Abstract
Introduction: The ablation of supraventricular tachycardias (SVT) using radiofrequency energy (RF) is a procedure with a high primary success rate. However, there is a scarcity of data regarding the long term outcome, particularly with respect to quality of life (QoL).
Methods and Results: In this retrospective single-center study, 454 patients who underwent ablation of SVT between 2002 and 2007 received a detailed questionnaire addressing matters of QoL. The questionnaire was a modified version of the SF-36 Health Survey questionnaire and the Symptom Checklist – Frequency and Severity Scale.
After a mean follow up of 4.5±1.3 years, 309 (68.1%) of the contacted 454 patients (269 female, 59.2%, mean age 58+/-6.5) completed the questionnaire. Despite of 27% of relapses in the study group, 91.7% considered the procedure a long-term success. The remainder of patients experienced no change in (3.7%) or worsening of (4.7%) symptoms. There were no significant differences between the various types of SVT (p=1). QoL in patients with Atrio-Ventricular Nodal Reentry Tachycardia (AVNRT) and Atrio-Ventricular Reentry Tachycardia (AVRT) improved significantly (p<0.0005 respectively p<0.043), whereas QoL in patients with Ectopic Atrial Tachycardia (EAT) showed a non-significant trend towards improvement. Main symptoms before ablation, such as tachycardia (91.5%), increased incidence of tachycardia episodes over time (78.1%), anxiety (55.5%) and reduced physical capacity in daily life (52%) were significantly improved after ablation (p<0.0001).
Conclusion: The high acute ablation success of SVT persists for years in long term follow up and translates into a significant improvement of QoL in most patients.
Keywords: Quality of Life, Ablation, SVT, Atrium, Radio Frequency
Introduction
RF catheter ablation of SVT is a well-established treatment in invasive electrophysiology with a primary success rate of more than 90% in all substrates. SVT ablation specifically targets the electroanatomical substrate, such as the slow pathway in AVNRT, the accessory pathway in AVRT or an ectopic focus in EAT.
Oftentimes, these specific SVT are difficult to treat medically due to therapy refractoriness. Therefore, RF ablation has become the treatment of choice due to its high primary success rate and low complication rate 1-6.
Patients with paroxysmal SVT often present with symptoms like palpitations, dyspnea, fatigue, chest pain or worsening of heart failure under physical or emotional stress. Heart rates of 200 beats per minute and more are not uncommon, especially in young patients or in patients with AVRT and associated atrial fibrillation (AF). Recurrent syncope or other life-threatening complications like ventricular tachycardia and/or ventricular fibrillation may occur.
Due to the paroxysmal character of the tachycardia, with sudden unexpected onset of symptoms, patients are limited in their daily life concerning work, social events and sports. Due to this nature of the disease QoL is increasingly impaired over time. Despite of the high immediate success rate of SVT catheter ablation, very little data is available concerning the development of QoL in the long-term. The published literature mainly deals with the electrophysiological long term results of RF ablation. So far, QoL before and after ablation has not been systematically investigated in these patients 7-13. In contrast, other SVT like atrial flutter and AF have been intensively investigated under this aspect 14-23.
Methods
Study population
All patients included either had a typical history of a paroxysmal on-off tachycardia or documented narrow complex SVT pattern in a twelve lead ECG. They consecutively underwent an electrophysiological study. If an AVNRT, AVRT or EAT could be induced and ablated with primary success, patients were later selected for participation in this retrospective single-center study.
All 454 patients, (59.2% female, 40.8% male, mean age 58 (+/- 16.5) years) who had undergone RF catheter ablation for AVNRT, AVRT or EAT at our institution between 2002 and 2007 were mailed a detailed questionnaire. This questionnaire was a version of the SF-36 Health Survey questionnaire and the Symptom Checklist-Frequency and Severity Scale, modified to specifically reflect questions of QoL in SVT, enabling the authors to translate the various domains and components of well being into a quantitative value.
For reasons of structure and to simplify answering for the patients we divided the questionnaire in three different blocks: the first block was related to the situation for the patients before ablation, questions in the second block dealt with the situation during ablation and the third block exclusively applied to the post ablation period.
The modified version of the SF-36 consists of a 36 item questionnaire that assesses eight health concepts: general health perception, physical functioning, social functioning, role limitations due to physical problems, bodily pain, mental health, role limitations due to emotional problems, and vitality. In addition the SF-36 also generates physical and mental component summery scores.
Irrespective of the well known shortcomings of the Symptom checklist because of the nonspecific nature of a number of the symptoms asked for and the lack of assessment of functional status the Symptom checklist is straightforward to use, sensitive to change, and has been utilized in a growing number of studies concerning arrhythmias. We asked for specific symptoms e.g. as tachycardia, palpitations, dyspnea, anxiety and angina pectoris.
If no response had been received after 4 weeks, the patients were contacted by telephone and asked to participate. 309 (68.1%) of the contacted 454 patients fully completed the questionnaire. 145 (31.9%) patients had to be excluded due to incomplete or incoherent answers or because they completely failed to participate. Patients suffering from new palpitations and SVT were contacted for a second time and were asked to additionally submit a recent 12 lead ECG for analysis.
