Abstract
Heterotopic ossification is a well-known complication after fixation of an acetabular fracture. Indomethacin and radiation therapy are used as prophylaxis to prevent heterotopic ossification. It is unclear, however, whether either is superior, although this may relate to lack of power in individual studies. To compare the effectiveness of indomethacin with the effectiveness of radiation therapy, we conducted a systematic review in which all published prospective studies were evaluated. We performed a literature search in PubMed®, MEDLINE®, EMBASE™, and the Cochrane Controlled Trial Register. The retrieved studies were analyzed and categorized according to the quality and validity score of Jadad et al. We found five appropriate prospective studies, describing 384 patients. Although the quality of the available studies made a proper meta-analysis inappropriate, the incidence of heterotopic ossification was significantly lower in patients treated with radiation than in patients receiving indomethacin (five of 160 versus 20 of 224, respectively). Until further information is available, we believe the evidence supports radiation therapy as the preferred method for preventing heterotopic ossification after operative treatment of acetabular fractures.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Open reduction and internal fixation often are used to treat acetabular fractures to restore joint congruency. The operations on acetabular fractures, however, are associated with heterotopic ossification (HO). The relation with the surgical approach, which can be ilioinguinal, extended iliofemoral, or dorsal, is unclear [1, 35], although some authors state the more extensile the approach, the higher the incidence of HO [8, 20]. Disabling ossification occurs in approximately 5% of nonoperatively treated patients [32], but after operative treatment, the incidence increases substantially [21, 41]. The reported incidence of HO varies from 18% to 90% [3, 22]. In a meta-analysis [11], the incidence of HO after operative repair of acetabular fractures was determined to be 25.6%. To prevent HO, two primary approaches have been used: radiation therapy [2, 7] and indomethacin [22, 23, 28]. Although both methods are effective [3, 30], both have disadvantages. For radiation therapy, patients must be transported from the ward to the radiation department, and radiation personnel must be available to perform the procedure. Especially in severely injured patients, this may not be feasible. Moreover, radiation is known to induce malignancy and oligospermia and influence fertility in women, although the dosage in pelvic radiation used for acetabular fractures is in a safe range regarding potential risk of cancer and infertility [31]. Finally, radiation therapy is relatively expensive. When using indomethacin, prolonged bleeding time, gastromucosal irritation, and an increase in nonunions of associated fractures can be observed [5].
Burd et al. reported no major difference between indomethacin and radiation therapy in preventing HO in acetabular fractures [6]. In a Letter to the Editor in 2002, Michalak [25] raised concerns regarding this study, pointing to the possibility of a Type II error, ie, not finding a difference when a difference does exist.
We therefore performed a systematic review of the existing literature with the intent of performing a meta-analysis of pooled data to ascertain whether indomethacin or radiation therapy was superior in preventing clinically important HO (Grade 3 or 4 according to Brooker et al. [4] and the studies of Johnson et al. [15] and Oertel et al. [31]) in patients with operatively treated acetabular fractures.
Materials and Methods
We performed searches of PubMed®, MEDLINE®, EMBASE™, and the Cochrane Controlled Trial Register. Search terms included indometacin, indomethacin, Indocid, acetabular fracture, clinical trial, heterotopic ossification, and Brooker Grade 3 or 4. We also screened the references of the obtained articles, and relevant references were retrieved. To obtain data from unpublished trials, we performed a search through the conference proceedings of the British Library. We examined references of all articles and relevant articles were read. In case of gray literature, efforts were made to retrieve the conclusions. If necessary, authors were contacted directly.
