Abstract
Full-thickness tears of the rotator cuff are common, but there is no clear consensus regarding indications for rotator cuff surgery. Because some patients with full-thickness rotator cuff tears who are asymptomatic or symptomatic can be successfully treated nonoperatively, clinical outcome studies of rotator cuff repair should describe the subjects in detail to allow appropriate interpretation of the results. However, we hypothesized the indications for surgery are poorly described in outcome studies of rotator cuff surgery. We undertook a detailed literature review over 11 years of six major orthopaedic journals to assess whether the indications for surgery were described adequately in studies of rotator cuff repair. Eighty-six papers fit the criteria for the study and were reviewed. Limitations of activities of daily living (31%), failure of nonoperative treatment (52%), duration of nonoperative treatment (26%), and history of nocturnal pain (16%) were reported in a minority of papers overall. The patients’ characteristics and indications for surgery were not described in a majority of clinical outcome studies of rotator cuff repair. It is important for these factors to be considered and reported because, without this information, the reasons for and results of rotator cuff repair are difficult to interpret.
Level of Evidence: Level III, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Full-thickness tears of the rotator cuff are common [76, 85, 97], but the indications for rotator cuff surgery have not been clearly described. A recent survey of American Academy of Orthopaedic Surgeons indicated considerable variations in practice patterns relating to the care of patients with rotator cuff tears [22]. Numerous nonoperative therapies are effective, including physical therapy, antiinflammatory medications, and cortisone injections [2, 11, 36, 44, 49, 93]. In 2004, there were an estimated 30,000 inpatient rotator cuff repairs performed in the United States, which represented approximately 20% of the total number of rotator cuff repairs [38]. Therefore, approximately 150,000 rotator cuff repairs were performed in the United States in 2004. This operation generally is judged beneficial for health-related quality of life [21, 61]. Because some patients with full-thickness cuff tears who are asymptomatic or symptomatic can be treated successfully nonoperatively, clinical outcome studies of rotator cuff repair should describe the subjects in detail to allow appropriate interpretation of the results.
Factors generally believed to affect outcome, and therefore the decision to perform elective rotator cuff repair, include size of the tear, duration of symptoms, failure of nonoperative treatment, duration of nonoperative treatment, nocturnal pain, history of trauma, and limitations of activities of daily living (ADL), not necessarily in that order [41]. Without detailed knowledge of these factors before surgery, it is difficult to interpret the outcome of the operation.
We hypothesized these factors, and therefore the indications for surgery, frequently are not described in outcome studies of rotator cuff surgery (ie, in less than 50% of papers). We undertook a detailed literature review of six leading orthopaedic journals to ascertain whether the indications for surgery actually are described in outcome studies of rotator cuff surgery.
Materials and Methods
The review was limited in scope to six journals we believed most likely to publish high-quality clinical studies of the outcome of rotator cuff surgery. These journals, The American Journal of Sports Medicine, Arthroscopy, Clinical Orthopaedics and Related Research, The Journal of Bone and Joint Surgery (American Volume), The Journal of Bone and Joint Surgery (British Volume), and The Journal of Shoulder and Elbow Surgery, were reviewed over an 11-year period to identify articles relating to the rotator cuff. We located 273 papers pertaining to rotator cuff surgery from 1995 through 2005 (inclusive). A manual search of the six journals was performed, and all articles with the term “rotator cuff, supraspinatus, subscapularis, infraspinatus, and teres minor” in the title or abstract were included. We excluded all papers that did not describe the results of rotator cuff repair surgery including those that were technique-focused, biomechanical studies, basic science research, or review articles (Table 1). There were 187 papers on the rotator cuff that were excluded, leaving 86 papers for inclusion in this study.
Table 1.
