Abstract
Patella baja is a rare condition that can result from conditions involving trauma around the knee. Risk factors are believed to include scar tissue formation in the retropatellar fat pad, extensor mechanism dysfunction, and immobilization in extension. Early recognition and aggressive treatment are critical components in minimizing long-term disability. We present a case report of a woman with a fracture of the femoral diaphysis who underwent retrograde placement of an intramedullary nail. Subsequent followup revealed development of patella baja with resultant disability. The diagnosis was made late and the treatment was ineffective. Although patella baja has been reported in trauma around the knee, causative factors include retrograde femoral nailing. We believe early recognition and institution of treatment are important.
Introduction
Since its introduction as a treatment for femoral shaft fractures, retrograde femoral nailing has become increasingly popular. Studies report high union rates, low incidence of malunion, and postoperative function that in some series equals that of other treatments [25, 26, 29, 34]. We present a case of patella baja after retrograde femoral nailing. Patella baja has been associated with injuries and surgeries around the knee, especially those that may promote scar tissue formation in the peripatellar tissues, impede range of motion, and interfere with extensor mechanism function [1–5, 8, 10, 16, 20, 27, 28, 30–32, 35, 39]. Treatment of patella baja is difficult but early recognition and intervention seem to improve outcomes compared with the natural history of this condition [24]. It is a potential source of considerable knee dysfunction. Despite its association with other surgeries around the knee, we are unaware of any previous connection between retrograde femoral nailing and patella baja.
Case Report
A 38-year-old woman was injured in a high-speed, head-on motor vehicle collision. She sustained a traumatic brain injury, first rib fractures with bilateral pneumothoraces, and bilateral, closed femoral shaft fractures (Fig. 1). She was admitted to a tertiary Level I trauma center. After resuscitation and placement of an intracranial pressure monitor, she was taken to the operating room for stabilization of her femur fractures. She underwent closed, antegrade nailing of her left femur through a piriformis fossa starting point (Fig. 2A). After this procedure, her right femur fracture was treated with closed, retrograde nailing (Fig. 2B). A medial parapatellar approach was described in the medical records from the time of initial nail placement. The reasons for the two choices of nail approaches were not clear from her medical records. No mention was made of any knee injury on either side. She later denied any history of knee injury or knee dysfunction before the injury.
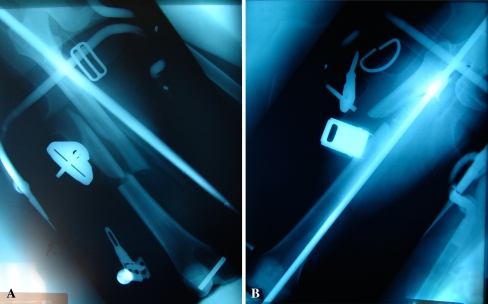
Fig. 1A–B.
Preoperative anteroposterior radiographs of the (A) right and (B) left femurs show the midshaft fracture.
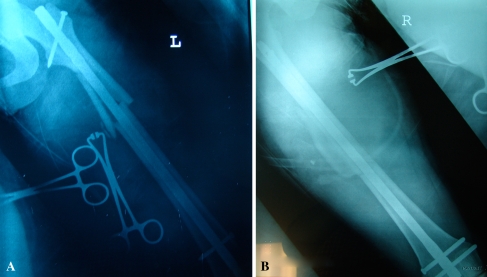
Fig. 2A–B.
Postoperative anteroposterior radiographs of (A) the left femur show the fracture and antegrade nail in place, and (B) the right femur with the fracture and retrograde nail in place.
After her acute care hospitalization, she received 6 weeks of inpatient rehabilitation. After her discharge, she returned home, across the country from the treating center. She continued with outpatient care and physical therapy.
Before her accident, she had been an avid runner, competing in marathons on a regular basis. Her physical therapy program focused on regaining range of motion and strength in her lower extremities and general conditioning. Despite almost 1 year of supervised physical therapy, the patient continued to experience activity-related pain in the right knee and left hip. She presented to the senior author (JCK) for an opinion regarding her left hip and right knee pain.