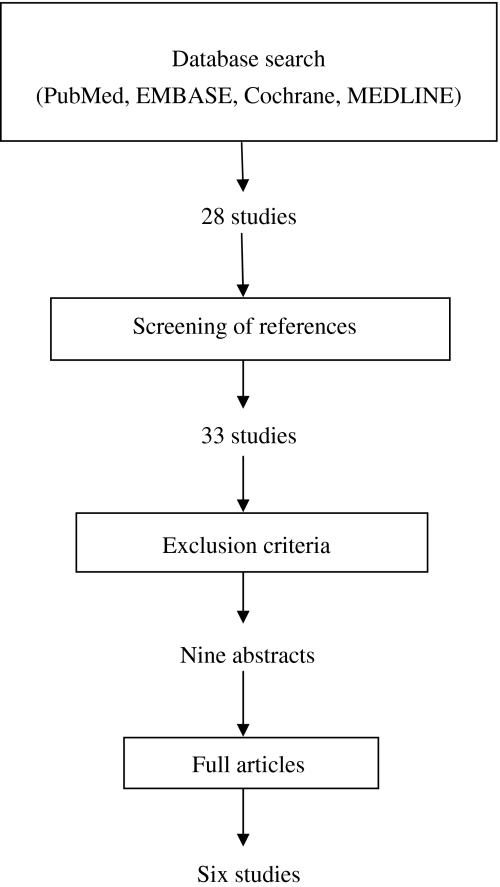
Searching these databases using the above-mentioned search terms yielded 28 results, and five more relevant studies were found in the references of the retrieved articles, leading to a total of 33 publications (Fig. 1) [1, 5–7, 9, 10, 12, 13, 15–22, 24, 26–34, 36–42]. Exclusion criteria included retrospective studies, observational studies, and case reports. The abstracts were screened for these exclusion criteria by both authors independently (TJB, JPF), leaving nine studies in our analysis [6, 7, 13, 17, 22, 26, 29, 33, 37]. After reading the full articles, two studies were excluded as they were based on retrospective data [33, 37]. One prospective study was classified as an observational study and therefore was excluded from our analysis [26]. Two studies were designed as randomized trials comparing indomethacin and radiation therapy [6, 29]. In these trials, identical treatment regimens (25 mg indomethacin three times per day versus 800 cGy radiation therapy) were used, and the end points—Brooker Grades 3 and 4—were identified. Both studies were performed by the same institution, and the study by Burd et al. [6] included the data described by Moore et al. [29]. The latter study therefore was excluded. Data of the remaining five studies were analyzed.
Fig. 1.
A flowchart illustrates the method of retrieval of articles and the decision making regarding acceptance or rejection of articles. Search terms are given in the text.
If studies involved a third treatment strategy (placebo control or various radiation regimens), we examined the possibility of data extraction from the study. This was the case in four studies. In the prospective study performed by Childs et al. [7], different radiation regimens, consisting of 700 cGy starting at different times, were compared. The aim of their study was to investigate whether logistic difficulties in radiation therapy could influence the final outcome, being the rate of Brooker Grades 3 and 4 ossification. This study concluded no differences in effectiveness were induced by different starting points of radiation therapy until 4 days postoperatively. Several patients in their study received indomethacin in addition to radiation therapy, and the data of these patients were not included in the current analysis. The other three studies randomized indomethacin versus placebo [17] or versus no prophylaxis [13, 22].
Randomization methods were documented, and in case of discussion regarding the method of randomization, consensus between the investigators decided whether a study was included. The start of the treatment regimen (preoperatively or postoperatively) and dosage were documented.
We (TJB, JPF) independently assessed the quality of the five studies for internal and external validity using the 5-point quality assessment scale of Jadad et al. [14] (Table 1). Differences in interpretation were discussed to achieve consensus.
Table 1.
Description of the assessment of validity and quality of articles according to Jadad et al. [14]
| Method | Assessment | Score* |
|---|---|---|
| Randomization | A method to generate the sequence of randomization will be regarded as appropriate if it allowed each study participant to have the same chance of receiving each intervention and the investigators could not predict which treatment was next. | 1 point |
| If the method to generate the sequence of randomization was described and it was appropriate (table of random numbers, computer generated, etc) | Add 1 point | |
| If the method to generate the sequence of randomization was described and it was inappropriate (patients were allocated alternately, or according to date of birth, date of admission, or hospital number, etc) | Deduct 1 point | |
| Double blinding | A study must be regarded as double blind if the word “double blind” is used. The method will be regarded as appropriate if it is stated that neither the person doing the assessments nor the study participant could identify the intervention being assessed, or if in the absence of such a statement the use of active placebos, identical placebos, or dummies is mentioned | 1 point |
| If the method of double blinding was described and it was appropriate (identical placebo, active placebo, dummy, etc) | Add 1 point | |
| If the study was described as double blind, but the method of blinding was inappropriate (eg, comparison of tablet versus injection with no double dummy) | Deduct 1 point | |
| Withdrawals and dropouts | Participants who were included in the study but did not complete the observation period or who were not included in the analysis must be described. The number and the reasons for withdrawal in each group must be stated. If there were no withdrawals, it should be stated in the article. If there is no statement on withdrawals, this item must be given no points | 1 point |
| Total score | 0–5 points | |
* The minimum score is 0 (poor quality, significant flaws in design or conduct of trial); the maximum score is 5. (Reprinted from Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12, copyright © 1996, with permission from Elsevier.)