Reasons for exclusion of articles
| Explanation | Number of articles excluded (n = 187) |
|---|---|
| Biomechanical | 32 |
| Imaging | 26 |
| Technical note | 23 |
| Review article | 18 |
| Basic science | 15 |
| Case report | 14 |
| Anatomic study | 5 |
| Diagnosis | 4 |
| Epidemiologic study | 4 |
| Nonoperative care | 4 |
| Physical examination | 4 |
| Cuff not repaired | 3 |
| Tendon transfer | 3 |
| Current concepts review | 3 |
| Development of outcome measure | 3 |
| Not outcomes | 3 |
| Database research | 2 |
| Débridement | 2 |
| Electromyography | 2 |
| Postoperative pain management | 2 |
| Partial thickness | 2 |
| Treatment of infection | 2 |
| Finite element analysis | 1 |
| Latissimus transfer | 2 |
| Not clinical | 1 |
| Not cuff tear, only impingement | 1 |
| Observation study of anatomy | 1 |
| Questionnaire development | 1 |
| Reruptures only | 1 |
| Reverse total shoulder arthroplasty | 1 |
| Study of followup | 1 |
| Treatment of complications | 1 |
Two investigators (SKC, PK) independently reviewed the 86 papers, evaluating specific indications for rotator cuff surgery in each paper. The factors studied were history of trauma, limitation of ADL, failure of nonoperative treatment, duration of nonoperative treatment, nocturnal pain, size of the tear, and duration of symptoms. We ascertained whether each of the factors was described, as explained below. Documentation of a history of trauma reported or not reported was recorded for each paper. Papers that mentioned limitation of ADL were recorded. Instances of ADL limitation that were recorded included specific ADL scores presented in the paper or references to difficulties performing routine daily tasks before surgery. We recorded failure of nonoperative treatment, such as nonsteroidal antiinflammatory drugs (NSAIDs), steroid injections, physical therapy, activity modification, rest, and exercise. General references to nonoperative treatment also were recorded. The duration of nonoperative treatment before surgery was recorded, if applicable. Specific mention of whether patients awoke at night as a result of pain was recorded. In addition, any references to patients having pain during the night but not specifically waking at night because of pain were noted. For each paper, the investigators recorded any mention of the size of the rotator cuff tear. This included average size (in centimeters), range of sizes, or another classification for tear size, such as small, medium, large, and massive. The number of tendons involved in the tear was recorded if other size measurements were not reported. The length of symptoms before rotator cuff surgery was recorded.
Results
Of the 86 papers, only 38 (44%) mentioned whether the patients had history of trauma.
Limitations of ADL were described for 27 of the 86 papers (Table 2). Twenty-three papers reported a preoperative score that measures function and activity level (UCLA, Constant-Murley, Simple Shoulder Test, American Shoulder and Elbow Society) but did not specifically mention limitations of ADL (Table 3). Greater than 40% of the papers did not mention any physical limitations before rotator cuff surgery that impaired the patients’ ability to perform normal daily functions.
Table 2.
Limitations of ADL
| ADL limitations | Number of papers | Percentage of papers | References |
|---|---|---|---|
| ADL limitations reported | 27 | 31% | [7, 15, 18, 21, 23, 32, 33, 39, 40, 45, 50, 54, 58, 59, 61–63, 65, 68, 69, 71, 74, 78, 89–91, 96] |
| Only ADL or function score reported | 23 | 27% | [1, 6, 13, 27–30, 37, 42, 43, 47, 48, 60, 66, 70, 77, 82–84, 86–88, 92] |
| No mention of ADL | 36 | 42% | [3–5, 8–10, 12, 14, 16, 17, 19, 20, 24–26, 31, 34, 35, 46, 51–53, 55–57, 64, 67, 72, 73, 75, 79–81, 89, 94, 95, 98] |
ADL = activities of daily living.
Table 3.
Scoring systems used
| Scoring system | Frequency | References |
|---|---|---|
| Constant-Murley | 26 | [3–5, 8–10, 12, 19, 20, 24, 26–30, 32, 39, 48, 50, 51, 58, 59, 65, 72, 73, 89] |
| American Shoulder and Elbow Society | 25 | [3–5, 17, 20, 23, 27, 29–31, 39, 48, 59, 63, 64, 66–69, 74, 75, 78, 80, 82, 98] |
| UCLA | 41 | [1, 2, 10, 12, 14–17, 25, 29, 30, 34, 35, 39, 40, 42, 43, 45–47, 53–55, 57, 62, 63, 65, 70–73, 75, 77, 82–84, 92, 94–96, 98] |
| Simple Shoulder Test | 8 | [13, 33, 60, 73, 78, 79, 90, 91] |
| Visual analog scale | 7 | [3–6, 13, 20, 28] |
| Short Form-36 | 6 | [29, 30, 33, 59–61] |
| Other validated | 7 | [7, 25, 29, 30, 33, 42, 43, 51, 52, 59–61, 87] |
| Nonvalidated | 4 | [18, 21, 37, 81] |
| None | 2 | [56, 86] |
In 37 of the 86 papers, failure of nonoperative treatment for patients was reported and the specific types of nonoperative treatment also were noted. In eight of the papers, failure of nonoperative treatment was mentioned, but no specific treatment types were presented. In 41 papers, nearly ½ of the total, nonoperative treatment was not mentioned (Table 4). In all, 49 papers (57%) did not report the specific method of nonoperative treatment before surgery.