On physical examination, she exhibited a right antalgic gait with a stiff knee during ambulation. Her right knee range of motion was from full extension to 120° flexion. However, flexion beyond 90° was accompanied by considerable pain and guarding. Her left knee range of motion was 0° to 140°. Her right patellar mobility was markedly decreased. Her right patellofemoral joint was tender with marked crepitus on range of motion. She had right quadriceps atrophy, which was obvious when compared with her left side. Her left hip was mildly irritable with range of motion that was symmetric to her right. She had a snapping sensation, accompanied by pain, with rotation.
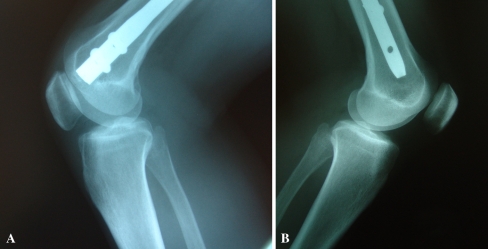
Radiographs were obtained of both femurs. Findings included healed femoral fractures with no evidence of hardware complications. The lateral views of the knees revealed an Insall-Salvati ratio of 0.45 on the right versus 1.0 on the left (Fig. 3). This difference also could be seen on the Merchant’s views of both knees (Fig. 4). Her initial postoperative radiographs (Fig. 5) revealed an Insall-Salvati ratio of 1.0 in the right knee [15].
Fig. 3A–B.
Lateral radiographs of the (A) left and (B) right knees at 16 months show Insall-Salvati ratios of 0.45 and 1.0, respectively.
Fig. 4.
A Merchant’s view of both knees show asymmetry of the patellae in the trochlear grooves.
Fig. 5.
A lateral radiograph of the right knee obtained immediately after retrograde nailing shows the Insall-Salvati ratio is 1.0
The patient underwent diagnostic arthroscopy of the right knee, right femoral nail removal, and open débridement of scar tissue from the patellar tendon and its surrounding paratenon and fat pad. The arthroscopy revealed only some thickened synovial lining and retropatellar fibrosis with no other disease. The scar tissue around the patellar tendon was extensive and was tethering the tendon, especially on the medial side. This area of maximal scarring was consistent with the previous surgical scar.
Postoperatively, she participated in an aggressive strengthening program with emphasis on quadriceps strength and patellar mobility. After 3 months, she had better motion but still had knee pain with activities requiring knee flexion.
Because she had continued to experience left hip pain, she underwent nail removal from the left femur. Her left hip pain subsequently resolved.
Two years after her initial injury, she continued to report right knee pain and activity limitations resulting from her intolerance of limited knee flexion. She was referred for another opinion. She underwent arthroscopic débridement of scar tissue around her right patella and lateral retinacular release. Scar tissue found at the time of débridement was consistent with the medial parapatellar approach described in the medical record. Knee range of motion was not reported by the operating surgeon. Again, the only finding at arthroscopy that was important was retropatellar fibrosis. She underwent a prescribed course of physical therapy, yet noted little improvement. The patient was contacted by phone 5 months after her arthroscopic débridement. At that time she reported that she remained unable to run, an activity in which she was quite active before her accident.
Discussion
Intramedullary nailing has become standard treatment for the majority of femoral shaft fractures in the skeletally mature individual [6, 7, 17, 37, 38, 40]. Although initially popularized using an antegrade technique using a piriformis fossa starting point [12, 36], other methods of insertion have been described. Among these is the retrograde approach with nail insertion at the posterior border of the trochlear groove [9, 13, 18, 22, 23]. The use of retrograde femoral nailing has increased, with some reportedly using it as the preferred treatment for the majority of femoral shaft fractures. Several series have had reported healing rates of retrograde nailing that generally are comparable to those of antegrade nailing [25, 26, 29, 34]. Despite earlier concerns regarding the use of a starting point that is intraarticular, studies of knee function after retrograde femoral nailing have, in many cases, compared favorably to antegrade approaches [26]. If anything, the conclusions drawn have led one to believe only minor knee problems should be expected [19]. However, the sample sizes in these studies have been relatively small.