The selected studies reported data from 384 patients (Table 2). Indomethacin was given in 224 patients and radiation therapy in 160. We compared the incidence of HO between the two treatment groups (radiation versus indomethacin) using the chi square test. SPSS® (Version 14.0; SPSS Inc, Chicago, IL) was used for the analysis.
Table 2.
Characteristics of included studies
| Study (year) | Number of patients | Randomization | Double blinding | Description of withdrawals/ dropouts | Validity score (Jadad et al. [14]) | ||
|---|---|---|---|---|---|---|---|
| Indomethacin | Radiation therapy | Control | |||||
| Burd et al. [5] (2003) | 72 | 78 | Yes, inappropriate | No | Yes | 2 | |
| Childs et al. [7] (2000) | 82 | No | No | No | 0 | ||
| Matta and Siebenrock [22] (1997) | 61 | 46 | Yes, inappropriate | No | No | 1 | |
| Karunakar et al. [17] (2006) | 63 | 64 | Yes, appropriate | Yes | No | 3 | |
| Iotov [13] (2000) | 28 | 24 | No | No | No | 0 | |
| Total | 224 | 160 | 134 | ||||
Results
A lower percentage (p = 0.034) of patients treated with radiation had HO develop than patients treated with indomethacin (five of 60 versus 20 of 224, respectively). We found no difference in treatment regimens or followup. The validity score of the studies according to the scale of Jadad et al. [14] varied between 0 (two studies) and 3 (one study) (Table 2).
Discussion
Operations on acetabular fractures, needed for restoration of joint congruency, are associated with HO. Disabling ossifications occur substantially more often after operative treatment, with a reported incidence between 18% and 90% [3, 22]. In a meta-analysis [11], the incidence of HO after operative repair of acetabular fractures was determined to be 25.6%. Two primary prophylactic approaches are well known: radiation therapy [2, 7] and indomethacin [22, 23, 28]. Several studies have been done to investigate whether indomethacin or radiation therapy is more effective in prevention of HO after surgical treatment of acetabular fractures. These studies were not able to show a difference, and as pointed out by Michalak [25], this may be the result of a Type II error. We therefore performed a systematic review of the literature to compare the effectiveness of these two approaches to prevent HO.
Pooling data of various studies increases the power and reduces the risk of a Type II error. The retrieved prospective studies in our systematic review were selected using rather strict criteria. However, the poor validity of the included studies, some of which were not randomized, made a meta-analysis inappropriate. Along with the poor validity, there was an uneven distribution of the patients among the studies, and although statistical corrections for an uneven distribution could have been applied, this was an additional argument against the performance of a meta-analysis. A large randomized clinical trial would be appropriate to confirm the findings in our systematic review. Based on the data in our systematic review, a sample size calculation using α = 0.05 and 1 – β = 0.80 indicates a sample size of 265 patients per arm, without dropout correction. Until such a demanding trial has been performed, new smaller trials could make a proper meta-analysis feasible.