Table 4.
Failure of nonoperative treatment
| Nonoperative treatment | Number of papers | Percentage of papers | References |
|---|---|---|---|
| Specific nonoperative treatment reported | 37 | 43% | [3, 6, 10, 12, 13, 17, 18, 24, 25, 28–30, 37, 39, 45, 50, 51, 54, 58, 59, 61–63, 65, 67–69, 71, 74, 75, 77, 78, 80, 81, 90, 91, 96] |
| General nonoperative treatment reported | 8 | 9% | [1, 27, 32, 55, 86, 92, 94, 95] |
| No mention of nonoperative treatment | 41 | 48% | [4, 5, 7–9, 14–16, 19–21, 23, 26, 31, 33–35, 40, 42, 43, 46–48, 52, 53, 56, 57, 60, 64, 66, 70, 72, 73, 79, 82–84, 87–89, 98] |
Thirty-seven papers mentioned nonoperative treatment. Physical therapy, steroid injections, and NSAIDs were the most common types of nonoperative treatment (Table 5). Activity modification, rest, and exercise also were listed as nonoperative treatment options.
Table 5.
Types of nonoperative treatment (includes 37 papers)
| Type of nonoperative treatment | Frequency | References |
|---|---|---|
| Physical therapy | 32 | [3, 10, 12, 13, 17, 18, 25, 28–30, 37, 39, 45, 51, 54, 58, 59, 61–63, 65, 67–69, 74, 75, 77, 78, 80, 81, 90, 96] |
| Steroid injections | 26 | [3, 10, 12, 18, 28–30, 39, 45, 50, 58, 59, 61–63, 65, 67, 68, 74, 75, 78, 80, 81, 90, 91, 96] |
| Nonsteroidal antiinflammatory drugs | 24 | [3, 6, 12, 17, 18, 24, 28–30, 39, 45, 50, 58, 59, 61, 62, 65, 67–69, 71, 74, 75, 78] |
| Activity modification | 10 | [24, 29, 30, 37, 39, 45, 61, 62, 71, 91] |
| Rest | 6 | [6, 24, 37, 68, 71, 78] |
| Exercise | 4 | [6, 24, 71, 92] |
The duration of nonoperative treatment was reported for only 22 of the 86 papers. Of these papers, the most frequent duration of nonoperative treatment before surgery was a minimum of 3 months (Table 6). Four papers included patients with less than 3 months of nonoperative treatment, whereas four papers cited patients with a minimum of 6 months of nonoperative treatment before rotator cuff surgery. Two papers reported an average duration of nonoperative treatment of 5.5 months (range, 1–24 months) and 34.9 months (range, 1–144 months), respectively.
Table 6.
Distribution of nonoperative treatment duration
Only 14 papers of the 86 (16%) made reference to patients with pain at night. None of the papers reported patients waking at night because of pain.
Of the 86 papers included in the study, 49 papers reported the size of rotator cuff tears as small (< 1 cm), medium (1–3 cm), large (3–5 cm), or massive (> 5 cm). Seventeen of the papers reported an average size of the tear, whereas eight reported a range of tear sizes. Nine papers only reported the number of tendons in the tear and four used another sizing scale such as that of Boehm et al. [9] or Ide et al. [42]. Finally, 10 papers did not mention the size of the tear (Table 7).
Table 7.
Size of tear
| Size of tear | Number of papers | Percentage of papers | References |
|---|---|---|---|
| Reported as small, medium, large, or massive | 49 | 44% | [1, 3, 5, 7, 13, 14, 18, 20, 21, 23, 25, 26, 28, 30, 32, 34, 35, 37, 39, 40, 43, 45–47, 50, 52–55, 58, 59, 61–63, 65–68, 70–72, 75, 77–79, 81, 82, 96, 97] |
| Average size reported | 17 | 20% | [7, 12, 15, 20, 29, 31, 39, 48, 54–56, 59, 63, 74, 83, 84, 87] |
| Only number of tendons reported | 9 | 10% | [4, 8, 16, 33, 60, 63, 80, 86, 89] |
| Size reported in a range | 8 | 9% | [19, 27, 30, 51, 74, 83, 89, 93] |
| Other size scale reported | 4 | 5% | [9, 10, 42, 69] |
| Not reported | 10 | 12% | [6, 17, 24, 57, 64, 73, 89–91, 94, 95] |
The duration of symptoms before rotator cuff surgery was reported in 48 papers, whereas 44% (38 papers) did not mention the duration of symptoms.
