Abstract
Severe distal femoral bone loss and instability in revision TKA is challenging. We retrospectively reviewed 39 rotating-hinged distal femoral replacement devices in 37 patients to examine whether improved results were obtainable, using one design, over previously published results. The average age of the patients was 76 years (standard deviation, 10 years). Indications for distal femoral replacement included 11 revision TKAs, 13 periprosthetic fractures, 11 reimplantations, two complex primary TKAs, one distal femoral nonunion, and one acute distal femur fracture. Minimum followup was 24 months (mean, 46 months; range, 24–109 months). Eight patients died during followup. There were five reoperations: two patients with recurrent infection after two-stage treatment, one patient with a periprosthetic fracture treated by open reduction and internal fixation, one patient with late hematogenous infection, and one patient with bearing exchange to treat hyperextension. No failures from aseptic loosening were seen. Knee Society scores improved from 39 preoperatively to 87, and pain scores improved from 18 preoperatively to 43. Distal femoral prosthetic replacement with a tumor-type implant in severe cases provides excellent pain relief and function with a low short-term reoperation rate and an implant survivorship rate of 87% at 46 months.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The most common use of modular distal femoral replacement prostheses is for knee reconstruction after tumor resection [7–9, 15, 19, 29]. However, there are nontumor situations in which severe bone loss, considerable instability, or both warrant consideration of rotating-hinge-style reconstruction. Constrained condylar TKA components remain the workhorse for revision TKA [20, 21]. In cases of sufficient loss of bone stock so as to destroy the ligamentous structures, gross ligamentous instability, or a combination of deformities, rotating-hinge knee designs may have an important role [3, 7, 8, 14, 31, 32, 34]. Additionally, in elderly, lower-demand patients, the immediate stability provided by distal femoral replacement may justify its use in cases of periprosthetic fracture, acute distal femoral fracture, and femoral nonunion [1, 3, 31, 32]. Many authors have described the indications and outcomes of using a rotating-hinge prosthesis in salvage revision TKAs [1, 3–5, 7, 8, 14, 15, 22, 26–29, 31, 32, 34, 37]. Indications have included revision of a previous hinged prosthesis, severe bone loss in revision and reimplantation TKA, extreme instability with collateral ligament deficiency, and various magnitudes of distal femoral fractures [3, 26]. The outcomes, much like the indications, have been mixed.
Outcomes have ranged from encouraging short-term results with no loosening and comparable results to those of condylar revision TKA designs to disastrous early failure with 1- and 5-year prosthetic survivals of only 80% and 68%, respectively [3, 26]. The most recent of these reports advises using caution when considering the use of rotating-hinged TKA in salvage reconstruction of the knee and suggests its use should be reserved for elderly and sedentary patients [26]. This echoes the results of Springer et al. [31] who noted a very high rate of infection, patellar complications, and implant breakage in their series. Contradictory results have raised the question of whether this high early failure rate is implant specific or rather more generally the concept of a rotating-hinged prosthesis in salvage situations. One such encouraging early report is that of Westrich et al. [37] who stated these devices represent a reasonable and acceptable option in cases of compromised bone and ligamentous instability.
To address the controversies, we sought to answer the following question: Does modular rotating-hinged TKA provide acceptable results in terms of implant survivorship and clinical outcomes at short-term when compared with previously published results?
