeks after the operation. We (HT) evaluated the quantity of callus over the entire 3-mm gap between the proximal and distal native bone using Scion Image Beta-3b software for Windows (Scion Corporation, Frederick, MD). Briefly, the bone density of the gap was measured by interpreting the entire image in units of thickness of the aluminum plate by comparing it with the gradient of luminosity obtained from the aluminum wedge. The bone density is reported in units of aluminum thickness (mm Al).
Fig. 1A–B.
(A) A series of anteroposterior radiographs taken of the human hepatocyte growth factor (hHGF) group (H) and control groups (C) from each single animal show faster callus formation at the 3-mm gap in the hHGF group. (B) A series of mediolateral radiographs taken of the hHGF group (H) and control groups (C) from each single animal show faster remodeling at the 3-mm gap in the hHGF group.
For the quantitative evaluation of the healing process, 10 rabbits in each group were euthanized by an intravenous dose of sodium pentobarbital 8 weeks after surgery after the soft tissues were dissected from the tibia and the external fixator was removed. The tibias were stored in gauze soaked in 0.9% saline solution at −20°C and thawed at room temperature before pQCT and mechanical analysis. A quantitative determination of callus development was performed with pQCT (XCT-Research SA+; Stratec, Pforzheim, Germany). A 3-mm gap bone section was analyzed with three consecutive transverse pQCT scans 0.77 mm thick, 2.5 mm apart, and with a pixel size of 0.1 × 0.1 mm. The XCT Series software package (Rev 6.00B; Stratec, Pforzheim, Germany) was used to calculate the mineral content (mg/mm), mineralized callus area (mm2), and bone mineral density (mg/cm3) at the gap level. To assess progression of remodeling, areas of higher bone density (greater than 690 mg/cm3) within the callus were measured and separated from areas of low mineral density. The mineral content and the area of this high mineral density callus were calculated. The threshold of 690 mg/cm3 was selected because it corresponds to the lower level of cortical bone. Furthermore, electronic sections through the long axis of each tibia were created on three-dimensional reconstructed images.
Both tibiae of each rabbit were mechanically tested using an electromechanical testing machine (model MZ-500D; Maruto Machine, Inc, Tokyo, Japan). A three-point bending test was performed at a rate of 2.5 mm per minute with 100 kgf of weight axial load. The central loading point was adjusted toward the osteotomy gap. The lower loading points were separated 30 mm from each other. Failure load values and load displacement curves were obtained for all samples. The stiffness of each unilateral tibia was calculated as the slope of the linear segment on the load displacement curve. Mechanical data ratios of the mechanical data of the fractured unilateral tibia to the intact tibia (percent failure load and percent stiffness) were calculated.
Ten rabbits in each group were euthanized 8 weeks after surgery, and the histology of the osteotomy gap was studied. Heparinized physiological saline was perfused through both femoral arteries followed by perfusion with 4% paraformaldehyde solution in a phosphate buffer (pH 7.4). The tibias were fixed for 24 hours in the same solution. The tibias were then decalcified with 10% EDTA solution and embedded in paraffin. The specimens were sectioned at a 5-μm thickness parallel to the bone axis and stained with hematoxylin and eosin.
Differences in the bone density, mineral contents, mineralized area, bone mineral density, failure load, and stiffness between the control vector group and the HGF group were determined by Student’s t test.
Results
The administration of HVJ-E/hHGF or HVJ-E/pcDNA to the rabbits produced no obvious adverse effects such as sudden death or abnormal weight loss during the 8 weeks of the experiment.
In radiographs, bony callus appeared on the lateral side at postoperative Week 2 in the control vector group and bridged the osteotomy gap at postoperative Week 3. After 3 weeks, the size of the bridging callus was reduced and the callus became gradually calcified at the osteotomy gap. At postoperative Week 8, however, corticalization was not sufficient to complete remodeling. The hHGF group demonstrated a similar course as the control vector group until postoperative Week 3. After that time point, the callus at the osteotomy gap became calcified to a greater extent and more rapidly than that of the control vector group. Furthermore, remodeling, especially corticalization and formation of the medullary canal, progressed in the hHGF group. At postoperative Week 8, remodeling in the hHGF group was complete, and the osteotomy gap looked homogeneous when compared with the host bone.