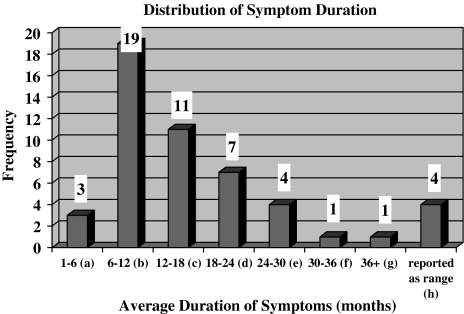
The distribution of symptom duration showed, in 19 of the 48 papers, the patients had an average duration of symptoms between 6 and 12 months (Fig. 1). Eleven papers reported patients with an average duration of symptoms between 12 and 18 months, whereas three papers reported an average duration between 1 and 6 months. Two papers [37, 87] reported the duration of symptoms for two separate groups of study patients. The duration of symptoms was reported as a range in four papers, with a duration greater than 3 months in three papers and greater than 6 months in one. The overall range of symptom duration before surgery was 1 to 244 months.
Fig. 1.
Distribution of symptom duration is shown (includes 48 papers). (a) References [6, 50, 69]; (b) References [12, 16, 17, 26, 39, 42, 43, 45, 47, 55, 61, 63, 65, 68, 72, 88–90, 92, 96]; (c) References [23, 24, 30, 40, 51, 75, 81, 83, 84, 87, 89]; (d) References [15, 29, 32, 67, 73, 80, 87]; (e) References [10, 18, 37, 66]; (f) Reference [58]; (g) Reference [37]; (h) References [13, 28, 71, 78].
Discussion
Numerous factors influence the decision to perform elective rotator cuff repair surgery. Although full-thickness tears of the rotator cuff are common, there seems to be no clear consensus regarding indications for rotator cuff surgery. Because some patients with full-thickness rotator cuff tears who are asymptomatic or symptomatic can be successfully treated nonoperatively, clinical outcome studies of rotator cuff repair should describe the subjects in detail to allow appropriate interpretation of the results. Based on our experience with the literature we hypothesized the indications for surgery are poorly described in outcome studies of rotator cuff surgery.
Limitations of this study include the fact that there may be other potential indicators for surgery that were not evaluated; however, we believe we included the most important factors. Additionally, the research was limited to six journals and was not a systematic review. As stated earlier, we limited our search to attempt to include the highest quality papers in the most frequently read and cited journals that publish studies relating to the rotator cuff.
We intentionally limited the scope of the review to the six journals we believed published the most detailed and comprehensive studies of rotator cuff surgery. Despite this, 44% of the papers did not discuss the duration of symptoms for the patients who underwent surgery. A majority of the papers included in this study did not report if there was a history of trauma or limitations of ADL. These factors, all important for the decision to perform the surgery, have been clearly underreported in outcome studies of rotator cuff surgery.
Nonoperative treatments such as physical therapy, NSAIDs, and steroid injections have beneficial effects for some patients with rotator cuff tears. Therefore, failure of nonoperative treatment is important to consider when evaluating the results of surgery. However, 41 of the 86 papers in this study do not mention nonoperative treatment of the cuff tears before surgery. Additionally, of the 45 papers that reported nonoperative management of rotator cuff tears, only 22 discussed the duration of nonoperative treatment. Although ½ of the papers did not mention whether patients had (with failed results) nonoperative treatment before having rotator cuff surgery, it is possible nonoperative treatment was administered but omitted from the paper. Without attempting nonoperative treatment for appropriate patients, there is the potential for patients whose rotator cuff problems could have been improved with nonoperative treatment to have had unnecessary surgery.