Electrophysiological study and radiofrequency catheter ablation
In all patients, a standard setting with four diagnostic catheters was used (high right atrium, HIS bundle region, right ventricular apex and coronary sinus). Before ablation, the underlying clinical tachycardia had to be able to be repeatedly induced before detailed mapping and the ablation maneuvers were performed. The ablation itself was performed in sinus rhythm in most cases or under continuing tachycardia, if so required for mapping.
The ablation itself was performed using either an irrigated tip or a conventional tip ablation catheter. Successful ablation was defined as the non-reinducibility of the native tachycardia or the loss of the delta wave in AVRT. Subsequently, further electrophysiological testing for additional tachycardias, which could potentially have been masked by the now ablated primary tachycardia, was performed. The aforementioned endpoints were re-evaluated after a waiting period of at least 20 minutes.
Statistical Analysis
For the description of the metric variables the results are expressed as number, mean, standard deviation (SDA) and extreme (minimum and maximum), quartile (25. and 75. percentile) and median. The distribution of categorical data is expressed by absolute and relative frequency.
The comparison of the distribution of the categorical variables before and after ablation concerning two variables was expressed by the McNemar Test. More than two variables were compared using the Chi-square-distribution. For the comparison of the distribution of categorical and ordinal variables of independent random samplings we used Fisher's exact test. If the Gaussian distribution acceptation was declined, we used a non-parametric test for differences in groups the Mann Whitney U Test or the Kruskal-Wallis-Test, otherwise the t- or F-test.
Results
Study population
309 (68.1%) patients were included into the study. In 230 of the 309 patients the SVT substrate was an AVNRT (74.4%), in 66 patients an AVRT (21.4%) and in 13 patients an EAT (4.2%). The distribution between the sexes (female/male) in AVNRT was 62.2/37.8, in AVRT 50/50 and in EAT 53.9/46.2. Mean age was 58 (±16.5) for the whole study group, 62 (±15.3) for AVNRT, 48 (±17.6) for AVRT and 63 (±13.3) for EAT. With respect to the underlying tachycardia, 66.9% of patients with AVNRT, 75% of patients with AVRT and 59.1% of patients with EAT respectively submitted a fully completed questionnaire.
Time to diagnosis, time to ablation, baseline data of ablation
Regarding the time interval between the first occurrence of the tachycardia, its diagnosis and the year of ablation, we found significant differences. Regarding the whole study cohort, the underlying SVT was diagnosed 9.1±11.2 years (25%/75% percentile - 1.0/15.0) and ablated 14.4±12.7 years (25%/75% percentile - 3.0/24.0) after the first episode of tachycardia. These time intervals (time to diagnosis/time to ablation) differed between the specific SVT (Table 1). The time interval between the first occurrence of the tachycardia and the diagnosis in AVRT was therefore significantly shorter compared to the AVNRT patients (p<0.05); however, the earlier diagnosis of AVRT did not lead to earlier ablation as well.
Table 1.
Baseline demographic characteristics and procedural findings in 309 patients with completed questionnaire.
| Patients | Numbers/percentage |
|---|---|
| Patients included | 309 - 68% |
| Female | 269 - 59% |
| Male | 185 - 41% |
| AVNRT | 230 - 74% |
| AVRT | 66 - 66% |
| EAT | 13 - 4% |
| From symptom to diagnosis (Years) | Total - 25%/75% perc. |
| All patients | 9.1±11.2 - 1.0/15.0 |
| AVNRT | 10.3±11.9 - 1.0/18.0 |
| AVRT | 4.7±7.2 - 0.0/9.0 |
| EAT | 7.5±8.7 - 0.0/18.0 |
| From symptom to ablation (Years) | |
| All patients | 14.4±12.7 - 3.0/24 |
| AVNRT | 15.0±13.3 - 3.0/25.0 |
| AVRT | 12.3±10.0 - 3.0/20 |
| EAT | 10.9±7.4 - 6.0/18.0 |
| RF-Applications (Number) | |
| All patients | 7.3±6.7 - 3.0/8.5 |
| AVNRT | 7.4±6.9 - 3.0/8.0 |
| AVRT | 6.8±6.5 - 2.0/10 |
| EAT | 8.0±3.6 - 6.0/9.0 |
| Examination time (Minutes) | |
| All patients | 141.3±55.6 - 100/170 |
| AVNRT | 134.3±52.4 - 96/160 |
| AVRT | 156.1±58.7 - 117.5/193.5 |
| EAT | 189.5±59.7 - 135/240 |
| Fluoroscop time (Minutes) | |
| All patients | 19.0±13.9 - 10.8/22.8 |
| AVNRT | 16.4±11.0 - 10.4/19.2 |
| AVRT | 25.5±19.2 - 12.3/31.9 |
| EAT | 30.5±11.4 - 21.7/35.1 |
Baseline data of the ablation procedure comparing the number of RF burns, the total examination time and the fluoroscopy duration are summarized in Table 1. There were no significant differences between the different types of SVT.
Quality of life and specific symptoms due to tachycardia prior to ablation
In the questionnaire, all patients were asked to state their symptoms and grade them on a severity scale. We inquired about the nature and quantity of tachycardia and the associated symptoms. Furthermore, the effect of symptoms on the patients` daily and social life, especially with respect to abstinence from work, sports and hobbies was surveyed.
