Abstract
OBJECTIVE—Low birth weight (LBW) is associated with increased risk of obesity, diabetes, and cardiovascular disease during adult life. Moreover, this programmed disease risk can progress to subsequent generations. We previously described a mouse model of LBW, produced by maternal caloric undernutrition (UN) during late gestation. LBW offspring (F1-UN generation) develop progressive obesity and impaired glucose tolerance (IGT) with aging. We aimed to determine whether such metabolic phenotypes can be transmitted to subsequent generations in an experimental model, even in the absence of altered nutrition during the second pregnancy.
RESEARCH DESIGN AND METHODS—We intercrossed female and male F1 adult control (C) and UN mice and characterized metabolic phenotypes in F2 offspring.
RESULTS—We demonstrate that 1) reduced birth weight progresses to F2 offspring through the paternal line (C♀-C♂ = 1.64 g; C♀-UN♂ = 1.57 g, P < 0.05; UN♀-C♂ = 1.64 g; UN♀-UN♂ = 1.60 g, P < 0.05), 2) obesity progresses through the maternal line (percent body fat: C♀-C♂ = 22.4%; C♀-UN♂ = 22.9%; UN♀-C♂ = 25.9%, P < 0.05; UN♀-UN♂ = 27.5%, P < 0.05), and 3) IGT progresses through both parental lineages (glucose tolerance test area under curve C♀-C♂ = 100; C♀-UN♂ = 122, P < 0.05; UN♀-C♂ = 131, P < 0.05; UN♀-UN♂ = 151, P < 0.05). Mechanistically, IGT in both F1 and F2 generations is linked to impaired β-cell function, explained, in part, by dysregulation of Sur1 expression.
CONCLUSIONS—Maternal undernutrition during pregnancy (F0) programs reduced birth weight, IGT, and obesity in both first- and second-generation offspring. Sex-specific transmission of phenotypes implicates complex mechanisms including alterations in the maternal metabolic environment (transmaternal inheritance of obesity), gene expression mediated by developmental and epigenetic pathways (transpaternal inheritance of LBW), or both (IGT).
Human and animal studies have demonstrated a strong association between intrauterine growth retardation/low birth weight (LBW) and increased susceptibility to cardiovascular disease, obesity, and type 2 diabetes during adult life (1–5). This association has been conceptualized by the developmental programming hypothesis, which proposes that environmental stimuli acting during critical windows of development, including fetal and/or early postnatal periods, can induce permanent alterations in cell/tissue structure and function (5).
A growing body of epidemiologic evidence indicates that the effects of developmental programming can be perpetuated to subsequent generations, even in the absence of further environmental stressors during intrauterine and early postnatal life (6,7). For example, offspring of LBW humans also have reduced birth weight (8), increased cardiovascular risk factors (8), and increased susceptibility to metabolic syndrome and type 2 diabetes (7). Similarly, intergenerational effects on birth weight, glucose tolerance, and hypothalamic function have been demonstrated in rat models of fetal programming (9–13). While multiple mechanisms may link nutritional imbalance during early life with transgenerational transmission of metabolic phenotypes, epigenetic mechanisms have gained particular prominence for several reasons (14–16). First, alterations in nutrition during development can alter epigenetic marks, including DNA methylation (12,17–19) and histone modifications (17,20,21) in rodents. Second, epigenetic marks are stable and can be inherited in somatic cells through mitosis or, if occurring in the germ line, through meiosis (22–24). Thus, inheritance of nutritionally induced epigenetic modifications through meiosis may contribute to intergenerational effects.
We have previously described a mouse model of intrauterine growth restriction induced by maternal global caloric restriction during pregnancy (25,26). LBW males develop severe glucose intolerance with aging (25), with major contributions from both obesity and impaired β-cell function. To assess intergenerational effects in this model, we intercrossed F1 males and females to 1) evaluate adiposity and ß-cell function in second-generation offspring and 2) to determine whether intergenerational inheritance is transmitted through the maternal and/or paternal line. Finally, we assessed expression of candidate genes potentially regulated by epigenetic mechanisms which might contribute to metabolic phenotypes in first- and second-generation offspring.
RESEARCH DESIGN AND METHODS
Protocols were approved by the Joslin Diabetes Center Institutional Animal Care and Use Committee. Virgin ICR females (6–8 weeks old, parental generation F0) were caged with ICR males (Fig. 1A). Pregnancy was dated by vaginal plug (day 0.5). Pregnant F0 females were housed individually with ad libitum access to Purina 9F chow. On pregnancy day 12.5, F0 females were assigned to either control (C) or undernutrition (UN) groups randomly. Food intake of F0-UN dams was restricted from day 12.5 until delivery by 50% compared with that consumed by F0 controls (25). Litters were equalized to eight pups per dam by removing both the heaviest and lightest mice in the litter, thus retaining those with birth weight closest to the median for each litter. Offspring of F0 mice were designated as first-generation offspring (F1) (Fig. 1A). After delivery, all F0 mothers received chow ad libitum. F1 pups nursed freely and were weaned at 3 weeks onto 9F chow, provided ad libitum.
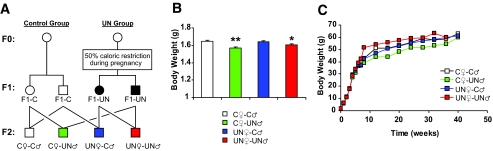
FIG. 1.
Experimental design, birth weight, and growth curves. A: Experimental design, including breeding scheme for second-generation (F2) offspring. Circles designate females and squares designate males. Note that mating pairs were nonsiblings. Metabolic analysis was performed in males only. B: Body weight at birth for F2 offspring. C: Postnatal growth curves for F2 male mice. For all panels, values are means ± SE (n ≥ 15 mice/group). *P < 0.05; **P < 0.01 vs. C♀-C♂ (ANOVA).
C and UN females from the F1 generation were mated at age 2 months with nonsibling F1-C or F1-UN males to generate four experimental groups (Fig. 1A). After confirmation of pregnancy, females were caged individually and fed ad libitum with no dietary manipulation during pregnancy. Pups were designated as second-generation offspring (F2): C♀-C♂ (both parents are controls); C♀-UN♂ (female control, male UN); UN♀-C♂(female UN, male control); and UN♀-UN♂ (both parents UN). F2 mice were weaned at 3 weeks onto 9F chow ad libitum; only males were followed for metabolic analysis given the higher prevalence of diabetes in UN-F1 males (100 vs. 30% in females, as described [25]).
