History and Physical Examination
A 16-year-old right-hand–dominant girl presented to her primary physician with a 6-month history of progressive pain and swelling in the region of the right sternoclavicular joint. The pain was not relieved by nonnarcotic analgesics. Exacerbation of the pain occurred with movement of the right shoulder. The doctor obtained plain radiographs and noted a lesion in the medial clavicle. The patient was then referred to us for evaluation. The patient reported, despite daily use of nonsteroidal antiinflammatory medications and narcotic analgesics, the pain in the region of her medial clavicle continued to progress. She described the pain as dull, aching, and constant. The pain was severe enough to awaken her regularly from sleep and was exacerbated with shoulder motion. The pain limited her activities of daily living and recreational activities. The patient denied fever, chills, night sweats, and weight loss.
On physical examination, the patient appeared uncomfortable. No deformity was present about the shoulder and clavicle. There was no erythema, and the overlying skin was normal. The region of the medial clavicle was exquisitely tender and fullness and slight warmth were observed on palpation. There was no cervical, axillary, or supraclavicular lymphadenopathy. Range of movement of the shoulder was full but painful at the extremes of movement. Cross-arm adduction of the right upper extremity elicited considerable pain. Sensory and motor function of the radial, median, ulnar, axillary, and musculocutaneous nerves was intact and symmetric when compared to the contralateral side. Grade 5 muscle power was present in the deltoid, biceps, triceps, wrist flexors, wrist extensors, finger flexors, and intrinsic hand muscles. Sensation was normal in all dermatome distributions. Distal perfusion was normal, and Adson’s test for thoracic outlet compression was negative.
We obtained plain radiographs (Fig. 1), CT scan (Fig. 2), and MR images (Fig. 3) of the clavicle to characterize the lesion.
Fig. 1.
An anteroposterior radiograph of the right clavicle shows a lytic, expansile lesion in the medial portion of the clavicle.
Fig. 2.
Coronal CT reconstruction shows the lytic lesion that does not cross the physis. No cortical disruption or fracture is seen.
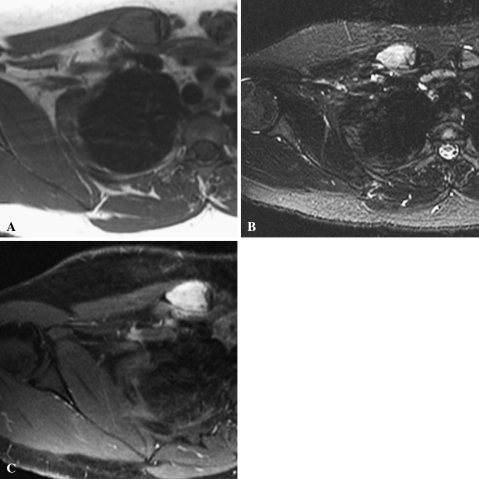
Fig. 3A–C.
(A) An axial T1-weighted MR image (TR = 416.7, TE = 8.9) shows a low signal intensity lesion with cortical thinning. The lesion is metaphyseal and does not cross the physis. (B) An axial T2-weighted MR image (TR = 4100, TE = 88.1) shows a high signal intensity lesion with a small rim of reactive edema posteriorly. (C) An axial T1-weighted MR image (TR = 466.6, TE = 8.9) with gadolinium contrast shows diffuse contrast enhancement. Slight posterior enhancement is seen in the surrounding tissues, but no soft tissue mass is seen.
Based on the history, physical examination, and imaging, what is the differential diagnosis?
Imaging Interpretation
Plain radiographs showed a lytic, expansile lesion in the medial clavicle (Fig. 1). No mineralized matrix production or cortical breakthrough was noted on plain films, but some internal trabeculations are present. CT (Fig. 2) showed an expansile lesion with considerable cortical thinning but no breakthrough. No mineralized matrix production was noted. The tumor did not appear to cross the physis. MRI (Fig. 3) showed a lesion in the medial clavicle with signal slightly hyperintense to muscle on T1-weighted images (Fig. 3A) and higher signal intensity on T2-weighted images (Fig. 3B). The lesion did not cross the physis. Uniform enhancement with intravenous gadolinium was noted (Fig. 3C). No soft tissue mass or cortical breakthrough was evident, but mild soft tissue edema was seen posteriorly.
