Abstract
Objective
It is commonly believed that some features of borderline personality disorder improve as individuals reach their late 30s and 40s. The current study examined age-related change in borderline criteria and functional impairment, testing the hypothesis that older age would be associated with relatively more improvement than younger age.
Method
216 male and female participants with borderline personality disorder were followed prospectively with yearly assessments over 6 years.
Results
Participants showed similar rates of improvement in borderline features regardless of age. A significant age by study year interaction showed functioning in older subjects to reverse direction and begin to decline in the latter part of the follow-up, in contrast to younger subjects who maintained or continued improvement over the six years. Despite the decline, functioning for the older subjects was comparable to or slightly better at year 6 than at year 1.
Conclusion
Improvement in borderline features is not specific to the late 30s and 40s. There may be a reversal of improvement in functioning in some borderline patients in this older age range.
Keywords: Borderline personality disorder, Longitudinal course, Age
Significant Outcomes.
Age was not associated with differential improvement in borderline personality disorder criteria over the 6 years of follow-up.
Age was associated with a differential course in functioning. Despite overall improvement, functioning in older borderline participants began to decline mid way through the follow-up, in contrast to maintenance or continuing improvement in younger participants.
Limitations.
Study participants began the study at different ages, and there could be age-related sampling biases influencing the findings.
The majority of participants were recruited as outpatients, and findings may not generalize to inpatient samples. The majority of participants received treatment, and the results may not generalize to untreated samples.
Findings are limited by the number of participants at different ages, the absence of subjects older than age 45 at the study baseline, and the length of follow-up.
It is commonly believed that symptoms of Borderline Personality Disorder (BPD) lessen with age. For example, the DSM-IV states: “The impairment from the disorder and the risk of suicide are greatest in the young-adult years and gradually wane with advancing age” (1). Further noted is that the majority of those with BPD attain greater stability in relationships and vocational functioning in their 30s and 40s.
Early studies leading to these conclusions included previously hospitalized patients with chart review diagnoses of BPD, followed up years later. McGlashan (2) assessed 81 such patients discharged over a period of 25 years, with follow-up averaging 15 years after discharge and a mean age at follow-up of 47 years. Outcome was found to vary as a function of time since discharge, with the best functioning in subjects in their 40s. McGlashan (2) concluded “For the BPD patients…the clinical shibboleth that patients with personality disorders improve with age seems borne out by our findings, especially in the realms of symptomatic and instrumental functioning” (p. 29). However, subjects at the older end of the cohort’s age group, generally in their 50s at follow-up, like the younger subjects, showed poorer functioning, suggesting a possible reappearance of difficulties with advancing age.
Another study followed up 100 former inpatients with BPD based on chart review an average of 15 years following hospitalization and a mean age of 41 at follow-up (3). Only 25 subjects were still rated as borderline and impulsive behavior dropped off almost entirely with time. The authors concluded that the decreases in BPD scores at follow-up supported the idea that active borderline pathology decreases with age. Like McGlashan (2), they reported a shift away from intense and unstable relationships, but in the direction of avoidance of relationships.
Stone reported on the long-term outcome (10 to 25 years) of a large sample (N=502) of inpatients later classified as having BPD or borderline personality organization (4). Most patients were rated as “good” or “recovered” (GAS score > 70) as they moved into their 30s and 40s. Stone described their course as a “ladle-shaped” curve, with a “dip” throughout the 20s, followed by a steady and stable improvement in function throughout the 30s and beyond (5). He noted, though, that a subgroup that remained chronically angry often experienced a second downturn in their mid-40s.
Stevenson and colleagues (6) used a cross-sectional design to test the hypothesis that impulsivity declines with age in BPD. Linear regression analyses examining age in relationship to affective disturbance, relationship disturbance, cognitive disturbance, and impulsive behavior were conducted in a sample of 123 outpatients with BPD (mean age of 32, range of 18 to 52). Impulsive behavior was significantly associated with age, with older patients rated as less impulsive; there was no age association with the other three domains. The findings supported the idea that “…the behavioral manifestations [of BPD] ‘burn out’ with age” (6) (p. 166).
Although all of the longitudinal studies show a decrease in manifestations of BPD, most notably in the more impulsive behaviors, the extent to which decrease in such symptoms is a function of age rather than time alone is unclear, as age and time are confounded. And in contrast to the above studies, Zanarini et al. (7) identified younger age as one of several predictors of earlier time to remission over 10 years of follow-up, challenging the belief that older age brings more improvement in BPD.