Patients were asked to assess the changes in daily and social life prior to the ablation procedure itself using a 5-level ranking scale (extreme, very strong, strong, moderate, low). In total, more than 60% of the patients (178, 60.7%) stated a strong to extreme impairment in daily life, whereas the rest of the patients (94, 29.3%) indicated only moderate or little changes due to the tachycardia. The detailed results are listed in Table 2.
Table 2.
Distribution of symptoms prior to ablation for AVNRT-, AVRT-and EAT patients. Panel A: Quantity and duration of episodes and the associated symptoms. Panel B: Detraction in daily life generally and in parts of daily life.
| AVNRT | AVRT | EAT | |||||
|---|---|---|---|---|---|---|---|
| variable | Value | N | % | N | % | N | % |
| PANAL A | |||||||
| Detraction in daily life | Extreme | 27 | 12.5 | 6 | 9.2 | 6 | 46.1 |
| Very strong | 49 | 22.8 | 16 | 24.6 | 3 | 23.1 | |
| Strong | 57 | 26.5 | 13 | 20.0 | 1 | 7.7 | |
| Moderate | 46 | 21.4 | 10 | 15.4 | 2 | 15.4 | |
| Low | 26 | 12.1 | 9 | 13.9 | 1 | 7.7 | |
| none | 10 | 4.7 | 11 | 16.9 | 0 | 0 | |
| Limited in Business/school | Yes | 5 | 20.0 | 19 | 38.0 | 1 | 11.1 |
| no | 20 | 80.0 | 31 | 62.0 | 8 | 88.9 | |
| Limited in sports | Yes | 33 | 22.8 | 16 | 30.2 | 1 | 10.0 |
| No | 112 | 77.2 | 37 | 69.8 | 9 | 90.0 | |
| Limited in hobbies | Yes | 35 | 31.3 | 21 | 48.8 | 2 | 18.2 |
| No | 77 | 68.8 | 22 | 51.2 | 9 | 81.8 | |
| Limited in Garden work | Yes | 39 | 30.2 | 20 | 48.8 | 2 | 18.2 |
| No | 90 | 69.8 | 21 | 51.2 | 9 | 81.8 | |
| Limited in Work at home | Yes | 4 | 16.0 | 18 | 43.9 | 2 | 20.0 |
| No | 21 | 84.0 | 23 | 56.1 | 8 | 80.0 | |
| Limited in Social life | Yes | 8 | 38.1 | 20 | 52.6 | 0 | 0 |
| No | 13 | 61.9 | 18 | 47.4 | 9 | 100 | |
| Limited in others | Yes | 70 | 30.4 | 9 | 13.6 | 6 | 46.2 |
| no | 160 | 69.6 | 57 | 86.4 | 7 | 53.8 | |
| PANAL B | |||||||
| Detraction in daily life | Extreme | 27 | 12.5 | 6 | 9.2 | 6 | 46.1 |
| Very strong | 49 | 22.8 | 16 | 24.6 | 3 | 23.1 | |
| Strong | 57 | 26.5 | 13 | 20.0 | 1 | 7.7 | |
| Moderate | 46 | 21.4 | 10 | 15.4 | 2 | 15.4 | |
| Low | 26 | 12.1 | 9 | 13.9 | 1 | 7.7 | |
| none | 10 | 4.7 | 11 | 16.9 | 0 | 0 | |
| Limited in Business/school | Yes | 5 | 20.0 | 19 | 38.0 | 1 | 11.1 |
| no | 20 | 80.0 | 31 | 62.0 | 8 | 88.9 | |
| Limited in sports | Yes | 33 | 22.8 | 16 | 30.2 | 1 | 10.0 |
| No | 112 | 77.2 | 37 | 69.8 | 9 | 90.0 | |
| Limited in hobbies | Yes | 35 | 31.3 | 21 | 48.8 | 2 | 18.2 |
| No | 77 | 68.8 | 22 | 51.2 | 9 | 81.8 | |
| Limited in Garden work | Yes | 39 | 30.2 | 20 | 48.8 | 2 | 18.2 |
| No | 90 | 69.8 | 21 | 51.2 | 9 | 81.8 | |
| Limited in Work at home | Yes | 4 | 16.0 | 18 | 43.9 | 2 | 20.0 |
| No | 21 | 84.0 | 23 | 56.1 | 8 | 80.0 | |
| Limited in Social life | Yes | 8 | 38.1 | 20 | 52.6 | 0 | 0 |
| No | 13 | 61.9 | 18 | 47.4 | 9 | 100 | |
| Limited in others | Yes | 70 | 30.4 | 9 | 13.6 | 6 | 46.2 |
| no | 160 | 69.6 | 57 | 86.4 | 7 | 53.8 | |
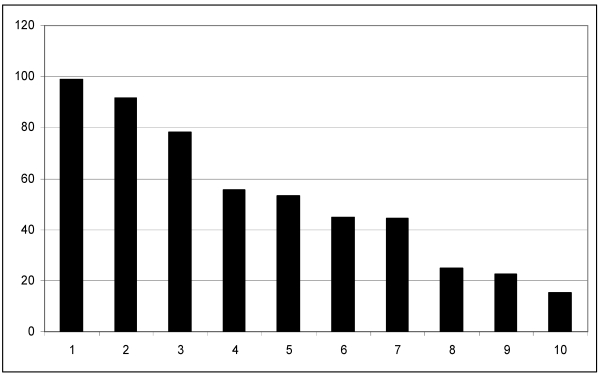
Regarding the whole study population prior to ablation, 305 patients (99.0%) had specific symptoms. The main reasons for patients seeking therapy were tachycardic palpitations (281 patients, 91.5%) and increasing incidence of episodes (224 patients, 78.1%). In descending order, patients as well complained of anxiety (171 patients, 55.5%), reduced work capacity (164 pts., 53.3%), dyspnea (138 patients, 44.8%) and angina pectoris (137 patients, 44.5%). Symptoms such as palpitations (77 patients, 25%), ophthalmic fibrillation (70 pts., 22.7%) and syncope (47 patients, 15.4%) were relatively infrequent (Table 1, Figure 1).