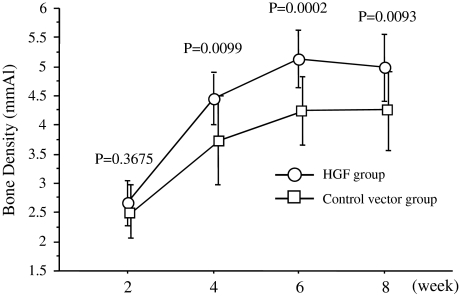
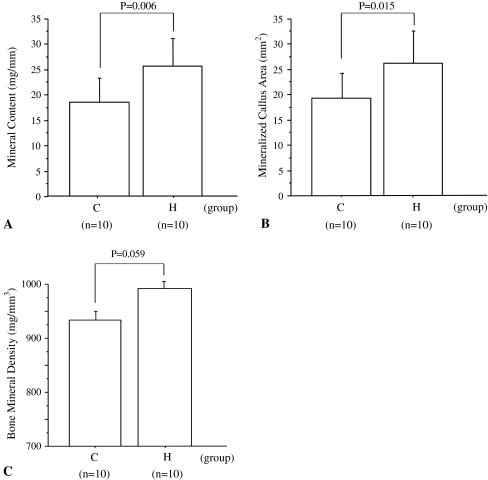
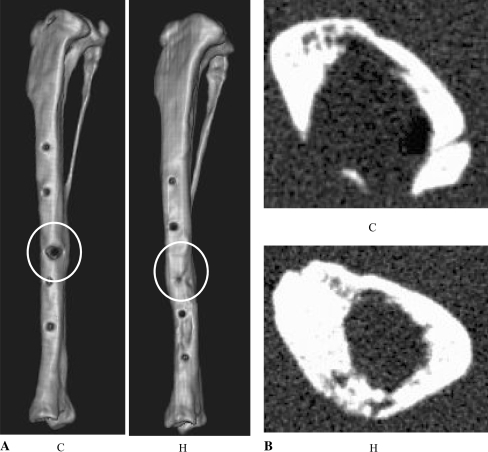
The bone density in the hHGF group was greater compared with the control vector group at postoperative Weeks 4 to 8 (Week 2, p = 0.3675; Week 4, p = 0.0099; Week 6, p = 0.0002; Week 8, p = 0.0093) (Table 1; Fig. 2). Mineral content in the hHGF group was greater (p = 0.006) at postoperative Week 8 compared with the control vector group (control vector group, 18.7 ± 4.7 mg/mm; hHGF group, 25.7 ± 5.4 mg/mm) (Fig. 3A). Mineralized callus area in the hHGF group was also greater (p = 0.015) at postoperative Week 8 compared with the control vector group (control vector group, 19.4 ± 4.9 mm2; hHGF group, 26.2 ± 6.4 mm2) (Fig. 3B). In addition, bone mineral density in the hHGF group was not different (p = 0.059) at postoperative Week 8 compared to the density in the control vector group (control vector group, 933.5 ± 67.3 mg/cm3; hHGF group, 987.7 ± 52.7 mg/cm3) (Fig. 3C). Three-dimensional computed tomographic reconstructed images and axial images of specimens obtained 8 weeks after surgery were created (Fig. 4A–B). The osteotomy gaps in the control vector specimen were not bridged completely with a partial defect of the cortical bone. However, no gap was observed in the osteotomy gap of the hHGF group (Fig. 4A). On the axial view, the osteotomy gaps in the hHGF group had a circular, thick cortical bone. In contrast, the cortex in the control vector group had a partial defect of circular cortical bone (Fig. 4B).
Table 1.
Bone density in the control vector group versus the hHGF group
| Group | Time point (weeks) | Bone density (mm Al) | p value |
|---|---|---|---|
| Control vector | 2 | 2.5 ± 0.5 | > 0.05 |
| 4 | 3.7 ± 0.7 | < 0.01 | |
| 6 | 4.2 ± 0.6 | < 0.01 | |
| 8 | 4.3 ± 0.7 | < 0.01 | |
| hHGF | 2 | 2.7 ± 0.4 | > 0.05 |
| 4 | 4.4 ± 0.4 | < 0.01 | |
| 6 | 5.1 ± 0.5 | < 0.01 | |
| 8 | 5 ± 0.6 | < 0.01 |
hHGF = human hepatocyte growth factor.
Fig. 2.
The HGF group had higher bone density in the 3-mm gap than the control vector group. The results of the bone density are given in units of aluminum thickness.
Fig. 3A–C.
(A) At postoperative Week 8, the mineral content (mean ± standard deviation [SD]) was higher in the human hepatocyte growth factor (hHGF) group (H) than in the control vector group (C). (B) Mineralized callus area at postoperative Week 8 (mean ± SD) was higher in the hHGF group (H) than in the control vector group (C). (C) Bone mineral density 8 weeks after the operation (mean ± SD) in the hHGF group was similar (p = 0.059) to that in the control vector group (C).
Fig. 4A–B.
(A) A reconstruction image of the whole tibia at postoperative Week 8 shows complete bridging in the human hepatocyte growth factor (hHGF) group (H), but not in the control vector group (C) with a partial defect in cortical bone. (B) An axial image at the gap level 8 weeks after the operation shows thick, circular cortical bone in the hHGF group (H), but not in the control vector group (C) with a partial defect of cortical bone.
