Abstract
There is a worldwide epidemic of obesity with far-reaching consequences for the health of our nation. Prevention of obesity, especially in children, has been deemed by public health policy makers to be one of the most important objectives for our country. This prevention project, called Louisiana (LA) Health, will test whether modification of environmental and behavioral factors can prevent inappropriate weight gain in children from rural parishes of Louisiana who are enrolled in the fourth to sixth grades during Year 1. The primary aim of the LA Health project is to test the efficacy of two school-based approaches for obesity prevention: primary prevention alone and a combination of primary and secondary prevention which will be compared to a no-intervention control group using a cluster randomization research design, with 17 school clusters randomly assigned to the three treatment arms. The study will span three years and will provide critical tests of strategies that: 1) modify the child’s environment as a primary prevention strategy and 2) provide health behavior modification via classroom instruction and internet counseling as a secondary prevention strategy. The study will also recruit a similar sample of students to measure changes in body weight relative to height, gender, and age over the same three-year period.
Keywords: obesity prevention, children, cluster randomized design, school-based intervention
Introduction
The obesity epidemic is a major health concern in the United States (U.S.) and the world [1]. Overweight and obesity is the second leading cause of preventable death in the U.S. and is associated with increased morbidity and mortality from cardiovascular disease [2, 3]. Based on these and other considerations, obesity has been established as a very important target for prevention research in the U.S. [4, 5] and the rest of the world [1].
Over the past 20 years, the prevalence of obesity has increased in industrialized societies [6, 7]. This increased prevalence of overweight and obesity extends to children and adolescents in the U.S. with recent estimates of 31% of children and adolescents with a BMI percentile (%tile) greater than or equal to the 85th percentile [8]. Given that obese children and adolescents often become obese adults [9, 10], it is most logical that preventive efforts should target inappropriate weight gain in children and young adolescents [11, 12]. The results of previous studies of childhood obesity prevention programs have yielded relatively weak preventive effects [13, 14]. Many of these studies were limited by relatively short duration, uncontrolled research designs, and single-level interventions that targeted a single health behavior [14, 15]. Furthermore, most studies have not included large samples of minority or economically disadvantaged children [13]. There is urgent need for testing the efficacy of multi-level prevention strategies that target disadvantaged children.
Most obesity prevention programs have utilized primary prevention approaches in schools [16, 17]. There is an emerging consensus that secondary prevention may not be desirable in the school setting due to the potential stigmatization of overweight children and therefore, might be most appropriate for treatment in general medical practice [18]. We have developed a method for delivering secondary prevention in the school setting in the context of a primary prevention program so that overweight children will not be “singled out” or stigmatized. If successful at preventing weight gain, this approach can avoid many of the logistical obstacles (e.g., additional travel, expense, and inconvenience) that are associated with clinic-based secondary prevention approaches.
The primary objective of this paper is to describe the development of a study called LA Health that was designed to address many of the deficiencies of earlier childhood obesity prevention studies. This paper will present the strategies that were required to initiate the LA Health project and the research design of the cluster (group) randomized controlled trial (RCT).
It is noteworthy that the state of Louisiana has one of the highest rates of poor health in the nation. A recent survey [19] reported that Louisiana is the second least healthy state in the U.S., with a ranking of 49 out of 50 states; Louisiana has held the ranking of either 49 or 50 for each of the 18 years of the annual report from this Foundation. In particular, the citizens of rural Louisiana have significantly higher rates of poverty and nutritionally related mortality and morbidity in comparison to the nation as a whole [20]. Furthermore, among the people of this region, African-Americans assume the greatest burden of health problems [20]. We elected to work with rural schools because children living in rural, economically deprived regions of Louisiana are excellent research targets for interventions that are designed for use in areas that lack universities and medical facilities.
Research Goals of the LA Health project
This project will test the efficacy of introducing three prevention programs via schools by randomly assigning each school cluster to one of three intervention arms (primary prevention, combined primary and secondary prevention, and no-intervention control) with repeated measures of outcomes collected over a three-year period. Body mass index (BMI) z-scores (using NHANES norms) of the students will be the primary endpoint of the trial.
Using this research design that randomly assigns schools to treatment arms, the primary aim of the study is to test the efficacy of the two intervention arms for prevention of weight gain via:
a primary prevention program that employs an environmental approach
-
a combined primary and secondary prevention program that uses a classroom/internet approach to promote weight loss in children with a baseline BMI percentile (%tile) ≥ 85th %tile.
In comparison to:
a no-intervention control group
An observation control group (that is not part of the RCT) will also be studied to evaluate secular changes in BMI z-scores.
Secondary aims of the study are:
To observe secular changes in BMI z-scores of students with similar demographic and geographic characteristics to those in the RCT. A secondary hypothesis is that the BMI z-scores of students in the observation control group will increase over the three-year period of the LA Health project.
To test the efficacy of the prevention programs for white (predominantly non-Hispanic) children and minority (primarily non-Hispanic black) children, while statistically controlling for socioeconomic status.
To test the efficacy of the prevention programs for boys and girls, while statistically controlling for race/ethnicity and socioeconomic status.
To test for differential changes in the food selections and food intake of students in the two prevention arms in comparison to the no-intervention control group.
To test for differential changes in physical activity of students in the two prevention arms in comparison to the no-treatment group.
To test for mediators and moderators of weight changes. Mediator and moderator variables to be tested are changes in food intake and physical activity. Utilization of the internet-based program (within the combined primary and secondary prevention arm) will be tested as a moderator of changes in the primary endpoint. Psychosocial variables (mood, eating attitudes, and social support for diet and physical activity) will be tested as moderators of treatment effects and changes in these variables will be tested as mediators of treatment effects.
Study Design
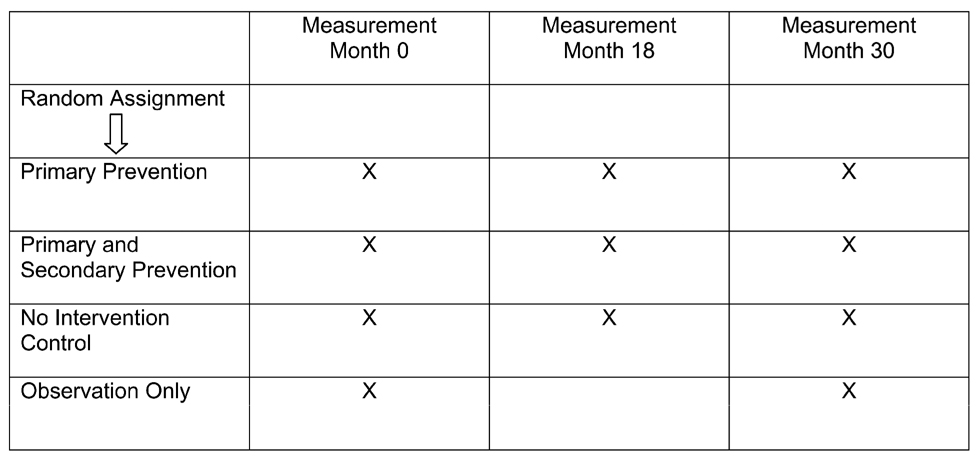
In order to test the experimental hypotheses, three treatment arms will be compared in a design that randomly assigns school clusters to treatment arms after the collection of baseline data. A fourth treatment arm, observation only, will serve as a nonrandomized control condition to observe secular trends in BMI z-scores. Students in this fourth treatment arm will be recruited to have height and weight measured at baseline and at Month 30, (the end of the study). This observation control condition will not be directly compared to the treatment arms in the RCT. Thus, the observation only condition serves as a “backdrop” for interpreting the results of the RCT. Since the observation control participants are not enrolled in Louisiana Gaining Early Awareness and Readiness for Undergraduate Programs (LA GEAR UP), they are a group of students who have no exposure to a prevention program. This study design is illustrated in Figure 1.