Figure 1.
Symptoms leading patients to therapy: X-axis: Symptoms in declinary order. (1) Overall symptoms without specification, (2) tachycardia, (3) increase of episodes over the years, (4) anxiety, (5) reduction in capacity, (6) dyspnea, (7) angina pectoris, (8) palpitations, (9) ophthalmic fibrillation, (10) syncope. Y-axis: percentage of patients presenting these symptom.
Ablation success rate
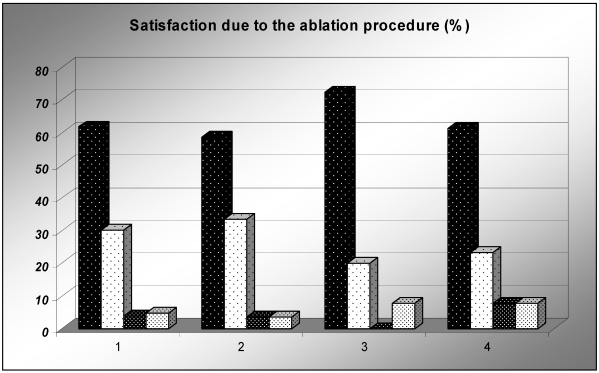
Independent of symptoms, the patients had to rate the perceived success of the ablation procedure in general (very successful, successful, moderately successful or not successful). The majority of patients rated the ablation procedure “very successful” or “successful”. This is true for the whole study population as well as for each SVT subgroup. Details are given in Figure 2.
Figure 2.
Satisfaction due to the ablation procedure. X-axis: (1) All patients, (2) AVNRT, (3) AVRT, (4) EAT. Pillars from left to right: very successful (black pillar), successful (white pillar), moderate (dark grey), not successful (light grey). Y-axis: Percentage of patients.
Comparison of quality of life before and after ablation
The general QoL and QoL with respect to the above mentioned symptoms were retrospectively evaluated before and after ablation. The aforementioned questionnaires included a section asking participants to grade their well-being using a six-level ranking scale (very good (1), good (2), satisfactory (3), sufficient (4), defective (5) and insufficient (6)).
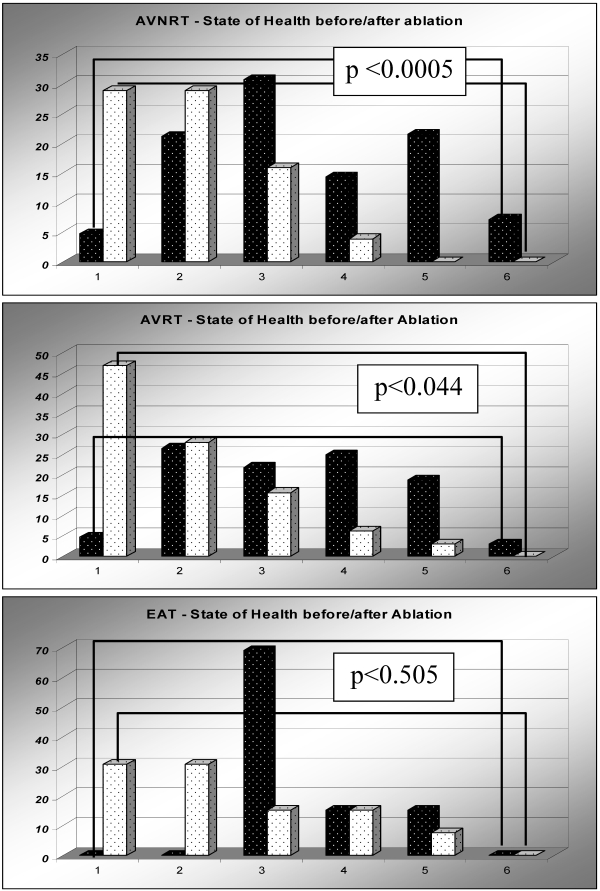
Patients with AVNRT, AVRT and EAT rated their state of health before and after ablation. The changes within the ranking scale before and after ablation is demonstrated in Figure 3.
Figure 3.