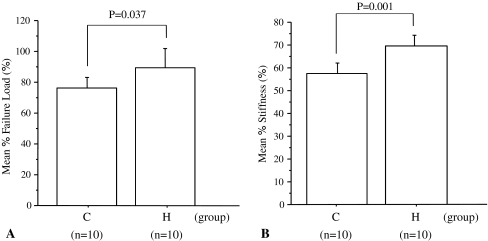
The mean ratio of failure loads of the hHGF group was greater (p = 0.037) than that of the control vector group (89.4% ± 17.5% versus 76.3% ± 9.1%, respectively) (Fig. 5A). The hHGF-treated tibiae were relatively stiffer (p = 0.001) than those of the control group when both were compared with their contralateral controls (69.7% ± 6.5% versus 57.5% ± 6.3%) (Fig. 5B).
Fig. 5A–B.
(A) Mean percentage of failure load at postoperative Week 8 (mean ± standard deviation [SD]) was higher in the human hepatocyte growth factor (hHGF) group (H) than in the control vector group (C). (B) Mean percentage stiffness at postoperative Week 8 (mean ± SD) was stronger in the hHGF group (H) than in the control vector group (C).
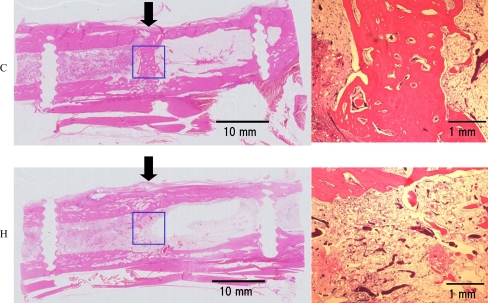
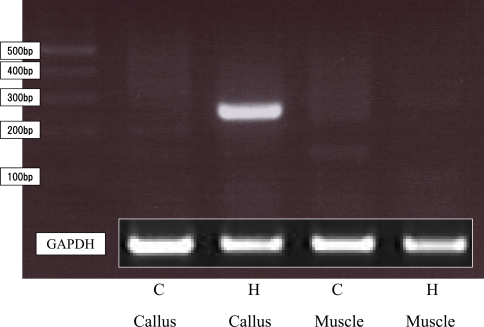
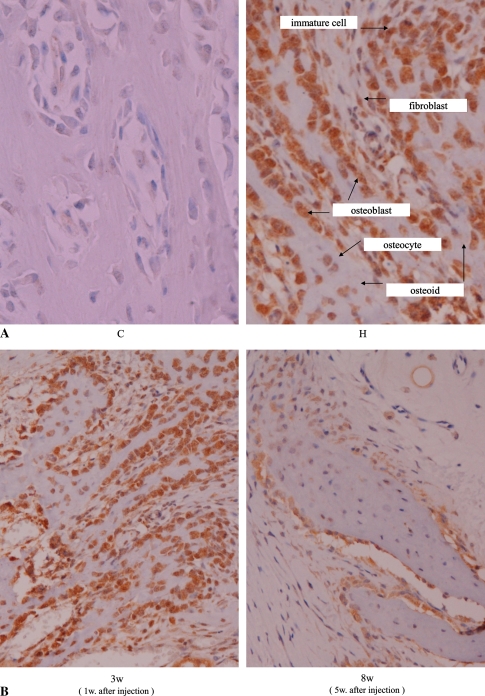
At postoperative Week 8 in the hHGF group, the osteotomy gaps were completely remodeled with a firm cortex and a reconstructed medullary canal almost identical to that of normal bone. In contrast, a medullary canal was not observed in the control vector group. In place of a medullary canal, mature cartilage and new trabecular bone were present in the middle of the osteotomy gap, which was not remodeled sufficiently (Fig. 6). In RT-PCR, expression of hHGF mRNA was detected only in the callus of the hHGF group and in the surrounding muscle of neither group (Fig. 7). Thus, HVJ-E/hHGF was transfected locally into the osteotomy gap sufficiently to express mRNA. By immunohistochemistry, we observed expression of hHGF in immature cells, fibroblasts, osteoblasts, and osteocytes (Fig. 8A). No immunohistochemical staining was observed in the surrounding muscle of the hHGF group. No hHGF-positive cells were observed in specimens from the control vector group. This indicates the HVJ-E/hHGF was transfected locally into the osteotomy gap at the level of protein. Human HGF expression was still observed at this time point; however, when expression at 8 weeks was compared with that at 3 weeks, hHGF protein decreased by the end point of treatment (Fig. 8B).
Fig. 6.