Figure 1.
Study design for the LA Health Project
Note. X indicates schedule of measurement procedures.
Participants will be categorized in terms of baseline BMI %tile using two groups: 1) < 85th %tile and 2) ≥ 85th %tile. The combined intervention is hypothesized to capitalize upon the strengths of primary and secondary prevention programs to magnify the benefits for the general student population and students ≥ 85th %tile, thus yielding an overall superior efficacy for prevention of inappropriate weight gain (a definition that includes weight maintenance and weight loss in overweight children).
Primary prevention
The primary prevention program is based on Social Learning Theory [21] with emphasis on: 1) modification of environmental cues, 2) enhancement of social support, and 3) promotion of self-efficacy for health behavior change. The program will use an environmental approach that was developed and tested in the Wise Mind study [22]. Goals of the program are compatible with conventional nutrition recommendations (e.g., five fruits and vegetables per day, less than 30% of dietary energy from total fat, less than 10% of dietary energy from saturated fat, and 20 to 30 grams of fiber/day). To increase physical activity, another goal is promotion of 60 minutes of moderate to vigorous activity per day. In addition, the program is intended to facilitate the Child Nutrition Program by meeting USDA guidelines for the National School Lunch Program [23], the WIC Reauthorization Act of 2004 [24], and Act 331 of the Louisiana Legislature related to advertisement of fast foods and the content of vending machines and concessions in schools [25].
Secondary prevention
Secondary prevention relies on intentional (conscious) efforts to change behavior. In contrast, the primary prevention approach attempts to alter the environment to prompt changes in behavior that are under less volitional control. Therefore, the secondary prevention approach places greater emphasis on behavior modification approaches that are designed to change these personal factors (i.e., increased healthy eating habits, increased physical activity, and decreased sedentary behavior). The internet-based approach that was developed and tested in the HIPTeens program [26] serves as a basis for this approach with one primary modification: the health behavior change program will be delivered as a part of regular classroom instruction, combined with synchronous (on-line) internet counseling and asynchronous (email) communications for children and their parents. Thus, the secondary prevention program uses frequent prompts to promote sustained website usage.
No-Intervention Control
The control group for the RCT has none of the prevention components that are hypothesized to yield weight gain prevention. This control arm can be viewed as a nonspecific control condition.
Observation Control
The student participants from these four schools did not participate in the RCT. During baseline measurement, the height, weight, and body fat of these students were measured. This measurement will be repeated in the final measurement period (Month 30).
Recruitment of Schools and Students
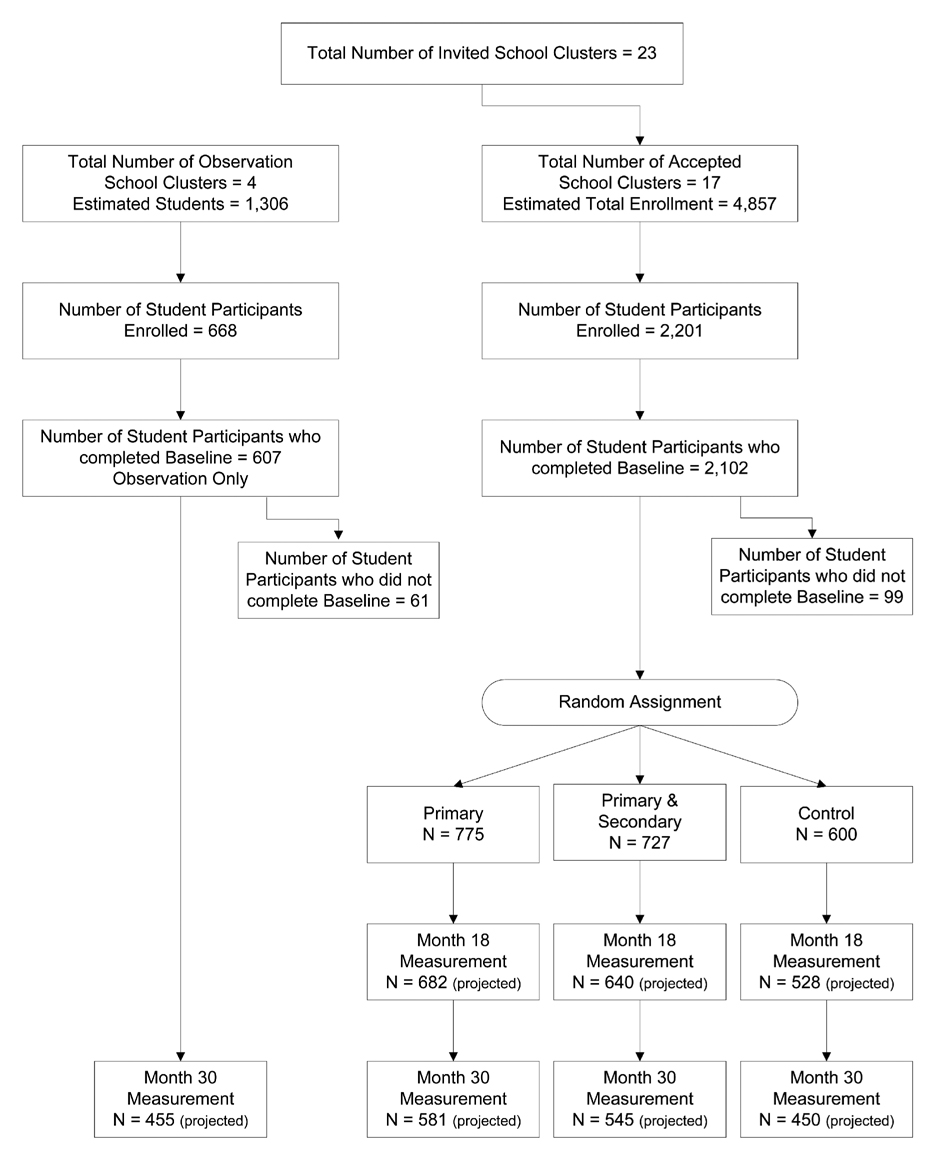
Much of the first two years of LA Health involved contacting and recruiting parish school administrations and principals, a process we completed in August 2006. Given our experience with recruitment for Wise Mind, we expected to recruit approximately half (50%) of the students enrolled in a school cluster. In keeping with the ecological changes that were successfully employed in the Wise Mind study [22], we initiated a series of actions that can be described as a top-down approach, i.e., we first sought the support of the highest levels of school administration and progressively sought support at lower levels. First, we obtained support from the Governor of Louisiana and then obtained support from the State Superintendent of Public Schools in Louisiana. Table 1 describes these actions. We also recognized a strategic opportunity: joining a partnership with an ongoing U.S. Department of Education project called LA GEAR UP. This project was started two years prior to the beginning of recruitment for LA Health and therefore a strong relationship with certain rural school systems was already established. Based on the criteria described in the next section, 23 school systems were invited to participate in LA Health. As shown in Table 1, the research team then contacted superintendents of school systems that had been invited to participate, gained their support, and progressed to obtaining the support of principals, teachers, staff, and parents. Students were recruited in the school environment by a variety of methods, including presentations to students and parents, fliers, and word of mouth. It is noteworthy that the task of recruitment was very time consuming and required the efforts of eight research staff members over a two-year period. The study was planned for 18 school clusters (described in the statistical power section), and 18 school clusters were recruited. One week before the beginning of the study, one school cluster dropped out, leaving 17 school clusters for the RCT. As shown in Figure 2, we have completed 1) recruitment of student participants from these 17 school clusters, 2) baseline measurement, and 3) randomization. The study is projected for completion in 2009.