Comparison and improvement state of health before (black pillars) and after (white pillars) ablation. X-axis: State of health ranking scale from 1 to 6: very good (1), good (2), satisfactory (3), sufficient (4), defective (5) and insufficient (6). Y-axis: Percentage of patients Panel A: AVNRT. Panel B: AVRT. Panel C: EAT
Comparing the categorical variables before and after ablation in AVNRT patients, applying the McNemar-Test we found a highly significant improvement with respect to state of health (p<0.0005) in this large patient group (Figure 3, Panel A). Regarding the single aspects of well-being, we found highly significant improvements in daily (hobbies and work at home, p<0.0005) and social life (p<0.039). Professional life and participation in sports as well showed a trend towards improvement; however, this difference was not significant (p>0.05).
Comparing the categorical variables in patients with AVRT before and after ablation applying the McNemar-Test, we found a significant improvement with respect to state of health (p<0.044) in this patient cohort (Figure 3, Panel B). Regarding the individual data, we found a highly significant improvement for all variables concerning daily and social life (p<0.0005).
In patients with EAT a remarkable improvement in state of health was found. This difference was not significant (p<0.505). Analysis of data concerning individual symptoms were not accomplished because of the small patient cohort.
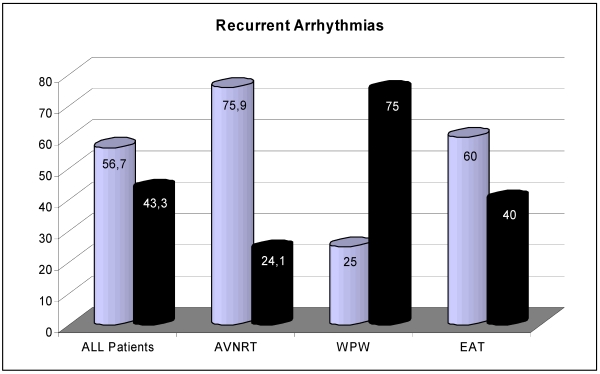
Recurrent arrhythmias
Recurrent arrhythmias were defined as relapse of the ablated tachycardia (true relapses), or the crossover to a new SVT like atrial flutter or AF. Figure 4 demonstrates the relationship between true relapses and the crossover to a new SVT. In long term follow up, 219 patients (73%) of the whole study population deemed themselves completely free of SVT, whereas 27% (81 pts.) stated to be suffering from recurrent tachycardia (AVNRT: 155 (69.8%) patients free of SVT, 67 (30.2%) patients with relapse; AVRT: 56 (86.2%) versus 9 (13.8%) patients and EAT 8 (61.5%) versus 5 (38.5%) patients).
Figure 4.
Recurrent arrhythmias dependent on true relapses of the pre-existing native tachycardia ablated (dark pillar), or the crossover to a new SVT (bright pillar). X-axis: Relapses in all patients, patients with AVNRT, AVRT and EAT. Y-axis: Percentage of patients
Bivariate analysis was performed to calculate if relapses were influenced by different types of variables, such as gender or age. Gender was found to not have a significant influence, this was true for the whole population and as well for patients with AVNRT or AVRT (Fischer`s exact test: All patients p=0.430, AVNRT p=0.552, AVRT p=0.149, EAT with too small a sample size). Age was as well found to not have a significant influence, this was true for the whole population and as well for patients with AVNRT or AVRT (Shapiro-Wilk-Test, Mann-Whitney-U-Test: All patients p=0.540, AVNRT p=0.179, AVRT p=0.352, EAT with too small a sample size).
Multivariate analysis was performed applying a logistic regression analysis. None of the abovementioned factors was shown to have an influence on the frequency of relapses, neither for the whole study cohort nor for patients with AVNRT or AVRT.
Concerning the patients with recurrent tachycardias, there still was a non-significant trend towards better QoL. We detected significant improvement in the symptoms tachycardia and anxiety as well as an increase in work capacity (McNemar Test: p<0.0005, p=0.007 and p=0.004 respectively).
Discussion
Background: The ablation of AVNRT, AVRT and EAT using RF energy has become the first line therapy for patients with recurrent episodes of these arrhythmias. Acute and long term success with respect to the primary electrophysiological outcome has been very well documented 6, 9, 10, 20, 24.
However, there are indications that, despite of successful primary ablation, new arrhythmias can arise in the long term 1, 2, 7. Data on QoL in short term follow-up after RF ablation of SVT is available from a few studies of smaller patient groups, but despite of the large number of patients ablated worldwide, there is a scarcity of data regarding the long term outcome, particularly with respect to QoL 8, 9, 25. This is somewhat surprising, as atrial flutter and AF have been intensively investigated under this aspect 14-23. This is the first study on long term electrophysiological outcome and its impact on the QoL in a large patient group.
Study cohort: The number of patients lost in long term follow up is consistent with long-term surveys using written questionnaires 14, 19. A significant number of submitted questionnaires had to be excluded because they were not fully completed. This is most likely due to patients not being able to remember the initial symptoms after the relatively long follow-up interval. We observed a linear increase in the proportions of sufficiently completed questionnaires over the time during which the ablations were performed.
Regarding the patients reporting tachycardic palpitations during follow-up, we found only a low rate of recurrences of the original tachycardia and mainly a shift to new SVT. This corresponds with the findings of other series in which catheter ablation was performed with a high primary success rate (1, 7, 14,). The technical data of the ablation procedure as well as the primary and long-term electrophysiological success rates are in line with the literature 1-6, 9, 10.