Materials and Methods
We queried our practice’s electronic medical record system (DocuMed®; DocuMed, Inc, Ann Arbor, MI) to identify all patients who had primary, revision, or reimplantation TKAs between 1998 and 2005 and found 7353 TKAs. For this review, we included only patients in whom the Orthopaedic Salvage System (OSS™; Biomet, Inc, Warsaw, IN) was used (Fig. 1). Although constrained condylar components are adequate for the majority of revision and reimplantation cases, a rotating-hinge device is indicated in salvage situations for gross instability, where the medial and lateral collateral ligaments are compromised and incompetent. In addition, the OSS™ provides a wide range of modular options for addressing severe bone loss. Among these 7353 TKAs, we identified 50 patients (52 knees) who had the OSS™ implanted. We excluded 13 patients in whom the OSS™ device was used for 13 total femoral reconstructions. Thus, the study group included 37 patients with 39 knees, with these extreme salvage scenarios representing 0.5% of our practice’s TKA population (Table 1). In one patient (two knees), the OSS™ device was inserted during complex primary TKA, and in 11 patients (11 knees) the procedure was a revision TKA. The device was used for reconstruction after two-stage treatment of an infected distal femoral nonunion in one knee (Fig. 2), periprosthetic TKA infection as part of a two-stage treatment protocol in 10 knees, and used acutely to treat a severely comminuted distal femur fracture in one knee. In one knee, the rotating-hinge device was used to treat chronic distal femoral nonunion. The remaining 13 knees were treated for acute periprosthetic distal femur fractures (Fig. 3). There were 27 women (two had bilateral TKAs) and 10 men in the study group. The left knee was affected in 23 patients. The average age at the time of rotating-hinge reconstruction was 75.6 years (range, 52.6–91.3 years; standard deviation, 10.1 years). Complete data, including revision status and mortality, were known for all patients. During the study period, eight patients (nine knees) died. Three patients died before a minimum 24-month followup; all other living and dead patients had a minimum 24-month followup (mean, 45 months; range, 24–109 months). Our Institutional Review Board gave prior approval for the database and the study.
Fig. 1.
A photograph of the Orthopaedic Salvage System (OSS™; Biomet, Inc) shows a device with a segmental femoral option (left) and a device with a resurfacing femoral option (right). (Reproduced with permission from Biomet, Inc, Warsaw, IN.).
Table 1.
Indications for the OSS™ rotating-hinged distal femoral replacement
| Indication | Number of knees |
|---|---|
| Revision cases | 11 (28.2%) |
| Aseptic loosening | 5 (12.8%) |
| Failed allograft-prosthetic composite | 1 (2.6%) |
| Instability | 4 (10.3%) |
| Failed nonmodular hinge | 1 (2.6%) |
| Infection | 11 (28.2%) |
| Two-stage reimplantation | 10 (25.6%) |
| Infected nonunion | 1 (2.6%) |
| Periprosthetic fracture | 13 (33.3%) |
| Other | 4 (10.3%) |
| Distal femoral nonunion | 1 (2.6%) |
| Acute femur fracture | 1 (2.6%) |
| Complex primary TKA | 2 (5.1%) |
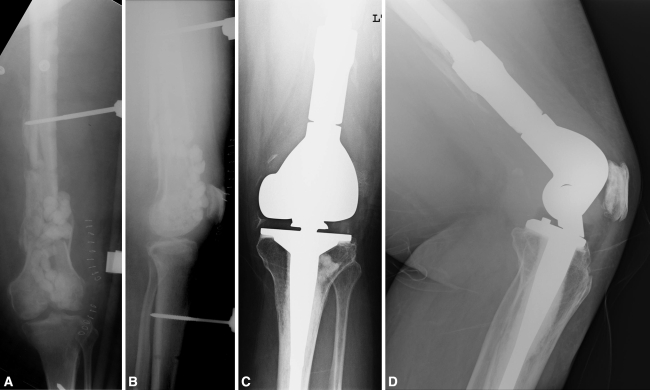
Fig. 2A–D.
A 52-year-old woman sustained a high-energy distal femur fracture initially treated with open reduction and internal fixation. This went on to become an infected nonunion. After hardware removal and placement of an external fixator and antibiotic-laden beads, the patient presented for evaluation. (A) Anteroposterior and (B) lateral radiographs show a comminuted nonunion with an external fixator and antibiotic beads in place. (C) Anteroposterior and (D) lateral radiographs show the large segmental distal femoral replacement device used during reimplantation after two-stage radical débridement and an intervening period of antibiotic therapy.
Fig. 3A–D.
(A) Anteroposterior and (B) lateral radiographs of a 77-year-old woman with considerable osteoporosis show a comminuted periprosthetic distal femur fracture. A distal femoral replacement with segmental components and a cementless stem was used with a monoblock cemented tibial implant. Postoperative (C) anteroposterior and (D) lateral radiographs show restoration of leg length and joint line with the use of a segmental replacement.
Eleven patients (12 knees) were admitted for surgery in the acute setting (eg, periprosthetic fracture) and thus preoperative evaluation was not possible. Of the 27 knees in 26 patients who were evaluated preoperatively, the average Knee Society score was 39 and the pain subscore averaged 18 [16]. The average range of motion (ROM) in knees available for preoperative examination was 63° with an average 8° flexion contracture. Considerable mediolateral or anteroposterior instability was present in 13 of 27 knees (48%).