Differential Diagnosis
Aneurysmal bone cyst
Giant cell tumor
Nonossifying fibroma
Eosinophilic granuloma
Osteomyelitis
A CT-guided biopsy and then an open biopsy were performed and the histology of the lesion was studied (Fig. 4).
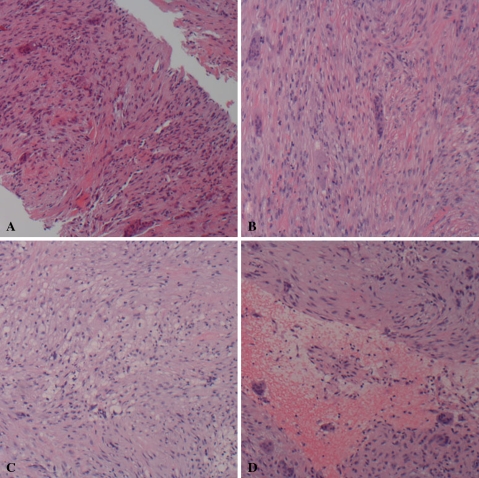
Fig. 4A–D.
(A) The CT-guided biopsy specimen contains a spindle cell proliferation with collagen production and scattered giant cells. (B) The tumor is made up of cords of benign spindle cells with irregularly dispersed giant cells. (C) A collection of foamy histiocytes is present in a background of spindle cells with a storiform pattern. (D) A cystic space with hemorrhage and giant cells is also present in the specimen (A–D: Stain, hematoxylin and eosin; original magnification, ×100).
Based on the history, physical findings, imaging studies, and histologic picture, what is the diagnosis and how should this lesion be treated?
Histology Interpretation
Histologic sections revealed benign spindle cells with a storiform pattern in areas. Irregularly dispersed giant cells were present within the tumor (Fig. 4A–B). Collections of foamy histiocytes were also present within the spindle cell background (Fig. 4C). Occasional cystic spaces with hemorrhage and giant cells were also found within the specimen (Fig. 4D). No atypical cells or mitoses were seen. Gram stain and culture were negative for bacteria, fungi, and acid-fast bacilli.
Diagnosis
Nonossifying fibroma with areas of secondary aneurysmal bone cyst formation.
Discussion and Treatment
Nonossifying fibromas are common benign bone lesions and are seen usually in the lower extremities of adolescents [5]. Upper extremity location of these tumors is uncommon. They are usually not painful in the absence of pathologic fracture; thus, they are usually discovered as incidental findings on imaging obtained for other complaints. Tenderness and abnormal physical examination findings are unusual without fracture.
Radiographically, nonossifying fibromas appear as eccentric, well-marginated, radiolucent, multiloculated lesions [5]. Their synonym, metaphyseal cortical defect, belies their usual location. A sclerotic rim of bone is usually seen around these lesions. Cortical expansion is unusual, but enlargement of these tumors is common [4]. Pathologic fracture is well described in larger lesions [1, 5, 7, 11]. Usually, clinical evaluation of the patient and plain radiographs are sufficient to make the diagnosis of nonossifying fibroma. Rarely, as in this case, they have a more aggressive, atypical presentation requiring further imaging and biopsy to confirm the diagnosis.