Representative longitudinal histologic sections of the 3-mm gap at postoperative Week 8 are shown. The arrows indicate the original 3-mm defect region (top row). Magnified histology of the 3-mm gap (bottom row). The gap in the control vector group (C) had a trabecular bone in the middle of the osteotomy gap, meanwhile in the human hepatocyte growth factor group (H), a firm cortex and a reconstructed medullary canal were observed (Stain, hematoxylin and eosin; original magnification, ×1 for left side and ×40 for right side).
Fig. 7.
Reverse transcriptase–polymerase chain reaction analysis demonstrated the expression of human hepatocyte growth factor (hHGF) mRNA in the injected callus and the surrounding muscle of both groups. hHGF mRNA was specifically detected in the callus of the hHGF group (H), but was not detected in the callus and muscle of the control vector group or in muscle of the hHGF group.
Fig. 8A–B.
(A) Immunohistochemistry of human hepatocyte growth factor (hHGF) at the osteotomy gap at postoperative Week 3 (1 week after the injection of plasmid) (Stain, immunohistochemistry of hHGF; original magnification, ×400). In the hHGF group (H), hHGF expression was markedly observed in immature cells, fibroblasts, osteoblasts, and osteocytes. No immunohistochemical staining was observed in specimens from the control vector group (C). (B) Immunohistochemistry of hHGF of the osteotomy gap at postoperative Week 3 or 8 (1 and 5 weeks after the injection of plasmid) (Stain, immunohistochemistry of hHGF; original magnification, ×400). hHGF expression was still observed at postoperative Week 8; however, it decreased compared with that of postoperative Week 3.
Discussion
HGF was originally identified from rat and human hepatocyte. Multiple studies subsequently confirmed the role of HGF in enhancing hepatocyte function. After that, HGF was recognized as a powerful and versatile factor with angiogenesis, mitogen, morphogen, and antiapoptotic activity in various tissues. The question arose as to whether HGF influences bone healing. We therefore hypothesized gene transfer of hHGF directly into osteotomy gaps would promote bone healing in the rabbit.
We note several limitations. First, we followed the repair process only 8 weeks. Although this time period was chosen because the control model showed bone union and corticalization on radiographs at postoperative Week 8, our mechanical test data did not reach that of the intact bones. Different results may occur at later stages of healing. However, this study demonstrates bone healing differences resulting from HGF, especially at an early stage. Second, we did not confirm the duration of hHGF gene expression. Because in a clinical setting gene therapy always accompanies the problem of its safety, we should ascertain its safety until at least the end of expression. We gave priority to economic and practical reasons. Third, the gap size was not critical (i.e., nonunion would develop without treatment). Although the osteotomy model is not a fracture the healing process of both models was the same [33, 40, 41].
Our data suggest percutaneous injection of HVJ-E/hHGF into tibial osteotomy gaps effectively promotes bone repair. Consequently, the treatment time for fractures could be shortened when the hHGF gene is administered during the early stages of fracture repair. These data indicate the high potential of hHGF gene therapy using the HVJ-E vectors for treatment of bone fractures.
Some osteogenetic factors have been used as therapeutic molecules for fracture healing and promote fracture repair. HGF, however, has not been used for this purpose to date. Many papers have been published describing therapeutic uses of HGF for various diseases such as limb ischemia [28, 49, 50], myocardial ischemia [5], brain ischemia [47, 52], hearing impairment [39], nerve injury [27], and spinal cord injury [45]. Notably, HGF plasmid delivery for peripheral limb ischemia is now in clinical trials [34].
HGF along with vitamin D promote growth and differentiation of human mesenchymal cells into osteogenic cells [12]. HGF also enhances osteoblast differentiation in vitro [22]. Further, HGF reportedly contributes to fracture repair by inducing the expression of BMP receptors during the early phase of fracture repair [24]. Our data support previous data suggesting the use of HGF for fracture repair will induce expression of BMPR, which will differentiate mesenchymal cells into osteoblasts and osteoblasts into ossification. Based on these observations, the use of HGF together with other factors such as BMP or vitamin D could enhance fracture healing more rapidly.
Gene delivery to bone has been accomplished by several vectors, including adenovirus, retrovirus, adenoassociated virus, lentivirus, and herpes simplex virus. In this study, we used the HVJ-E vector system as the delivery method for bone osteotomy gaps. HVJ-E is a novel vector system that converts inactivated HVJ into a gene transfer vector by introducing plasmid DNA directly into inactivated HVJ particles after treatment with a mild detergent and centrifugation in the presence of plasmid DNA [26]. Previous studies demonstrated the successful delivery of DNA to cultured cells and animal tissues such as the inner ear [39], liver, skin, uterus, lung, eye, tumor tissues [26], and brain [46]. HVJ-E is a nonviral vector that is generally less efficient than other viral delivery vehicles. However, it is inexpensive, safe, nonimmunogenic, and easy to handle [19].