The OSS™ is a modular reconstruction system consisting of six possible resurfacing or segmental distal femoral replacement devices. The appropriate style of distal femoral replacement can be attached to modular diaphyseal segments of various lengths to address major diaphyseal bone loss. Femoral fixation consists of cemented or fully porous-coated cementless stems of varying lengths and diameters. The tibial component is available in a monoblock cemented design and a modular design with cemented or porous-coated cementless stem options. The design rationale is based on the work of Finn et al. [11] who described an improved articular design with geometry providing increased contact area throughout a useful ROM and improved patellofemoral biomechanics [3, 11, 37]. The study device received clearance as the OSS™ from the US Food and Drug Administration in November 2000. The only design change from the original Finn® System (Biomet, Inc) to the OSS™ was a switch from two separate male tapers to a universal male taper.
The technique of rotating-hinged knee reconstruction was described by Springer et al. [32] and Barrack [3]. We used a similar technique for bony preparation for the OSS™ device in our series, with proprietary elements of the implant assembled according to the manufacturer’s specifications. All procedures were performed using an extensile medial-parapatellar approach. We used antibiotic-impregnated cement in all cases of cemented or partially cemented components. The most commonly used femoral device in this series is the segmental replacement used in 24 knees, whereas the 3-cm resurfacing design was used in 15 knees. The femoral stem was cemented in 55% of cases. The majority (79%) of tibial implants were fully cemented. The most common tibial component was a monoblock implant with a 10-mm-diameter and 160-mm-length cemented smooth stem, which was used in 52% of cases. In concert with femoral and tibial reconstruction, several simultaneous procedures were performed. Patellar revision was performed in five of the revision-type cases. Open reduction and internal fixation to decrease the potential for a periprosthetic fracture between the OSS™ stem and a THA implant was performed in one knee, and a medial gastrocnemius rotational flap was performed in one knee to provide adequate soft tissue coverage.
We applied a bulky, well-padded dressing for one night after surgery. Routinely, the patients were allowed to mobilize as tolerated the day after surgery. Postoperatively, patients were instructed and advised to use a walker or crutches for 6 weeks. Passive assisted and active ROM exercises were encouraged for up to 4 weeks under the instruction of a physical therapist.
Clinical and radiographic evaluations were performed by clinical nurses, physician assistants, or the surgeon at 2 weeks, 6 weeks, and annually thereafter. These observers (KRB, AVL, others in Acknowledgments, MT, KB, JW, JH, TK, DB, JR, KD, KS, BW, under the supervision of the surgeon authors) determined the Knee Society rating system [16] (0–100 clinical and 0–100 functional) and pain subscore (0–50) at each visit. Range of motion was measured with the patient supine and the hip flexed to 90° using a goniometer. One of the authors (KRB) examined followup radiographs to look for gross signs of loosening such as changes in implant position or migration, radiolucencies that were progressive or complete, or mechanical problems such as dissocation of the implant, breakage of the implant, or signs of instability or malalignment. No radiographic rating system was used.
Data were recorded in a prospective fashion and mined using DocuMed®. Kaplan-Meier survival estimates with 95% confidence intervals were calculated using any reoperation as the end point and censoring patients on death or loss to followup. We performed survival analysis using StatsDirect software (StatsDirect Ltd, Cheshire, UK).
Results
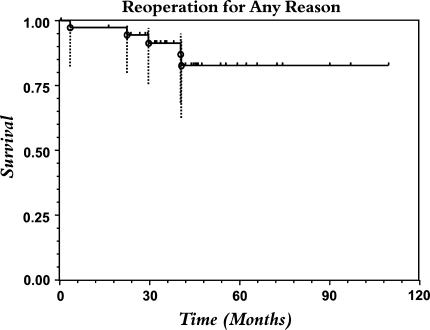
Overall implant survivorship free of any reoperation for all patients was 87% at 4 years. Kaplan-Meier survival estimates were 97% at 1 year, 95% at 2 years, 91% at 3 years, and 83% at 4 and 5 years (Fig. 4). At 34 months, one knee with aseptic failure was revised with a polyethylene exchange for symptomatic hyperextension without revision of the femoral and tibial components. We had recurrent infection after two-stage treatment in two knees, one at 3 months resulting in above-knee amputation and the second at 45 months successfully treated with a repeat two-stage protocol and reimplantation with a second hinged prosthesis. One patient underwent incision and drainage with modular polyethylene implant exchange for acute hematogenous infection 45 months after surgery. She remains free of infection with good function. One patient underwent open reduction and internal fixation at 40 months for periprosthetic fracture about the tip of the femoral stem.