Table 1.
Steps for recruiting schools and students for the LA Health project
| Step | Strategy |
|---|---|
| 1 | Secure partnership with LA GEAR UP project |
| 2 | Obtain support of Superintendent of Education |
| 3 | Obtain support of State Board of Education |
| 4 | Obtain support of Board of Regents |
| 5 | Obtain support of Governor |
| 6 | Establish Executive Advisory Committee |
| 7 | Invite eligible school systems to participate |
| 8 | Obtain support from superintendents of each school system |
| 9 | Obtain support of principals, teachers, and school staff |
| 10 | Announcement of study to parents and teachers |
| 11 | Recruitment of students |
| 12 | Obtain informed consent from students and parents |
| 13 | End period of enrollment |
Figure 2.
Flowchart of recruitment and study procedures
Schools/Participants
Seventeen school clusters were recruited for the LA Health project. The schools met the following inclusion criteria: 1) one of the 38 schools or elementary feeder schools in the LA GEAR UP program, 2) located in a rural section of Louisiana, 3) a minimum of 100 students available for study, and 4) the structure of the school system - elementary schools that feed students to a single middle school.
All of the selected school clusters have at least eight grades. Therefore, students in grades 4 through 6 will be followed for three consecutive school years in the same school. Figure 2 illustrates the recruitment process that resulted in a study sample of 2,102 student participants in the RCT and 607 student participants in the observation control group.
Professional Development
The orientation and training of teachers in the LA Health schools that were randomized began in July 2005. In this professional development program, teachers received information about the LA Health Project, instruction on modeling and implementing content standards as they relate to LA Health, and technology training critical to project implementation. Treatment specific training began in the spring semester of 2006, after random assignment of schools, and was held at locations convenient for the teachers. Professional development sessions will continue throughout the three-year trial as a means to provide critical treatment-specific training for faculty members at their respective school locations. The purpose and goals of training aligned grade-specific content standards with the scientific study design of LA Health, making a definitive connection between LA Health and math, science, technology, and physical education instruction, and assisting teachers with implementation of LA Health programs in their classrooms.
Measurement
Outcome/Assessment Strategy
Baseline assessment was conducted after the completion of recruitment and prior to randomization of schools to the treatment arms. Recruitment of students was completed at the beginning of the 2006–2007 academic year prior to baseline measurements. All baseline data were collected in Fall 2006 with the remaining assessments planned for the end of the school year in Years 2 and 3. The week of assessment was randomly assigned for each school prior to the baseline assessment, and this schedule will be followed for the other two assessment periods. Table 2 provides an overview of the outcome measures that will be collected at each of the measurement periods.
Table 2.
Summary of outcome measures and schedule of measurement.
| Measurement Month 0 |
Measurement Month 18 |
Measurement Month 30 |
|
|---|---|---|---|
| Height | x | x | x |
| Weight | x | x | x |
| %BF | x | x | x |
| Digital photography | x | x | x |
| Physical activity social support | x | x | x |
| SAPAC | x | x | x |
| FIQ | x | x | x |
| Dietary social support | x | x | x |
| ChEAT | x | x | x |
| CDI-S | x | x | x |
| *Accelerometer | x | x | x |
| *W:H | x | x | x |
| *CTQ | x | x | x |
Note. * denotes subsample of 316 participants. Abbreviations: %BF: Percent body fat as measured by the Tanita Body Fat analyzer. SAPAC-Self-Administered Physical Activity Checklist; FIQ-Food Intake Questionnaire; ChEAT-Children’s Eating Attitudes Test; CDI-S-Children’s Depression Inventory-Short form; W:H-waist to hip ratio; CTQ-Child Treatment Questionnaire.
Outcomes and Study Measures
Selection of Endpoints and Outcome Measures for LA Health
The behavioral targets for the obesity prevention programs were selected because they are viewed as healthy behaviors that would lead to negative energy balance and also improve health and fitness [1]. With regard to energy or nutrient intake, the behavioral targets are: 1) decreased total caloric intake in children with a BMI %tile ≥ 85th %tile, 2) increased consumption of fruits, vegetables, legumes, and whole grains, 3) decreased intake of sweets, salts (sodium), and dietary fat (with a shift away from saturated fats and trans fats and towards unsaturated fats), and 4) overall moderation or balance of macronutrients. These behavioral targets were selected based on findings that people generally do not consume adequate quantities of fruits and vegetables [27] or whole grains [28]. Also, there is a strong consensus that a diet with less than 30% fat is desirable for a number of health reasons [23]. Furthermore, reduced dietary fat intake has been one of the more frequent goals of previous prevention programs for obesity-related problems [29, 30]. The behavioral targets for physical activity are: 1) reduction of sedentary behavior, and 2) increased lifestyle physical activity during school hours and after school. These targets were selected because there is a growing consensus that the current obesity epidemic may stem, in part, from increased sedentary behaviors (e.g., watching television, playing video games, use of computers, etc,) [11, 31–33]. Enhancement of physical activity during and after school hours has been a target of many other prevention programs and is generally viewed as an important goal in obesity-related prevention trials [34]. Since objective measurement of physical activity using accelerometers is costly and labor-intensive, we planned a sub-study in which approximately 20 participants in each school cluster were randomly selected to undergo measurement of physical activity using accelerometers. In this sub-sample, we also measured waist and hip circumference and assessed if program concepts were reaching the home. Therefore, the behavioral targets of the intervention will be multi-faceted and will focus on the modification of energy intake and expenditure.
Primary Endpoint
Body Mass Index z-scores and Percentile (BMI %tile)
Height and weight of each child will be measured, in normal school clothing, without shoes and socks. Height will be measured using a stadiometer. Weight will be measured using Tanita (model TBF-310) scales that capture body weight and body composition (described below) using a laptop computer. Height and weight will be converted to body mass index (kg/m2). In growing children, BMI increases with age [35]; therefore, BMI will be converted to z-scores and %tile scores based on gender and age using norms provided by Centers for Disease Control in 2000,that cover the NHANES surveys from 1963 to 1994 [36].
Secondary Endpoints
Successful weight gain prevention
Success will be defined in terms of a participant’s BMI %tile [36] at Year 3 being equal or less than the participant’s BMI %tile at baseline. Therefore, each participant will be given a “Yes,” which indicates successful prevention of weight gain or a “No”, which indicates unsuccessful weight gain prevention. The proportion of affirmatives will be compared to those in the control condition.
Body fat
The Tanita Body Composition Analyzer (model TBF-310) measures body weight and body impedance simultaneously by standing on the scale with bare feet. Body fat and lean body mass are automatically recorded using a laptop computer. Body impedance has been validated as a measure of body fat and lean body mass.
Digital photography of food selections and food intake
On three consecutive days, the digital photography method will be used to measure food selections and food intake of students enrolled in the study. At lunch, foods selected by the students prior to eating and after eating will be photographed by research assistants using two Sony DCR-TRV22 digital video cameras. Camera angle and distance is standardized to allow the apparent size of all foods to remain constant across photographs. Digital video cameras are used so that photographs are automatically recorded by placing the child’s food tray in front of the camera. Photographs will be captured only for those students who enrolled in the study.
