Abstract
Orthopaedic adult reconstruction subspecialists are sued for alleged medical malpractice at a rate over twice that of the physician population as a whole, and the rate appears disproportionately high in the first decade of practice. The overall risk of a malpractice claim is related to years spent in practice. After 30 years in an adult reconstruction practice, the cumulative rate of being sued at least once is over 90%. Previous investigations suggest factors such as practice setting and size, fellowship training, years in practice, volume, and location of practice correlate with malpractice risk. In contrast, we were unable to identify any relationship between the type, size, or location of practice, fellowship training, or surgery volume and the risk of an adult reconstruction surgeon being named as a defendant in a malpractice suit.
Level of Evidence: Level V, economic and decision analysis. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Physician specialty has been consistently associated with different malpractice claim rates, and orthopaedic surgery is among the highest [23]. Several theories to explain these findings have been suggested [17, 23], but none has proven conclusive. Variations may reflect differences related to the physician’s practice (eg, frequency or difficulty of procedures), patient characteristics (age, attitude, or underlying morbidity), physician–patient relationship, imperfect compensation scheme for bad outcomes, or the actual quality of care.
To better understand the factors that contribute to orthopaedic medical malpractice, Kilmo and colleagues [15] performed a randomized nationwide survey of medical malpractice attorneys. They found physician error was the most common factor associated with orthopaedic malpractice and the lumbar spine was the most common anatomic area involved in lawsuits. A surgeon appearing rushed and uninterested was more likely to encounter patient litigation, possibly because of a suboptimal physician–patient relationship. Kilmo et al. [15] did not, however, distinguish between various subspecialty groups within orthopaedics in their study. Fox and Richardson [12] reviewed International Classification of Diseases, 9th Revision (ICD-9) codes for common spine disorders and showed no major difference in the rate at which claims were paid relative to the primary diagnosis. Improper performance of a surgical procedure and diagnosis error resulted in the majority of paid claims. Upadhyay et al. [25] investigated malpractice experiences of adult reconstruction surgeons and reported 78% of responding surgeons had been named as a defendant in at least one lawsuit alleging medical malpractice. They did not report the possible contribution of demographic factors.
We sought to test whether this group of specialists (with a high rate of medical malpractice) might have certain demographic characteristics such as practice setting and size, fellowship training, years in practice, volume, and location of practice that predict medical malpractice.
Materials and Methods
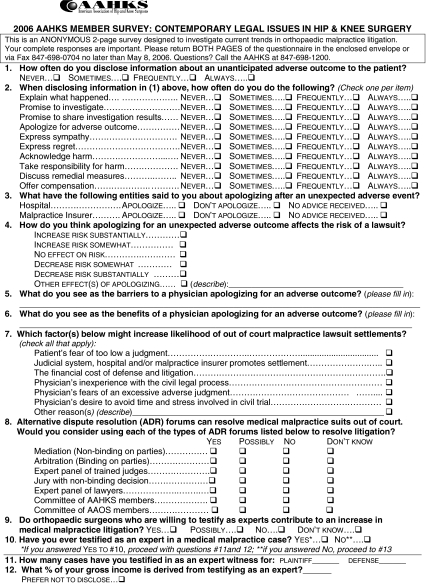
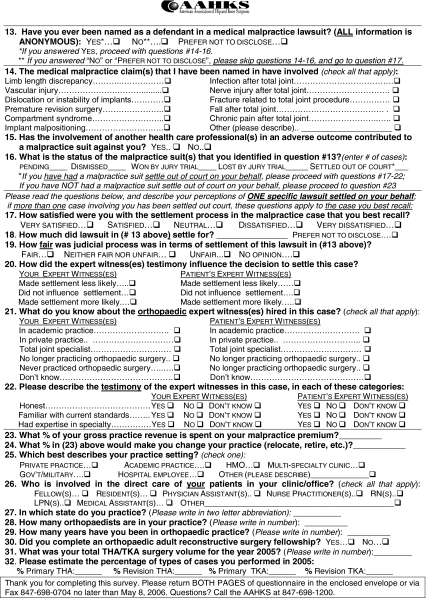
We surveyed all 749 active members of the American Association of Hip and Knee Surgeons (AAHKS) using a questionnaire developed with the Research and Legal Committees of this professional body [25]. AAHKS promotes education, research, and advocacy related to the health and disorders of the hip and knee and is comprised of members who devote at least 50% of their practice to adult hip and knee arthroplasty. We used the survey methodology of Dillman to design the questionnaire [10]. Dillman’s survey research-based tailored design methods have been developed and proven to obtain greater than 50% response rate from surveys of professional populations [10]. Each stage, element, and detail of this survey process has been found to statistically improve survey response rates from professional population samples [10].