Aims of the Study
The aim of the current study is to examine age-related change in BPD using six years of prospective follow-up from a naturalistic longitudinal study of personality disorders. Based on prior literature, our hypothesis is that among BPD subjects, older age is associated with more improvement in BPD criteria and in psychosocial functioning.
Material and methods
Participants
The Collaborative Longitudinal Personality Disorders Study (CLPS) is a multi-site, naturalistic, longitudinal study examining the course of four DSM-IV personality disorders. This study has been in compliance with Human Subjects Internal Review Boards at each participating site since its inception. Detailed information regarding the study procedures and sample characteristics has been previously published (8). In brief, an initial sample of 668 participants with at least one of four personality disorders (schizotypal, borderline, avoidant, or obsessive-compulsive), or with major depressive disorder and no personality disorder, was recruited primarily from outpatient clinical sites associated with the four CLPS recruitment sites. All were currently or previously in treatment or seeking treatment. To be included, participants had to be within the age range of 18 to 45, and could not have any current condition that precluded a valid interview (e.g. active psychosis, acute substance intoxication or withdrawal), or a history of schizophrenia or schizoaffective disorder. All participants provided written informed consent after a full explanation of study procedures. Earlier publications have described high rates of improvement and remission in the four personality disorders followed in the CLPS (9, 10).
The current investigation includes participants meeting criteria at baseline for BPD. Of this baseline sample of 240, 24 participants were excluded because they did not complete 2 or more years of follow up. The 24 excluded participants did not significantly differ from the 216 in the analytic sample in demographics, Axis I comorbidity, or number of BP criteria. The numbers of participants included from study years 1 – 6 are: 216, 216, 204, 200, 195, and 188, respectively. At baseline these participants had a mean age of 31.97 (SD=8.06). Table 1 lists the demographic characteristics of the analytic sample.
Table 1.
Sample Characteristics (N=216)
| Percent (N) | |
|---|---|
| Baseline Age | |
| 18 – 24 | 40.3 (87) |
| 25 – 34 | 36.6 (79) |
| 35 – 45 | 23.2 (50) |
| Gender | |
| Female | 73.2 (158) |
| Male | 26.9 (58) |
| Race | |
| White | 71.8 (155) |
| Non-White | 28.2 (61) |
| Marital Status | |
| Single | 58.3 (126) |
| Married/Living Together | 21.8 (47) |
| Separated/Divorced/Widowed | 19.9 (43) |
| Education | |
| High School or less | 34.3 (74) |
| Some College | 38.9 (84) |
| BA or more | 26.8 (58) |
| Employment Status | |
| Working Full or Part Time | 29.6 (64) |
| Student | 15.7 (34) |
| Not Employed or Student | 54.7 (118) |
| Number of Axis I Disorders at Baseline | |
| 0 | 7.4 (16) |
| 1-2 | 39.8 (86) |
| 3 or more | 52.8 (114) |
| Number of Additional Axis II Disorders at Baseline* | |
| 0 | 14.8 (32) |
| 1-2 | 46.3 (99) |
| 3 or more | 38.9 (84) |
Note: n does not add up to total N because one observation was missing on this variable.
Assessment
Participants were interviewed at baseline and at follow-up assessments (6 months, 12 months, then yearly) by experienced interviewers with the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) (11), a semistructured interview for assessment of DSM-IV Axis II disorders. The DIPD-IV probes for evidence of personality disorder criteria over the prior two years, and then determines if those present have been characteristic of the individual since late adolescence or early adulthood. Interviewers were trained using live or videotaped interviews under the supervision of the author of the DIPD-IV (M.C.Z.). Interrater and test-retest kappas for BPD in the current study were .68 and .69 respectively; median reliability correlations for total criteria scores were .90 and .84 (12). To assess the longitudinal course of the study personality disorders, the DIPD-IV was modified to record the presence of each criterion for each month of the follow-up interval. Interviewers asked the standard probes for presence of each criterion; if it was present at all, the participant was then queried about any change over the interval to determine whether or when the criterion was absent. Ratings were then made for each month of the follow-up interval. For the current report, the BPD criterion ratings for the month preceding each follow-up interview were used. BPD variables examined include the total number of BPD criteria, and factor scores (disturbed relatedness, behavioral dysregulation, and affective dysregulation) derived from confirmatory factor analysis of the CLPS data (13). The disturbed relationship factor consists of criteria for unstable relationships, identity disturbance, and chronic feelings of emptiness; behavioral dysregulation consists of impulsivity and suicidal or self-mutilative behavior; affective dysregulation includes affective instability, inappropriate anger, and frantic efforts to avoid abandonment.