Fig. 4.
Kaplan-Meier survivorship estimates with time with reoperation for any reason as the end point are shown. The number of patients at risk at the time of each failure is: amputation attributable to recurrent infection at 3 months: 37; poly change attributable to hyperextension at 34 months: 27; open reduction and internal fixation of periprosthetic fracture at 41 months: 22; incision and drainage with poly exchange for treatment of infection and radical débridement for two-stage treatment of recurrent infection at 45 months: 17. The upward ticks represent censored patients. The dotted lines = 95% confidence intervals.
At an average followup of 45 months, the Knee Society clinical knee score improved an average of 47 points from 39 to 87. The Knee Society functional score improved an average of 22 points from 13 to 35. The pain subscore improved an average of 25 points from 18 to 43 at the most recent followup. The mean ROM was 106° with less than 1° flexion contracture.
Discussion
Published results using the rotating-hinged knee implants for nontumor reconstruction have varied from acceptable to poor (Table 2). Whether these differences relate to specific design features or the general concept of a rotating-hinged implant is unclear. To address the controversy, we sought to answer the following question: Does a contemporary design modular rotating-hinged TKA prosthesis provide acceptable results in terms of implant survivorship and clinical outcomes at short-term when compared with published results?
Table 2.
Published results with rotating-hinge devices in nontumor use
| Study | Year | Number of patients | Number of knees | Mean followup (months) | Device* | Postoperative Hospital for Special Surgery score (0–100) | Postoperative Knee Society clinical score (0–200) | Postoperative range of motion | Survival free of open reoperation for any reason |
|---|---|---|---|---|---|---|---|---|---|
| Shindell et al. [30] | 1986 | 14 | 18 | 60–75 | Noiles | 77 | 44% | ||
| Rand et al. [28] | 1987 | 36 | 38 | 50 | Kinematic | 100° | 48% | ||
| Berman et al. [5] | 1996 | 9 | 9 | 24 | Kinematic | 71 | 93° | 67% | |
| Lombardi et al. [22] | 1997 | 109 | 113 | 25 | Endo-Model | 73 | 95° | 85% | |
| Barrack et al. [4] | 2000 | 15 | 16 | 51 | S-ROM | 131 | 93° | 94% | |
| Westrich et al. [37] | 2000 | 21 | 24 | 33 | Finn | 128 | 92% | ||
| Barrack [3] | 2001 | 22 | 23 | 58 | S-ROM | 133 | 95° | 96% | |
| Jones et al. [17] | 2001 | 15 | 16 | 47 | S-ROM | 137 | 105° | 88% | |
| Jones et al. [18] | 2001 | 29 | 30 | 49 | S-ROM | 134 | 100° | 90% | |
| Springer et al. [31] | 2001 | 58 | 69 | 75 | Kinematic | 100 | 94° | 67% | |
| Springer et al. [32] | 2004 | 25 | 26 | 59 | Kinematic | 101 | 97° | 73% | |
| Pradham et al. [27] | 2004 | 50 | 51 | 48 | Endo-Model | 72 | 89° | ||
| Petrou et al. [25] | 2004 | 80 | 100 | 132 | Endo-Model | 163 | 120° | 87% | |
| Utting and Newman [34] | 2004 | 30 | 36 | Custom Endo-Model (21 rotating; 9 fixed) | 106 | 70% | |||
| Pour et al. [26] | 2007 | 43 | 44 | 50 | 31 Kinematic; 13 Finn | 117 | 70% | ||
| Back et al. [2] | 2008 | 30 | 32 | 58 | SMILES | 95 | 88° | 84% | |
| Current study | 2008 | 37 | 39 | 46 | OSS | 123 | 106° | 87% |
* Devices included Noiles™ (DePuy Orthopaedics, Inc, Warsaw, IN), Kinematic® (Stryker Orthopaedics, Mahwah, NJ), Endo-Model® (Waldemar Link, Hamburg, Germany), S-ROM® (DePuy Orthopaedics, Inc), Finn® (Biomet, Inc, Warsaw, IN), SMILES™ (Stanmore Implant Worldwide Ltd, Stanmore, UK), and OSS™ (Biomet, Inc).