In vivo metabolic testing.
Intraperitoneal glucose (2 g/kg weight) and insulin tolerance (1 unit/kg) tests were performed in unrestrained conscious mice after a 16- and 4-h fast, respectively. Intraperitoneal tolbutamide tolerance (1 mg/kg) was assessed after a 4-h fast.
Islet isolation and insulin secretion.
Islets were isolated from 4-month-old mice following intraductal collagenase infusion as previously described (25). For indicated experiments, diazoxide and tolbutamide (Sigma) were added during incubation (final concentration 250 and 200 μmol/l, respectively).
Gene expression (quantitative PCR).
Total RNA was isolated using RNeasy (Qiagen) and cDNA was synthesized using oligo-dT primers (Advantage; Clontech) for real-time quatitative PCR with SybrGreen detection (ABI Prism 7700; Applied Bioscience). Full list of primer sequences is available in supplementary Table 1 (available at http://dx.doi.org/10.2337/db08-0490).
DNA methylation.
Methylation of the Sur1 promoter was analyzed by PCR (MethylScreen; Orion Genomics) (27) (supplementary methods), while methylation of differentially methylated regions at the Pref1 locus was assessed by Southern blotting (28).
Body composition.
Body composition was analyzed by dual-energy X-ray absorptiometry (Hologic, Waltham, MA) (29).
Serum analysis.
Blood samples from adult mice were collected from the tail vein, while trunk blood was collected from ED16.5 fetuses after decapitation. Blood glucose was measured with Glucometer Elite (Bayer, Elkhart, IN). Insulin, leptin (enzyme-linked immunosorbent assay; Crystal Chem), triglycerides, glycerol (GTO-Trinder Triglycerides assay; Sigma), and nonesterified fatty acids (Half-micro test; Roche) were measured on 2- to 5-μl serum samples.
Statistical analysis.
Data are expressed as means ± SE. Statistical analysis was performed using a two-tailed t test or ANOVA (Statview). P ≤ 0.05 was considered significant.
RESULTS
Intergenerational inheritance of body weight.
As previously described, 50% global caloric restriction of F0 dams during the last week of gestation blunted feto-maternal growth and resulted in 15% decrease in offspring birth weight (F1-UN) (25). In pregnancies of F1 mice, both maternal food intake and feto-maternal weight gain (supplementary Table 2) were similar among the four experimental groups. Despite this, birth weight was modestly, but significantly, reduced in C♀-UN♂ and UN♀-UN♂ offspring compared with C♀-C♂ (Fig. 1B); UN♀-C♂ mice had normal birth weight compared with controls. Litter size and length of gestation were similar in all groups (supplementary Table 2). After delivery, all four F2 groups had similar weights to 40 weeks (Fig. 1C).
Since feto-maternal nutritional status during pregnancy might account for observed differences in birth weight, we determined both maternal and fetal serum concentrations of major macronutrients contributing to fetal growth. In F0-UN females, caloric restriction resulted in 34% reduction in serum glucose and 80% reduction in triglycerides by day 16.5 of gestation (P < 0.05, Table 1). Likewise, serum insulin and leptin were reduced in F0-UN dams by 77 and 94%, respectively (P < 0.05) (Table 1). Maternal dysregulation of fuel metabolism was also accompanied by alterations in fetal metabolism. Fetal glucose and leptin levels were decreased by 45 and 63%, respectively, in ED16.5 F1-UN fetuses (P < 0.05) (Table 2), while triglycerides, free fatty acids (FFAs), glycerol, and insulin did not differ from controls (not shown).
TABLE 1.
Maternal physiology at day 16.5 of pregnancy
| F0 dams
|
F1 dams
|
|||||
|---|---|---|---|---|---|---|
| Control | Undernourished | Control female × control male | Control female × undernourished male | Undernourished female × control male | Undernourished female × undernourished male | |
| Blood glucose (mg/dl) | 99 ± 3 | 65 ± 4* | 111 ± 6 | 103 ± 5 | 105 ± 4 | 108 ± 4 |
| Serum insulin (ng/ml) | 0.84 ± 0.33 | 0.19 ± 0.13* | 1.6 ± 0.36 | 1.7 ± 0.22 | 2.0 ± 0.41 | 1.4 ± 0.34 |
| Serum leptin (ng/ml) | 7.2 ± 1.9 | 0.42 ± 0.22* | 32.9 ± 0.6 | 34.3 ± 0.5 | 38.7 ± 14 | 38.4 ± 6.8 |
| Serum TG (mg/dl) | 218 ± 29 | 44 ± 27* | 156 ± 47 | 202 ± 15 | 210 ± 47 | 185 ± 23 |
| Serum glycerol (mg/dl) | 41.8 ± 5.7 | 32.4 ± 5.9 | 37 ± 5.1 | 55 ± 10.5* | 59 ± 6.8* | 51 ± 5.7 |
| Serum FFAs (mmol/l) | 1.2 ± 0.17 | 1.0 ± 0.13 | 1.2 ± 0.20 | 1.5 ± 0.19 | 1.6 ± 0.23 | 1.4 ± 0.24 |
Data are means ± SE. Maternal serum levels of hormones and nutrients at pregnancy day 16.5.
P < 0.05 vs. controls. Significance was determined by Student's t test in F0 dams and ANOVA in F1 dams. TG, triglycerides.
TABLE 2.
ED16.5 serum metabolites
| F1 offspring
|
F2 offspring
|
|||||
|---|---|---|---|---|---|---|
| Control | Undernourished | Control female–control male | Control female–undernourished male | Undernourished female− control male | Undernourished female–undernourished male | |
| Blood glucose (mg/ dl) | 20 ± 3 | 11 ± 2* | 26.4 ± 3.1 | 31.9 ± 3.4 | 30.0 ± 14 | 43.9 ± 5.2* |
| Serum insulin (pg/ml) | 216 ± 26 | 230 ± 28 | 221 ± 27 | 312 ± 27* | 307 ± 21 | 316 ± 33 |
| Serum leptin (pg/ml) | 263 ± 48 | 96 ± 28* | 379 ± 237 | 321 ± 99 | 192 ± 203 | 695 ± 124 |
Data are means ± SE. Fetal serum levels of glucose, insulin, and leptin at embryonic day 16.5.
P < 0.05 vs. controls. Significance was determined by Student's t test in F1 offspring and ANOVA in F2 offspring.