Interviewers assessed psychosocial functioning using the psychosocial section of the Longitudinal Interval Follow-up Evaluation (LIFE) (14). This measure assesses functioning in multiple areas including work, interpersonal relationships, and recreation. Functioning is rated on 5- point scales of severity ranging from 1 (no impairment, high level of functioning) to 5 (severe impairment, very poor functioning). The LIFE also includes ratings on the Global Assessment of Functioning Scale (GAF), a 100-point scale with 100 indicating the highest level of functioning. The Range of Impaired Functioning Tool (LIFE-RIFT) is a brief scale of functional impairment derived from the psychosocial ratings of the LIFE, and consists of items targeting functioning in four domains: work, interpersonal relations, recreation, and global satisfaction (15). The LIFE-RIFT score is a sum of the four items, with possible scores ranging from 4 (no impairment in all areas) to 20 (severe impairment in all areas).
As described below, a number of covariates were included. Number of Axis I disorders at baseline was assessed using the Structured Interview for DSM-IV Disorder (SCID-IV). The psychopathology section of the LIFE includes weekly Psychiatric Status Ratings (PSRs) to quantify course of Axis I Disorders. PSRs for Major Depressive Disorder (MDD), a six point scale indicating status of depressive symptoms from no symptoms to severe, were used to assess depression. The LIFE also assesses mental health treatment use, with detailed ratings of pharmacological and psychosocial treatments. Medication and dosages of medications, frequency of all mental health contacts, including number of sessions, length of treatment, and number of days of inpatient and partial hospitalization are recorded. A global measure of treatment intensity was derived for use as a summary variable for treatment. Weights for levels of care (inpatient, day hospital, or outpatient) were multiplied by the amount of treatment received at each level.
Data Analyses
We conducted a series of growth models to examine the extent to which change in BPD severity and functioning over the course of the study period differed according to age. Age was examined as a continuous variable. Dependent variables included the total number of BPD criteria, the three BPD factor scores, the GAF, and the RIFT. We used SAS PROC GLIMMIX to estimate all models. This procedure accommodates non-normal distributions for the dependent variable and also allows for specification of random effects. In all models, we used random effects to control for the repeated measures and the clustering of subjects within the four study sites. In addition to our predictors of interest, study year and age, we also controlled for several covariates including gender, minority status, education, number of Axis I disorders at baseline, number of Axis II disorders other than BPD, and baseline scores on the dependent variable. Depression and intensity of treatment were included as time-varying covariates in all of the models. These included the MDD PSR rating, and the treatment intensity rating, for the week prior to each assessment.
We ran an initial set of models specifying only main effects for study year and age. A second series of models added the interaction between study year and age. Graphs are used for illustration purposes, showing outcome by three categories defined by age at study baseline: 18 - 24, 25 - 34, and 35 - 45. The choice of these age groups was somewhat arbitrary, but intended to roughly approximate developmental groupings from early adulthood into middle adulthood. As noted, all analyses used age as a continuous variable; the categories were not used in data analyses.
Results
Results of the first set of models examining age and study year showed significant effects for study year for all variables examined except for the GAF, and age effects for the RIFT (older age associated with more impairment). Table 2 shows findings from the second series of models, adding the interaction between age and study year. There is one significant interaction, on the RIFT (DF=1, 998) F = 4.81, p = .029.
Table 2.
Model Estimates (SE) for age, study year, and their interaction as predictors of BPD severity and functioning over 6 years.
| Outcome | Age | Study Year | Age* Study Year |
|---|---|---|---|
| Severity | |||
| Number of BPD criteria | .007 (.018) | -.348 (.104)*** | |
| Disturbed relationships | .006 (.018) | -.224 (.160) | .000 (.005) |
| Behavioral dysregulation | -.009 (.019) | -.119 (.167) | .000 (.005) |
| Affective dysregulation | .005 (.018) | -.157 (.154) | -.002 (.005) |
| Functioning | |||
| GAF | -.076 (.088) | .233 (.557) | -.015 (.017) |
| RIFT | .010 (.023) | -.424 (.157)** | .010 (.005)* |
Notes: indicates significant at p<.05,
indicates significant at p<.01,
indicates significant at <.001.
All models included random effects to control for repeated measures and clustering of subjects within study site, fixed effects for gender, minority status, education, number of axis I disorders at baseline, number of Axis II disorders other than BPD, and baseline scores on the dependent variable, and time-varying effects of depression and treatment intensity.