Quality of life in long term follow-up: Prior to interventional therapy, patients mainly suffered from symptoms like tachycardia, increasing incidence of episodes over time, reduction in physical work capacity, dyspnea and angina pectoris. These symptoms were the main reasons why patients seeked treatment.
More than 90% of the patients in each arrhythmia subgroup described the procedure as successful in the long-term follow up. A highly significant improvement in QoL could be demonstrated in the majority of patients. More detailed analysis as well revealed highly significant and sustained improvement in fundamental daily and social life, both for the whole study cohort and for the different types of SVT.
In contrast, patients without ablation therapy and longstanding medical therapy suffer from side effects of medication as well as from recurrent episodes of SVT leading to reduced QoL 12.
Recurrent arrhythmias: 27% of all patients suffered from recurrent arrhythmias which, apart from AVRT patients, to the largest part were not relapses of the primary SVT, (Figure 4). This phenomenon has as well been observed by other groups 26, 27. Bi- and multivariate analysis of the data collected in this study did not identify independent predictive factors of arrhythmia recurrence. The data does not comprise information on total RF energy used; therefore, no statement with regards to its effect on arrhythmia recurrence can be made based on this study.
Even if the patients developed a recurrent arrhythmia, their QoL still measurably improved. Although the total QoL-score only showed a non-significant trend towards improvement, various symptoms, such as tachycardia, anxiety and performance capacity were significantly improved. Previous studies have suggested a causal relationship between different types of right inferior atrial SVT, such as common type atrial flutter and AVNRT, because of a possible shared pathway in the low right atrium, leading to an electrical modulation of atrial tissue substrate 28, 29, 30. A placebo effect as well might be responsible for the improvement in QoL in patients with recurrent arrhythmias.
Study limitations
There are some limitations to this study: First, the subjective benefit of an ablation procedure is complex. Various tools have been developed trying to translate the various domains and components of well-being into a quantitative value. We assessed the subjective benefit with a modified version of the SF-36 Health Survey questionnaire and the Symptom Checklist - Frequency and Severity Scale. Although conclusions are clinically relevant, it still remains difficult to provide quantitative assessment of QoL.
Second, since all patients had been willing to undergo an invasive procedure with potentially significant adverse effects, this study group was highly motivated and highly selected. The perspective of a definitive treatment and ongoing medical surveillance after the procedure may have induced a perception bias in patients and have lead to overstatement of the perceived ablation success.
Third, the potential negative impact of anti-arrhythmic drug therapy on QoL may have significantly contributed to the low baseline scores, further motivating patients to seek non-pharmacological therapy. The marked improvement in measurement of QoL may have been related to reduced symptoms from side effects after the discontinuation of anti-arrhythmic medication. Pharmacological treatment was not studied in detail. Finally, the study was retrospective and the time interval between the ablation procedure and the questionnaire was not uniform. Patients who had more recently undergone the procedure may therefore have had a different recollection of symptoms than those having undergone the procedure at an earlier point of time. Therefore, placebo effects as well may have affected the perception of the patients of the success of the procedure and improvement in their QoL.
Conclusions
Patients with symptomatic arrhythmias treated with RF catheter ablation show significant reductions in arrhythmia-related symptoms and improvement in physical, emotional and social indexes of their health-related QoL. Self-imposed restrictions on physical and social activities are markedly reduced after catheter ablation. These improvements persist during long term follow up. Efforts should be made to increase awareness of symptoms and treatment options of SVT among patients and physicians, aiming at the elimination of delays in the process of symptom onset, first diagnosis and ablation therapy.
Abbreviations
- AVNRT
Atrio-Ventricular Nodal Reentry Tachycardia
- AVRT
Atrio-Ventricular Reentry Tachycardia
- AF
Atrial Fibrillation
- EAT
Ectopic Atrial Tachycardia
- F
French
- INR
International Normalized Ratio
- QoL
Quality of Life
- RF
Radio Frequency
- SDA
Standard Deviation
- SVT
Supraventricular Tachycardia.