We then used a four-stage mixed-mode survey of all AAHKS members during April and May 2006. In the first stage of the survey, a survey prenotice was emailed or faxed to active members followed by the second stage in which a cover letter with the questionnaire and a return envelope was sent from AAHKS to all active members by first class mail. The third survey stage consisted of a faxed reminder, and the fourth stage was a faxed reminder with a replacement questionnaire. The questionnaire (Appendix 1) was designed to inquire about prior experience with malpractice claims as well as basic demographic data of the respondent including type of practice setting, practice size, fellowship training in adult reconstructive surgery, years in practice, volume of arthroplasty surgeries in the previous year, and practice location. Surgeon location was categorized by US Census Bureau regions [7] (ie, Northeast, Midwest, South, and West). We considered categorizing study respondents by the state in which the surgeon practiced and the 10 Health Care Financing Administration regions [8], but the data lacked appropriate power for analysis.
Lawsuits were self-reported and included claims that were dismissed, settled out of court, won or lost at trial or by judicial ruling as well as claims that were still pending. The response rate for the survey was 56.3% (n = 422). Using Dillman’s [10] survey sample size calculations, this rate corresponded to a 95% confidence level with a ± 5% sampling error in representing the entire AAHKS membership (Table 1). Survey responses were analyzed using SPSS 12.0 (SPSS Inc, Chicago, IL).
Table 1.
Practice characteristics of 2006 AAHKS member survey respondents
| Characteristics | Number of respondents (%) |
|---|---|
| Type of practice setting* (n = 413) | |
| Private orthopaedic practice | 308 (72) |
| Academic practice | 76 (18) |
| Multispecialty clinic | 26 (6) |
| Hospital employee | 9 (2) |
| Government or military | 5 (1) |
| Health maintenance organization | 3 (1) |
| Practice size (n = 410) | |
| Solo practice | 41 (10) |
| 2–10 physicians | 211 (52) |
| 11–20 physicians | 110 (27) |
| 21–50 physicians | 42 (10) |
| 51–400 physicians | 6 (1) |
| Fellowship-trained in adult reconstructive surgery (n = 413) | |
| Yes | 245 (59) |
| No | 168 (41) |
| Years in practice (n = 412) | |
| 1–10 years | 64 (16) |
| 11–20 years | 181 (44) |
| 21–45 years | 167 (40) |
| Year 2005 total hip/knee arthroplasty surgery volume (n = 408) | |
| 0–49 casesa | 6 (2) |
| 50–100 cases | 38 (9) |
| 101–200 cases | 116 (28) |
| 201–500 cases | 219 (54) |
| 501–974 cases | 29 (7) |
| U.S. Census Bureau region (n = 415) | |
| Northeast (Region 1)** | 90 (22) |
| Midwest (Region 2)† | 105 (25) |
| South (Region 3)‡ | 137 (33) |
| West (Region 4)§ | 83 (20) |
*14 respondents indicated two types of practice settings.
aIncludes three respondents currently retired from surgery but still in practice.