Prior to any photography of the student’s food selection, standard portion sizes of the possible food choices are recorded for comparison to the digital photographs of the participants. One digital camera photographs incoming trays (food selection), and the second digital camera is used for photographing outgoing trays (plate waste). Food intake is defined as the difference between food selections and plate waste.
Following initial data collection, digital photographs of the reference portion, food selection, and plate waste for test meals are digitally captured and incorporated into a computer application designed for estimation of food portions in digital photographs. Research associates use the software to simultaneously view photos of the food selection and plate waste test meals along with photos of the reference portion of each food. The observers independently estimate the percent of the reference portion of each food in the photographs in units of 10% and these estimates are entered into a data entry grid in the computer software application for statistical analysis and food composition analysis using the Pennington Biomedical Research Center (PBRC) nutrient database. In previous studies with adults [22, 37] and children [38], we have found this procedure to be highly reliable and valid. The dietary measures include: total calories, macronutrient content (% fat, protein, and carbohydrates), servings of fruit, vegetables, grains, meats, added fats, and total dietary fat.
Questionnaires
The following questionnaires are administered in a group format in the classroom setting. All questionnaires have been formatted so that they can be optically scanned for the purposes of scoring and data entry.
Food Intake
The Food Intake Questionnaire (FIQ, [39]) is a 65-item self-report measure that assesses changes in food intake in children 9–14 years old over time using a yes/no format. The FIQ is based on recall of foods eaten the day before and has been shown to detect changes in food intake over time. The reliability and validity of the measure has been established [40].
Physical Activity
The Self-Administered Physical Activity Checklist (SAPAC) is a self-report, one-day recall of physical activity using a checklist format. Students report the number of minutes spent in each of 24 different physical activities during three periods of the previous school day, i.e., before school, during school, and after school.
Sedentary Behavior
Children will be instructed to report the number of hours they spend in sedentary pursuits both before and after school using the SAPAC. The sedentary activities assessed will include TV, video, computer, reading, homework, and telephone [41].
Dietary Social Support
The Children’s Dietary Social Support scale (DSS; [42]) is a 7-item measure of perceived social support for healthy dietary choices. The scale assesses support from family, friends, and teachers in a yes/no format.
Physical Activity Social Support
The Physical Activity Social Support Scale (PASS; [43]) is an 18-item measure that assesses perceived support for physical activity. Support from family, teachers, and friends is assessed in a yes/no format.
Mood
The Child Depression Inventory-Short Form (CDI-S; [44]) will be used to assess children’s subjective levels of depressed mood. The CDI-S is a 10-item self-report scale that measures overt symptoms of childhood depression. The reliability and validity of the CDI-S has been established [44].
Eating Attitudes
The Children's Eating Attitudes Test (ChEAT, [45, 46]) is a 26-item measure of eating disorder symptoms. It is designed to discriminate between normal dieters and individuals with anorexia and bulimia. The reliability and validity of the scale have been confirmed [45].
Accelerometers
Physical activity will be objectively measured with the Actigraph accelerometer (ActiGraph, Pensacola, FL.). The reliability of the measure has been established [47]. A subset of approximately 316 students will wear the instrument for three consecutive days during each measurement period.
Waist and hip ratio
A non-elastic metric tape capable of 1mm repeatability will be used to measure waist and hip circumferences. The measurement will be taken twice for each assessment and will be read to the nearest 0.50 cm, using umbilicus as a landmark and keeping the measuring tape horizontal to the ground. A third measurement will be taken if the difference between the first two measurements is greater than 1 cm. An average of the measurements will be entered as the datum.
Child Treatment Questionnaire
The purpose of this questionnaire is to assess family involvement in the LA Health program. Questions will assess if children have discussed program elements with their parents. A 9 item questionnaire was developed and assesses parent-child discussions across all treatment arms in the RCT.
Measurement of participation in the internet-based interventions
We have developed a highly advanced tracking system for website utilization and participant feedback. The computer server automatically tracks utilization of the website. Utilization of the LA Health website will also be tracked by the following methods: 1) completion of quizzes following each session, 2) percent correct answers to the questions in each quiz, and 3) number of emails to internet counselors.
Prevention Programs
The research design requires three intervention arms in the RCT: (1) primary prevention, which consists of the environmental approach for prevention of weight gain, (2) combination of the primary and secondary prevention, which consists of the internet-based secondary prevention program, as well as the primary prevention program, and (3) a no-treatment control group. For all three intervention arms, all students in the relevant grades (beginning with grades 4 to 6 in Year 1) are provided all components of the prevention programs with one exception. Only those students who were enrolled in the study and assigned to the combination of the primary and secondary prevention are provided on-line counseling. The following sections describe these three intervention arms in further detail. As noted earlier, a fourth group will be followed during the three-year period to observe secular changes in BMI z-scores in a group of students who are not participants in a formal obesity prevention (LA Health) or educational enhancement (LA GEAR UP) program.
Primary Prevention Program
Primary prevention program components
The primary prevention program will consist only of providing campaign materials in the classroom, hallways, and other locations within the school via media (e.g., posters). The descriptions of these campaigns are presented in Table 3. The primary prevention program has three components: 1) healthy diet promotion, 2) physical activity promotion, and 3) a program for families.
Table 3.
Schedule of environmental campaigns to promote healthy eating and activity in the LA Health Primary Prevention Program
| LA Health Environmental Campaigns | |||
|---|---|---|---|
| # | Months | Campaign | Description |
| 1 | Feb–Mar 2007 | Food and Fun: An Introduction to Healthy Nutrition and Physical Activity | The goals of this campaign are to provide an introduction to healthy nutrition and physical activity. The students will learn about proper portion sizes and reading nutrition labels. Indoor physical activity will be encouraged through the provision of equipment and activities. |
| 2 | Apr–May 2007 | Live each day the rainbow way: Try a variety of fruits and vegetables and physical activity each day | The goals of this campaign are to increase fruit and vegetable intake, reduce TV watching and computer use, and learn about the benefits of physical activity. The students will learn how to make a rainbow on their plates by incorporating a variety of fruits and vegetables into every meal, and will also learn fun, safe, methods of activity to incorporate into their daily routine. |
| ***Summer 2007- No campaigns*** | |||
| 3 | Sept–Oct 2007 | Energy Balance: Keep Your Weight in Check | The goal of this campaign is to increase students’ awareness of energy intake versus energy expenditure and weight gain. Students will identify and assess healthy and unhealthy habits. |
| 4 | Nov–Dec 2007 | Health is the Reason to Get Moving and Cooking this Holiday Season | The goal of this nutrition campaign is to increase the students’ participation in the kitchen and to increase family cooking and fun and fitness during the holidays. Students will learn recipes and techniques for helping out in the kitchen and will be given information on how to increase their activity over the holidays. |