Our study has several shortcomings. First, there was a high mortality rate in these elderly patients during the study period and thus questions of long-term fixation, wear, and breakage cannot be answered in these cases. Second, the use of a rotating-hinge OSS™ is based on surgeon experience and preference and thus a major bias may exist for the use of this device in some cases. This limits our ability to identify ideal indications for this procedure using this device. The use of one device precludes direct comparison of this device to others with varying design features. Thus, we can make only general comparisons to other devices, indications, and surgeons.
Other rotating-hinge designs have been used during the more than 37-year history of our practice, most notably the Endo-Model® (Waldemar Link, Hamburg, Germany) with results published in an earlier study [22]. In a series of 109 patients (113 TKAs) with a mean 25-month followup, survival was 85% with any open reoperation as the end point. Although the survival was similar in the current series of patients with the OSS™, the followup in the OSS™ series was twice as long. Other studies have noted problems with dislocation of the Endo-Model® implant, despite an antidislocation feature [24, 35, 36]. Femoral-tibial dislocations occurred in two knees in our Endo-Model® series whereas none were observed in the current study.
In younger, more active patients, a rotating-hinge TKA prosthesis may be a second choice behind an allograft-prosthetic composite, the success of which has been reported in multiple series [6, 10, 12, 13, 23, 33]. In our series, the average age of the patients was 76 years, with 62% of patients older than 75 years and 46% older than 80 years. This demographic underscores the usefulness of a modular, rotating-hinge reconstruction system for treatment of complex prosthetic problems in elderly, low-demand patients. Springer et al. [31, 32] and Pour et al. [26] also noted an elderly average age and a preponderance of female patients in their study. The majority of our severely affected patients were female, perhaps reflecting the increased longevity of female patients and the added surgical problems associated with osteoporosis.
There have been favorable reports of modern rotating-hinge prostheses use for complex TKAs [2–4, 17, 18, 22, 25, 27, 37]. Barrack [3] reported only one intraoperative complication and one subsequent surgery without any loosening or failure directly related to a hinged device. Other reports have been less favorable [24, 26, 28, 30–32, 34–36]. Springer et al. [32] reported a 31% complication rate and an associated 19% rate of deep infection. Perhaps the most sobering experience is that of Pour et al. [26] who had a 79.8% rate of prosthetic survival at 1 year and 68.2% at 5 years. In contrast to these results, our overall complication rate was 18%: one acute death, one early death, and five reoperations. Furthermore, only three infections occurred, two of which were recurrent in patients who had two-stage reimplantations, for a rate of 8%. These two recurrent infections were in patients who had the only reoperations resulting in removal of the femoral and tibial components. Although these rates may be higher than those in routine revision TKAs, they represent the most complex clinical scenarios in patients who are likely older and more infirmed. The Kaplan-Meier predicted survivorship rate of 97% at 1 year is higher in our series than that of Pour et al. [26], as is the survivorship estimate at 5 years of 83% compared with 68%. We suspect advancements in design, fixation, and modularity may be responsible for the improved results in our study.
In these difficult situations, the choice to proceed with resection of the distal femur seems to result in good survivorship and function. However, rerevision or failure of these devices is complex and may result in an unsalvageable situation. Therefore, while caution is advised, distal femoral replacement seems a reasonable option in these difficult cases that, fortunately, represent a small percentage of our TKA volume. Our data support the continued use of a modular rotating-hinge knee system in cases of complex knee reconstruction similar to those described with severe instability and massive bone loss, complex primary TKA, periprosthetic fracture, or acute distal femoral fracture in elderly patients in addition to the standard tumor uses. As the revision burden increases, so will the number of multiple revision surgeries and the complexity of revision procedures, making the need for these devices likely to grow.
Acknowledgments
We thank Joanne Adams and Tawnya Tucker for assistance in preparation of this manuscript and completion of this study. We also thank the excellent members of our clinical staff, current and past, who assisted in the care of our patients, including Mike Thomas, PA-C, Kurt Berlekamp, PA-C, Jeff Williams, PA-C, Jenifer Hickman, CNP, Tina Klemp, RN, Doug Brewer, Jackie Russell, RN, Kathie Dodds, RN, Kris Stone, RN, and Bob Waterman, PA-C.
