Abstract
Background
The Overall Anxiety Severity and Impairment Scale (OASIS) is a 5-item self-report measure that can be used to assess severity and impairment associated with any anxiety disorder or multiple anxiety disorders. A prior investigation with a nonclinical sample supported the reliability and validity of the OASIS; however, to date it has not been validated for use in clinical samples.
Methods
The present study assessed the psychometric properties of the OASIS in a large sample (N = 1,036) of primary care patients whose physicians referred them to an anxiety disorders treatment study. Latent structure, internal consistency, convergent/discriminant validity, and cut-score analyses were conducted.
Results
Exploratory and confirmatory factor analyses supported a unidimensional structure. The five OASIS items displayed strong loadings on the single factor and had a high degree of internal consistency. OASIS scores demonstrated robust correlations with global and disorder-specific measures of anxiety, and weak correlations with measures of unrelated constructs. A cut-score of 8 correctly classified 87% of this sample as having an anxiety diagnosis or not.
Limitations
Convergent validity measures consisted solely of other self-report measures of anxiety. Future studies should evaluate the convergence of OASIS scores with clinician-rated and behavioral measures of anxiety severity.
Conclusions
Overall, this investigation suggests that the OASIS is a valid instrument for measurement of anxiety severity and impairment in clinical samples. Its brevity and applicability to a wide range of anxiety disorders enhance its utility as a screening and assessment tool.
Keywords: anxiety, self-report, assessment, validity, factor analysis
Introduction
Anxiety disorders are common and disabling problems that are associated with high rates of medical and psychiatric comorbidity (Mendlowicz & Stein, 2000; Stein et al. 2005; Sareen et al. 2006; Kroenke et al. 2007). Individuals who meet criteria for an anxiety disorder demonstrate elevated rates of other anxiety disorders (Carter et al. 2001; Kessler et al. 2006; Ruscio et al. 2008) and in clinical settings the majority of individuals seeking anxiety treatment may have multiple anxiety disorders (Brown et al. 2001). Anxiety comorbidity is clinically significant in that the presence of multiple anxiety disorders is associated with greater distress and impairment than the presence of a single disorder (Mennin et al. 2000; Kroenke et al. 2007). Therefore, in order to provide optimal assessment and treatment for individuals with anxiety disorders, clinicians often must monitor multiple anxiety-related problems.
Self-report measures can be valuable components of a comprehensive assessment of anxiety, and numerous well-validated measures of anxiety disorders exist (Antony et al. 2001). Many of these measures are designed to assess specific diagnostic categories such as panic disorder (e.g., Panic Disorder Severity Scale – Self Report Version; Houck et al. 2002) or generalized anxiety disorder (GAD-7; Spitzer et al. 2006). These disorder-specific scales are ideal for detailed assessment and outcome measurement of the disorder in question; however, they may be less useful in clinical situations that demand a broader initial assessment of anxiety or for regular assessment of patients with multiple anxiety-related problems. For example, in busy clinical settings such as primary care (where many patients with anxiety disorders are assessed and treated; Stein et al. 2005), use of several disorder-specific measures to screen for anxiety disorders would be impractical. Similarly, time constraints would limit use of multiple self-report inventories to monitor treatment response in patients with more than one anxiety disorder. For primary care and other settings that require broad and efficient assessment, a brief instrument that could be used for screening and outcome measurement of any anxiety disorder (and multiple anxiety disorders) would be optimal.
Several well-known scales assess anxiety more broadly and therefore should be able to capture symptoms related to any anxiety disorder or multiple anxiety disorders (e.g., State-Trait Anxiety Inventory; Spielberger, 1983; Beck Anxiety Inventory; Beck & Steer, 1993). These scales generally present lists of somatic and cognitive-affective symptoms that are associated with anxiety. While these measures do provide a broad assessment of anxiety severity, they are somewhat limited as clinical assessment tools in that they do not inquire about the behavioral and functional consequences of anxiety. Phobic avoidance and functional impairment associated with anxiety are often as clinically important as frequency and intensity of somatic and cognitive-affective symptoms (Telch et al. 1995).