References
- 1.Calkins H, Yong P, Miller JM, Olshansky B, Carlson M, Saul JP, Huang SK, Liem LB, Klein LS, Moser SA, Bloch DA, Gillette P, Prystowsky E. Catheter ablation of accessory pathways, atrioventricular nodal reentrant tachycardia, and the atrioventricular junction: final results of a prospective, multicenter clinical trial. Circulation. 1999;99(2):262–270. doi: 10.1161/01.cir.99.2.262. [DOI] [PubMed] [Google Scholar]
- 2.Dagres N, Clague JR, Kottkamp H, Hindricks G, Breithardt G, Borggrefe M. Radiofrequency catheter ablation of accessory pathways. Outcome and use of antiarrhythmic drugs during follow up. European Heart Journal. 1999;20(24):1826–1832. doi: 10.1053/euhj.1999.1749. [DOI] [PubMed] [Google Scholar]
- 3.Iturralde-Torres P, Colin-Lizalde L, Kershenovich S, Gonzalez-Hermosillo JA. Radiofrequency ablation in the treatment of tachyarrhythmias. Experience concearning 1000 consecutive patients. Gac Med Mex. 1999;135:559–575. [PubMed] [Google Scholar]
- 4.Rodriguez LM, Geller JC, Tse HF, Timmermans C, Reek S, Lee KL, Ayers GM, Lau CP, Klein HU, Crijns HJ. Acute results of transvenous cryoablation of supraventricular tachycardia (atrial fibrillation, atrial flutter, Wolff-Parkinson-White syndrome, atrioventricular nodal reentry tachycardia) Journal of cardiovascular electrophysiology. 2002;13:1082–1089. doi: 10.1046/j.1540-8167.2002.01082.x. [DOI] [PubMed] [Google Scholar]
- 5.Bernat R, Pfeiffer D. Long-term results and learning curve for radio frequency ablation of accessory pathways. Coll Anthropol. 2003;27:83–91. [PubMed] [Google Scholar]
- 6.Gaita F, Montefusco A, Riccardi R, Scaglione M, Grossi S, Caponi D, Caruzzo E, Guistetto C, Bocchiardo M, Di Donna P. Acute and long-term outcome of transvenous cryothermal catheter ablation of supraventricular arrhythmias involving the perinodal region. J Cardiovasc Med. 2006;7:785–792. doi: 10.2459/01.JCM.0000250865.25413.44. [DOI] [PubMed] [Google Scholar]
- 7.Kimman GP, Bogaard MD, van Hemel NM, van Dessel PF, Jessurun ER, Boersma LV, Wever EF, Theuns DA, Jordaens LJ. Ten year follow-up after radiofrequency catheter ablation for atrioventricular nodal re-entrant tachycardia in the early days forever cured, or a source for new arrhythmias? Pace. 2005;28:1302–1309. doi: 10.1111/j.1540-8159.2005.00271.x. [DOI] [PubMed] [Google Scholar]
- 8.Bubien RS, Knotts-Dolson SM, Plumb VJ, Kay GN. Effect of Radiofrequency catheter ablation on health-related quality of life and activities of daily living in patients with recurrent arrhythmias. Circulation. 1996;94:1585–1591. doi: 10.1161/01.cir.94.7.1585. [DOI] [PubMed] [Google Scholar]
- 9.Schläpfer J, Fromer M. Late clinical outcome after successful radiofrequency ablation of accessory pathways. Eur Heart J. 2001;22:605–609. doi: 10.1053/euhj.2000.2409. [DOI] [PubMed] [Google Scholar]
- 10.Maggi R, Quartieri F, Donateo P, Bottoni N, Solano A, Lolli G, Tomasi C, Croci F, Oddone D, Puggioni E, Menozzi C, Brignole M. Seven-year follow-up after catheter ablation of atrioventricular nodal re-entrant tachycardia. J Cardiovasc Med. 2006;7:39–44. doi: 10.2459/01.JCM.0000199784.56642.f7. [DOI] [PubMed] [Google Scholar]
- 11.Bathina MN, Mickelsen S, Brooks C, Jaramillo J, Hepton T, Kusumoto FM. Radiofrequency catheter ablation versus medical therapy for initial treatment of supraventricular tachycardia and its impact on quality of life and healthcare costs. Am J Cardiol. 1998;82:589–593. doi: 10.1016/s0002-9149(98)00416-0. [DOI] [PubMed] [Google Scholar]
- 12.Lau CP, Tai YT, Lee PW. The effects of radiofrequency ablation versus medical therapy on the quality-of-life and exercise capacity in patients with accessory pathway-mediated supraventricular tachycardia: a treatment comparison study. Pace. 1995;18:424–432. doi: 10.1111/j.1540-8159.1995.tb02541.x. [DOI] [PubMed] [Google Scholar]
- 13.Knotts S, Bubiens RS, Miers LJ, McLaughlin S, Sington L, Kay GN. Is quality of life improved by radiofrequency catheter ablation? A pilot study to asses measurable outcomes. Pace. 1994;17:261–267. [Google Scholar]
- 14.Anne W, Willems R, Adriaenssens B, Adams J, Ector H, Heidbüchel H. Long -term symptomatic benefit after radiofrequency catheter ablation for atrial flutter despite a high incidence of post-procedural atrial fibrillation. Acta Cardiol. 2006;61:75–82. doi: 10.2143/AC.61.1.2005143. [DOI] [PubMed] [Google Scholar]
- 15.Anselme F, Saoudi N, Poty H, Douillet R, Cribier A. Radiofrequency catheter ablation of common atrial flutter: Significance of palpitations and quality-of-life Evaluation in patients with proven isthmus block. Circulation. 1999;99:534–540. doi: 10.1161/01.cir.99.4.534. [DOI] [PubMed] [Google Scholar]