**CT, ME, MA, NH, RI, VT, NJ, NY, PA.
†IN, IL, MI, OH, WI, IA, KS, MN, MO, NE, ND, SD.
‡DE, DC, FL, GA, MD, NC, SC, VA, WV, AL, KY, MS, TN, AR, LA, OK, TX.
§AZ, CO, ID, NM, MT, UT, NV, WY, AK, CA, HI, OR, WA.
Three hundred twenty-five (78%) respondents reported being named as a defendant in at least one claim alleging medical malpractice. The demographic characteristics of two groups (those reporting one or more of the previously reported claims for AAHKS members (Table 2) [25] and those reporting no claims) were compared to investigate the theory that factors such as practice setting and size, fellowship training, years in practice, volume, and location of practice correlate with malpractice risk (Table 3).
Table 2.
Self-reported nature of claims in which AAHKS members have been named as malpractice defendant [25]
| Nature of claim | Number of claims |
|---|---|
| Nerve injury after total joint procedure | 64 |
| Limb-length discrepancy | 39 |
| Infection after total joint procedure | 34 |
| Vascular injury | 31 |
| Dislocation or instability of implants | 26 |
| Compartment syndrome | 22 |
| Chronic pain after total joint procedure | 19 |
| DVT/nonfatal PE/fatal PE (related specific surgical procedure not named in most cases) | 19 |
| Fracture related to total joint procedure | 18 |
| Nontotal joint procedure adverse outcome | 18 |
| Adverse skin-related event/outcome/complication | 17 |
| Implant malpositioning | 15 |
| Death | 14 |
| Adverse fracture complication/outcome | 13 |
| Other claims (minimal or no information given) | 13 |
| Fall after total joint procedure | 11 |
| Premature arthroplasty revision surgery | 9 |
| Lower extremity injury/fracture | 9 |
| Nontotal joint procedure infection | 9 |
| Nontotal joint procedure nerve injury | 9 |
| Failure to diagnose | 9 |
| Nontotal joint pain/RSD-related | 9 |
| Adverse systemic event | 9 |
| Upper extremity injury/fracture | 8 |
| Trauma-related case | 8 |
| Arthrofibrosis | 6 |
| Wrong site/side surgery | 5 |
| Adverse medication event | 5 |
| Hardware/cement related | 5 |
| Adverse anesthesia event | 4 |
| Other total joint procedure adverse outcome | 3 |
| Sulzer cup case | 2 |
| Wrong procedure | 2 |
| Failure to consent | 2 |
| Nontotal joint procedure fall | 1 |
| Retained sponge | 1 |
| Impaired mobility | 1 |
| Workers’ compensation - patient dissatisfaction with return to work date | 1 |
| Total | 490 |
Note: Many respondents reported more than one claim type; respondents not asked to name number of claims in each category, only types of claims they have been named in.
Table 3.
Practice characteristics of 2006 AAHKS member survey respondents and association to malpractice
| Characteristics | All respondents* | Respondents named in one or more malpractice claims | p value** |
|---|---|---|---|
| Type of practice setting | 413 | 323 | 0.992 |
| Practice size | 410 | 320 | 0.352 |
| Fellowship-trained in adult reconstructive surgery | 413 | 323 | 0.49 |
| Years in practice | 412 | 322 | 0.00 |
| Year 2005 total hip/knee arthroplasty surgery volume | 408 | 320 | 0.00 |
| U.S. Census Bureau regions | 415 | 324 | 0.289 |
*Number of all respondents who completed survey question.
**Pearson chi-square P value.
Differences in adult reconstruction surgeons who had reported being named in at least one malpractice claim among “practice setting,” “practice size,” “fellowship training,” “years in practice,” “practice volume,” and “location of practice” were determined by Pearson chi square test univariate analysis. Those factors that correlated with a p value of < 0.05 were further examined by logistic regression multivariate analysis using Stata 10 (StataCorp, College Station, TX). A nonparametric trend analysis (based on sums of ranks) was used to confirm the regression study.