Our patient had patella baja develop after retrograde femoral nailing. The case is unusual because the patient had bilateral femoral shaft fractures and was treated with one antegrade nail and one retrograde nail. Because of this constellation of injuries, she had regular radiographic followup of both knees. The side treated with the retrograde nail developed symptomatic patella baja. Patella baja is a relatively rare condition that has been associated with other knee surgeries [1–5, 8, 10, 16, 20, 27, 28, 30–32, 35, 39], but apparently not retrograde nailing. It especially has been associated with surgery that involves the patellar tendon and retropatellar fat pad such as anterior cruciate ligament reconstruction with patellar tendon autograft. Its cause is poorly understood, although Noyes et al. and Paulos et al. described immobilization associated with intraarticular injury resulting in arthrofibrosis as a major risk factor [24, 27].
Development of patella baja has been associated with surgery that disrupts the soft tissue of the envelope around the patellar tendon. It seems prudent to recommend a careful surgical technique around the patellar tendon and retropatellar fat pad to minimize scar tissue formation. Hemostasis should be maintained and dissection through the fat pad minimized.
Because decreased range of motion and quadriceps weakness have been associated with patella baja, early physical therapy after retrograde femoral nailing should emphasize knee motion and quadriceps strengthening.
Noyes et al. described progression of patella baja [24]. The initial phase is characterized by transient patella infera resulting from peripatellar scar tissue formation, including in the retropatellar fat pad, contracture of the retropatellar fat pad scar tissue, and quadriceps weakness or malfunction. This is accompanied by decreased motion. Eventually, permanent shortening of the patellar tendon occurs, leading finally to patellofemoral arthrosis. They emphasized the importance of early diagnosis, within the first 6 months. It is hoped that diagnosis and intervention within 6 months, although some of the changes are irreversible, can lead to improvement in function, decrease shortening of the patellar tendon, and prevent permanent contracture of this structure. Initially, physical therapy for knee range of motion, quadriceps strengthening, and patellar mobilization may be effective. More severe cases have benefited from arthroscopic débridement. Early débridement reportedly improves patellar height radiographically and improves function clinically [24]. Once a patellar tendon contracture has become permanent, treatment is less successful and more complicated [24, 27].
Our patient had no history of knee problems. Her only apparent risk factors for development of patella baja were the femur fracture and placement of a retrograde femoral nail, surgery involving her knee, and peripatellar soft tissues. The diagnosis was made late, by which time the contracture of her patellar tendon was permanent despite surgical débridement of the scar and lateral retinacular release. Unfortunately, patella baja is a condition that can be a source of major disability, and once the condition is well established, few successful treatment options exist [11, 14, 21, 24, 28, 33].
New techniques will introduce new challenges. These include new modes of failure and new types of surgical complications. Among surgical complications, there are problems that are relatively frequent but generally of low severity. These may include nonunion and malunion, two commonly measured outcomes of fracture treatment. These are the types of complications that a relatively small series can be fairly good at detecting. However, there are complications that have a low incidence but are high in severity. It is our suspicion that patella baja in this patient was related to the surgical approach for insertion of a retrograde femoral nail. Thus, it represents a low-incidence, high-severity complication of retrograde femoral nailing. This should be considered when deciding among treatment modalities for femoral shaft fractures. For patients who undergo retrograde femoral nailing, early rehabilitation should emphasize knee range of motion, quadriceps strengthening, and patellar mobility. Patients who do not progress in these areas should be examined, clinically and radiographically, for possible development of patella baja.