We believe the studies we identified contain the best available evidence at this time regarding the prophylactic regimen for HO after surgical treatment of acetabular fractures. The incidence of HO seems lower in patients treated with radiation therapy, and therefore, despite the shortcomings of the gathered literature, when practical we advocate the use of radiation therapy for this indication rather than indomethacin.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Alonso JE, Davila R, Bradley E. Extended iliofemoral versus triradiate approaches in management of associated acetabular fractures. Clin Orthop Relat Res. 1994;305:81–87. [DOI] [PubMed]
- 2.Anglen JO, Moore KD. Prevention of heterotopic bone formation after acetabular fracture fixation by single-dose radiation therapy: a preliminary report. J Orthop Trauma. 1996;10:258–263. [DOI] [PubMed]
- 3.Bosse MJ, Poka A, Reinert CM, Ellwanger F, Slawson R, McDevitt ER. Heterotopic ossification as a complication of acetabular fracture: prophylaxis with low-dose irradiation. J Bone Joint Surg Am. 1988;70:1231–1237. [PubMed]
- 4.Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed]
- 5.Burd TA, Hughes MS, Anglen JO. Heterotopic ossification prophylaxis with indomethacin increases the risk of long-bone nonunion. J Bone Joint Surg Br. 2003;85:700–705. [PubMed]
- 6.Burd TA, Lowry KJ, Anglen JO. Indomethacin compared with localized irradiation for the prevention of heterotopic ossification following surgical treatment of acetabular fractures. J Bone Joint Surg Am. 2001;83:1783–1788. [DOI] [PubMed]
- 7.Childs HA 3rd, Cole T, Falkenberg E, Smith JT, Alonso JE, Stannard JP, Spencer SA, Fiveash J, Raben D, Bonner JA, Westfall AO, Kim RY. A prospective evaluation of the timing of postoperative radiotherapy for preventing heterotopic ossification following traumatic acetabular fractures. Int J Radiat Oncol Biol Phys. 2000;47:1347–1352. [DOI] [PubMed]
- 8.Chiu FY, Chen CM, Lo WH. Surgical treatment of displaced acetabular fractures: 72 cases followed for 10 (6–14) years. Injury. 2000;31:181–185. [DOI] [PubMed]
- 9.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach: description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123. [DOI] [PubMed]
- 10.Ellis T, Schmidt A. Total hip arthroplasty following failed internal fixation of acetabular fractures. Tech Orthop. 2002;17:427–433. [DOI]
- 11.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum: a meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed]
- 12.Griffin DB, Beaule PE, Matta JM. Safety and efficacy of the extended iliofemoral approach in the treatment of complex fractures of the acetabulum. J Bone Joint Surg Br. 2005;87:1391–1396. [DOI] [PubMed]
- 13.Iotov A. Heterotopic ossification in surgically treated patients with acetabular fractures and indomethacin prophylaxis for its prevention. Ortoped Travmatol. 2000;36:367–373.
- 14.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. [DOI] [PubMed]
- 15.Johnson EE, Kay RM, Dorey FJ. Heterotopic ossification prophylaxis following operative treatment of acetabular fracture. Clin Orthop Relat Res. 1994;305:88–95. [PubMed]
- 16.Johnson EE, Matta JM, Mast JW, Letournel E. Delayed reconstruction of acetabular fractures 21–120 days following injury. Clin Orthop Relat Res. 1994;305:20–30. [PubMed]
- 17.Karunakar MA, Sen A, Bosse MJ, Sims SH, Goulet JA, Kellam JF. Indometacin as prophylaxis for heterotopic ossification after the operative treatment of fractures of the acetabulum. J Bone Joint Surg Br. 2006;88:1613–1617. [DOI] [PubMed]
- 18.Kuner EH. Indication, technique and complications in the surgical treatment of acetabular fractures [in German]. Orthopade. 1997;26:327–335. [DOI] [PubMed]
- 19.Martini F, Sell S, Reize P, Jani R, Kusswetter W. Perioperative side effects of preventative measures against heterotopic ossification: diclofenac versus irradiation. Aktuelle Rheumatol. 1995;20:61–65. [DOI]
- 20.Matityahu A, Bruck N, Miclau T. Heterotopic ossification and acetabular fractures. Curr Opin Orthop. 2006;17:34.