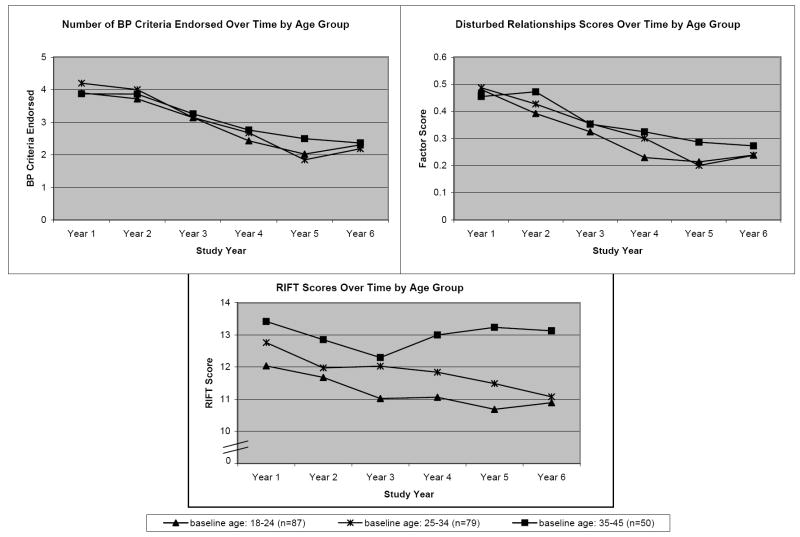
The figure shows the mean scores for the three groups defined by baseline age on number of BPD criteria, the disturbed relationship factor, and the RIFT. For the two BPD criteria variables, the graphs illustrate the similar pattern of improvement across study years for all age groups. On the RIFT, there is a similar pattern of decline (improvement) among the three age groups over years 1–3, but during years 4-6 the younger cohorts remain stable or continue to improve while impairment reverses direction and begins to increase for the oldest cohort (baseline age 35-45).
Discussion
The central question of this study is whether the amount of improvement in BPD symptoms and functioning varies by age. Contrary to our hypothesis that increasing age would be associated with greater improvement, our findings show little influence of age on improvement. Younger subjects show as much improvement as older subjects. In terms of BPD symptoms, we find no interactions between age and study year on any of the factors or the total number of criteria. The only significant interaction between age and study year is on a measure of psychosocial functioning (the RIFT). Older subjects change direction from improvement to worsening in functioning (Figure 1) midway through the 6 years of follow-up, in contrast to the younger aged cohorts. This pattern is compatible with findings from McGlashan (2) and Stone (4,5) that while those in their 30s to early 40s were functioning the best, some in their mid-40s to 50s showed poorer functioning, suggesting a reappearance of difficulties with advancing age.
Figure 1.
An important consideration for the current findings is the possible influence of age-related bias in our sample. Given that subjects had to meet criteria for BPD at baseline, it may be that older subjects in our study group-- those in their late 30s to mid 40s at baseline had more severe psychopathology. If such individuals had been recruited in their 20s, perhaps there would have been more persistence in impulsive behaviors and other impairment throughout their 20s, in contrast to the improvement we find for subjects entering the study in their late teens or early 20s, who may be a more heterogeneous group. While other recent studies have similarly shown significant declines in personality disorder features among college age (16) and adolescent / early adulthood participants (17), suggesting that our younger participants are not atypical, the participants entering the study with active borderline psychopathology in their late 30s to 40s could be a more severe or restrictive subgroup of BPD. Despite their overall improvement over the follow-up, it is notable that at least on one measure (the RIFT), the older participants reverse direction and show an increase in psychosocial impairment mid way through the 6 years of follow-up. It will be important to investigate with longer follow-up whether the younger cohorts similarly show worsening when reaching the same age range.
An additional consideration is that our study excluded individuals older than 45, limiting the older end of the age range. Further follow-up is needed to examine whether individuals in their late 40s and 50s show the predicted pattern of improvement. The findings are also limited by the length of follow-up examined: 6 years may be too brief to show the hypothesized age patterns.
The findings of improvement across the age range raise the compelling question: what factors may explain the decreases in psychopathology, in younger as well as older subjects, now observed in multiple studies of BPD? One explanation may be the use of the DSM criteria as outcome, some of which are symptomatic behaviors (e.g., self-injury or other destructive behaviors) as opposed to traits (10, 18). In studies of clinical samples, an important factor may be treatment. It is difficult to determine treatment effects in naturalistic studies, but the fact that most subjects received treatment of some form is notable. Another factor in clinical samples may be that, despite emphasis on enduring behaviors in personality disorder interviews, subjects are in more distress at the time of study recruitment, and over-report their “usual” maladaptive behaviors and feelings. Subsequent assessments may capture their more typical level of functioning, which could be less disordered than initially reported. Similar improvements, however, have been found in non-clinical samples (16, 17). It is possible that the simple repetition of assessments draws ever more conservative responses for various reasons, including having already been accepted into the study (in which case the follow-up would be a more accurate assessment), or wishing to avoid detailed questioning that affirmative responses trigger (in which case the follow-up would be an underestimate). In the current study, outcome is examined at six repeated evaluations, controlling for the baseline score, thus minimizing the impact of change from baseline to the first follow-up.