By contrast, during the F1 generation pregnancy, maternal glucose, triglycerides, FFAs, insulin, and leptin did not differ between groups at pregnancy day 16.5 (Table 1). However, serum glycerol was increased by 49 and 59% in dams of C♀-UN♂ and UN♀-C♂ pregnancies, respectively (P < 0.05) compared with C♀-C♂ (Table 1). Despite no major differences in maternal metabolism, we observed some differences in ED16.5 F2 fetuses. Glucose levels were increased by 66% in UN♀-UN♂ fetuses (P < 0.05), and insulin increased by 41% in C♀-UN♂ fetuses (P < 0.05) (Table 2). There were no significant differences in UN♀-C♂ fetuses.
Intergenerational inheritance of glucose intolerance.
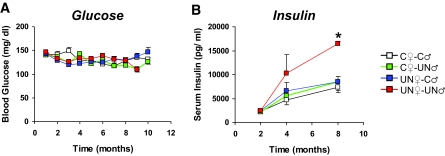
Glucose levels in F2 males did not differ in either fed (Fig. 2A) or fasting conditions (supplementary Fig. 1A) up to 10 months of age. Likewise, serum levels of triglycerides, glycerol, and FFAs were also similar among the four F2 groups at 2 and 4 months (not shown). However, UN♀-UN♂, but not C♀-UN♂ or UN♀-C♂ mice, developed hyperinsulinemia in the fed state between 4 and 8 months of age (P < 0.05) (Fig. 2B). Fasting insulin was similar in all F2 groups (supplementary Fig. 1B). To better define glucose homeostasis, we performed intraperitoneal glucose tolerance testing in all F2 mice. Strikingly, glucose tolerance was impaired (relative to C♀-C♂) in C♀-UN♂, UN♀-C♂, and UN♀-UN♂ mice between 4 and 6 months of age (P = 0.03, P = 0.003, and P = 0.007, respectively) (Fig. 3A).
FIG. 2.
Random fed blood glucose (A) and serum insulin (B) levels from 2 to 8 months of age in F2 male mice. Values are means ± SE (n ≥ 8 mice/group). *P < 0.05 vs. C♀-C♂ (ANOVA).
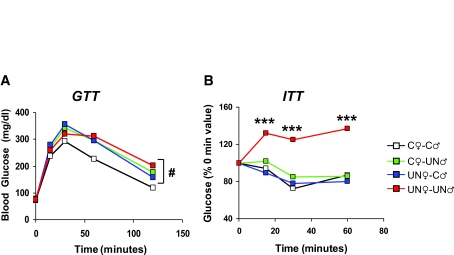
FIG. 3.
Glucose and insulin tolerance tests in 6-month-old male mice. A: Intraperitoneal glucose tolerance test (2 g glucose/kg body wt) was performed after an overnight fast. B: Intraperitoneal insulin tolerance test (1 unit insulin/kg body wt) was performed after a 4-h fast. Results are expressed as means ± SE (n ≥ 6 mice/group). #P < 0.05; ***P < 0.001 vs. C♀-C♂ (repeated-measures ANOVA).
We next explored potential mechanisms responsible for glucose intolerance in F2 offspring of UN parents. UN♀-UN♂ mice were clearly insulin resistant (assessed by insulin tolerance) by age 6 months (P < 0.001) (Fig. 3B). By contrast, C♀-UN♂ and UN♀-C♂ mice exhibited normal insulin sensitivity.
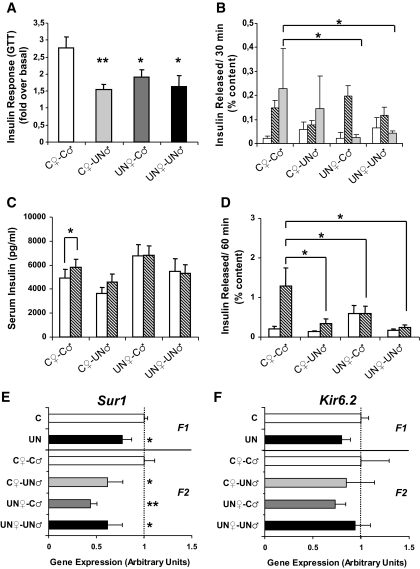
Since glucose intolerance may also reflect dysregulation of insulin secretion, we assessed glucose-stimulated insulin secretion in vivo and ex vivo. We first measured serum insulin with fasting and 30 min after a glucose load (glucose tolerance test) (Fig. 4A); glucose-stimulated insulin secretion was reduced in F2 offspring from F1-UN parents compared with C♀-C♂ mice at age 4 months (P < 0.05 for all comparisons) (Fig. 4A). Likewise, ex vivo glucose-stimulated insulin secretion was also impaired in islets from 4-month-old UN♀-C♂ and UN♀-UN♂ mice (P < 0.05 for both) but not C♀-UN♂ mice (Fig. 4B). Thus, reduced glucose-stimulated insulin secretion may also contribute to impaired glucose tolerance (IGT) in F2 mice.
FIG. 4.
Islet physiology. A: In vivo: insulin levels during an intraperitoneal glucose tolerance test in 4-month-old male mice. Data are provided as the fold increase in serum insulin (over basal) at 30 min after the glucose bolus injection (n ≥ 8 mice/group). B: Ex vivo glucose-stimulated insulin secretion in islets isolated from 4-month-old mice (n ≥ 4 replicates/group in at least 2 independent isolations). □, 1 mmol/l;  , 5.5 mmol/l;
, 5.5 mmol/l;  , 16.7 mmol/l. C: Intraperitoneal tolbutamide tolerance test (1 mg tolbutamide/kg body wt) was performed after a 4-h fast on 4-month-old mice (n ≥ 8 mice/group). □, 0 min;
, 16.7 mmol/l. C: Intraperitoneal tolbutamide tolerance test (1 mg tolbutamide/kg body wt) was performed after a 4-h fast on 4-month-old mice (n ≥ 8 mice/group). □, 0 min;  30 min tolbutamide. D: Tolbutamide stimulation (200 μmol/l) of insulin release from isolated islets ex vivo (n ≥ 4 replicates/group in at least 2 independent isolations). □, none;
30 min tolbutamide. D: Tolbutamide stimulation (200 μmol/l) of insulin release from isolated islets ex vivo (n ≥ 4 replicates/group in at least 2 independent isolations). □, none;  tolbutamide. E: Sur1 gene expression was assessed by quantitative PCR in islets from 4-month-old mice (n ≥ 5 replicates/group). F: Kir6.2 gene expression was assessed by quantitative PCR in islets from 4-month-old mice (n ≥ 5 replicates/group). For all panels, results are expressed as means ± SE. *P < 0.05 vs. C♀-C♂; **P < 0.01 vs. C♀-C♂ (ANOVA).
tolbutamide. E: Sur1 gene expression was assessed by quantitative PCR in islets from 4-month-old mice (n ≥ 5 replicates/group). F: Kir6.2 gene expression was assessed by quantitative PCR in islets from 4-month-old mice (n ≥ 5 replicates/group). For all panels, results are expressed as means ± SE. *P < 0.05 vs. C♀-C♂; **P < 0.01 vs. C♀-C♂ (ANOVA).