The Overall Anxiety Severity and Impairment Scale (OASIS; Norman et al. 2006) was developed in an effort to fulfill the need for a self-report measure of anxiety that (1) assesses multiple domains of clinical severity including functional impairment; (2) effectively captures severity of any anxiety disorder as well as multiple anxiety disorders; and (3) is brief enough to be used in busy clinical settings such as primary care. The OASIS is a 5-item measure that assesses frequency of anxiety, intensity of anxiety symptoms, behavioral avoidance, and functional impairment associated with anxiety. The instructions for the OASIS ask the patient to consider a variety of experiences such as panic attacks, worries, and flashbacks and to consider all of their anxiety symptoms when answering the questions. The OASIS is therefore potentially applicable to any anxiety disorder and should be able to simultaneously assess severity and impairment associated with multiple anxiety disorders. Moreover, at five items it is one of the shortest anxiety scales available, which enhances its utility for many clinical settings (e.g., primary care) and research purposes (e.g., population-based surveys in which respondent burden is a concern).
The psychometric properties of the OASIS have been evaluated in one study to date. In a college student sample, the OASIS demonstrated excellent test-retest reliability and convergent and discriminant validity (Norman et al. 2006). The OASIS was found to be unidimensional in an exploratory factor analysis, and the five items had high degree of internal consistency. Although these results were promising, it is unknown whether they generalize to clinical populations or populations with a wider range of age and education.
The goal of the present study was to evaluate the psychometric properties of the OASIS in a demographically diverse clinical sample. We analyzed OASIS responses from a large sample of primary care patients referred to an anxiety disorders treatment study. The latent structure, internal consistency, and convergent/discriminant validity of the OASIS were evaluated. Other analyses sought to determine whether the OASIS was useful in characterizing severity across a diverse range of anxiety disorders and for patients with multiple disorders. Finally, cut-score analyses were conducted to determine appropriate parameters for using the OASIS as a screening tool.
Method
Participants
Participants were 1,036 patients from primary care clinics located in Little Rock AK, Lancaster CA, Palm Springs CA, San Diego CA, and Seattle WA. All participants were referred to the Coordinated Anxiety Learning and Management (CALM) study by their primary care providers, who felt that they would benefit from treatment of anxiety. The CALM study tests the effectiveness of a collaborative care intervention targeting panic disorder with or without agoraphobia (PD/A), social anxiety disorder (SAD), posttraumatic stress disorder (PTSD), and generalized anxiety disorder (GAD). Characteristics of the participating clinics and other aspects of the design of the CALM study are presented elsewhere (Sullivan et al. 2007).
Proportions of the total sample who met criteria for each anxiety disorder were as follows: GAD (63.1%), PD/A (46.4%), SAD (34.7%), PTSD (15.9%), agoraphobia without a history of panic disorder (9.7%), and obsessive-compulsive disorder (8.3%). A minority of the sample (10.7%) did not meet criteria for any anxiety disorder. Almost two-thirds of the participants reported current unipolar mood disorders, with 60.6% meeting criteria for major depressive disorder (MDD) and 4.3% meeting criteria for dysthymic disorder (DD). Some participants also endorsed alcohol (10.6%) and/or substance use (3.9%) disorders.
Demographic information was available for those patients who were eligible for the CALM treatment study and subsequently completed a baseline assessment (n = 653;63%). The majority of these participants were female (71.2%) and the mean age was 42.8 (SD = 13.5; range = 18 to 75). Most participants identified their racial background as Caucasian/White (61.9%), Mixed (12.2%), Black/African American (10.0%), or Other (6.4%) with smaller proportions of patients identifying as Asian (1.2%), American Indian/Alaskan Native (1.0%), and Hawaiian Native/Other Pacific Islander (0.3%). Another 7.1% of participants did not endorse a racial category. In terms of ethnicity, 16.8% of the sample identified as Hispanic.