In principle, gene delivery is performed in two ways, in vivo or ex vivo [8, 9, 14]. In vivo gene delivery is a direct approach, in which the vector is injected directly into the specified target tissue. Ex vivo is an indirect approach, in which the therapeutic gene is delivered outside the body to various cells grown in culture before implantation into the body. In vivo gene delivery involves directly delivering the gene into a specific anatomic gap. The advantages of this method are that it is a simple technique favoring its transfer into a clinical application and that it has the potential for lower costs. The disadvantages are the difficulties in targeting specific cells for transduction and in achieving high transduction efficiency [14]. Ex vivo gene transfer is considered safer because transfected cells are introduced into the body, and safety tests are possible before introduction. However, it is technically more complex and more expensive.
We used gene delivery rather than protein delivery. Gene therapy has potential advantages over protein delivery as a result of (1) long-term expression of the protein from the delivered gene; (2) high local concentration of protein expression; (3) low manufacturing cost; (4) reduced systemic effects; and (5) longer shelf life and easier storage of vectors [31, 32, 38, 48]. Ido et al. [23] reported recombinant hHGF administered intravenously was rapidly decreased in serum with a short half-life of 2.4 minutes. We detected expression of hHGF 6 weeks after the injection of plasmid. Therefore, gene transfer of HGF plasmid is expected to generate much longer expression of HGF than direct administration of HGF protein. Yoshimura et al. [52] also demonstrated gene transfer of HGF plasmid markedly increased cerebral blood flow in the ischemic brain, whereas a single injection of recombinant HGF failed to do so.
Multiple studies relate to gene therapy for bone defects and fractures [6–8, 15, 18, 43]. However, therapeutic gene therapy for bone regeneration with a nonviral vector has never been demonstrated. Egermann et al. [15] reported inflammation resulting from an immune reaction to adenovirus vectors caused severe retardation of bone formation. Similar results occurred with injection of Ad-BMP-2 into muscles of immunocompetent rats, causing poor bone formation and an inflammatory response at the injection gap [1].
Furthermore, a small number of studies address direct percutaneous injection of a gene to a fracture gap [7, 8, 43]. Gene transfer by direct percutaneous injection leading to endogenous bioactive protein expression offers the potential advantage of simple direct delivery without the requirement for a carrier or surgery and could be used to treat closed fractures in clinical cases. Rundle et al. [43] also performed percutaneous injection of the BMP-4 gene with a retroviral vector into the subperiosteum, which required the deposit of all vector within the periosteum while avoiding the muscle. Therefore, it was technically difficult and not practical. Percutaneous injections of gene to muscle are widely used to promote bone repair resulting from the high efficiency and ease of transfection and longer duration of gene expression [1, 11, 35]. With intramuscular injections, however, the area of gene expression is uncertain, which raises questions about the effect of gene expression at the fracture gap. Furthermore, the immune response differs between intraosseous and intramuscular gaps, because the muscle has a stronger immunologic reaction [6].
Our preliminary data suggest HGF promotes fracture healing in rabbit tibia and in vivo gene therapy using HVJ-E/hHGF effectively enhances bone formation in fracture healing. Use of these methods could shorten treatment time, resulting in improved physical and mental well-being of patients. In the future, the safety evaluation of this gene therapy technique and the mechanisms whereby HGF promotes bone healing should be assessed further.