| 5 | Jan–Feb 2008 | Dishing out the facts on physical fitness and dietary fat | This campaign will discuss the role of fat in the diet and differentiate between healthy and unhealthy fat. Additional goals are to learn about the differences between aerobic, resistance, and flexibility exercises, and their relationship to fitness. Students will be provided with examples of different kinds of exercise, and will learn about appropriate amounts of fat in the diet. |
| 6 | Mar–Apr 2008 | Fast Food Slows You Down, Let’s Race Across America | The goals of this campaign are to decrease the frequency of fast food meals and increase the frequency of healthy meals at home, family self-monitoring, and goal setting The students will learn fast food nutritional facts, how to use the food guide pyramid, and recipes for fast, healthy meals at home. The students will also learn how to set physical activity goals by monitoring their activity. The students will learn to increase family self-monitoring and goal setting. This campaign entails a pedometer challenge where the students will be given pedometers and will learn how to monitor their activity. |
| 7 | May 2008 | “Moove” and Eat to a Healthy Beat! | The goal of this campaign is to increase and/or maintain low-fat dairy consumption and increase consumption of whole grains, as well as the benefits of physical activity. The students will learn the importance of low-fat dairy in the diet, foods that should be incorporated into the diet and methods on how to incorporate those foods. Additional goals are to provide information on the physical and mental benefits of exercise, and how to prevent injuries. |
| ***Summer 2008-No campaigns*** | |||
| 8 | Sept–Oct 2008 | Healthy and Cool: Water plus Activity is the Rule | The goals of this campaign are to increase water intake and increase lifestyle physical activity. The students will learn about the value of water in their diet and the negative aspects of consuming beverages with added sugars. They will also learn about lifestyle activity and ways to incorporate these into their daily lives. |
| 9 | Nov–Dec 2008 | Be a SMART Star Wherever You Are…Supermarket, Restaurant, and PE! | The goals of this campaign are to increase the students’ knowledge of healthy choices to make in the supermarket and in a restaurant. The students will learn the nutritional value of food items, how to read food labels, and how to make wise, healthy decisions in these environments. Also this campaign will focus on goal setting for improved fitness. Students will be encouraged to utilize all components of fitness to develop a realistic plan for improving their fitness. The students will also be given access to various pieces of fitness related physical activity equipment. |
| 10 | Jan–Feb 09 | How Sweet it is: The Truth about Sugar and Making Flexibility Fun | The goals of this campaign are to provide information on the harmful effects of over consumption of added sugars and to discuss the role of flexibility. This campaign will highlight the hidden sugars in food items and ways to reduce added sugar intake. The students will be provided with examples of different stretching exercises as it relates to safety and prevention of injuries. |
| 11 | Mar–Apr | Spice up your life with a variety of food and activity. | The goals of this campaign are to provide information on the importance of eating a variety of foods and physical activity intensity. Students will be provided with information on balancing their diet to include a variety of foods with an emphasis on incorporating whole grains. Also children will learn what activities qualify as moderate intensity and why engaging in moderate intensity activities is important. |
| 12 | May 09 | Let's review! Tips to a healthier you. | This campaign will review energy balance. |
Healthy Diet Promotion
Several changes will occur throughout the school that are compatible with conventional nutrition recommendations (e.g., five fruits and vegetables per day, less than 30% of dietary energy from total fat, less than 10% of dietary energy from saturated fat, and 20 to 30 grams of fiber/day) and are intended to facilitate the Child Nutrition Program in meeting USDA guidelines for the National School Lunch Program [23]. Cafeteria staff in collaboration with research dieticians will increase the availability of fruits, vegetables, and whole grains. Acceptability of foods will be enhanced by producing an appealing presentation. Furthermore, recipes for foods will be modified while trying to have the least impact on food procurement practices. Cafeteria staff will also be prompted to reduce the availability of foods with high dietary fat and sugar. The cafeteria staff will be provided continuing education regarding proper cooking methods, serving correct portion sizes and limiting “seconds” of high fat foods. Consistent with these modifications, LA Health stars will direct children to healthy food choices in the school cafeterias. The “Healthy Tip of the Day” will be recognized by the classroom teacher or cafeteria manager and communicated to the students prior to lunch. In conjunction with the WIC Reauthorization Act of 2004 [24] and Act 331 of the Louisiana Legislature [25], advertisement and consumption of soft drinks, candy, and fast foods will be limited and eventually eliminated. Foods available in vending machines will be modified to promote the consumption of non-caloric beverages, 100% fruit juices, and healthy snacks that are derived from a list published by PBRC and the LA Department of Education. Enforcement of these practices is accomplished by evaluations by the research staff every three to four months with corrective action taken as needed.
Physical Activity Promotion
The physical activity promotion program is designed to increase physical activity and decrease sedentary behavior in three school settings: the classroom, recess, and physical education (PE). In the classroom, these goals will be met by incorporating regular 5 minute physical activity breaks after 30 minutes of instruction (30 minute rule), providing suitable indoor physical activity equipment (Physical Activity Centers – “PACs”), by engaging in educational activities that increase physical activity, and by placing LA Health posters in the classroom that are designed to promote decreased sedentary behavior and increased physical activity. Teachers are encouraged to increase physical activity during recess by provision of outdoor equipment supplied in PACs. The Sports, Play and Active Recreation for Kids (SPARK) curriculum will be provided to support PE teachers. SPARK is designed to provide at least 30 minutes of physical education per day, includes both skill-related and fitness-related activities, and has been shown to be effective in increasing physical activity in PE classes [48].
Primary Prevention Program for Families
Family members will learn the same principles taught to the students through the primary prevention program at school. Bi-monthly newsletters will be sent home with the student providing campaign-specific information, suggestions on how to alter the home environment consistent with campaign topics, and specific activities that children are to complete at home with their parents. Family involvement is encouraged by the distribution of health promotion items, including MyPyramid refrigerator magnets and More Matters rulers. Furthermore, menus will be sent to parents with emphasis placed on the food choices recommended by the LA Health program.
Combination of Primary and Secondary Prevention
The secondary prevention program will be administered in tandem with the primary prevention program for schools randomized to this treatment arm (primary prevention plus secondary prevention). The intervention incorporates all three components of the primary prevention plus the secondary prevention program, which is modeled after the HIPTeens project [26]. The secondary prevention program has two components: 1) classroom curriculum and 2) internet counseling and education.
Classroom curriculum
Children in the primary prevention plus secondary prevention treatment arm will receive weekly lessons on healthy eating and exercise that are delivered by designated teachers who are trained to deliver the intervention in professional development workshops. The lessons include a 20 to 25 minute interactive didactic segment followed by hands-on activities to help the children learn and apply the material to their lives. The teachers will deliver standardized material to the children and the topic of each classroom lesson will correspond to the content of the internet lesson. An outline of the lesson topics is provided in Table 4. Children complete the internet lesson after each classroom lesson or during the next scheduled class. As shown in Table 4, the schedule of topics typically calls for completion of two topics per month.
Table 4.
Content of classroom and internet lessons for children in the primary plus secondary prevention condition. The content of the classroom and internet lessons correspond to each other.