One potential candidate underlying insulin secretory dysfunction in F2 mice is altered expression and/or function of the β-cell ATP-dependent K+ channel, composed of Sur1/Kir6.2 subunits. We assessed the functional capacity of this complex using in vivo challenge with the sulfonylurea tolbutamide (1 mg/kg i.p.). Tolbutamide induced a 15% increase in serum insulin after 30 min in C♀-C♂ mice (P < 0.05) (Fig. 4C) (supplementary Fig. 2A). In contrast, F2 offspring from UN parents had impaired tolbutamide response (Fig. 4C) (supplementary Fig. 2A). Paralleling in vivo data, tolbutamide stimulated insulin release from freshly isolated C♀-C♂ islets by fivefold (Fig. 4D), while responses in all other groups were significantly reduced, with only minor increments in C♀-UN♂ and UN♀-UN♂ islets and no effect in UN♀-C♂ islets (Fig. 4D). We also incubated islets with diazoxide, a potassium channel stimulator. Diazoxide tended to reduce insulin release from C♀-C♂ islets (>50%, P = 0.1) (supplementary Fig. 2B). Interestingly, response in UN♀-C♂ islets was nearly normal, but diazoxide had only minimal effect in C♀-UN♂ and UN♀-UN♂ islets (5–10% decrease) (supplementary Fig. 2B). Together, these data suggest that dysfunctional potassium channel activity may contribute to impaired insulin secretion in F2 mice.
To determine whether alterations in expression might contribute to dysfunction of potassium channels, we assessed Sur1 and Kir6.2 expression in isolated islets. Sur1 expression was reduced by 23% (P < 0.05) in F1-UN islets (Fig. 4E). Likewise, Sur1 expression was reduced by 33% in C♀-UN♂ (P < 0.05), by 56% in UN♀-C♂(P < 0.05), and by 38% in UN♀-UN♂ islets (P < 0.05) (Fig. 4E). By contrast, Kir6.2 expression was normal in both F1 and F2 islets (Fig. 4F).
Since epigenetic regulation at the Sur1 locus might be mechanistically linked to differential expression in F2 offspring of LBW mice, we assessed DNA methylation within CpG islands at the Sur1 promoter using methylation-sensitive PCR (27); we did not detect differential methylation in either F1 (Supplementary Fig. 3) or F2 islets (not shown).
Intergenerational inheritance of obesity.
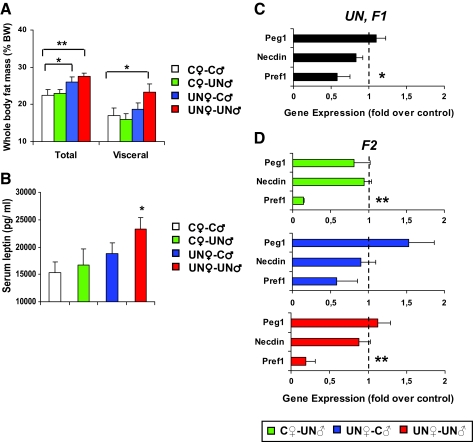
We have previously shown that F1-UN males develop increased adiposity as early as 2 months of age (26). In the F2 generation, both maternal lineage offspring groups developed increased adiposity by 4 months (P < 0.05) (Fig. 5A). Interestingly, adiposity in UN♀-UN♂mice is largely visceral in location (Fig. 5A). In parallel, serum leptin is increased in UN♀-UN♂ mice (P < 0.05) (Fig. 5B). We observed no differences in epididymal adipocyte size distribution or histology (not shown) or in adipose expression of genes regulating differentiation and/or metabolic function, including peroxisome proliferator–activated receptor γ, CCAAT/enhancer binding protein α, fatty acid binding protein 4, and Glut4, from any F2 group at 4 months of age (supplementary Table 3).
FIG. 5.
Characterization of the obese phenotype. A: Total and visceral fat mass by dual-energy X-ray absorptiometry in 4-month-old males (n ≥ 6 mice/group). B: Serum leptin levels in 4-month-old males (n ≥ 6/group). C and D: Expression of imprinted genes assessed by quantitative PCR in epididymal fat from 4-month-old F1 males (C) (n = 6/group) and 4-month-old F2 males (D) (n = 6/group). Results are expressed as means ± SE. *P < 0.05 vs. C♀-C♂; **P < 0.01 vs. C♀-C♂ (ANOVA).
Since obesity in UN♀-UN♂ mice implicates a contribution from epigenetic factors, we determined expression of imprinted genes known to regulate adipocyte development and/or function and thus potentially contributing to obesity, including preadipocyte factor 1 (Pref1) (30), Necdin (31), and paternally expressed gene 1 (Peg1) (32). Pref1, an inhibitor of adipogenesis expressed from the paternally inherited chromosome, was reduced in epididymal fat from F1-UN males (P < 0.05) and from both paternal F2 lineages, C♀-UN♂ and UN♀-UN♂ (P < 0.01) (Figs. 5C and D). This effect appeared restricted to Pref1 since expression of Necdin and Peg1, also paternally expressed, was not statistically different from controls in either F1 or F2 offspring (Figs. 5C and D). In addition, expression of retrotransposon-like 1 (Rtl1) and maternally expressed 2 (Gtl2), two genes also regulated by the same imprinting signals as Pref1 (28), did not differ among groups in F1 and F2 offspring (not shown).
To determine whether changes in Pref1 gene expression were related to differential methylation at this imprinted locus, we assessed DNA methylation by Southern blotting. We did not detect any alterations in DNA methylation at the Pref1 differentially methylated region, the intergenic differentially methylated region, or the Gtl2 promoter region (supplementary Fig. 4A and B).