Acknowledgments
We thank Yoh Zen, MD, PhD, Department of Pathology, Kanazawa University, for assistance in the histologic examination. Anges MG Inc (Tokyo, Japan) kindly supplied the hHGF expression vector.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the animal protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Alden TD, Pittman DD, Hankins GR, Beres EJ, Engh JA, Das S, Hudson SB, Kerns KM, Kallmes DF, Helm GA. In vivo endochondral bone formation using a bone morphogenetic protein 2 adenoviral vector. Hum Gene Ther. 1999;10:2245–2253. [DOI] [PubMed]
- 2.Alkhiary YM, Gerstenfeld LC, Krall E, Westmore M, Sato M, Mitlak BH, Einhorn TA. Enhancement of experimental fracture-healing by systemic administration of recombinant human parathyroid hormone (PTH 1–34). J Bone Joint Surg Am. 2005;87:731–741. [DOI] [PubMed]
- 3.Al-Sayyad MJ. Taylor Spatial Frame in the treatment of pediatric and adolescent tibial shaft fractures. J Pediatr Orthop. 2006;26:164–170. [DOI] [PubMed]
- 4.Aoyama I, Anzai J, Nakamura T, Hiyama Y, Tamura M. Acceleration of fracture healing in nonhuman primates by fibroblast growth factor-2. J Clin Endocrinol Metab. 2001;86:875–880. [DOI] [PubMed]
- 5.Azuma J, Taniyama Y, Takeya Y, Iekushi K, Aoki M, Dosaka N, Matsumoto K, Nakamura T, Ogihara T, Morishita R. Angiogenic and antifibrotic actions of hepatocyte growth factor improve cardiac dysfunction in porcine ischemic cardiomyopathy. Gene Ther. 2006;13:1206–1213. [DOI] [PubMed]
- 6.Baltzer AW, Lattermann C, Whalen JD, Ghivizzani S, Wooley P, Krauspe R, Robbins PD, Evans CH. Potential role of direct adenoviral gene transfer in enhancing fracture repair. Clin Orthop Relat Res. 2000;379:S120–125. [DOI] [PubMed]
- 7.Bertone AL, Pittman DD, Bouxsein ML, Li J, Clancy B, Seeherman HJ. Adenoviral-mediated transfer of human BMP-6 gene accelerates healing in a rabbit ulnar osteotomy model. J Orthop Res. 2004;22:1261–1270. [DOI] [PubMed]
- 8.Betz OB, Betz VM, Nazarian A, Pilapil CG, Vrahas MS, Bouxsein ML, Gerstenfeld LC, Einhorn TA, Evans CH. Direct percutaneous gene delivery to enhance healing of segmental bone defect. J Bone Joint Surg Am. 2006;88:355–365. [DOI] [PubMed]
- 9.Blanquaert F, Delany AM, Canalis E. Fibroblast growth factor-2 induces hepatocyte growth factor/scatter factor expression in osteoblasts. Endocrinology. 1999;140:1069–1074. [DOI] [PubMed]
- 10.Chen WJ, Jingushi S, Aoyama I, Anzai J, Hirata G, Tamura M, Iwamoto Y. Effects of FGF-2 on metaphyseal fracture repair in rabbit tibiae. J Bone Miner Metab. 2004;22:303–309. [DOI] [PubMed]
- 11.Chen Y, Cheung KM, Kung HF, Leong JC, Lu WW, Luk KD. In vivo new bone formation by direct transfer of adenoviral-mediated bone morphogenetic protein-4 gene. Biochem Biophys Res Commun. 2002;298:121–127. [DOI] [PubMed]
- 12.D’Ippolito G, Schiller PC, Perez-stable C, Balkan W, Roos BA, Howard GA. Cooperative actions of hepatocyte growth factor and 1,25-dihydroxyvitamin D3 in osteoblastic differentiation of human vertebral bone marrow stromal cell. Bone. 2002;31:269–275. [DOI] [PubMed]
- 13.Eckardt H, Ding M, Lind M, Hansen ES, Christensen KS, Hvid I. Recombinant human vascular endothelial growth factor enhances bone healing in an experimental nonunion model. J Bone Joint Surg Br. 2005;87:1434–1438. [DOI] [PubMed]
- 14.Egermann M, Goldhahn J, Schneider E. Animal models for fracture treatment in osteoporosis. Osteoporos Int. 2005;16:S129–138. [DOI] [PubMed]
- 15.Egermann M, Lill CA, Griesbeck K, Evans CH, Robbins PD, Schneider E, Baltzer AW. Effect of BMP-2 gene transfer on bone healing in sheep. Gene Ther. 2006;13:1290–1299. [DOI] [PubMed]
- 16.Einhorn TA. Enhancement of fracture-healing. J Bone Joint Surg Am. 1995;77:940–956. [DOI] [PubMed]
- 17.Einhorn TA, Majeska RJ, Mohaideen A, Kagel EM, Bouxsein ML, Turek TJ, Wozney JM. A single percutaneous injection of recombinant human bone morphogenetic protein-2 accelerates fracture repair. J Bone Joint Surg Am. 2003;85:1425–1435. [DOI] [PubMed]