A more definitive examination of age related differences in course in BPD would include comparisons of multiple age cohorts of larger sizes over a longer interval than the 6 years of the current study. Nonetheless, our findings suggest the need to revisit the idea of increasing age as the explanation for improvement in BPD psychopathology.
Acknowledgments
Funded by National Institute of Mental Health grants MH-50837, MH-50839, MH-50840, MH-50838, MH-50850, MH-01654, and MH-73708
Principal Investigators are Drs. Gunderson, McGlashan, Morey, Shea, and Skodol. This article has been reviewed and approved by the Publications Committee of the Collaborative Longitudinal Personality Disorders Study.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association; 1994. pp. 652–653. [Google Scholar]
- 2.McGlashan TH. The Chestnut Lodge follow-up study III. Long-term outcome of borderline personalities. Arch Gen Psychiatry. 1986;43:20–30. doi: 10.1001/archpsyc.1986.01800010022003. [DOI] [PubMed] [Google Scholar]
- 3.Paris J, Brown R, Nowlis D. Long-term follow-up of borderline patients in a general hospital. Compr Psychiatry. 1987;28:530–535. doi: 10.1016/0010-440x(87)90019-8. [DOI] [PubMed] [Google Scholar]
- 4.Stone MH. The fate of borderline patients: successful outcome and psychiatric practice. Guilford Press; New York: 1990. [Google Scholar]
- 5.Stone MH. Natural history and long-term outcome. In: Livesley WJ, editor. Handbook of personality disorders, theory, research, and treatment. Guilford Press; NY: 2001. pp. 259–273. [Google Scholar]
- 6.Stevenson J, Meares MD, Comerford A. Diminished impulsivity in older patients with borderline personality disorder. American Journal of Psychiatry. 2003;160:165–166. doi: 10.1176/appi.ajp.160.1.165. [DOI] [PubMed] [Google Scholar]
- 7.Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Prediction of the 10-year course of borderline personality disorder. Am J Psychiatry. 2006;163:827–832. doi: 10.1176/ajp.2006.163.5.827. [DOI] [PubMed] [Google Scholar]
- 8.Gunderson JG, Shea MT, Skodol AE, et al. The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. J Personal Disord. 2000;14:300–315. doi: 10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- 9.Grilo CM, Shea MT, Sanislow CA, et al. Two-year stability and change in schizotypal, borderline, avoidant and obsessive-compulsive personality disorders. J Consult Clin Psychol. 2004;72:767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shea MT, Stout R, Gunderson JG, et al. Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Am J Psychiatry. 2002;159:2036–2041. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- 11.Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- 12.Zanarini MC, Skodol AE, Bender D, et al. The Collaborative Longitudinal Personality Disorders Study: reliability of Axis I and II diagnoses. J Personal Disord. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- 13.Sanislow CA, Grilo CM, Morey LC, et al. Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: findings from the Collaborative Longitudinal Personality Disorders Study. Am J Psychiatry. 2002;159:284–290. doi: 10.1176/appi.ajp.159.2.284. [DOI] [PubMed] [Google Scholar]
- 14.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 15.Leon AC, Solomon DA, Mueller TI, Turvey CL, Endicott J, Keller MB. The Range of Impaired Functioning Tool (LIFE-RIFT): a brief measure of functional impairment. Psychol Med. 1999;29:869–878. doi: 10.1017/s0033291799008570. [DOI] [PubMed] [Google Scholar]
- 16.Lenzenweger M. Stability and change in personality disorder features: The longitudinal study of personality disorders. Arch Gen Psychiatry. 1999;56:1009–1015. doi: 10.1001/archpsyc.56.11.1009. [DOI] [PubMed] [Google Scholar]
- 17.Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: a community-based longitudinal investigation. Acta Psychiatr Scand. 2000;102:265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- 18.McGlashan TH, Grilo CM, Sanislow CA, et al. Two-year prevalence and stability of individual criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. Am J Psychiatry. 2005;162:883–889. doi: 10.1176/appi.ajp.162.5.883. [DOI] [PMC free article] [PubMed] [Google Scholar]