Results
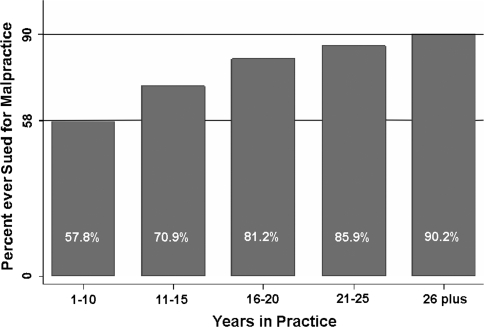
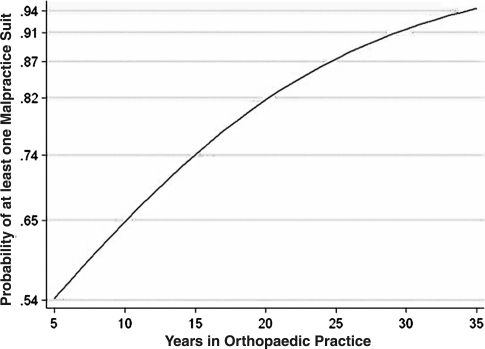
Only years in practice predicted a malpractice suit (odds ratio, 1.1; p < 0.000) (Fig. 1). The cumulative risk of being sued over time for an adult reconstructive surgeon was evaluated (Fig. 2). (Univariate analysis of data originally identified years in practice and arthroplasty volume as predictors of medical malpractice, but multivariate analysis showed years in practice was the only independent variable.) Type of practice setting, practice size, fellowship training in adult reconstruction, and practice location (by US Census Bureau region) were not related to a claim of malpractice (Table 3).
Fig. 1.
This bar graph shows percentage of membership sued for malpractice versus years in practice.
Fig. 2.
Curve demonstrates the probability of at least one malpractice lawsuit depending on years in orthopaedic practice for adult reconstructive surgeons.
Discussion
Based on prior studies showing relationships between medical malpractice and various surgeon demographics, we sought to determine if any relationships existed for these variables in the subspecialty of adult reconstructive orthopaedic surgery.
Several issues should be considered when evaluating our conclusions. The malpractice data from the AAHKS questionnaire is self-reported and, unlike closed-claim data, this study relies on surgeon recollection. It is difficult to compare the present data with other studies because our data include not only closed-claim, but also open- and pending-claims data. Also, we did not limit malpractice experience to a particular timeframe and therefore collected cumulative malpractice data. We did not specifically ask if malpractice related to total joints and did not stratify for referred cases. Future studies could examine trends in malpractice experience and the timing of such during the surgeon’s career as well as quantifying risks associated with referral cases. It should also be pointed out that the conclusions for this association of specialty surgeons may not apply to all orthopaedic surgeons performing arthroplasty because of membership requirements (eg, higher volume, likely greater interest, and perhaps expertise).
An understanding of the trends and associations in medical malpractice claims could help decrease the incidence of lawsuits when surgeons and patients are faced with a poor outcome. Many theories have been proposed as to the cause of lawsuits alleging medical malpractice [9, 12, 17, 23, 24], and multiple studies have assessed physician and practice characteristics that correlate or do not correlate with the incidence of such claims (Table 4). We found years in practice correlated with malpractice, whereas type of practice, practice size, fellowship training in adult reconstruction, surgeon volume, and practice location did not correlate.
Table 4.