- 16.Bielik H, Schrickel J, Shlevkov N, Yang A, Schwab JO, Bitzen A, Lüderitz B, Lewalter T. Pharmacological and ablative hybrid therapy of atrial fibrillation. Long term effect on quality of life and arrhythmia-related symptoms. Z Kardiol. 2005;94:564–569. doi: 10.1007/s00392-005-0263-9. [DOI] [PubMed] [Google Scholar]
- 17.Lee SH, Tai CT, Yu WH, Chen YJ, Hsieh MH, Tsai CF, Chang MS, Chen SA. Effects of radiofrequency catheter ablation on quality of life in patients with atrial flutter. Am J Cardiol. 1999;84:278–283. doi: 10.1016/s0002-9149(99)00276-3. [DOI] [PubMed] [Google Scholar]
- 18.O´Callaghan PA, Meara M, Kongsgaard E, Poloniecki J, Luddington L, Foran J, Camm AJ, Rawland E, Ward DE. Symptomatic improvement after radiofrequency catheter ablation for typical atrial flutter. Heart. 2001;86:167–171. doi: 10.1136/heart.86.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meissner A, Christ M, Maagh P, Borchard R, van Bracht M, Wickenbrock I, Trappe HJ, Plehn G. Quality of life and occurrence of atrial fibrillation in long term follow up of common type atrial flutter: Ablation with irrigated 5 mm tip- and conventional 8 mm tip electrode. Clin Res Cardiol. 2007;96:794–802. doi: 10.1007/s00392-007-0559-z. [DOI] [PubMed] [Google Scholar]
- 20.Weerasooriya R, Jais P, Hocini M, Scavee C, MacLe L, Hsu LF, Sandars P, Garrigue S, Clémenty J, Haïssaguerre M. Effect of catheter ablation on quality of life of patients with paroxysmal atrial fibrillation. Heart Rhythm. 2005;2:619–613. doi: 10.1016/j.hrthm.2005.02.1037. [DOI] [PubMed] [Google Scholar]
- 21.Pappone C, Rosanio S, Augello G, Gallus G, Vicedomini G, Mazzone P, Gulletta S, Gugliotta F, Pappone A, Sanfinelli V, Tortoriello V, Sala S, Zangrillo A, Crescenzi G, Benussi S, Alfieri O. Mortality, morbidity, and quality of life after circumferential pulmonary vein ablation for atrial fibrillation: outcomes from a controlled nonrandomized long-term study. J Am Coll Cardiol. 2003;42:185–197. doi: 10.1016/s0735-1097(03)00577-1. [DOI] [PubMed] [Google Scholar]
- 22.Erdogan A, Carlsson J, Neumann T, Berkowitsch A, Neuzner J, Hamm CW, Pitschner HF. Quality-of-life in patients with paroxysmal atrial fibrillation after catheter ablation: results of long-term follow-up. Pace. 2003;26:678–684. doi: 10.1046/j.1460-9592.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- 23.Lee Sh, Chen SA, Tai CT, Chiang CE, Wen ZC, Cheng JJ, Ding YA, Chang MS. Comparisons of quality of life and cardiac performance after complete atrioventricular junction ablation and atrioventricular junction modofication in patients with medically refractory atrial fibrillation. J Am Coll Cardiol. 1998;31:637–644. doi: 10.1016/s0735-1097(97)00530-5. [DOI] [PubMed] [Google Scholar]
- 24.Delise P, Sitta N, Bonso A, Coro L, Fantinel M, Mantovan R, Sciarra L, Zoppo F, Marras E, Verlato R, D'Este D. Pace mapping of Koch's triangle reduces risk of atrioventricular block during ablation of atrioventricular nodal reentrant tachycardia. J Cardiovasc Eelectrophysiol. 2005;16:30–35. doi: 10.1046/j.1540-8167.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 25.Hamer ME, Blumenthal JA, McCarthy EA, Phillips BG, Pritchett EL. Quality of life assessment in patients with paroxysmal atrial fibrillation or paroxysmal supraventricular tachycardia. Am J Cardiol. 1994;74:826–829. doi: 10.1016/0002-9149(94)90448-0. [DOI] [PubMed] [Google Scholar]
- 26.Benjamin EJ, Levy D, Vaziri SM, D`Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Study. JAMA. 1994;271:840–844. [PubMed] [Google Scholar]
- 27.Emori T, Fukushima K, Saito H, Nakayama K, Ohe T. Atrial electrograms and activation sequences in the transition between atrial fibrillation and atrial flutter. J Cardiovasc Electrophysiol. 1998;9:1173–1179. doi: 10.1111/j.1540-8167.1998.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 28.Kimman GP, van Hemel NM, Jessurun ER, van Dessel PF, Kelder J, Defauw JJ, Guiraudon GM. Comparison of late results of surgical or radiofrequency catheter modification of the atrioventricular node for atrioventricular nodal re-entrant tachycardia. Eur Heart J. 1999;20:527–534. doi: 10.1053/euhj.1998.1337. [DOI] [PubMed] [Google Scholar]
- 29.Kalbfleisch SJ, El-Atassi R, Calkins H, Langberg JJ, Morady F. Association between atrioventricular node reentrant tachycardia and inducible atrial flutter. J Am Coll Cardiol. 1993;22:80–84. doi: 10.1016/0735-1097(93)90818-l. [DOI] [PubMed] [Google Scholar]
- 30.Interian A, Cox MM, Jimenez RA, Duran A, Levin E, Garcia O, Cooper DK, Castellanos A, Myerburg RJ. A shared pathway in atrio-ventricular nodal reentrant tachycardia and atrial flutter: Implications for pathophysiology and therapy. Am J Cardiol. 1993;71:297–303. doi: 10.1016/0002-9149(93)90794-d. [DOI] [PubMed] [Google Scholar]