- 18.Franceschi RT, Yang S, Rutherford RB, Krebsbach PH, Zhao M, Wang D. Gene therapy approaches for bone regeneration. Cells Tissues Organs. 2004;176:95–108. [DOI] [PMC free article] [PubMed]
- 19.Giannoudis PV, Tzioupis CC, Tsiridis E. Gene therapy in orthopaedics. Injury. 2006;37:S30–40. [DOI] [PubMed]
- 20.Greiwe RM, Archdeacon MT. Locking plate technology: current concepts. J Knee Surg. 2007;20:50–55. [DOI] [PubMed]
- 21.Hirano S, Bless DM, Rousseau B, Welham N, Montequin D, Chan RW, Ford CN. Prevention of vocal fold scarring by topical injection of hepatocyte growth factor in a rabbit model. Laryngoscope. 2004;114:548–556. [DOI] [PubMed]
- 22.Hossain M, Irwin R, Baumann MJ, McCabe LR. Hepatocyte growth factor (HGF) adsorption kinetics and enhancement of osteoblast differentiation on hydroxyapatite surfaces. Biomaterials. 2005;26:2595–2602. [DOI] [PubMed]
- 23.Ido A, Moriuchi A, Kim I, Numata M, Nagata Y, Hasuike S, Uto H, Tsubouchi H. Pharmacokinetic study of recombinant human hepatocyte growth factor administered in a bolus intravenously or via portal vein. Hepatology Research. 2004;30:175–181. [DOI] [PubMed]
- 24.Imai Y, Terai H, Nomura-Furuwatari C, Mizuno S, Matsumoto K, Nakamura T, Takaoka K. Hepatocyte growth factor contributes to fracture repair by upregulating the expression of BMP receptors. J Bone Miner Res. 2005;20:1723–1730. [DOI] [PubMed]
- 25.Jin M, Chen Y, He S, Ryan SJ, Hinton DR. Hepatocyte growth factor and its role in the pathogenesis of retinal detachment. Invest Ophthalmol Vis Sci. 2004;45:323–329. [DOI] [PubMed]
- 26.Kaneda Y, Nakajima T, Nishikawa T, Yamamoto S, Ikegami H, Suzuki N, Nakamura H, Morishita R, Kotani H. Hemagglutinating virus of Japan (HVJ) envelope vector as a versatile gene delivery system. Mol Ther. 2002;6:219–226. [DOI] [PubMed]
- 27.Kato N, Nemoto K, Nakanishi K, Morishita R, Kaneda Y, Uenoyama M, Ikeda T, Fujikawa K. Nonviral HVJ (hemagglutinating virus of Japan) liposome-mediated retrograde gene transfer of human hepatocyte growth factor into rat nervous system promotes functional and histological recovery of the crushed nerve. Neurosci Res. 2005;52:299–310. [DOI] [PubMed]
- 28.Koike H, Morishita R, Iguchi S, Aoki M, Matsumoto K, Nakamura T, Yokoyama C, Tanabe T, Ogihara T, Kaneda Y. Enhanced angiogenesis and improvement of neuropathy by cotransfection of human hepatocyte growth factor and prostacyclin synthase gene. FASEB J. 2003;17:779–781. [DOI] [PubMed]
- 29.Lane JM. Bone morphogenic protein science and studies. J Orthop Trauma. 2005;19:S17–22. [DOI] [PubMed]
- 30.Lieberman JR, Daluiski A, Einhorn TA. The role of growth factors in the repair of bone. Biology and clinical applications. J Bone Joint Surg Am. 2002;84:1032–1044. [DOI] [PubMed]
- 31.Lieberman JR, Daluiski A, Stevenson S, Wu L, McAllister P, Lee YP, Kabo JM, Finerman GA, Berk AJ, Witte ON. The effect of regional gene therapy with bone morphogenetic protein-2-producing bone-marrow cells on the repair of segmental femoral defects in rats. J Bone Joint Surg Am. 1999;81:905–917. [DOI] [PubMed]
- 32.Luo J, Sun MH, Kang Q, Peng Y, Jiang W, Luu HH, Luo Q, Park JY, Li Y, Haydon RC, He TC. Gene therapy for bone regeneration. Curr Gene Ther. 2005;5:167–179. [DOI] [PubMed]
- 33.Matsushita T, Kurokawa T. Comparison of cyclic compression, cyclic distraction and rigid fixation. Bone healing in rabbits. Acta Orthop Scand. 1998;69:95–98. [DOI] [PubMed]
- 34.Morishita R, Aoki M, Hashiya N, Makino H, Yamasaki K, Azuma J, Sawa Y, Matsuda H, Kaneda Y, Ogihara T. Safety evaluation of clinical gene therapy using hepatocyte growth factor to treat peripheral arterial disease. Hypertension. 2004;44:203–209. [DOI] [PubMed]
- 35.Musgrave DS, Bosch P, Ghivizzani S, Robbins PD, Evans CH, Huard J. Adenovirus-mediated direct gene therapy with bone morphogenetic protein-2 produces bone. Bone. 1999;24:541–547. [DOI] [PubMed]
- 36.Nakamura T, Nawa K, Ichihara A, Kaise N, Nishino T. Purification and subunit structure of hepatocyte growth factor from rat platelets. FEBS Lett. 1987;224:311–316. [DOI] [PubMed]