| Year 1 (August 2006–May 2007) | |
|---|---|
| Month | Lesson |
| March 2007 | |
| Standardized Testing (only one lesson is delivered) | Overview of health outcomes |
| April 2007 | Reducing sedentary behaviors |
| Why is exercise so important? | |
| May 2007 | High calorie vs. low calorie foods |
| One food vs. another – how they fill you up | |
| June–July 2007 | School is out, no lessons |
| Year 2 (August 2007–May 2008) | |
| September 2007 | Sweetened drinks vs. water |
| Energy balance: Balance between caloric intake and exercise | |
| October 2007 | Goal Setting – Vague vs. Clear |
| Portion Control | |
| November 2007 | Tips on how to increase physical activity |
| Introduction to 5-A-Day program | |
| December 2007 | Family fun indoor activities |
| Healthy holiday activities / Healthy holiday snacks | |
| January 2008 | Aerobic activities |
| Fast Food Survival | |
| February 2008 | Fat in foods |
| Warm-up and Cool-down to Prevent Injuries | |
| March 2008 | |
| Standardized Testing (only one lesson is delivered) | Stretching and flexibility exercises |
| April 2008 | Let’s talk about fried foods |
| The purpose of various exercises | |
| May 2008 | Fruit facts and the Variety of Veggies |
| How Much and Why do You Watch TV? | |
| June–July 2008 | School is out, no lessons |
| Year 3 (August 2008–May 2009) | |
| September 2008 | High fiber foods |
| Getting the family on board: How can they help you meet your goals | |
| October 2008 | Eating healthy with your friends |
| Planning ahead for get-togethers | |
| November 2008 | Introduction to the grocery store and food labels |
| Food safety….what you need to know | |
| December 2008 | Planning ahead to increase physical activity / Healthy snacks to go |
| Aerobic Activity for the Whole Family | |
| January 2009 | The keys to maintaining an active lifestyle |
| Planning ahead for a healthy breakfast | |
| February 2009 | Portion Sizes (repeat) |
| Food and Activity “Cues” | |
| March 2009 | Ways to motivate yourself to engage in physical |
| Standardized Testing (only one lesson is delivered) | activity |
| April 2009 | Energy balance: Balance between caloric intake and exercise (repeat) |
| High calorie vs. low calorie foods / One food vs. another- how they fill you up (repeat) | |
| May 2009 | Let’s talk about fried foods (repeat) |
| Overview of health outcomes (repeat) | |
Internet Counseling and Education
The primary plus secondary prevention program also includes an internet-based intervention. Each child whose school was assigned to the primary plus secondary prevention condition is provided with login identification and is trained by school coordinators and teachers to use the website. One feature of the website is the ability of the child to send an email to an internet counselor who is located at the research site and to participate in online “chats” with an internet counselor at specified days/times (these times generally coincide with delivery of the classroom lesson). The internet counselor is trained to provide support and instruction related to healthy behavior change. The children can also access the website and email an internet counselor from home or any location that has internet access. Access to the website and utilization of the internet program are monitored by the primary plus secondary prevention program team, which is led by a clinical psychologist and includes the computer programmers who developed the website, registered dietitians, and school coordinators. Email communication outside the classroom is asynchronous, i.e. does not require an online direct response from an internet counselor. During school, children will complete internet lessons that correspond to the classroom lesson (the lesson topics are summarized in Table 4). The internet lessons include reviewing educational material on the website and completing a quiz (with questions related to the topic) to evaluate the extent to which content of the topic was learned by each student. The students typically visit the website at least every two weeks during the classroom lesson. The typical duration of an internet visit is about 15 minutes per student. Children who did not sign a consent form and are not enrolled in the study are able to logon to the website using a generic identification and password. These children have access to the lesson, quiz, and interactive features of the website, but they do not have access to an internet counselor, nor can the intervention team identify these children.
Unlike the classroom lesson, during which the content of the material is standardized, the internet component is designed to promote weight loss in overweight students (baseline BMI %tile ≥ 85th %tile) and improve health behaviors in the other students to promote weight maintenance. The website is programmed to automatically deliver these two components to the students of the two weight classes. The weight status (above or below 85th %tile) of each student is determined by baseline measurement of weight and height and is coded into the website as a part of each student’s profile (a child’s status can not change based on measurements collected during the study). From the perspective of classroom instruction, children of different weight status are treated identically, but the overweight children (at baseline) receive information on weight loss when they logon to the website using their unique profile. The internet counselors can observe the child’s weight status as they chat online with the student; therefore, the internet counselors provide direct recommendations to reduce calorie intake and increase exercise to lose weight for children who are ≥ 85th BMI %tile. The children who are not overweight (at baseline) will receive information on nutrition and exercise that is designed to promote weight maintenance. The format and appearance of the websites for both overweight and non-overweight children are identical. These safeguards make it unlikely that any child will be “singled out” due to weight status. From the participant’s perspective, the website appears to be identical for all students.
In addition to the lessons outlined in Table 4, the website includes: 1) automated interactive components (e.g., interactive graphics that display information about healthy food choices and fun activities) and 2) nutrition education and behavior modification.
No-Intervention Control
Schools assigned to this treatment arm will not receive a weight gain prevention program but will participate in the complete data collection process throughout the three-year study. This control group will be given access to a website that provides information on stress management, and study skills. This treatment arm will receive the educational enhancement program (LA GEAR UP), which will control for nonspecific effects (that targets academic achievement but does not target weight gain prevention).
Observation Control Group
Uncontrolled social factors might substantially impact weight gain in students over the three-year study. Based upon this possibility an untreated control was included in the study design. Previous research findings lead to the hypothesis that we should observe a progressive increase in average weight over the 30-month intervention period for students in the observation control arm. Identifying and measuring an untreated, but demographically similar, student population permits a more precise accounting of the fashion in which the treatment arms will impact the hypothesized weight gain. To accomplish this objective, a purely observational group has been recruited from schools that are not participating in LA GEAR UP or other educational enhancement programs that emphasize health improvement. This recruitment is summarized in Figure 2.
Statistical Considerations
Statistical Power Analysis
The LA Health study has three levels of treatment: control, primary prevention program, and a combination of primary and secondary prevention programs. The primary endpoint is the change in age-adjusted gender-specific z-scores [36] after three years of intervention. Power analysis for this endpoint formed the basis for determining the number of school clusters and the number of students from each school for the trial.
During the planning phase, we anticipated that six school clusters (with an average of 263 students) would be available for each treatment arm, and that, on average, 131 students per school cluster (based upon 50% recruitment rate) would enroll in the project, and with 25% attrition, 98 students per school cluster would complete the study. The power analysis was based on the change in adjusted BMI z-scores over 3 years for each treatment group. To evaluate the outcome of the study, the primary comparisons included: (1) comparison between the primary prevention program and the control, (2) comparison between the primary plus secondary prevention program and the control, and (3) comparison between two prevention programs for the overweight population with baseline BMI %tile ≥ 85th percentile. The statistical power calculations were performed for all three comparisons.
Specification of Correlations
Due to the nature of cluster randomized trial of this study, the school level Intraclass Correlation Coefficient (ICC) was considered. Using the data from the Wise Mind study [22], the ICC between schools in BMI z-score was 0.003 for the whole population and 0.015 for the overweight population.
Specification of Detectable Differences and Standard Deviations
Based on data from the Wise Mind study [22], we estimated that the overall standard deviation in BMI z-scores over a year was 0.40. Minimum expected mean differences in BMI z-score changes between the prevention programs and the control were specified as 0.09 in the statistical power calculations. For the overweight (baseline BMI ≥ 85th %tile) population, a standard deviation of 0.30 was estimated, and the power required to detect BMI z-score changes at least 0.125 between the prevention programs was calculated. These BMI z-score differences were selected on the premise that they represent minimal differences that are meaningful for directing public health policy. From these statistical power calculations, we determined that we should recruit a minimum of 1,926 students and 18 school clusters (six per treatment arm), assuming an attrition rate of 25% that would result in a final study sample of 1,445 students. As shown in Figure 2, we recruited 2,102 students for the RCT. With 25% attrition, we project 1,578 students will be available for the study at Month 30. Subsequent power analyses based on 17 school clusters indicated that recruitment goals exceeded statistical power needs.