Measures
Overall Anxiety Severity and Impairment Scale (OASIS)
All participants completed the OASIS, which consists of five items that measure the frequency and severity of anxiety, as well as level of avoidance, work/school/home interference, and social interference associated with anxiety. The instructions orient the respondent to consider a wide range of anxiety symptoms (e.g., panic attacks, worries, flashbacks) when answering the questions, and the time frame is “over the past week.” Respondents select among five different response options for each item, which are coded 0–4 and summed to obtain a total score. A psychometric analysis of the OASIS in an undergraduate sample suggested that the scale was unidimensional and had good internal consistency, test-retest reliability, and convergent/discriminant validity (Norman et al., 2006).
Convergent and Discriminant Validity Measures
Participants who were eligible for and enrolled in the larger CALM study (n = 653) completed well-validated measures of anxiety (Brief Symptom Inventory 18 Anxiety Subscale; BSI-18-A; Derogatis, 2000), depression (Patient Health Questionnaire 9; PHQ-9; Kroenke et al. 2001), alcohol use (3 items from the Alcohol Use Disorders Identification Test; AUDIT; Bohn et al. 1995), general health and functioning (Short-Form Health Survey; SF-12; Ware et al. 1996), disability (Sheehan Disability Scale; SDS; Sheehan et al. 1996), quality of life (EuroQol; EQ-5D; Rabin & de Charro, 2001), and social support (adapted from the Medical Outcomes Study Social Support Survey; MOS-SSS; Sherbourne & Stewart, 1991) during their baseline assessment. These participants also completed additional measures depending on the diagnoses they endorsed during their eligibility interview. Participants with PD/A completed the self-report version of the Panic Disorder Severity Scale (PDSS; Houck et al. 2002), patients with SAD completed the Social Phobia Inventory (SPIN; Connor et al. 2000), patients with PTSD completed the PTSD Checklist –Civilian Version (PCL-C; Weathers et al., 1994), and patients with GAD completed the Generalized Anxiety Disorder Severity Scale (GADSS; Shear et al. 2006).
Procedure
The IRBs at all participating sites (University of Arkansas for Medical Sciences, University of California Los Angeles, University of California San Diego, University of Washington, and RAND Corporation) approved the study procedures.
Participants completed the OASIS as part of their eligibility assessment for the CALM study. The eligibility assessment was conducted by an “anxiety clinical specialist” (ACS), who was a health care or mental health professional (e.g., nurse, social worker) who was trained in assessment and treatment of anxiety for the purposes of the CALM study (see Sullivan et al., 2007). The ACS obtained written informed consent for participation in the study and administered the Mini International Neuropsychiatric Interview (MINI; Sheehan et al. 1998) to establish psychiatric diagnoses. At the end of the MINI, the patient was asked to identify which diagnosis, out of all diagnoses they endorsed on the MINI, was most distressing to them. If they did not choose one of the four anxiety disorders treated in the CALM study, they were asked a follow-up question regarding which of these four anxiety disorders was the most distressing to them. The MINI was followed by administration of the OASIS, PHQ-9, the full AUDIT, and two items that inquired about expectancies for treatment (not reported here). After the eligibility assessment, the ACS reviewed any diagnostic questions with a clinical supervisor and a decision was made regarding eligibility for the CALM study.
Participants who were eligible for the CALM study were contacted for a baseline assessment, which was conducted by telephone by an interviewer from the RAND Survey Research Group. The mean number of days between the eligibility interview and baseline assessment was 10.42 days (SD = 9.41).1 The baseline assessment lasted about one hour and included demographic questions, symptom measures, and questions about treatment and medical utilization (Sullivan et al., 2007). All of the convergent and discriminant validity measures used in this study came from the baseline assessment except for the AUDIT, which was administered at the eligibility assessment.