DISCUSSION
Human data indicate that metabolic phenotypes associated with exposure to maternal undernutrition can also be observed in second-generation offspring. Conceptually, transgenerational inheritance of disease risk may be mediated by nongenomic mechanisms, including either 1) epigenetic mechanisms (16) or 2) other broader indirect mechanisms associated with parental physiology (rev. in 6). First, alterations in nutrition during development can alter epigenetic marks, thus regulating gene expression through DNA methylation (12,17–19) and/or histone modifications (17,20,21). Interestingly, such epigenetic modifications may progress with aging during postnatal life, in association with metabolic phenotypes, as recently observed at the pancreatic duodenal homeobox-1 and GLUT4 locus in rodent models of intrauterine programming (33–35). If these epigenetic changes occur in the germ line, they can be inherited through meiosis (22–24), thus providing a plausible explanation for intergenerational effects, transmitted via either maternal or paternal lines.
In addition, other indirect biological processes may influence phenotypes in subsequent generations. For example, uterine size is reduced in girls that are born small (F1) and remain short (36); this may influence fetal growth and reduce weight in their progeny (F2) (rev. in 6). Therefore, physical constraints may alter birth size through the maternal lineage. Furthermore, maternal metabolism may also influence cross-generational phenotypes (37). Maternal undernutrition during pregnancy (F0) increases risk for developing diabetes and obesity in her offspring (F1). When these high-risk adult F1 females become pregnant, the metabolic stress of pregnancy may result in hyperglycemia and/or overt gestational diabetes that may, in turn, contribute to fetal hyperinsulinemia, obesity, and increased diabetes risk in F2 offspring (37). For these two examples, intergenerational transmission of phenotypes would occur exclusively through the maternal lineage, as opposed to epigenetic mechanisms.
Since it is difficult to dissect the relative parental contributions and the molecular mechanisms that lead to F2 offspring outcomes in humans, we have utilized our mouse model of maternal undernutrition during pregnancy to address these important questions. We have previously shown that global caloric restriction during the last week of gestation in pregnant females (F0) impairs fetal growth, resulting in 15–20% reduction in birth weight, and the development of both obesity and glucose intolerance in F1 offspring (25,26). These alterations are multifactorial in origin, with glucose intolerance mediated, in part, by impaired glucose-stimulated insulin secretion (25). We now demonstrate that metabolic phenotypes are also observed in the F2 generation: 1) reduced birth weight progresses from F1 to F2 through the paternal, but not the maternal, line (Fig. 1B); 2) F2 offspring of both F1-UN males and females develop IGT with aging, in parallel with β-cell dysfunction (Figs. 3A and 4A and B) and, in UN♀-UN♂, insulin resistance (Figs. 2B and 3B); and 3) obesity progresses through the maternal, but not the paternal, lineage (Fig. 5A).
Intergenerational transmission of LBW.
Maternal undernutrition (F0) during the last week of gestation results in reduced birth weight in both F1 (25) and F2 offspring of F1-UN males (C♀-UN♂ and UN♀-UN♂) but not offspring of F1-UN females (UN♀-C♂) (Fig. 1B). Such patrilineal inheritance of reduced birth weight may be attributed to alterations in fetoplacental gene expression and/or function, most likely mediated by epigenetic modifications. While we did not detect major metabolic dysregulation in C♀-UN♂ and UN♀-UN♂ mice at embryonic day 16.5 (Tables 1 and 2), it is likely that more subtle or time-dependent effects on placental function account for paternally mediated reductions in birth weight in this setting.
While experimental (9,11,38,39) and human (40,41) data show similar paternal transmission patterns of birth weight, population-based studies also indicate that intergenerational aggregation of LBW can also occur through maternal lineages (40,41). Such results may reflect species differences and complex influences on human birth weight (e.g., genetics, maternal size). Furthermore, human population data generally exclude complicated pregnancies (e.g., gestational diabetes) and thus may also exclude the impact of fetal “overgrowth” due to increased nutrient supply in the context of previous maternal LBW.
Intergenerational transmission of glucose intolerance.
F1-UN males exhibit moderate hyperglycemia and IGT with aging and dysregulated glucose-stimulated insulin secretion (25). Additionally, all F2 offspring of F1-UN parents develop glucose intolerance by age 4 months (Fig. 3A). Therefore, intergenerational progression of glucose intolerance can derive from both the maternal and paternal lines. While maternal and grandmaternal inheritance of diabetes has been demonstrated in rats (9,11,38,39), here we present the first experimental evidence for transgenerational transmission of IGT also through the paternal lineage. In agreement, paternal LBW in humans has recently been linked to risk of metabolic syndrome in both offspring and grandoffspring (7).
We previously demonstrated that impaired glucose-stimulated insulin secretion is an early key phenotype in F1-UN males (25). Multiple metabolic adaptations lead to β-cell dysfunction in F1-UN mice, including altered glucokinase, hexokinase-1, and ATP-dependent K+ channel activities (25) (J.C.J.-C., unpublished data). We now find that glucose-stimulated insulin secretion is also impaired in islets of F2 mice from UN parents and is likely a major contributor to glucose intolerance (Fig. 4A and B). Additionally, we show that potassium channel activity is also altered in islets from F2-UN offspring both in vivo and in vitro (Fig. 4C and D; supplementary Fig. 2A and B). Thus, it is interesting that expression of Sur1 is reduced by 30% in islets from both F1-UN mice and islets from F2 C♀-UN♂, UN♀-UN♂, and UN♀-UN♂ mice (Fig. 4E), indicating that dysregulation of Sur1 gene expression and function can be transmitted to F2 through both maternal and paternal lines. This effect was specific to Sur1, since Kir6.2 gene expression was normal in both F1 and F2 islets (Fig. 4F). Together, these data suggest that dysregulation of Sur1 expression may alter potassium channel function (42) and ultimately contribute to whole-body glucose intolerance in our model. In agreement, genetic ablation of Sur1 results in metabolic phenotypes similar to those of our mouse model. Sur1−/− mice remain euglycemic for the majority of their lifespan, displaying moderate glucose intolerance with aging (43,44). Isolated islets from Sur−/− mice show impaired glucose-stimulated insulin secretion and lack of responsiveness to tolbutamide in vitro (43).