Prior studies of statistical relationships between medical malpractice and various surgeon demographics
| Study | Type of physician | Characteristic |
|---|---|---|
| Positive correlation | ||
| Meadow et al. [17] | Neonatal intensivists | Years in practice |
| Community versus university setting | ||
| Taragin et al. [23] | New Jersey doctors | Specialty |
| Neurosurgery | ||
| Orthopaedic surgery | ||
| Obstetrics / gynecology | ||
| Male gender | ||
| Kahan et al. [13] | Urologists | Procedure type |
| Inpatient | ||
| Adult | ||
| Surgical procedures | ||
| Geographic location | ||
| Sloan et al. [20] | Florida doctors | Prior malpractice claim |
| Taragin et al. [22] | New Jersey doctors | Prior malpractice claim |
| Abbott et al. [2] | Ophthalmologists | Increased surgical volume |
| Prior malpractice claim | ||
| For high-volume surgeons | ||
| Gender | ||
| Advertising use | ||
| Preoperative time spent | ||
| Co-management | ||
| Taragin et al. [23] | New Jersey doctors | Specialty |
| Waters et al. [26] | Physicians, three states | Medical school |
| Ely et al. [11] | Florida family practice | Graduation from US/Canadian medical school |
| Board certification | ||
| AMA physician recognition award | ||
| AOA honor society | ||
| Rodriguez [19] | Massachusetts physican organization | Specialty |
| Kilmo et al. [15] | California members of liability protection trust | No fellowship training |
| No clinical faculty affiliation | ||
| Not a member of professional society | ||
| Not a graduate of US/Canadian medical school | ||
| No board certification | ||
| Not in group practice | ||
| Orthopaedists | ||
| No religious affiliation | ||
| No RN in office | ||
| No correlation | ||
| Meadow et al. [17] | Neonatal intensivists | Physician gender |
| Fox and Richardson [12] | Spine surgeon | Procedure type |
| Sloan et al. [20] | Florida doctors | Prestegious credentials |
| Taragin et al. [23] | New Jersey doctors | Physician performance |
| Physician age, degree, site of training, certification status, severity of injury | ||
| Rodriguez et al. [19] | Massachusetts physican organization | Care coordination |
| Quality of physician–patient interaction | ||
| Moore et al. [18] | Not stated | Day of the week |
| Taragin et al. [24] | New Jersey doctors | Specialty |
| Psychiatry | ||
| Kocher et al. [16] | Orthopaedists, three states | Board certification |
Physician malpractice claims have been paid at a rate between 1.9% (2003) and 0.9% (2007) per year for all doctors practicing in the United States, except those who are active military physicians [5, 21]. When analyzed by specialty, neurosurgery, orthopaedic surgery, and obstetrics have the highest reported claim rates [23], although actual claims data to support this contention are difficult to identify and obtain. When orthopaedic adult reconstruction surgeons were asked about their experience with malpractice claims, over 75% reported they had been sued [25]. If this number is divided by years in practice, the rate is more than twice the annual estimate for all physicians [5, 21] and three times as high in the first decade of practice. This disproportionately high rate of claims reported in the first 10 years of practice (5.8%) may be a reflection of surgeon inexperience or recent increases in malpractice claims [3, 6]. It should be underscored that these comparisons are only approximate because the national and orthopaedic subspecialist data were obtained in different ways: (1) our questionnaire data include both open and closed claims, whereas the national general physician data represent only closed claims; and (2) our data ask about one or more claims and the national data reports all claims.
Our analysis of the questionnaire data identified surgeon characteristics that correlate and do not correlate with the risk of being named in a malpractice claim. Type of practice, practice size, fellowship training in adult reconstruction, surgeon volume, and practice location (by US Census Bureau region) did not correlate with whether a surgeon had been named in a malpractice claim. In contrast, Adamson and coworkers [4] reported reduced claim rates among a general group of surgeons who had “exemplary modes of professional peer relationships and responsible clinical behavior.” Examples of such predictive factors included fellowship training, belonging to a clinical faculty, and being a member of a group practice. Our findings may differ because of greater potential homogeneity in practice patterns among members of one subspecialty such as arthroplasty surgeons. Abbott et al. [1, 2] showed that for ophthalmologists performing certain procedures, the chances of incurring a malpractice claim correlated with surgical volume. Less preoperative time spent with the patient was a predictor of malpractice for high-volume surgeons. We suspect volume did not correlate in our cohort of subspecialists because they were all relatively high-volume surgeons; possibly the increased skills and decreased complications associated with a high volume of surgery [14] were offset by less favorable physician–patient relationships from decreased time available to spend with patients before and after surgery. Finally, Kahan et al. [13] showed some propensity for geography to play into malpractice rates in urologic surgery. However, when analyzed by relative distribution of urologists, the difference in malpractice rates was not meaningful, and because the geographic units were both smaller and different from those in the present study, it is not possible to compare the studies.