Acknowledgments
We thank the patient who is the subject of this report and who gave her consent for its publication.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution either has waived or does not require approval for the reporting of this case and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Aglietti P, Buzzi R, Vena LM, Baldini A, Mondaini A. High tibial valgus osteotomy for medial gonarthrosis: a 10- to 21-year study. J Knee Surg. 2003;16:21–26. [PubMed]
- 2.Almekinders LC. Early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop Relat Res. 1993;288:310–312. [DOI] [PubMed]
- 3.Bach BR Jr, Wojtys EM, Lindenfeld TN. Reflex sympathetic dystrophy, patella infera contracture syndrome, and loss of motion following anterior cruciate ligament surgery. Instr Course Lect. 1997;46:251–260. [PubMed]
- 4.Backstein D, Meisami B, Gross AE. Patella baja after the modified Coventry-Maquet high tibial osteotomy. J Knee Surg. 2003;16:203–208. [PubMed]
- 5.Benoit B, Laflamme GY, Laflamme GH, Rouleau D, Delisle J, Morin B. Long-term outcome of surgically-treated habitual patellar dislocation in children with coexistent patella alta: minimum follow-up of 11 years. J Bone Joint Surg Br. 2007;89:1172–1177. [DOI] [PubMed]
- 6.Brooker AF Jr, Brumback RJ. Brooker-Wills nails in treatment of infra-isthmal injuries of the femur. J Trauma. 1988;28:688–691. [DOI] [PubMed]
- 7.Brumback RJ, Reilly JP, Poka A, Lakatos RP, Bathon GH, Burgess AR. Intramedullary nailing of femoral shaft fractures. Part I: decision-making errors with interlocking fixation. J Bone Joint Surg Am. 1988;70:1441–1452. [PubMed]
- 8.Cameron HU, Jung YB. Patella baja complicating total knee arthroplasty: a report of two cases. J Arthroplasty. 1988;3:177–180. [PubMed]
- 9.Carmack DB, Moed BR, Kingston C, Zmurko M, Watson JT, Richardson M. Identification of the optimal intercondylar starting point for retrograde femoral nailing: an anatomic study. J Trauma. 2003;55:692–695. [DOI] [PubMed]
- 10.Chase JM, Hennrikus WL, Cullison TR. Patella infera following arthroscopic anterior cruciate ligament reconstruction. Contemp Orthop. 1994;28:487–493. [PubMed]
- 11.Cosgarea AJ, DeHaven KE, Lovelock JE. The surgical treatment of arthrofibrosis of the knee. Am J Sports Med. 1994;22:184–191. [DOI] [PubMed]
- 12.Hansen ST, Winquist RA. Closed intramedullary nailing of the femur: Kuntscher technique with reaming. Clin Orthop Relat Res. 1979;138:56–61. [PubMed]
- 13.Herscovici D Jr, Whiteman KW. Retrograde nailing of the femur using an intercondylar approach. Clin Orthop Relat Res. 1996;332:98–104. [DOI] [PubMed]
- 14.In Y, Kim SJ, Kwon YJ. Patellar tendon lengthening for patella infera using the Ilizarov technique. J Bone Joint Surg Br. 2007;89:398–400. [DOI] [PubMed]
- 15.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–104. [DOI] [PubMed]
- 16.Kastelec M, Veselko M. Inferior patellar pole avulsion fractures: osteosynthesis compared with pole resection. J Bone Joint Surg Am. 2004;86:696–701. [DOI] [PubMed]
- 17.Kempf I, Grosse A, Beck G. Closed locked intramedullary nailing: its application to comminuted fractures of the femur. J Bone Joint Surg Am. 1985;67:709–720. [PubMed]
- 18.Krupp RJ, Malkani AL, Goodin RA, Voor MJ. Optimal entry point for retrograde femoral nailing. J Orthop Trauma. 2003;17:100–105. [DOI] [PubMed]
- 19.Leggon RE, Feldmann DD. Retrograde femoral nailing: a focus on the knee. Am J Knee Surg. 2001;14:109–118. [PubMed]