Which mechanism(s) is responsible for reduced Sur1 expression in both F1 and F2 islets? Since decreased Sur1 gene expression progresses to F2 offspring through the paternal lineage, we hypothesized that reductions in Sur1 expression would be mediated, in part, by altered DNA methylation; however, we did not observe differences in methylation of the Sur1 proximal promoter region (supplementary Fig. 2). A potential limitation of our approach is that we utilized DNA from islets (a mixture of β-, α-, δ-, and PP cells), potentially masking β-cell–specific differences. Alternatively, reduced expression of Sur1 in islets from F1 and F2 mice might also be due to 1) altered methylation of another genomic region(s), 2) altered histone modification, or 3) changes in binding/expression of other transcription factors regulating Sur1. Future experiments will focus on potential mechanisms mediating decreased expression of Sur1.
An additional factor likely to contribute to impaired glucose tolerance in UN♀-UN♂ mice is insulin resistance, observed by age 6 months (Figs. 2B and 3B). Of note, insulin resistance arises when both parents were growth restricted in utero, suggesting that interface between these two lineages is necessary and sufficient to induce insulin resistance. While the specific mechanisms underlying insulin resistance in UN♀-UN♂ mice remain under investigation, it is interesting to note that UN♀-UN♂ mice also display increased visceral fat by age 4 months (Fig. 5A). Therefore, it is tempting to speculate that insulin resistance may develop secondary to progressive accumulation of visceral fat in UN♀-UN♂.
Intergenerational transmission of obesity.
Childhood obesity is linked to parental obesity (45). Although it is difficult to dissect the relative contribution of shared environmental factors to these phenotypes in humans, maternal metabolic dysregulation during pregnancy may be a key contributor (46,47). We similarly demonstrate that adiposity phenotypes progress to F2 offspring through the maternal lineage (Fig. 5A), implicating subtle maternal metabolic dysfunction during pregnancy and/or maternal epigenetic effects. It is important to note that despite increased adiposity in these groups, body weight remained similar to that of controls (Fig. 1C). Therefore, offspring of F1-UN females do not have overt obesity but have a shift in body composition (higher fat mass with concomitantly reduced lean body mass) (26). On the other hand, although paternal transmission alone is not sufficient to drive adiposity in C♀-UN♂ mice, paternal effects may contribute to the increased abdominal fat accumulation in UN♀-UN♂ mice as compared with UN♀-C♂ mice.
We next evaluated potential mechanisms mediating increased adiposity in UN♀-C♂ and UN♀-UN♂ mice. First, food intake was similar in all groups (not shown). Second, expression of adipocyte differentiation markers, including peroxisome proliferator–activated receptor γ, CCAAT/enhancer binding protein α, fatty acid binding protein 4, or Glut4, was similar in all F1 and F2 groups (supplementary Table 3) (E.I., J.C.J.-C., M. Woo, A.C., J. DeCoste, M. Vokes, M. Liu, S. Kasif, A.-M. Zavacki, R. Leshan, M. Myers, M.E.P., unpublished data). Similarly, we observed no major differences in adipocyte size distribution among F2 groups (not shown). Additional studies will be required to determine whether alterations in adipocyte metabolic function or in systemic energy homeostasis also contribute to adiposity.
Since obesity in UN♀-UN♂ mice implicates a partial role for epigenetic factors, it is very interesting that Pref1 expression was significantly decreased in F1-UN, C♀-UN♂, and UN♀-UN♂ mice (Fig. 5C and D). Patrilineal inheritance of Pref1 expression may be explained by the fact that it is expressed from the paternally inherited chromosome; altered expression would be predicted to be inherited from F1-UN males but not F1-UN females. Mice lacking functional Pref1 have increased adiposity (48); conversely, mice overexpressing Pref1 have reduced fat content (49) (A.F.-S., unpublished data). Thus, decreased Pref1 expression may contribute, in part, to development of obesity in F1-UN, UN♀-C♂, and UN♀-UN♂ mice. While our data support a potential role of Pref1 in the development of adiposity in our mouse model, it has to be noted that its expression has been determined in epididymal fat, a depot without direct parallel in humans. Thus, although many adipose genes are similarly expressed in both rodents and humans (50), extrapolation of Pref1 gene expression data from our model to humans must be undertaken with caution.
Imprinting of Pref1 is under complex control by both paternal and maternal alleles (28). We did not detect changes in methylation of the differentially methylated regions that regulate imprinting at this locus in fat from 4-month-old mice of either F1 or F2 generations (supplementary Fig. 4). These data suggest that, as with Sur1, altered expression of Pref1 is due to either changes in expression or function of an upstream transcription factor, histone modification, or another yet-unknown genomic region that is epigenetically modified. Thus, additional studies are required to define the potential role of epigenetics in adipose development in our model.
In conclusion, we demonstrate that maternal undernutrition during pregnancy programs reduced birth weight, glucose intolerance, and obesity in first- and second-generation offspring, even despite ad libitum feeding during second pregnancy. Different aspects of these phenotypes are transmitted via the maternal lineage (obesity), the paternal lineage (reduced birth weight), or both (glucose intolerance). Sex differences in transmission of phenotypes implicate complex mechanisms: 1) matrilineal inheritance of disease is multifactorial and includes metabolic, epigenetic, and mitochondrial mechanisms; and 2) patrilineal inheritance is primarily due to epigenetic mechanisms. While we do not yet understand the complex array of molecular mechanisms associated with fetal programming of disease, such studies will be of great importance for the design of future therapeutic interventions aimed to prevent and/or modulate adult phenotypes, not only in LBW humans but also in their children and grandchildren.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge support for this study from the American Diabetes Association (Research Award, to M.E.P.), the Graetz Family Fund (to M.E.P.), the Marie Curie International Reintegration Grant (MIRG-CT-2007-046542, to J.C.J.-C.), and the Diabetes Endocrinology Research Center (P30-DK36836).
No potential conflicts of interest relevant to this article were reported.
Published ahead of print at http://diabetes.diabetesjournals.org on 18 November 2008.