Of the variables examined, only years in practice correlated with malpractice risk for members of AAHKS. This dramatic correlation (Fig. 2) increases from 58% at between 5 and 10 years to over 90% after 26 years in practice. This relationship has not been previously described, but makes sense in light of the cumulative risk of lawsuit exposure over time. It is interesting to note the curve is very steep in the first decade, near linear up to 20 years of practice, and tends to plateau toward three decades of practice. This could be because of the present experience of younger versus older surgeons with malpractice (ie, the fact that malpractice claims are more frequent in the past decade compared with 20 to 30 years ago [3]) or may relate to the previously demonstrated trend that surgeons who have not been sued are less likely to be sued [1, 2, 20, 22]. Also possible is the suggestion that as skill levels increase with experience, errors become less frequent, and the corresponding frequency of claims diminishes.
Our data suggest the high rate of medical malpractice experienced by adult reconstruction orthopaedic subspecialists is weighted toward the first decade of practice. Furthermore, for adult reconstruction subspecialists, the risk of a malpractice claim is related to years in practice. Practicing as an adult reconstruction surgeon exposes a physician to a cumulative risk of malpractice exposure that is not offset by any beneficial effects of surgeon experience gained over time with a high volume of a limited set of surgeries. The incidence of being named in a claim alleging malpractice is over 90% after 30 years in practice. Unlike many studies that show correlations of malpractice risk and surgeon demographics, we were unable to demonstrate a relationship to type, size, or location of practice, fellowship training, or surgery volume.
Acknowledgments
We thank Frank deLibero, PhD (Data 2 Information, Inc, Lacey, WA) for his assistance with statistical analysis of the data and critique of the study design. Official sponsorship from the AAHKS was obtained for this study, and the questionnaire was developed in collaboration with and approved by the AAHKS research and legal committees. Human subjects criteria were used in the questionnaire development, survey distribution, and data management stages to protect the anonymity and confidentiality of AAHKS members. We are grateful to the AAHKS members for their time spent during the completion of the survey. Hopefully, the article will help them better understand the climate in which they work.
Appendix
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the reporting of this case and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Abbott R. Medical malpractice predictors and risk factors for ophthalmologists performing LASIK and PRK surgery. Trans Am Ophthalmol Soc. 2003;101:239–274. [PMC free article] [PubMed]
- 2.Abbott R, Ou R, Bird M. Medical malpractice predictors and risk factors for ophthalmologists performing LASIK and photorefractive keratectomy surgery. Ophthalmology. 2003;110:2137–2146. [DOI] [PubMed]
- 3.Adams E, Zuckerman S. Variation in the growth and incidence of medical malpractice claims. J Health Polit Policy Law. 1984;9:475–488. [DOI] [PubMed]
- 4.Adamson TE, Baldwin DC, Sheehan TJ, Oppenberg AA. Characteristics of surgeons with high and low malpractice claims rates. West J Med. 1997;166:37–44. [PMC free article] [PubMed]
- 5.Budetti P, Waters T, Kaiser Commission on Medicaid and the Uninsured, Henry J. Kaiser Family Foundation, et al. Medical Malpractice Law in the United States. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2005.
- 6.Cascardo D. The medical malpractice crisis. What is the cause? Is there a cure? J Med Pract Manage. 2007;22:283–286. [PubMed]
- 7.Census regions and divisions of the United States. Available at: http://www.census.gov/geo/www/us_regdiv.pdf. Accessed January 2008.