As seen through the analysis of 86 papers in this study, numerous important factors relating to the indications for surgery often are omitted from clinical studies of rotator cuff repair. It is important for all of these factors to be considered and reported because, without this information, the reasons for and the results of rotator cuff repair are difficult to interpret.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Baker CL, Liu SH. Comparison of open and arthroscopically assisted rotator cuff repairs. Am J Sports Med. 1995;23:99–104. [DOI] [PubMed]
- 2.Bartolozzi A, Andreychik D, Ahmad S. Determinants of outcome in the treatment of rotator cuff disease. Clin Orthop Relat Res. 1994;308:90–97. [PubMed]
- 3.Bennett WF. Arthroscopic repair of full-thickness supraspinatus tears (small-to-medium): a prospective study with 2- to 4-year follow-up. Arthroscopy. 2003;19:249–256. [DOI] [PubMed]
- 4.Bennett WF. Arthroscopic repair of isolated subscapularis tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003;19:131–143. [DOI] [PubMed]
- 5.Bennett WF. Arthroscopic repair of massive rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003;19:380–390. [DOI] [PubMed]
- 6.Blevins FT, Hayes WM, Warren RF. Rotator cuff injury in contact athletes. Am J Sports Med. 1996;24:263–267. [DOI] [PubMed]
- 7.Blevins FT, Warren RF, Cavo C, Altchek DW, Dines D, Palletta G, Wickiewicz TL. Arthroscopic assisted rotator cuff repair: results using a mini-open deltoid splitting approach. Arthroscopy. 1996;12:50–59. [DOI] [PubMed]
- 8.Boehm TD, Matzer M, Brazda D, Gohlke FE. Os acromiale associated with tear of the rotator cuff treated operatively: review of 33 patients. J Bone Joint Surg Br. 2003;85:545–549. [DOI] [PubMed]
- 9.Boehm TD, Werner A, Radtke S, Mueller T, Kirschner S, Gohlke F. The effect of suture materials and techniques on the outcome of repair of the rotator cuff: a prospective, randomised study. J Bone Joint Surg Br. 2005;87:819–823. [DOI] [PubMed]
- 10.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. [DOI] [PubMed]
- 11.Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res. 1993;294:103–110. [PubMed]
- 12.Boszotta H, Prunner K. Arthroscopically assisted rotator cuff repair. Arthroscopy. 2004;20:620–626. [DOI] [PubMed]
- 13.Buess E, Steuber KU, Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy. 2005;21:597–604. [DOI] [PubMed]
- 14.Burkhart SS, Danaceau SM, Pearce CE Jr. Arthroscopic rotator cuff repair: analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17:905–912. [DOI] [PubMed]
- 15.Burkhart SS, Tehrany AM. Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy. 2002;18:454–463. [DOI] [PubMed]
- 16.Checchia SL, Doneux PS, Miyazaki AN, Silva LA, Fregoneze M, Ossada A, Tsutida CY, Masiole C. Biceps tenodesis associated with arthroscopic repair of rotator cuff tears. J Shoulder Elbow Surg. 2005;14:138–144. [DOI] [PubMed]
- 17.Chen AL, Shapiro JA, Ahn AK, Zuckerman JD, Cuomo F. Rotator cuff repair in patients with type I diabetes mellitus. J Shoulder Elbow Surg. 2003;12:416–421. [DOI] [PubMed]
- 18.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears: a prospective long-term study. J Bone Joint Surg Am. 2001;83:71–77. [DOI] [PubMed]
- 19.Cummins CA, Strickland S, Appleyard RC, Szomor ZL, Marshall J, Murrell GA. Rotator cuff repair with bioabsorbable screws: an in vivo and ex vivo investigation. Arthroscopy. 2003;19:239–248. [DOI] [PubMed]
- 20.Davidson PA, Rivenburgh DW. Rotator cuff repair tension as a determinant of functional outcome. J Shoulder Elbow Surg. 2000;9:502–506. [DOI] [PubMed]
- 21.Djurasovic M, Marra G, Arroyo JS, Pollock RG, Flatow EL, Bigliani LU. Revision rotator cuff repair: factors influencing results. J Bone Joint Surg Am. 2001;83:1849–1855. [DOI] [PubMed]
- 22.Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF, Marx RG. Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am. 2005;87:1978–1984. [DOI] [PubMed]
- 23.Duralde XA, Bair B. Massive rotator cuff tears: the result of partial rotator cuff repair. J Shoulder Elbow Surg. 2005;14:121–127. [DOI] [PubMed]