- 37.Nakamura T, Nishizawa T, Hagiya M, Seki T, Shimonishi M, Sugimura A, Tashiro K, Shimizu S. Molecular cloning and expression of human hepatocyte growth factor. Nature. 1989;342:440–443. [DOI] [PubMed]
- 38.Niyibizi C, Baltzer A, Lattermann C, Oyama M, Whalen JD, Robbins PD, Evans CH. Potential role for gene therapy in the enhancement of fracture healing. Clin Orthop Relat Res. 1998;355:S148–153. [DOI] [PubMed]
- 39.Oshima K, Shimamura M, Mizuno S, Tamai K, Doi K, Morishita R, Nakamura T, Kubo T, Kaneda Y. Intrathecal injection of HVJ-E containing HGF gene to cerebrospinal fluid can prevent and ameliorate hearing impairment in rats. FASEB J. 2004;18:212–214. [DOI] [PubMed]
- 40.Park SH, O’Connor K, Sung R, McKellop H, Sarmiento A. Comparison of healing process in open osteotomy model and closed fracture model. J Orthop Trauma. 1999;13:114–120. [DOI] [PubMed]
- 41.Park SH, Silva M. Effect of intermittent pneumatic soft-tissue compression on fracture-healing in an animal model. J Bone Joint Surg Am. 2003;85:1446–1453. [DOI] [PubMed]
- 42.Radomsky ML, Aufdemorte TB, Swain LD, Fox WC, Spiro RC, Poser JW. Novel formulation of fibroblast growth factor-2 in a hyaluronan gel accelerates fracture healing in nonhuman primates. J Orthop Res. 1999;17:607–614. [DOI] [PubMed]
- 43.Rundle CH, Miyakoshi N, Kasukawa Y, Chen ST, Sheng MH, Wergedal JE, Lau KH, Baylink DJ. In vivo bone formation in fracture repair induced by direct retroviral-based gene therapy with bone morphogenetic protein-4. Bone. 2003;32:591–601. [DOI] [PubMed]
- 44.Sekalska B, Ciechanowicz A, Dolegowska B, Naruszewicz M. Optimized RT-PCR method for assaying expression of monocyte chemotactic protein type 1 (MCP-1) in rabbit aorta. Biochem Genet. 2006;44:133–143. [DOI] [PubMed]
- 45.Shi E, Jiang X, Kazui T, Washiyama N, Yamashita K, Terada H, Bashar AH. Nonviral gene transfer of hepatocyte growth factor attenuates neurologic injury after spinal cord ischemia in rabbits. J Thorac Cardiovasc Surg. 2006;132:941–947. [DOI] [PubMed]
- 46.Shimamura M, Morishita R, Endoh M, Oshima K, Aoki M, Waguri S, Uchiyama Y, Kaneda Y. HVJ-envelope vector for gene transfer into central nervous system. Biochem Biophys Res Commun. 2003;300:464–471. [DOI] [PubMed]
- 47.Shimamura M, Sato N, Oshima K, Aoki M, Kurinami H, Waguri S, Uchiyama Y, Ogihara T, Kaneda Y, Morishita R. Novel therapeutic strategy to treat brain ischemia: overexpression of hepatocyte growth factor gene reduced ischemic injury without cerebral edema in rat model. Circulation. 2004;109:424–431. [DOI] [PubMed]
- 48.Southwood LL, Frisbie DD, Kawcak CE, McIlwraith CW. Delivery of growth factors using gene therapy to enhance bone healing. Vet Surg. 2004;33:565–578. [DOI] [PubMed]
- 49.Taniyama Y, Morishita R, Aoki M, Nakagami H, Yamamoto K, Yamazaki K, Matsumoto K, Nakamura T, Kaneda Y, Ogihara T. Therapeutic angiogenesis induced by human hepatocyte growth factor gene in rat and rabbit hindlimb ischemia models: preclinical study for treatment of peripheral arterial disease. Gene Ther. 2001;8:181–189. [DOI] [PubMed]
- 50.Taniyama Y, Morishita R, Hiraoka K, Aoki M, Nakagami H, Yamasaki K, Matsumoto K, Nakamura T, Kaneda Y, Ogihara T. Therapeutic angiogenesis induced by human hepatocyte growth factor gene in rat diabetic hind limb ischemia model: molecular mechanisms of delayed angiogenesis in diabetes. Circulation. 2001;104:2344–2350. [DOI] [PubMed]
- 51.Welch RD, Jones AL, Bucholz RW, Reinert CM, Tjia JS, Pierce WA, Wozney JM, Li XJ. Effect of recombinant human bone morphogenetic protein-2 on fracture healing in a goat tibial fracture model. J Bone Miner Res. 1998;13:1483–1490. [DOI] [PubMed]
- 52.Yoshimura S, Morishita R, Hayashi K, Kokuzawa J, Aoki M, Matsumoto K, Nakamura T, Ogihara T, Sakai N, Kaneda Y. Gene transfer of hepatocyte growth factor to subarachnoid space in cerebral hypoperfusion model. Hypertension. 2002;39:1028–1034. [DOI] [PubMed]