- 20.Linclau L, Dokter G. Iatrogenic patella ‘baja.’ Acta Orthop Belg. 1984;50:75–80. [PubMed]
- 21.Mariani PP. A new surgical procedure for the treatment of patella infera. Knee Surg Sports Traumatol Arthrosc. 1994;2:238–241. [DOI] [PubMed]
- 22.Moed BR, Watson JT. Retrograde intramedullary nailing, without reaming, of fractures of the femoral shaft in multiply injured patients. J Bone Joint Surg Am. 1995;77:1520–1527. [DOI] [PubMed]
- 23.Moed BR, Watson JT. Retrograde nailing of the femoral shaft. J Am Acad Orthop Surg. 1999;7:209–216. [DOI] [PubMed]
- 24.Noyes FR, Wojtys EM, Marshall MT. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop Relat Res. 1991;265:241–252. [PubMed]
- 25.Ostrum RF, Agarwal A, Lakatos R, Poka A. Prospective comparison of retrograde and antegrade femoral intramedullary nailing. J Orthop Trauma. 2000;14:496–501. [DOI] [PubMed]
- 26.Ostrum RF, DiCicco J, Lakatos R, Poka A. Retrograde intramedullary nailing of femoral diaphyseal fractures. J Orthop Trauma. 1998;12:464–468. [DOI] [PubMed]
- 27.Paulos LE, Rosenberg TD, Drawbert J, Manning J, Abbott P. Infrapatellar contracture syndrome: an unrecognized cause of knee stiffness with patella entrapment and patella infera. Am J Sports Med. 1987;15:331–341. [DOI] [PubMed]
- 28.Paulos LE, Wnorowski DC, Greenwald AE. Infrapatellar contracture syndrome: diagnosis, treatment, and long-term followup. Am J Sports Med. 1994;22:440–449. [DOI] [PubMed]
- 29.Ricci WM, Bellabarba C, Evanoff B, Herscovici D, DiPasquale T, Sanders R. Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma. 2001;15:161–169. [DOI] [PubMed]
- 30.Sakai N, Koshino T, Okamoto R. Patella baja after displacement of tibial tuberosity for patellofemoral disorders. Bull Hosp Jt Dis. 1993;53:25–28. [PubMed]
- 31.Schwab JH, Agarwal P, Boland PJ, Kennedy JG, Healey JH. Patellar complications following distal femoral replacement after bone tumor resection. J Bone Joint Surg Am. 2006;88:2225–2230. [DOI] [PubMed]
- 32.Shaffer BS, Tibone JE. Patellar tendon length change after anterior cruciate ligament reconstruction using the midthird patellar tendon. Am J Sports Med. 1993;21:449–454. [DOI] [PubMed]
- 33.Shelbourne KD, Patel DV, Martini DJ. Classification and management of arthrofibrosis of the knee after anterior cruciate ligament reconstruction. Am J Sports Med. 1996;24:857–862. [DOI] [PubMed]
- 34.Tornetta P 3rd, Tiburzi D. Antegrade or retrograde reamed femoral nailing: a prospective, randomised trial. J Bone Joint Surg Br. 2000;82:652–654. [DOI] [PubMed]
- 35.Weale AE, Murray DW, Newman JH, Ackroyd CE. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br. 1999;81:790–795. [DOI] [PubMed]
- 36.Winquist RA, Hansen ST. Segmental fractures of the femur treated by closed intramedullary nailing. J Bone Joint Surg Am. 1978;60:934–939. [PubMed]
- 37.Winquist RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral fractures: a report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529–539. [PubMed]
- 38.Wolinsky PR, McCarty E, Shyr Y, Johnson K. Reamed intramedullary nailing of the femur: 551 cases. J Trauma. 1999;46:392–399. [DOI] [PubMed]
- 39.Wright JM, Heavrin B, Begg M, Sakyrd G, Sterett W. Observations on patellar height following opening wedge proximal tibial osteotomy. Am J Knee Surg. 2001;14:163–173. [PubMed]
- 40.Zuckerman JD, Veith RG, Johnson KD, Bach AW, Hansen ST, Solvik S. Treatment of unstable femoral shaft fractures with closed interlocking intramedullary nailing. J Orthop Trauma. 1987;1:209–218. [DOI] [PubMed]