- 24.Edwards TB, Walch G, Sirveaux F, Mole D, Nove-Josserand L, Boulahia A, Neyton L, Szabo I, Lindgren B. Repair of tears of the subscapularis. J Bone Joint Surg Am. 2005;87:725–730. [DOI] [PubMed]
- 25.Fealy S, Kingham TP, Altchek DW. Mini-open rotator cuff repair using a two-row fixation technique: outcomes analysis in patients with small, moderate, and large rotator cuff tears. Arthroscopy. 2002;18:665–670. [DOI] [PubMed]
- 26.Fokter SK, Cicak N, Skorja J. Functional and electromyographic results after open rotator cuff repair. Clin Orthop Relat Res. 2003;415:121–130. [DOI] [PubMed]
- 27.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224. [DOI] [PubMed]
- 28.Galatz LM, Griggs S, Cameron BD, Iannotti JP. Prospective longitudinal analysis of postoperative shoulder function: a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2001;83:1052–1056. [PubMed]
- 29.Gartsman GM, Brinker MR, Khan M. Early effectiveness of arthroscopic repair for full-thickness tears of the rotator cuff: an outcome analysis. J Bone Joint Surg Am. 1998;80:33–40. [DOI] [PubMed]
- 30.Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 1998;80:832–840. [DOI] [PubMed]
- 31.Gartsman GM, O’Connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes. J Shoulder Elbow Surg. 2004;13:424–426. [DOI] [PubMed]
- 32.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. [DOI] [PubMed]
- 33.Goldberg BA, Lippitt SB, Matsen FA 3rd. Improvement in comfort and function after cuff repair without acromioplasty. Clin Orthop Relat Res. 2001;390:142–150. [DOI] [PubMed]
- 34.Grondel RJ, Savoie FH 3rd, Field LD. Rotator cuff repairs in patients 62 years of age or older. J Shoulder Elbow Surg. 2001;10:97–99. [DOI] [PubMed]
- 35.Hata Y, Saitoh S, Murakami N, Seki H, Nakatsuchi Y, Takaoka K. A less invasive surgery for rotator cuff tear: mini-open repair. J Shoulder Elbow Surg. 2001;10:11–16. [DOI] [PubMed]
- 36.Hawkins RH, Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop Relat Res. 1995;321:178–188. [PubMed]
- 37.Hawkins RJ, Morin WD, Bonutti PM. Surgical treatment of full-thickness rotator cuff tears in patients 40 years of age or younger. J Shoulder Elbow Surg. 1999;8:259–265. [DOI] [PubMed]
- 38.HCUPnet: Healthcare Cost and Utilization Project. Available at: http://www.hcupnet.ahrq.gov. Accessed January 15, 2007.
- 39.Hersch JC, Sgaglione NA. Arthroscopically assisted mini-open rotator cuff repairs: functional outcome at 2- to 7-year follow-up. Am J Sports Med. 2000;28:301–311. [DOI] [PubMed]
- 40.Hoellrich RG, Gasser SI, Morrison DS, Kurzweil PR. Electromyographic evaluation after primary repair of massive rotator cuff tears. J Shoulder Elbow Surg. 2005;14:269–272. [DOI] [PubMed]
- 41.Iannotti JP. Full-thickness rotator cuff tears: factors affecting surgical outcome. J Am Acad Orthop Surg. 1994;2:87–95. [DOI] [PubMed]
- 42.Ide J, Maeda S, Takagi K. Arthroscopic transtendon repair of partial-thickness articular-side tears of the rotator cuff: anatomical and clinical study. Am J Sports Med. 2005;33:1672–1679. [DOI] [PubMed]
- 43.Ide J, Maeda S, Takagi K. A comparison of arthroscopic and open rotator cuff repair. Arthroscopy. 2005;21:1090–1098. [DOI] [PubMed]
- 44.Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res. 1992;275:165–173. [PubMed]
- 45.Jones CK, Savoie FH 3rd. Arthroscopic repair of large and massive rotator cuff tears. Arthroscopy. 2003;19:564–571. [DOI] [PubMed]
- 46.Kessler KJ, Bullens-Borrow AE, Zisholtz J. LactoSorb plates for rotator cuff repair. Arthroscopy. 2002;18:279–283. [DOI] [PubMed]
- 47.Kim SH, Ha KI, Park JH, Kang JS, Oh SK, Oh I. Arthroscopic versus mini-open salvage repair of the rotator cuff tear: outcome analysis at 2 to 6 years’ follow-up. Arthroscopy. 2003;19:746–754. [DOI] [PubMed]
- 48.Klepps S, Bishop J, Lin J, Cahlon O, Strauss A, Hayes P, Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722. [DOI] [PubMed]