- 21.Matta JM, Mehne DK, Roffi R. Fractures of the acetabulum: early results of a prospective study. Clin Orthop Relat Res. 1986;205:241–250. [PubMed]
- 22.Matta JM, Siebenrock KA. Does indomethacin reduce heterotopic bone formation after operations for acetabular fractures? A prospective randomised study. J Bone Joint Surg Br. 1997;79:959–963. [DOI] [PubMed]
- 23.McLaren AC. Prophylaxis with indomethacin for heterotopic bone. After open reduction of fractures of the acetabulum. J Bone Joint Surg Am. 1990;72:245–247. [PubMed]
- 24.McMaster J, Powell J. Acetabular fractures. Curr Orthop. 2005;19:140–154. [DOI]
- 25.Michalak RE. Prevention of heterotopic bone formation and type-II errors. J Bone Joint Surg Am. 2002;84:1272–1273. [PubMed]
- 26.Moed BR, Karges DE. Prophylactic indomethacin for the prevention of heterotopic ossification after acetabular fracture surgery in high-risk patients. J Orthop Trauma. 1994;8:34–39. [DOI] [PubMed]
- 27.Moed BR, Letournel E. Low-dose irradiation and indomethacin prevent heterotopic ossification after acetabular fracture surgery. J Bone Joint Surg Br. 1994;76:895–900. [PubMed]
- 28.Moed BR, Maxey JW. The effect of indomethacin on heterotopic ossification following acetabular fracture surgery. J Orthop Trauma. 1993;7:33–38. [DOI] [PubMed]
- 29.Moore KD, Goss K, Anglen JO. Indomethacin versus radiation therapy for prophylaxis against heterotopic ossification in acetabular fractures: a randomised, prospective study. J Bone Joint Surg Br. 1998;80:259–263. [DOI] [PubMed]
- 30.Morgan SJ, Jeray KJ, Phieffer LS, Grigsby JH, Bosse MJ, Kellam JF. Attitudes of orthopaedic trauma surgeons regarding current controversies in the management of pelvic and acetabular fractures. J Orthop Trauma. 2001;15:526–532. [DOI] [PubMed]
- 31.Oertel S, Schneider U, Keel M, Lutolf UM, Bosshard G. Prophylaxis of heterotopic ossification in patients sedated after polytrauma: medical and ethical considerations. Strahlenther Onkol. 2008;184:212–217. [DOI] [PubMed]
- 32.Pennal GF, Davidson J, Garside H, Plewes J. Results of treatment of acetabular fractures. Clin Orthop Relat Res. 1980;151:115–123. [PubMed]
- 33.Petsatodis G, Antonarakos P, Chalidis B, Papadopoulos P, Christoforidis J, Pournaras J. Surgically treated acetabular fractures via a single posterior approach with a follow-up of 2–10 years. Injury. 2007;38:334–343. [DOI] [PubMed]
- 34.Piatek S, Westphal T, Arbter D, Winckler S. Value of a combined ossification prophylaxis with indomethacin and radiotherapy for acetabular fractures [in German]. Unfallchirurg. 2006;109:556–562. [DOI] [PubMed]
- 35.Routt ML Jr, Swiontkowski MF. Operative treatment of complex acetabular fractures: combined anterior and posterior exposures during the same procedure. J Bone Joint Surg Am. 1990;72:897–904. [PubMed]
- 36.Ruesch PD, Holdener H, Ciaramitaro M, Mast JW. A prospective study of surgically treated acetabular fractures. Clin Orthop Relat Res. 1994;305:38–46. [DOI] [PubMed]
- 37.Schafer SJ, Schafer LO, Anglen JO, Childers M. Heterotopic ossification in rehabilitation patients who have had internal fixation of an acetabular fracture. J Rehabil Res Dev. 2000;37:389–393. [PubMed]
- 38.Stannard JP, Alonso JE. Controversies in acetabular fractures. Clin Orthop Relat Res. 1998;353:74–80. [DOI] [PubMed]
- 39.Starr AJ, Watson JT, Reinert CM, Jones AL, Whitlock S, Griffin DR, Borer DS. Complications following the “T extensile” approach: a modified extensile approach for acetabular fracture surgery-report of forty-three patients. J Orthop Trauma. 2002;16:535–542. [DOI] [PubMed]
- 40.Stockle U, Hoffmann R, Sudkamp NP, Reindl R, Haas NP. Treatment of complex acetabular fractures through a modified extended iliofemoral approach. J Orthop Trauma. 2002;16:220–230. [DOI] [PubMed]
- 41.Triantaphillopoulos PG, Panagiotopoulos EC, Mousafiris C, Tyllianakis M, Dimakopoulos P, Lambiris EE. Long-term results in surgically treated acetabular fractures through the posterior approaches. J Trauma. 2007;62:378–382. [DOI] [PubMed]
- 42.Vanden Bossche L, Vanderstraeten G. Heterotopic ossification: a review. J Rehabil Med. 2005;37:129–136. [DOI] [PubMed]