Statistical Analysis
We used the total sample (N = 1,036) for factor analysis, calculation of internal consistency, and analyses to determine clinical cut-scores. Cases were randomly assigned to one of three subsamples for factor analysis. Subsample 1 (n = 344) and subsample 2 (n = 345) were used for exploratory factor analysis (EFA) and subsample 3 (n = 346) was used for confirmatory factor analysis (CFA). The sample variance-covariance matrices were analyzed using a latent variable software program (Mplus 2.12, Muthén & Muthén, 1998). Maximum likelihood estimation and promax rotation were used. Goodness of fit was evaluated using the chi-square test (χ2), root-mean-square error of approximation (RMSEA) and its 90% confidence interval, p value for test of closeness of fit (Cfit; estimates the probability that RMSEA < .05), standardized root-mean-square residual (SRMR), and comparative fit index (CFI). Final acceptance or rejection of models was based on conventional criteria for good model fit (RMSEA < .08, Cfit, 90% CI < .08; SRMR < .05; CFI > .90; Jaccard & Wan, 1996), strength of parameter estimates (i.e., primary factor loadings > .35, absence of salient cross-loadings), and the conceptual interpretability of the solution.
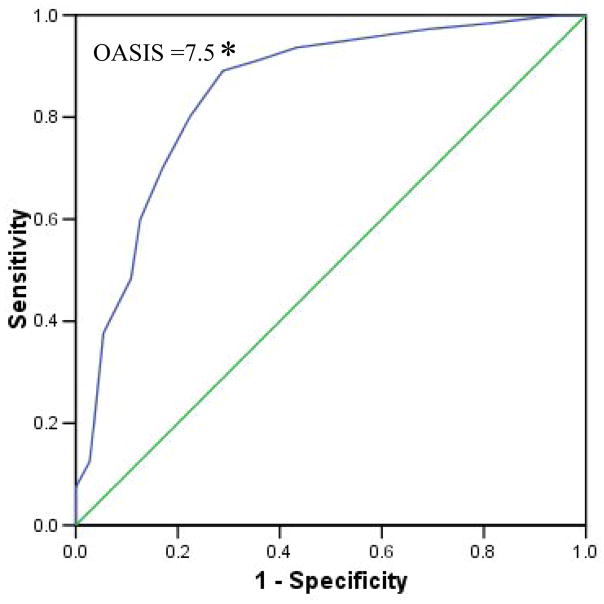
Receiver operating characteristics (ROC) curves were used to determine sensitivity and specificity for each cut-score on the OASIS. Presence versus absence of an anxiety disorder diagnosis on the MINI was used as the categorical outcome. A ROC curve is a plot of the true positive rate (sensitivity) against the false positive rate (1- specificity) for the different possible cut points and thus provides a visual representation of the tradeoff between sensitivity and specificity of cut-scores for a diagnostic test. Chi-square tests, sensitivity values, and specificity values were used to calculate percentage of patients correctly classified as meeting criteria for an anxiety disorder based on the three most promising cut-scores from the ROC analyses. The sensitivity, specificity, and percent correctly classified values were used to select an appropriate cut-score for identifying patients with probable anxiety disorders using the OASIS.
We used the subsample of patients who were eligible and enrolled in the CALM treatment study (n = 653) for convergent and discriminant validity analyses.2 Smaller groups of patients who completed measures of GAD (n = 470), PD/A (n = 320), SAD (n = 276), and PTSD (n = 125) were used for convergent validity analyses that entailed correlating the OASIS with disorder-specific measures. Strong positive correlations of the OASIS with global (BSI-18-A) and disorder-specific (PDSS, SPIN, PCL-C, and GADSS) anxiety scales were interpreted as evidence for convergent validity. We also expected the OASIS to correlate with measures of depression (PHQ-9), mental health (SF-12-M), disability (SDS) and quality of life (EQ-5D). To assess discriminant validity, we computed correlations between the OASIS and measures of alcohol use (AUDIT), social support (MOS-SSS), and physical health (SF-12-P). Correlations below .30 were considered supportive of discriminant validity.
Results
The mean OASIS score for this sample was 10.77 (SD = 4.02). Patients who endorsed an anxiety disorder on the MINI scored higher on the OASIS (n = 925, M = 11.37, SD = 3.61) than patients who received no anxiety diagnoses on the MINI (n = 111, M = 5.82, SD = 3.81), t (1,034) = 15.20, p < .001. OASIS scores were positively correlated with number of anxiety disorder diagnoses, r = .51, p < .001. OASIS scores did not vary significantly depending on which anxiety disorder (PD/A, SAD, PTSD, or GAD) was identified by the patient as most distressing, F (3) = 2.26, ns. There were no significant relationships between OASIS scores and sex, age, race, ethnicity, or income.