- 49.Krabak BJ, Sugar R, McFarland EG. Practical nonoperative management of rotator cuff injuries. Clin J Sport Med. 2003;13:102–105. [DOI] [PubMed]
- 50.Kronberg M, Wahlstrom P, Brostrom LA. Shoulder function after surgical repair of rotator cuff tears. J Shoulder Elbow Surg. 1997;6:125–130. [DOI] [PubMed]
- 51.Lam F, Mok D. Open repair of massive rotator cuff tears in patients aged sixty-five years or over: is it worthwhile? J Shoulder Elbow Surg. 2004;13:517–521. [DOI] [PubMed]
- 52.Lastayo PC, Wright T, Jaffe R, Hartzel J. Continuous passive motion after repair of the rotator cuff: a prospective outcome study. J Bone Joint Surg Am. 1998;80:1002–1011. [DOI] [PubMed]
- 53.Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004;20:22–33. [DOI] [PubMed]
- 54.Lo IK, Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy. 2004;20:250–267. [DOI] [PubMed]
- 55.Lo IK, Parten PM, Burkhart SS. Combined subcoracoid and subacromial impingement in association with anterosuperior rotator cuff tears: an arthroscopic approach. Arthroscopy. 2003;19:1068–1078. [DOI] [PubMed]
- 56.Malcarney HL, Bonar F, Murrell GA. Early inflammatory reaction after rotator cuff repair with a porcine small intestine submucosal implant: a report of 4 cases. Am J Sports Med. 2005;33:907–911. [DOI] [PubMed]
- 57.Mallon WJ, Misamore G, Snead DS, Denton P. The impact of preoperative smoking habits on the results of rotator cuff repair. J Shoulder Elbow Surg. 2004;13:129–132. [DOI] [PubMed]
- 58.Massoud SN, Levy O, Copeland SA. Subacromial decompression: treatment for small- and medium-sized tears of the rotator cuff. J Bone Joint Surg Br. 2002;84:955–960. [DOI] [PubMed]
- 59.McBirnie JM, Miniaci A, Miniaci SL. Arthroscopic repair of full-thickness rotator cuff tears using bioabsorbable tacks. Arthroscopy. 2005;21:1421–1427. [DOI] [PubMed]
- 60.McCallister WV, Parsons IM, Titelman RM, Matsen FA 3rd. Open rotator cuff repair without acromioplasty. J Bone Joint Surg Am. 2005;87:1278–1283. [DOI] [PubMed]
- 61.McKee MD, Yoo DJ. The effect of surgery for rotator cuff disease on general health status: results of a prospective trial. J Bone Joint Surg Am. 2000;82:970–979. [DOI] [PubMed]
- 62.Misamore GW, Ziegler DW, Rushton JL 2nd. Repair of the rotator cuff: a comparison of results in two populations of patients. J Bone Joint Surg Am. 1995;77:1335–1339. [DOI] [PubMed]
- 63.Murray TF Jr, Lajtai G, Mileski RM, Snyder SJ. Arthroscopic repair of medium to large full-thickness rotator cuff tears: outcome at 2- to 6-year follow-up. J Shoulder Elbow Surg. 2002;11:19–24. [DOI] [PubMed]
- 64.O’Holleran JD, Kocher MS, Horan MP, Briggs KK, Hawkins RJ. Determinants of patient satisfaction with outcome after rotator cuff surgery. J Bone Joint Surg Am. 2005;87:121–126. [DOI] [PubMed]
- 65.Pai VS, Lawson DA. Rotator cuff repair in a district hospital setting: outcomes and analysis of prognostic factors. J Shoulder Elbow Surg. 2001;10:236–241. [DOI] [PubMed]
- 66.Park JY, Chung KT, Yoo MJ. A serial comparison of arthroscopic repairs for partial- and full-thickness rotator cuff tears. Arthroscopy. 2004;20:705–711. [DOI] [PubMed]
- 67.Park JY, Levine WN, Marra G, Pollock RG, Flatow EL, Bigliani LU. Portal-extension approach for the repair of small and medium rotator cuff tears. Am J Sports Med. 2000;28:312–316. [DOI] [PubMed]
- 68.Payne LZ, Altchek DW, Craig EV, Warren RF. Arthroscopic treatment of partial rotator cuff tears in young athletes: a preliminary report. Am J Sports Med. 1997;25:299–305. [DOI] [PubMed]
- 69.Popowitz RL, Zvijac JE, Uribe JW, Hechtman KS, Schurhoff MR, Green JB. Rotator cuff repair in spinal cord injury patients. J Shoulder Elbow Surg. 2003;12:327–332. [DOI] [PubMed]
- 70.Rebuzzi E, Coletti N, Schiavetti S, Giusto F. Arthroscopic rotator cuff repair in patients older than 60 years. Arthroscopy. 2005;21:48–54. [DOI] [PubMed]
- 71.Rokito AS, Cuomo F, Gallagher MA, Zuckerman JD. Long-term functional outcome of repair of large and massive chronic tears of the rotator cuff. J Bone Joint Surg Am. 1999;81:991–997. [DOI] [PubMed]