Statistical power was also calculated to examine the BMI z-score trends for the observation control group. The power calculation was performed for a two-sided dependent t-test for changes in BMI z-scores, with a type I error rate of .05, after incorporating the within-cluster correlation. We concluded that six school clusters with an average of 75 students per school cluster would assure 80% power to detect a 0.075 difference (change) in BMI z-scores over 3 years for the whole population; and 25 students per school (total = 150) would assure 80% power to detect a 0.10 BMI z-score difference (change) for the overweight population. These calculations suggested that we had adequate power to detect relatively small changes in BMI z-scores (i.e., at least 0.075 BMI z-score change) by recruiting a total of 600 participants in the observation control group, with approximately 200 children with BMI %tile ≥ 85th %tile. As shown in Figure 2, we have recruited and collected baseline data for 607 students. With an attrition rate of 25%, we anticipate 455 students will be available for measurement at Month 30. In summary, recruitment goals for the RCT and observation control group were met.
Data Management
This study follows an intention-to-treat design. Every effort will be made to encourage students to complete all assessments. The drop out rate for the proposed study is predicted to be 25% based on our 12% drop out rate for the first 18 months of the Wise Mind study [22]. Reasons and time of drop out will be documented. Each participant will be issued a unique randomly allocated identification number that will be retained throughout the study. Only trained and certified examiners will collect data.
Statistical Analyses
The last observation carried forward approach will be used to impute missing data. The results will be compared with results from the complete case analysis, in a sensitivity analysis, to evaluate the reliability of the findings [49]. The proposed study has 3 levels of treatment: control, primary intervention, and primary intervention plus secondary intervention. The primary endpoint is the change in the age-adjusted gender-specific BMI z-score after 30 months of intervention. Only two visits, baseline and end-of-study will be included for the purpose of testing intervention effects. An interim data analysis will be conducted to assess safety and to evaluate the progression of changes in the dependent variables. The primary aim of the study is to: a) compare either intervention arm to the control group for prevention of inappropriate weight gain (as measured by BMI z-scores, in relation to BMI %tile); and b) compare the primary plus secondary intervention arm to the primary intervention arm for the overweight population (baseline BMI % tile ≥ 85th percentile).
Two analytic strategies will be considered to test the intervention effect. First, using a mixed model ANCOVA method with treatment groups as fixed effect, the analysis of end-of-study change from baseline (Month 30 – Baseline) will be conducted. Adding baseline BMI z-scores as a covariate, time-related information is included without modeling time explicitly in the analysis. Alternatively, a mixed–model ANCOVA will be performed to analyze the Pretest-Posttest data. In this analysis, the intervention arms and time are fixed effects, and the school within treatment arm and subject are random effects.
All secondary aims will be analyzed with the similar approach as described for the primary aim. Chi-square analysis will be used to test for differential rates of weight gain prevention across the four treatment arms. The first secondary aim will be tested with a mixed-model ANCOVA with only pre and post measurements for observation control schools. In addition, a mixed-model ANCOVA will be performed with covariates of gender, race, and socioeconomic status.
For secondary aims 2 and 3, interactions between treatment arm and race and sex will be tested using separate stratified analyses for each stratification factor. When the effects of race are tested, socioeconomic status at baseline and baseline BMI z-scores will be included as covariates. When the effects of gender are tested, race, socioeconomic status, and BMI z-scores at baseline will be included as covariates.
For secondary aims 4 and 5, the two intervention arms will be combined to compare with no-treatment control group. The dependent variables will be changes in the food selections and food intake, and covariates will be baseline food selections and food intake, respectively. Additional covariates will be included as appropriate: baseline age, gender, and baseline BMI %tile.
For mediation analyses, putative mediator variables will be tested against the following criteria [50]: 1) the weight gain prevention program must prevent weight gain relative to the control group, 2) the weight gain prevention program must significantly change a putative mediator variable, (e.g., increased physical activity, fruit intake, or reduced caloric intakes relative to the control group), 3) the putative mediator variable must be associated with prevention of weight gain when the effects of the prevention program are removed, and 4) this association must be statistically significant. The mediators and moderators variables that will be tested will be: eating habits/food intake, physical activity, psychosocial variables including mood, social support for diet, and social support for physical activity.
All statistical analyses will be performed using Statistical Analysis Software (SAS) 9.1. The analyses will be conducted by the single-stage, mixed model strategy to take care of the special design feature of cluster (group) randomized trials, in which identifiable clusters or groups of individuals rather than actual individual members are randomized to conditions with observations taken on members of those groups [51].
Federal Sponsors
LA Health is sponsored by the National Institute for Child Health and Human Development of the National Institutes of Health and the U.S. Department of Agriculture. Funding for the Professional Development Program was provided by a grant from the U.S. Department of Education administered by the Louisiana GEAR UP program. LA Health is a single-site study.
Executive Advisory Committee
Policy decisions are made by a five-person committee that includes scientists and community and state education leaders. This committee meets once or twice per year to evaluate progress and to resolve issues related to the conduct of the study.
Data and Safety Monitoring Board
Safety issues and assessment of risks versus benefits of the study are evaluated by a three-person committee that includes scientists and medical professionals. This board meets every six months.
Discussion and Conclusions
The LA Health project addresses an important health problem, i.e., prevention of childhood obesity, in a special and highly vulnerable population, i.e., children from rural communities. Most of these children are from poor families who could not readily access appropriate health care or preventive services. Furthermore, a majority of the children are African-American. The prevention programs that will be tested in this controlled study include elements of primary and secondary prevention. They are delivered in schools and if they are successful, can be implemented on a much larger scale.
Acknowledgements
The authors greatly appreciate the assistance and support that the LA Health project has received from Kerry Davidson, Ph.D., the LA GEAR UP program, and the LA Board of Regents. We would also like to thank the superintendents, principals, and staff at each of the schools in the project. We express our appreciation to Melinda Sothern, Ph.D. and Larry Webber, Ph.D. for their role as consultants to the project.