In this case, the clinical and radiographic features of the lesion raised several diagnostic possibilities. Aneurysmal bone cyst was certainly a possible diagnosis in this case, and the plain radiographic features could be consistent with this diagnosis. There were no fluid-fluid levels present on MRI and there was a solid component to the tumor that made this diagnosis less likely. Secondary aneurysmal bone cyst in the setting of a solid primary tumor was still possible, however. Giant cell tumor of bone was another possible differential consideration in this case. The patient was slightly young for a giant cell tumor but still well within the age range. In addition, the tumor was metaphyseal in location, making the diagnosis of giant cell tumor of bone less likely. Also, the location of a giant cell tumor in the clavicle is very uncommon. Nonossifying fibroma was a consideration in this case, but the imaging and clinical findings had several unusual features. The tumor appeared more aggressive on plain radiographs and MRI than a classic nonossifying fibroma, and the patient’s clinical symptoms of significant pain, swelling, and tenderness are unusual in nonossifying fibroma. Eosinophilic granuloma was another possibility, and eosinophilic granuloma can mimic other types of bone tumors radiographically. Finally, osteomyelitis was not likely, given the radiographic findings of an expansile, lytic lesion, but the physical findings of tenderness, warmth, and swelling could have been the result of an infectious process.
Histologically, nonossifying fibroma appears as benign fibroblastic cells arranged in a storiform pattern. Giant cells and lipid-laden histiocytes are present in an irregular distribution [4]. Secondary aneurysmal bone cyst formation has been reported in a variety of benign bone tumors; however, it is not a common finding in nonossifying fibroma [7–10]. Grossly, a hemorrhagic cavitary expansion is usually present. Microscopically, blood-filled cystic areas are seen with fibrous lining, macrophages, and giant cells. The presence of a secondary aneurysmal bone cyst component can lead to a more aggressive clinical and radiographic appearance [8, 9]. Often patients with an aneurysmal bone cyst present with pain and swelling, in contrast to the subtle clinical presentation of nonossifying fibroma [9, 10]. The extent of aneurysmal change grossly and histologically in this case was minimal; however, it may account for the more aggressive clinical and radiographic appearance of the tumor.
The shoulder girdle is the third most common site of primary bone tumors; however, clavicular tumors are rare, accounting for only 5% to 6% of shoulder girdle tumors [6, 13]. Smith et al. [13] reported their series of 58 clavicle tumors, 28 of which were benign. Osteochondroma, hemangioma, giant cell tumor, aneurysmal bone cyst, eosinophilic granuloma, fibrous dysplasia, simple cyst, and brown tumor of hyperparathyroidism were the benign tumors reported in the clavicle. Only two lesions, an osteochondroma and a giant cell tumor, were located in the medial clavicle. Cleeman et al. [6] reported eight clavicle tumors, benign and malignant, in their series of 194 shoulder girdle tumors. Barlow and Newman [2] also had eight clavicle tumors in their series of 145 shoulder girdle tumors. Three of these were benign tumors; however, no fibrous tumors were present. None of these series reported a nonossifying fibroma in the clavicle. Other medial clavicle tumors reported in the literature as isolated case reports include enchondroma and osteochondroma [3, 12]. It appears the medial clavicle is an unusual site for bone tumors, and nonossifying fibroma is extremely rare in this location.
The treatment of nonossifying fibroma is almost always nonoperative, as the overwhelming majority of these tumors are asymptomatic. Serial radiographic followup is indicated to assess stability of the lesion. Occasionally, large, symptomatic lesions at risk for pathologic fracture can be treated surgically. If a pathologic fracture occurs, the usual treatment is immobilization until the fracture heals, followed by curettage and bone grafting to prevent refracture. Upper extremity lesions are treated similarly to those found in the lower extremities.
Our patient had an unusual clinical, radiographic, and pathologic presentation of nonossifying fibroma. The initial clinical and radiographic features of the tumor led us to believe it was a benign/aggressive tumor such as an aneurysmal bone cyst or giant cell tumor. A malignant process was not favored, but still considered, as telangiectatic osteosarcoma can be purely lytic in appearance radiographically. The initial CT-guided biopsy showed findings consistent with aneurysmal bone cyst, and indeed, the clinical and radiographic features were consistent with this; therefore, we offered the patient an open biopsy, curettage, and bone-grafting procedure. The patient was taken to the operating room, where a 5-cm incision was made along the inferior border of the clavicle. The soft tissues were dissected in the standard fashion, and the medial portion of the clavicle was exposed. The anterior cortex of the clavicle was opened. Grossly, the tumor appeared solid with small, focal cystic areas and hemorrhage—it did not resemble an aneurysmal bone cyst. Frozen section showed a benign, giant cell-containing tumor consistent with nonossifying fibroma. The curettage was completed and allograft chips and demineralized bone matrix were packed into the defect. Postoperatively, the patient was treated in a sling as needed for 2 weeks. The incision healed uneventfully, and by the 2-week followup, the patient’s symptoms and use of the extremity had markedly improved. At the 3-month followup, the patient was pain-free and had full use and range of motion of the extremity.