- 72.Romeo AA, Hang DW, Bach BR Jr, Shott S. Repair of full thickness rotator cuff tears: gender, age, and other factors affecting outcome. Clin Orthop Relat Res. 1999;367:243–255. [DOI] [PubMed]
- 73.Romeo AA, Mazzocca A, Hang DW, Shott S, Bach BR Jr. Shoulder scoring scales for the evaluation of rotator cuff repair. Clin Orthop Relat Res. 2004;427:107–114. [DOI] [PubMed]
- 74.Sauerbrey AM, Getz CL, Piancastelli M, Iannotti JP, Ramsey ML, Williams GR Jr. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcome. Arthroscopy. 2005;21:1415–1420. [DOI] [PubMed]
- 75.Severud EL, Ruotolo C, Abbott DD, Nottage WM. All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy. 2003;19:234–238. [DOI] [PubMed]
- 76.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15. [DOI] [PubMed]
- 77.Shinners TJ, Noordsij PG, Orwin JF. Arthroscopically assisted mini-open rotator cuff repair. Arthroscopy. 2002;18:21–26. [DOI] [PubMed]
- 78.Smith AM, Sperling JW, Cofield RH. Rotator cuff repair in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2005;87:1782–1787. [DOI] [PubMed]
- 79.Sonnabend DH, Watson EM. Structural factors affecting the outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002;11:212–218. [DOI] [PubMed]
- 80.Sonnery-Cottet B, Edwards TB, Noel E, Walch G. Rotator cuff tears in middle-aged tennis players: results of surgical treatment. Am J Sports Med. 2002;30:558–564. [DOI] [PubMed]
- 81.Sperling JW, Cofield RH, Schleck C. Rotator cuff repair in patients fifty years of age and younger. J Bone Joint Surg Am. 2004;86:2212–2215. [DOI] [PubMed]
- 82.Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–1316. [DOI] [PubMed]
- 83.Tauro JC. Arthroscopic rotator cuff repair: analysis of technique and results at 2- and 3-year follow-up. Arthroscopy. 1998;14:45–51. [DOI] [PubMed]
- 84.Tauro JC. Arthroscopic repair of large rotator cuff tears using the interval slide technique. Arthroscopy. 2004;20:13–21. [DOI] [PubMed]
- 85.Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296–299. [DOI] [PubMed]
- 86.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;344:275–283. [DOI] [PubMed]
- 87.Trenerry K, Walton JR, Murrell GA. Prevention of shoulder stiffness after rotator cuff repair. Clin Orthop Relat Res. 2005;430:94–99. [DOI] [PubMed]
- 88.Vives MJ, Miller LS, Rubenstein DL, Taliwal RV, Becker CE. Repair of rotator cuff tears in golfers. Arthroscopy. 2001;17:165–172. [DOI] [PubMed]
- 89.Warner JJ, Higgins L, Parsons IM, Dowdy P. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001;10:37–46. [DOI] [PubMed]
- 90.Warner JJ, Tetreault P, Lehtinen J, Zurakowski D. Arthroscopic versus mini-open rotator cuff repair: a cohort comparison study. Arthroscopy. 2005;21:328–332. [DOI] [PubMed]
- 91.Watson EM, Sonnabend DH. Outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002;11:201–211. [DOI] [PubMed]
- 92.Wilson F, Hinov V, Adams G. Arthroscopic repair of full-thickness tears of the rotator cuff: 2- to 14-year follow-up. Arthroscopy. 2002;18:136–144. [DOI] [PubMed]
- 93.Wirth MA, Basamania C, Rockwood CA Jr. Nonoperative management of full-thickness tears of the rotator cuff. Orthop Clin North Am. 1997;28:59–67. [DOI] [PubMed]
- 94.Wolf EM, Pennington WT, Agrawal V. Arthroscopic rotator cuff repair: 4- to 10-year results. Arthroscopy. 2004;20:5–12. [DOI] [PubMed]
- 95.Wolf EM, Pennington WT, Agrawal V. Arthroscopic side-to-side rotator cuff repair. Arthroscopy. 2005;21:881–887. [DOI] [PubMed]
- 96.Worland RL, Arredondo J, Angles F, Lopez-Jimenez F. Repair of massive rotator cuff tears in patients older than 70 years. J Shoulder Elbow Surg. 1999;8:26–30. [DOI] [PubMed]
- 97.Worland RL, Lee D, Orozco CG, SozaRex F, Keenan J. Correlation of age, acromial morphology, and rotator cuff tear pathology diagnosed by ultrasound in asymptomatic patients. J South Orthop Assoc. 2003;12:23–26. [PubMed]
- 98.Youm T, Murray DH, Kubiak EN, Rokito AS, Zuckerman JD. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg. 2005;14:455–459. [DOI] [PubMed]