Contributions of Specific Diagnoses to Predicting OASIS Scores
To investigate the effects of specific disorders on OASIS scores, a hierarchical regression was conducted. The presence/absence of anxiety disorders that frequently appeared in this sample (PD/A, SAD, PTSD, GAD) was entered on the first step, and the presence/absence of unipolar mood disorders (MDD, DD) was entered on the second step. The model that included both anxiety and unipolar mood disorders was statistically significant, F (6, 1029) = 102.06, p < .001, R = .61, R2 = .37, and explained more variance in OASIS scores than the model that only included anxiety disorders, hierarchical F (2, 1029) = 88.14, p < .001, ΔR2 = .11. Presence of each anxiety disorder was independently associated with higher OASIS scores, and presence of each unipolar mood disorder was independently associated with higher OASIS scores (see Table 1). Inspection of unstandardized regression coefficients suggested that the anxiety disorders were associated with 1.1-point (PTSD) to 1.9-point (GAD) increases in OASIS score. Presence of MDD was associated with a 3-point increase and presence of DD was associated with a 1.4-point increase in OASIS score.
Table 1.
Hierarchical Regression Analysis of Diagnostic Predictors of OASIS Score
| Diagnosis | B | SE B | β |
|---|---|---|---|
| Step 1 | |||
| PD/A | 1.69 | 0.20 | .21*** |
| SAD | 1.65 | 0.21 | .20*** |
| PTSD | 1.11 | 0.28 | .10*** |
| GAD | 1.79 | 0.21 | .22*** |
| Step 2 | |||
| MDD | 2.98 | 0.23 | .36*** |
| DD | 1.39 | 0.51 | .07** |
Note. R2 = .27 for Step 1; ΔR2 = .11 for Step 2 (ps <.001). PD/A = panic disorder with or without agoraphobia. SAD = social anxiety disorder. PTSD = posttraumatic stress disorder. GAD = generalized anxiety disorder. MDD = major depressive disorder. DD = dysthymic disorder.
p < .01,
p < .001.
Factor Analysis
The five OASIS items were submitted to EFA in two independent subsamples. Given the small number of items that comprise the OASIS, only one- and two-factor models were evaluated. The two-factor model was rejected because it produced invalid parameter estimates in one of the samples. Therefore, data are reported for the single-factor solution only.
Subsample 1 (n = 344) was used for the first EFA. Eigenvalues > 1 for the unreduced correlation matrix were 3.19 (next highest eigenvalue = 0.66). All five items displayed salient loadings on the latent factor (range = .65 to .78). Although eigenvalues and factor loadings suggested a one-factor solution, the single-factor model did not meet other criteria for good model fit, χ2 (5) = 39.12, p < .001; RMSEA = .14, 90% CI = .10–.18, CFit = .00. For subsample 2 (n = 345), eigenvalues > 1 for the unreduced correlation matrix were 3.05 (next highest eigenvalue = 0.68). All five items displayed salient loadings on the latent factor (range = .60 to .77). However, once again the single-factor model did not meet other criteria for good model fit, χ2 (5) = 31.22, p < .001; RMSEA = .12, 90% CI = .08–.17, CFit = .00.
Given the mixed EFA results (i.e., eigenvalues and factor loadings implied a single latent factor, but χ2 and RMSEA suggested poor fit of the single-factor model) we considered the possibility of other sources of covariance between items (e.g., correlated error variance). We hypothesized that items 1 and 2 had correlated error variance because a zero response to item 1 regarding frequency (“no anxiety in the past week”) would necessitate a zero response to item 2 regarding intensity (“anxiety was absent or barely noticeable”). We planned to freely estimate covariance of the error terms associated with items 1 and 2 in the CFA model.