- 8.Center for Medicare Services Regional Offices. Information for professionals, 2005. Available at: http://www.cms.hhs.gov/about/regions/professionals.asp. Accessed January 2008.
- 9.Crawford L. Why winners win: decision making in medical malpractice cases. J Am Acad Orthop Surg. 2007;15(Suppl 1):S70-S74. [DOI] [PubMed]
- 10.Dillman DA. Mail and Internet Surveys: The Tailored Design Method. New York, NY: Wiley; 2000.
- 11.Ely J, Dawson J, Young P, Doebbeling B, Goerdt C, Elder N, Olick R. Malpractice claims against family physicians are the best doctors sued more? J Fam Pract. 1999;48:23–30. [PubMed]
- 12.Fox B, Richardson W. Medical liability: the spinal surgery perspective. AAOS Bulletin. 2006;54.
- 13.Kahan S, Goldman H, Marengo S, Resnick M. Urological medical malpractice. J Urol. 2001;165:1638–1642. [DOI] [PubMed]
- 14.Katz J, Losina E, Barrett J, Phillips C, Mahomed N, Lew R, Guadagnoli E, Harris W, Poss R, Baron J. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001;83:1622–1629. [DOI] [PubMed]
- 15.Kilmo G, Daum W, Brinker MR, McGruire E, Elliott MN. Orthopaedic medical malpractice: an attorney’s perspective. Am J Orthop. 2000;29:93–97. [PubMed]
- 16.Kocher M, Dichtel L, Kasser J, Gebhardt M, Katz J. Orthopaedic board certification and physician performance: an analysis of medical malpractice, hospital disciplinary action, and state medical board disciplinary action rates. Am J Orthop. 2008;37:73–75. [PubMed]
- 17.Meadow W, Bell A, Lantos J. Physicians’ experience with allegations of medical malpractice in the neonatal intensive care unit. Pediatrics. 1997;99:E10. [DOI] [PubMed]
- 18.Moore J, Berry D, Knox G. Dispelling urban myths in healthcare risk management. J Health Risk Manag. 1999;19:2–10. [DOI] [PubMed]
- 19.Rodriguez HP, Rodday AM, Marshall RE, Nelson KL, Rogers WH, Safran DG. Relation of patients’ experiences with individual physicians to malpractice risk. Int J Qual Health Care. 2008;20:5–12. [DOI] [PubMed]
- 20.Sloan F, Mergenhagen P, Burfield W, Bovbjerg R, Hassan M. Medical malpractice experience of physicians. Predictable or haphazard. JAMA. 1989;262:3291–3297. [DOI] [PubMed]
- 21.Statehealthfacts.org Web site. Available at: http://statehealthfacts.org/. Accessed February 26, 2008.
- 22.Taragin MI, Martin K, Shapiro S, Trout R, Carlson J. Physician malpractice: does the past predict the future? J Gen Intern Med. 1995;10:550–556. [DOI] [PubMed]
- 23.Taragin MI, Sonnenberg FA, Karns ME, Trout R, Shaprio S, Carson JL. Does physician performance explain interspecialty differences in malpractice claim rates? Med Care. 1994;32:661–667. [DOI] [PubMed]
- 24.Taragin MI, Wilczek AP, Karns ME, Trout R, Carson JL. Physician demographics and the risk of medical malpractice. Am J Med. 1992;93:537–542. [DOI] [PubMed]
- 25.Upadhyay A, York SC, Macaulay W, McGrory B, Robbennolt J, Bal B. Medical malpractice in hip and knee arthroplasty. J Arthroplasty. 2007;22(Suppl 2):2–7. [DOI] [PubMed]
- 26.Waters T, Lefevre F, Budetti P. Medical school attended as a predictor of medical malpractice. Qual Saf Health Care. 2003;12:330–336. [DOI] [PMC free article] [PubMed]