This case represents a constellation of rare findings in the clinical, radiographic, and pathologic arenas. Nonossifying fibromas tend to be asymptomatic lesions serendipitously discovered on plain radiographs as incidental findings. They tend to be eccentrically and cortically based lesions with well-defined sclerotic borders and minimal cortical expansion. Histologically, association of a nonossifying fibroma with secondary aneurysmal bone cyst is rare. Our case of nonossifying fibroma with secondary aneurysmal bone cyst component presenting as an expansile, lytic lesion in the medial clavicle associated with severe pain, swelling, and tenderness is an unusual and interesting variant.
Footnotes
One of the authors (VOL) is a consultant for Stryker Orthopaedics, Mahwah, NJ.
Each author certifies that his or her institution has approved this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
References
- 1.Arata MA, Peterson HA, Dahlin DC. Pathological fractures through non-ossifying fibromas: review of the Mayo Clinic experience. J Bone Joint Surg Am. 1981;63:980–988. [PubMed]
- 2.Barlow IW, Newman RJ. Primary bone tumours of the shoulder: an audit of the Leeds Regional Bone Tumour Registry. J R Coll Surg Edinb. 1994;39:51–54. [PubMed]
- 3.Bernard RN, Haddad RJ. Enchondroma of the proximal clavicle: an unusual cause of pathologic fracture-dislocation of the sternoclavicular joint. Clin Orthop Relat Res. 1982;167:239–241. [PubMed]
- 4.Bertoni F, Calderoni P, Bacchini P, Sudanese A, Baldini N, Present D, Campanacci M. Benign fibrous histiocytoma of bone. J Bone Joint Surg Am. 1986;68:1225–1230. [PubMed]
- 5.Betsy M, Kupersmith LM, Springfield DS. Metaphyseal fibrous defects. J Am Acad Orthop Surg. 2004;12:89–95. [DOI] [PubMed]
- 6.Cleeman E, Auerbach JD, Springfield DS. Tumors of the shoulder girdle: a review of 194 cases. J Shoulder Elbow Surg. 2005;14:460–465. [DOI] [PubMed]
- 7.Hoeffel C, Panuel M, Plenat F, Mainard L, Hoeffel JC. Pathological fracture in non-ossifying fibroma with histological features simulating aneurysmal bone cyst. Eur Radiol. 1999;9:669–671. [DOI] [PubMed]
- 8.Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol. 1995;164:573–580. [DOI] [PubMed]
- 9.Levy WM, Miller AS, Bonakdarpour A, Aegerter E. Aneurysmal bone cyst secondary to other osseous lesions: report of 57 cases. Am J Clin Pathol. 1975;63:1–8. [DOI] [PubMed]
- 10.Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC. Aneurysmal bone cyst: a review of 150 patients. J Clin Oncol. 2005;23:6756–6762. [DOI] [PubMed]
- 11.Matsuo M, Ehara S, Tamakawa Y, Kitagawa Y, Abe M, Sakuma T. Aggressive appearance of non-ossifying fibroma with pathologic fracture: a case report. Radiat Med. 1997;15:113–115. [PubMed]
- 12.Mollano AV, Hagy ML, Jones KB, Buckwalter JA. Unusual osteochondroma of the medial part of the clavicle causing subclavian vein thrombosis and brachial plexopathy: a case report. J Bone Joint Surg Am. 2004;86:2747–2750. [DOI] [PubMed]
- 13.Smith J, Yuppa F, Watson RC. Primary tumors and tumor-like lesions of the clavicle. Skeletal Radiol. 1988;17:235–246. [DOI] [PubMed]