Footnotes
One or more of the authors (KRB, AVL) have received institutional research funding, consulting income, from a commercial interest related to the subject of this manuscript (Biomet, Inc, Warsaw, IN).
Each author certifies that his institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Appleton P, Moran M, Houshian S, Robinson CM. Distal femoral fractures treated by hinged total knee replacement in elderly patients. J Bone Joint Surg Br. 2006;88:1065–1070. [DOI] [PubMed]
- 2.Back DL, David L, Hilton A, Blunn G, Briggs TW, Cannon SR. The SMILES prosthesis in salvage revision knee surgery. Knee. 2008;15:40–44. [DOI] [PubMed]
- 3.Barrack RL. Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res. 2001;392:292–299. [DOI] [PubMed]
- 4.Barrack RL, Lyons TR, Ingraham RQ, Johnson JC. The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplasty. 2000;15:858–866. [DOI] [PubMed]
- 5.Berman AT, O’Brien JT, Israelite C. Use of the rotating hinge for salvage of the infected total knee arthroplasty. Orthopedics. 1996;19:73–76. [DOI] [PubMed]
- 6.Bezwada HP, Shah AR, Zambito K, Cerynik DL, Johanson NA. Distal femoral allograft reconstruction for massive osteolytic bone loss in revision total knee arthroplasty. J Arthroplasty. 2006;21:242–248. [DOI] [PubMed]
- 7.Cameron HU, Hu C, Vyamont D. Hinge total knee replacement revisited. Can J Surg. 1997;40:278–283. [PMC free article] [PubMed]
- 8.Cameron HU, Jung YB. Hinged total knee replacement: indications and results. Can J Surg. 1990;33:53–57. [PubMed]
- 9.Choong PF, Sim FH, Pritchard DJ, Rock MG, Chao EY. Megaprostheses after resection of distal femoral tumors: a rotating hinge design in 30 patients followed for 2–7 years. Acta Orthop Scand. 1996;67:345–351. [DOI] [PubMed]
- 10.Clatworthy MG, Ballance J, Brick GW, Chandler HP, Gross AE. The use of structural allograft for uncontained defects in revision total knee arthroplasty: a minimum 5-year review. J Bone Joint Surg Am. 2001;83:404–411. [DOI] [PubMed]
- 11.Finn HA, Golden D, Kneisl JA, Simon MA. The Finn Knee. Rotating-hinge replacement of the knee: preliminary report of a new design. In: Brown KLB, ed. Complications of Limb Salvage. Prevention, Management, Outcome. Montreal, Canada: International Symposium on Limb Salvage; 1991;413–416.
- 12.Ghazavi MT, Stockley I, Yee G, Davis A, Gross AE. Reconstruction of massive bone defects with allograft in revision total knee arthroplasty. J Bone Joint Surg Am. 1997;79:17–25. [DOI] [PubMed]
- 13.Harris AI, Poddar S, Gitelis S, Sheinkop MB, Rosenberg AG. Arthroplasty with a composite of an allograft and a prosthesis for knees with severe deficiency of bone. J Bone Joint Surg Am. 1995;77:373–386. [DOI] [PubMed]
- 14.Harrison RJ Jr, Thacker MM, Pitcher JD, Temple HT, Scully SP. Distal femoral replacement is useful in complex total knee arthroplasty revisions. Clin Orthop Relat Res. 2006;446:113–120. [DOI] [PubMed]
- 15.Hui FC, Fitzgerald RH Jr. Hinged total knee arthroplasty. J Bone Joint Surg Am. 1980;62:1513–1519. [PubMed]
- 16.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed]
- 17.Jones RE, Barrack RL, Skedros J. Modular, mobile-bearing hinge total knee arthroplasty. Clin Orthop Relat Res. 2001;392:306–314. [DOI] [PubMed]
- 18.Jones RE, Skedros JG, Chan AJ, Beauchamp DH, Harkins PC. Total knee arthroplasty using the S-ROM mobile-bearing hinge prosthesis. J Arthroplasty. 2001;16:279–287. [DOI] [PubMed]