Grant Support: This project was supported by the National Institute for Child Health and Human Development of the National Institutes of Health (R01 HD048483) and the U.S. Department of Agriculture (58-6435-4-90). The clinical trial number for this project is: NCT00289315. In addition, this work was partially supported by the CNRU Center Grant #1P30 DK072476 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by NIDDK.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.World Health Organization. Dietary changes and exercise needed to counter chronic diseases worldwide. 2003. Rev Panam Salud Publica. 2003;13:346–348. [PubMed]
- 2.Norman JE, Bild D, Lewis CE, Liu K, West DS. The impact of weight change on cardiovascular disease risk factors in young black and white adults: the CARDIA study. Int J Obes Relat Metab Disord. 2003;27:369–376. doi: 10.1038/sj.ijo.0802243. [DOI] [PubMed] [Google Scholar]
- 3.Rashid MN, Fuentes F, Touchon RC, Wehner PS. Obesity and the risk for cardiovascular disease. Prev Cardiol. 2003;6:42–47. doi: 10.1111/j.1520-037x.2003.01358.x. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services. Rockville, MD: The Surgeon General's Call to Action to Prevent and Decrease Overweight and Obesity. 2002
- 5.U.S. Department of Health and Human Services. Rockville, MD: Strategic Plan for NIH Obesity Research: A Report of the NIH Obesity Research Task Force. 2004
- 6.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 7.National Center for Health Statistics. Prevalence of overweight and obesity among adults: United States. 2001
- 8.Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 9.Berkowitz RI, Stunkard AJ. Development of childhood obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. New York: Guilford; 2002. pp. 515–531. [Google Scholar]
- 10.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 11.Dietz WH. The obesity epidemic in young children. Reduce television viewing and promote playing. BMJ. 2001;322:313–314. doi: 10.1136/bmj.322.7282.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hassink S. Problems in childhood obesity. Prim Care. 2003;30:357–374. doi: 10.1016/s0095-4543(03)00014-9. [DOI] [PubMed] [Google Scholar]
- 13.Koplan JP, Liverman CT, Kraak VI, Wisham SL, editors. Progress in Preventing Childhood Obesity How Do We Measure Up? Washington, DC: Institute of Medicine; 2007. Committee on Progress in Preventing Childhood Obesity. [Google Scholar]
- 14.Summerbell CD, Waters E, Edmunds LD, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews. (I (ed)) 2005 doi: 10.1002/14651858.CD001871.pub2. 2005. [DOI] [PubMed] [Google Scholar]
- 15.Flynn MA, McNeil DA, Maloff B, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with 'best practice' recommendations. Obes Rev. 2006;7 Suppl 1:7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- 16.Caballero B. Obesity prevention in children: opportunities and challenges. Int J Obes Relat Metab Disord. 2004;28 Suppl 3:S90–S95. doi: 10.1038/sj.ijo.0802797. [DOI] [PubMed] [Google Scholar]
- 17.Fowler-Brown A, Kahwati LC. Prevention and treatment of overweight in children and adolescents. Am Fam Physician. 2004;69:2591–2598. [PubMed] [Google Scholar]
- 18.Wake MA, McCallum Z. Secondary prevention of overweight in primary school children: what place for general practice? Med J Aust. 2004;181:82–84. doi: 10.5694/j.1326-5377.2004.tb06179.x. [DOI] [PubMed] [Google Scholar]
- 19.United Health Foundation. America's Health: State Health Rankings. 2007
- 20.Smith J, Lensing S, Horton JA, et al. Prevalence of self-reported nutrition-related health problems in the Lower Mississippi Delta. Am J Public Health. 1999;89:1418–1421. doi: 10.2105/ajph.89.9.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 22.Williamson DA, Copeland AL, Anton SD, et al. Wise Mind project: a school-based environmental approach for preventing weight gain in children. Obesity. 2007;15:906–917. doi: 10.1038/oby.2007.597. [DOI] [PubMed] [Google Scholar]
- 23.Melancon K, Dwyer J. Popular diets for treatment of overweight and obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of obesity treatment. New York: Guilford; 2002. pp. 249–282. [Google Scholar]
- 24.United States of America: Child Nutrition and WIC Reauthorization Act of 2004. 2004
- 25.State of Louisiana: Foods and beverages other than school breakfast or lunch in public elementary and secondary schools; legislative findings; restrictions. 2005
- 26.Williamson DA, Martin PD, White MA, Newton R, Walden H, York-Crowe E, et al. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eat Weight Disord. 2005;10:193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- 27.Li R, Serdula M, Bland S, et al. Trends in fruit and vegetable consumption among adults in 16 US states: Behavioral Risk Factor Surveillance System, 1990–1996. Am J Public Health. 2000;90:777–781. doi: 10.2105/ajph.90.5.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicklas TA, O'Neil CE, Berenson GS. Nutrient contribution of breakfast, secular trends, and the role of ready-to-eat cereals: a review of data from the Bogalusa Heart Study. Am J Clin Nutr. 1998;67:757S–763S. doi: 10.1093/ajcn/67.4.757S. [DOI] [PubMed] [Google Scholar]
- 29.Luepker RV, Perry CL, McKinlay SM, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative group. JAMA. 1996;275:768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 30.Caballero B, Clay T, Davis SM, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–1038. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dowda M, Ainsworth BE, Addy CL, Saunders R, Riner W. Environmental influences, physical activity, and weight status in 8- to 16-year-olds. Arch Pediatr Adolesc Med. 2001;155:711–717. doi: 10.1001/archpedi.155.6.711. [DOI] [PubMed] [Google Scholar]
- 32.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- 33.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. School-based obesity prevention: a blueprint for taming the epidemic. Am J Health Behav. 2002;26:486–493. doi: 10.5993/ajhb.26.6.9. [DOI] [PubMed] [Google Scholar]
- 34.Robinson TN, Killen JD. Obesity prevention for children and adolescents. In: Thompson JK, Smolak L, editors. Body image, eating disorders, and obesity in youth: Assessment, prevention, and treatment. Washington, DC: American Psychological Association; 2001. pp. 261–292. [Google Scholar]
- 35.Harsha DW, Bray GA. Body composition and childhood obesity. In: Bray GA, editor. Obesity. Philadelphia: W. B. Saunders Company; 1996. pp. 871–885. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control. CDC Growth Charts: United States. 2000
- 37.Williamson DA, Martin PD, Allen HR, et al. Changes in food intake and body weight associated with basic combat training. Mil Med. 2002;167:248–253. [PubMed] [Google Scholar]
- 38.Martin CK, Newton RL, Jr, Anton SD, et al. Measurement of children's food intake with digital photography and the effects of second servings upon food intake. Eat Behav. 2007;8:148–156. doi: 10.1016/j.eatbeh.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 39.Hackett AF, Kirby S, Howie M. A national survey of the diet of children aged 13 – 14 years living in urban areas of the United Kingdom. J Hum Nutr Diet. 1997;10:37–51. [Google Scholar]
- 40.Johnson B, Hackett A, Roundfield M, Coufopoulos A. An investigation of the validity and reliability of a food intake questionnaire. J Hum Nutr Diet. 2001;14:457–465. doi: 10.1046/j.1365-277x.2001.00320.x. [DOI] [PubMed] [Google Scholar]
- 41.Sallis JF, Strikmiller PK, Harsha DW, et al. Validation of interviewer- and self-administered physical activity checklists for fifth grade students. Med Sci Sports Exerc. 1996;28:840–851. doi: 10.1097/00005768-199607000-00011. [DOI] [PubMed] [Google Scholar]
- 42.Parcel GS, Edmundson E, Perry CL, et al. Measurement of self-efficacy for diet-related behaviors among elementary school children. J Sch Health. 1995;65:23–27. doi: 10.1111/j.1746-1561.1995.tb03335.x. [DOI] [PubMed] [Google Scholar]
- 43.Edmundson E, Parcel GS, Feldman HA, et al. The effects of the Child and Adolescent Trial for Cardiovascular Health upon psychosocial determinants of diet and physical activity behavior. Prev Med. 1996;25:442–454. doi: 10.1006/pmed.1996.0076. [DOI] [PubMed] [Google Scholar]
- 44.Kovacs M. The Children's Depression Inventory: Manual. New York: Multi-Health Systems; 2001. [Google Scholar]
- 45.Maloney MJ, McGuire JB, Daniels SR. Reliability testing of a children's version of the Eating Attitude Test. J Am Acad Child Adolesc Psychiatry. 1988;27:541–543. doi: 10.1097/00004583-198809000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Netemeyer SB, Williamson DA. Assessment of eating disturbance in children and adolescents with eating disorder and obesity. In: Thompson JK, Smolak L, editors. Body image, eating disorders, and obesity in youth: Assessment, prevention, and treatment. Washington, D. C.: American Psychological Association; 2001. pp. 215–234. [Google Scholar]
- 47.Plasqui G, Westerterp KR. Physical activity assessment with accelerometers: an evaluation against doubly labeled water. Obesity. 2007;15:2371–2379. doi: 10.1038/oby.2007.281. [DOI] [PubMed] [Google Scholar]
- 48.Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Faucette N, Hovell MF. The effects of a 2-year physical education program (SPARK) on physical activity and fitness in elementary school students. Sports, Play and Active Recreation for Kids. Am J Public Health. 1997;87:1328–1334. doi: 10.2105/ajph.87.8.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319:670–674. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 51.Murray DM. Design and analysis of group-randomized trials. New York: Oxford University Press; 1998. [Google Scholar]