J.C.J.-C. is currently affiliated with Hospital Sant Joan de Deu, Universitat de Barcelona, Barcelona, Spain.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Hales CN, Barker DJ: Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia 35: 595–601, 1992 [DOI] [PubMed] [Google Scholar]
- 2.Barker DJ: In utero programming of chronic disease. Clin Sci (Lond) 95: 115–128, 1998 [PubMed] [Google Scholar]
- 3.McMillen IC, Robinson JS: Developmental origins of the metabolic syndrome: prediction, plasticity, and programming. Physiol Rev 85: 571–633, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Saenger P, Czernichow P, Hughes I, Reiter EO: Small for gestational age: short stature and beyond. Endocr Rev 28: 219–251, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Gluckman PD, Hanson MA, Cooper C, Thornburg KL: Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 359: 61–73, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gluckman PD, Hanson MA, Beedle AS: Non-genomic transgenerational inheritance of disease risk. Bio Essays 29: 145–154, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Veena SR, Geetha S, Leary SD, Saperia J, Fisher DJ, Kumaran K, Coakley P, Stein CE, Fall CH: Relationships of maternal and paternal birthweights to features of the metabolic syndrome in adult offspring: an inter-generational study in South India. Diabetologia 50: 43–54, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emanuel I, Filakti H, Alberman E, Evans SJ: Intergenerational studies of human birthweight from the 1958 birth cohort. 1. evidence for a multigenerational effect. Br J Obstet Gynaecol 99: 67–74, 1992 [DOI] [PubMed] [Google Scholar]
- 9.Zambrano E, Martinez-Samayoa PM, Bautista CJ, Deas M, Guillen L, Rodriguez-Gonzalez GL, Guzman C, Larrea F, Nathanielsz PW: Sex differences in transgenerational alterations of growth and metabolism in progeny (F2) of female offspring (F1) of rats fed a low protein diet during pregnancy and lactation. J Physiol 566: 225–236, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crescenzo R, Lionetti L, Mollica MP, Ferraro M, D'Andrea E, Mainieri D, Dulloo AG, Liverini G, Iossa S: Altered skeletal muscle subsarcolemmal mitochondrial compartment during catch-up fat after caloric restriction. Diabetes 55: 2286–2293, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Drake AJ, Walker BR, Seckl JR: Intergenerational consequences of fetal programming by in utero exposure to glucocorticoids in rats. Am J Physiol Regul Integr Comp Physiol 288: R34–R38, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Burdge GC, Slater-Jefferies J, Torrens C, Phillips ES, Hanson MA, Lillycrop KA: Dietary protein restriction of pregnant rats in the F0 generation induces altered methylation of hepatic gene promoters in the adult male offspring in the F1 and F2 generations. Br J Nutr 97: 435–439, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thamotharan M, Garg M, Oak S, Rogers LM, Pan G, Sangiorgi F, Lee PW, Devaskar SU: Transgenerational inheritance of the insulin resistant phenotype in embryo-transferred intra-uterine growth restricted adult female rat offspring. Am J Physiol Endocrinol Metab 292: E1270–E1279, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Gallou-Kabani C, Junien C: Nutritional epigenomics of metabolic syndrome: new perspective against the epidemic. Diabetes 54: 1899–1906, 2005 [DOI] [PubMed] [Google Scholar]
- 15.Jirtle RL, Skinner MK: Environmental epigenomics and disease susceptibility. Nat Rev Genet 8: 253–262, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ozanne SE, Constancia M: Mechanisms of disease: the developmental origins of disease and the role of the epigenotype. Nat Clin Pract Endocrinol Metab 3: 539–546, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Maclennan NK, James SJ, Melnyk S, Piroozi A, Jernigan S, Hsu JL, Janke SM, Pham TD, Lane RH: Uteroplacental insufficiency alters DNA methylation, one-carbon metabolism, and histone acetylation in IUGR rats. Physiol Genomics 18: 43–50, 2004 [DOI] [PubMed] [Google Scholar]
- 18.Waterland RA, Dolinoy DC, Lin JR, Smith CA, Shi X, Tahiliani KG: Maternal methyl supplements increase offspring DNA methylation at Axin Fused. Genesis 44: 401–406, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Dolinoy DC, Weidman JR, Waterland RA, Jirtle RL: Maternal genistein alters coat color and protects Avy mouse offspring from obesity by modifying the fetal epigenome. Environ Health Perspect 114: 567–572, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ke X, Lei Q, James SJ, Kelleher SL, Melnyk S, Jernigan S, Yu X, Wang L, Callaway CW, Gill G, Chan GM, Albertine KH, McKnight RA, Lane RH: Uteroplacental insufficiency affects epigenetic determinants of chromatin structure in brains of neonatal and juvenile IUGR rats. Physiol Genomics 25: 16–28, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Fu Q, McKnight RA, Yu X, Wang L, Callaway CW, Lane RH: Uteroplacental insufficiency induces site-specific changes in histone H3 covalent modifications and affects DNA-histone H3 positioning in day 0 IUGR rat liver. Physiol Genomics 20: 108–116, 2004 [DOI] [PubMed] [Google Scholar]
- 22.Chong S, Vickaryous N, Ashe A, Zamudio N, Youngson N, Hemley S, Stopka T, Skoultchi A, Matthews J, Scott HS, de Kretser D, O'Bryan M, Blewitt M, Whitelaw E: Modifiers of epigenetic reprogramming show paternal effects in the mouse. Nat Genet 39: 614–622, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morgan HD, Sutherland HG, Martin DI, Whitelaw E: Epigenetic inheritance at the agouti locus in the mouse. Nat Genet 23: 314–318, 1999 [DOI] [PubMed] [Google Scholar]
- 24.Anway MD, Cupp AS, Uzumcu M, Skinner MK: Epigenetic transgenerational actions of endocrine disruptors and male fertility. Science 308: 1466–1469, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jimenez-Chillaron JC, Hernandez-Valencia M, Reamer C, Fisher S, Joszi A, Hirshman M, Oge A, Walrond S, Przybyla R, Boozer C, Goodyear LJ, Patti ME: β-Cell secretory dysfunction in the pathogenesis of low birth weight-associated diabetes: a murine model. Diabetes 54: 702–711, 2005 [DOI] [PubMed] [Google Scholar]