- 19.Kawai A, Muschler GF, Lane JM, Otis JC, Healey JH. Prosthetic knee replacement after resection of a malignant tumor of the distal femur: medium to long-term results. J Bone Joint Surg Am. 1998;80:636–647. [DOI] [PubMed]
- 20.Lombardi AV Jr, Berend KR. The role of constraint in revision TKA: striking the balance. Orthopedics. 2006;29:847–849. [DOI] [PubMed]
- 21.Lombardi AV Jr, Berend KR. Posterior cruciate ligament-retaining, posterior stabilized, and varus/valgus posterior stabilized constrained articulations in total knee arthroplasty. Instr Course Lect. 2006;55:419–427. [PubMed]
- 22.Lombardi AV Jr, Mallory TH, Eberle RW, Adams JB. Rotating hinge prosthesis in revision total knee arthroplasty: indications and results. Surg Tech Int. 1997;6:379–382. [PubMed]
- 23.Mow CS, Wiedel JD. Structural allografting in revision total knee arthroplasty. J Arthroplasty. 1996;11:235–241. [DOI] [PubMed]
- 24.Pacha-Vicente D, Malik A, Castellet-Feliu E, Nardi-Vilardaga J. Dislocation of rotating-hinge knee prosthesis with antidislocation mechanism. J Arthroplasty. 2008;23:299–303. [DOI] [PubMed]
- 25.Petrou G, Petrou H, Tilkeridis C, Stavrakis T, Kapetsis T, Kremmidas N, Gavras M. Medium-term results with a primary cemented rotating-hinge total knee replacement: a 7- to 15-year follow-up. J Bone Joint Surg Br. 2004;86:813–817. [DOI] [PubMed]
- 26.Pour AE, Parvizi J, Slenker N, Purtill JJ, Sharkey PF. Rotating hinged knee replacement: use with caution. J Bone Joint Surg Am. 2007;89:1735–1741. [DOI] [PubMed]
- 27.Pradham NR, Bale L, Kay P, Porter ML. Salvage revision total knee replacement using the Endo-Model rotating hinge prosthesis. Knee. 2004;11:469–473. [DOI] [PubMed]
- 28.Rand JA, Chao EY, Stauffer RN. Kinematic rotating-hinge total knee arthroplasty. J Bone Joint Surg Am. 1987;69:489–497. [PubMed]
- 29.Shih LY, Sim FH, Pritchard DJ, Rock MG, Chao EY. Segmental total knee arthroplasty after distal femoral resection for tumor. Clin Orthop Relat Res. 1993;292:269–281. [PubMed]
- 30.Shindell R, Neumann R, Connolly JF, Jardon OM. Evaluation of the Noiles hinged knee prosthesis: a five-year study of seventeen knees. J Bone Joint Surg Am. 1986;63:579–585. [PubMed]
- 31.Springer BD, Hanssen AD, Sim FH, Lewallen DG. The kinematic rotating hinge prosthesis for complex knee arthroplasty. Clin Orthop Relat Res. 2001;392:283–291. [DOI] [PubMed]
- 32.Springer BD, Sim FH, Hanssen AD, Lewallen DG. The modular segmental kinematic rotating hinge for nonneoplastic limb salvage. Clin Orthop Relat Res. 2004;421:181–187. [DOI] [PubMed]
- 33.Tsahakis PJ, Beaver WB, Brick GW. Technique and results of allograft reconstruction in revision total knee arthroplasty. Clin Orthop Relat Res. 1994;303:86–94. [PubMed]
- 34.Utting MR, Newman JH. Customised knee replacements as a salvage procedure for failed total knee arthroplasty. Knee. 2004;11:475–479. [DOI] [PubMed]
- 35.Wang CJ, Wang HE. Early catastrophic failure of rotating hinge total knee prosthesis. J Arthroplasty. 15:387–391. [DOI] [PubMed]
- 36.Ward WG, Haight D, Ritchie P, Gordon S, Eckardt JJ. Dislocation of rotating hinge total knee prosthesis: a biomechanical analysis. J Bone Joint Surg Am. 2003;85:448–453. [DOI] [PubMed]
- 37.Westrich GH, Mollano AV, Sculco TP, Buly RL, Laskin RS, Windsor R. Rotating hinge total knee arthroplasty in severely affected knees. Clin Orthop Relat Res. 2000;379:195–208. [DOI] [PubMed]