- 26.Jimenez-Chillaron JC, Hernandez-Valencia M, Lightner A, Faucette RR, Reamer C, Przybyla R, Ruest S, Barry K, Otis JP, Patti ME: Reductions in caloric intake and early postnatal growth prevent glucose intolerance and obesity associated with low birthweight. Diabetologia 49: 1974–1984, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Ordway JM, Bedell JA, Citek RW, Nunberg A, Garrido A, Kendall R, Stevens JR, Cao D, Doerge RW, Korshunova Y, Holemon H, McPherson JD, Lakey N, Leon J, Martienssen RA, Jeddeloh JA: Comprehensive DNA methylation profiling in a human cancer genome identifies novel epigenetic targets. Carcinogenesis 27: 2409–2423, 2006 [DOI] [PubMed] [Google Scholar]
- 28.Lin SP, Youngson N, Takada S, Seitz H, Reik W, Paulsen M, Cavaille J, Ferguson-Smith AC: Asymmetric regulation of imprinting on the maternal and paternal chromosomes at the Dlk1-Gtl2 imprinted cluster on mouse chromosome 12. Nat Genet 35: 97–102, 2003 [DOI] [PubMed] [Google Scholar]
- 29.Nagy TR, Clair AL: Precision and accuracy of dual-energy X-ray absorptiometry for determining in vivo body composition of mice. Obes Res 8: 392–398, 2000 [DOI] [PubMed] [Google Scholar]
- 30.Wang Y, Kim KA, Kim JH, Sul HS: Pref-1, a preadipocyte secreted factor that inhibits adipogenesis. J Nutr 136: 2953–2956, 2006 [DOI] [PubMed] [Google Scholar]
- 31.Goldfine AB, Crunkhorn S, Costello M, Gami H, Landaker EJ, Niinobe M, Yoshikawa K, Lo D, Warren A, Jimenez-Chillaron J, Patti ME: Necdin and E2F4 are modulated by rosiglitazone therapy in diabetic human adipose and muscle tissue. Diabetes 55: 640–650, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Takahashi M, Kamei Y, Ezaki O: Mest/Peg1 imprinted gene enlarges adipocytes and is a marker of adipocyte size. Am J Physiol Endocrinol Metab 288: E117–E124, 2005 [DOI] [PubMed] [Google Scholar]
- 33.Park JH, Stoffers DA, Nicholls RD, Simmons RA: Development of type 2 diabetes following intrauterine growth retardation in rats is associated with progressive epigenetic silencing of Pdx1. J Clin Invest 118: 2316–2324, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raychaudhuri N, Raychaudhuri S, Thamotharan M, Devaskar SU: Histone code modifications repress glucose transporter 4 expression in the intrauterine growth-restricted offspring. J Biol Chem 283: 13611–13626, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woo M, Patti ME: Diabetes risk begins in utero. Cell Metab 8: 5–7, 2008 [DOI] [PubMed] [Google Scholar]
- 36.Ibanez L, Potau N, Enriquez G, de Zegher F: Reduced uterine and ovarian size in adolescent girls born small for gestational age. Pediatr Res 47: 575–577, 2000 [DOI] [PubMed] [Google Scholar]
- 37.Aerts L, Van Assche FA: Animal evidence for the transgenerational development of diabetes mellitus. Int. J Biochem Cell Biol 38: 894–903, 2006 [DOI] [PubMed] [Google Scholar]
- 38.Blondeau B, Avril I, Duchene B, Breant B: Endocrine pancreas development is altered in foetuses from rats previously showing intra-uterine growth retardation in response to malnutrition. Diabetologia 45: 394–401, 2002 [DOI] [PubMed] [Google Scholar]
- 39.Benyshek DC, Johnston CS, Martin JF: Glucose metabolism is altered in the adequately-nourished grand-offspring (F3 generation) of rats malnourished during gestation and perinatal life. Diabetologia 49: 1117–1119, 2006 [DOI] [PubMed] [Google Scholar]
- 40.Jaquet D, Swaminathan S, Alexander GR, Czernichow P, Collin D, Salihu HM, Kirby RS, Levy-Marchal C: Significant paternal contribution to the risk of small for gestational age. BJOG 112: 153–159, 2005 [DOI] [PubMed] [Google Scholar]
- 41.Veena SR, Kumaran K, Swarnagowri MN, Jayakumar MN, Leary SD, Stein CE, Cox VA, Fall CH: Intergenerational effects on size at birth in South India. Paediatr Perinat Epidemiol 18: 361–370, 2004 [DOI] [PubMed] [Google Scholar]
- 42.Koster JC, Permutt MA, Nichols CG: Diabetes and insulin secretion: the ATP-sensitive K+ channel (KATP) connection. Diabetes 54: 3065–3072, 2005 [DOI] [PubMed] [Google Scholar]
- 43.Seghers V, Nakazaki M, DeMayo F, Aguilar-Bryan L, Bryan J: Sur1 knockout mice: a model for KATP channel-independent regulation of insulin secretion. J Biol Chem 275: 9270–9277, 2000 [DOI] [PubMed] [Google Scholar]
- 44.Shiota C, Larsson O, Shelton KD, Shiota M, Efanov AM, Hoy M, Lindner J, Kooptiwut S, Juntti-Berggren L, Gromada J, Berggren PO, Magnuson MA: Sulfonylurea receptor type 1 knock-out mice have intact feeding-stimulated insulin secretion despite marked impairment in their response to glucose. J Biol Chem 277: 37176–37183, 2002 [DOI] [PubMed] [Google Scholar]
- 45.Danielzik S, Langnase K, Mast M, Spethmann C, Muller MJ: Impact of parental BMI on the manifestation of overweight 5–7 year old children. Eur J Nutr 41: 132–138, 2002 [DOI] [PubMed] [Google Scholar]
- 46.Dabelea D, Pettitt DJ: Intrauterine diabetic environment confers risks for type 2 diabetes mellitus and obesity in the offspring, in addition to genetic susceptibility. J Pediatr Endocrinol Metab 14: 1085–1091, 2001 [DOI] [PubMed] [Google Scholar]
- 47.Hillier TA, Pedula KL, Schmidt MM, Mullen JA, Charles MA, Pettitt DJ: Childhood obesity and metabolic imprinting: the ongoing effects of maternal hyperglycemia. Diabetes Care 30: 2287–2292, 2007 [DOI] [PubMed] [Google Scholar]
- 48.Moon YS, Smas CM, Lee K, Villena JA, Kim KH, Yun EJ, Sul HS: Mice lacking paternally expressed Pref-1/Dlk1 display growth retardation and accelerated adiposity. Mol Cell Biol 22: 5585–5592, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee K, Villena JA, Moon YS, Kim KH, Lee S, Kang C, Sul HS: Inhibition of adipogenesis and development of glucose intolerance by soluble preadipocyte factor-1 (Pref-1). J Clin Invest 111: 453–461, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gesta S, Bluher M, Yamamoto Y, Norris AW, Berndt J, Kralisch S, Boucher J, Lewis C, Kahn CR: Evidence for a role of developmental genes in the origin of obesity and body fat distribution. Proc Natl Acad Sci USA 103: 6676–6681, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.