Subsample 3 (n = 346) was used for CFA. First we tested a one-factor model with no error theory. As expected based on EFA, the single-factor model did not fit the data well, χ2 (5) = 100.33, p < .001; RMSEA = .24, 90% CI = .20–.28, CFit = .00; SRMR = .08; CFI = .86. Modification indices suggested a clear point of strain in the model pertaining to unexplained covariance between items 1 and 2 (M.I. = 96.65; standardized expected parameter change = .37).
Our final CFA model specified that all five items loaded on a single latent factor, and also freed the path between the error terms of items 1 and 2. This model fit the data well, χ2 (4) = 7.46, ns; RMSEA = .05, 90% CI = .00–.11, CFit = .42; SRMR = .02; CFI = .99. Each item displayed salient loadings on the latent factor (.51 to .78) and the correlation between the error terms of items 1 and 2 was significant (r = .35, z = 7.63, p < .001). Standardized residuals and modification indices did not suggest any points of strain in the model. Factor determinacies are validity coefficients indicating the correlation between factor score estimates and their respective factors (Grice, 2001). The determinacy of the single factor was favorable at .92 (Gorsuch, 1983).
These results were replicated after combining Samples 1–3 (n = 1,036) to obtain the most accurate parameter estimates (see Table 2). Results in the total sample were consistent with those obtained using the Sample 3 data, χ2 (4) = 29.52, p < .001; RMSEA = .079, 90% CI = .053–.106, CFit = 0.032; SRMR = .022; CFI = .99; Determinacy = .93. Again, the error terms of items 1 and 2 were significantly correlated, r = .22, z = 9.11, p < .001. Cronbach’s alpha for the five items of the OASIS was .84.
Table 2.
Confirmatory Factor Analysis of the OASIS: Completely Standardized Solution
| Item | Description | Factor Loading |
|---|---|---|
| 1 | Frequency of anxiety | .55 |
| 2 | Intensity of anxiety symptoms | .67 |
| 3 | Degree of avoidance due to anxiety | .75 |
| 4 | Work/school/home interference | .78 |
| 5 | Social life/relationship interference | .78 |
| Determinacy | .92 | |
| Reliability | .84 | |
| M | 10.77 | |
| SD | 4.02 |
Note. All estimates in this table are based on analyses with the total sample (n = 1,036). The final solution specified correlated error variance between items 1 and 2.
Sensitivity, Specificity, and Correct Classification
We assessed whether a particular cut-score on the OASIS was best able to discriminate those who met criteria for any anxiety disorder from those who did not. To do so, we generated a ROC curve with OASIS as the continuous variable and diagnostic status as the categorical outcome of interest. The three cut-scores with the most promising balance of sensitivity and specificity were selected for follow up analyses to calculate percent of patients correctly classified using these cut-scores. Correct classification was calculated as the sum of true positives plus true negatives divided by the total sample size.
The ROC curve and corresponding sensitivity and specificity values indicated that a cut-score between 7 and 9 would maximize sensitivity relative to specificity (Figure 1). Table 3 shows the chi-square values and percentages of patients correctly classified with cut-scores of 7, 8, and 9. We judged a cut-score of ≥ 8 to be optimal given that it successfully classified 87% of the sample with the most favorable balance of sensitivity (89%) and specificity (71%).
Figure 1.
Receiving Operator Characteristic (ROC) Curve for OASIS score to Predict Anxiety Disorder Diagnostic Status. A cut-score of 8 correctly identified the anxiety disorder status of 87% of the sample (i.e., an OASIS score of 8 or above indicates probable anxiety disorder).
Table 3.
Sensitivity, Specificity, and Efficiency of three possible OASIS Cut-Scores for Identification of Patients with Anxiety Diagnoses
| OASIS Cut-Score | X2 (1, 1036) | Sensitivity | Specificity | % Correctly Classified |
|---|---|---|---|---|
| 7 | 241.28*** | .91 | .64 | 88.32 |
| 8 | 250.63*** | .89 | .71 | 87.16 |
| 9 | 172.67*** | .80 | .88 | 80.02 |
Note. The three candidate cut-scores were chosen based on visual inspection of the ROC curve depicted in Figure 1. OASIS = Overall Anxiety Severity and Impairment Scale.
p < .001.
Convergent and Discriminant Validity
Table 4 shows that the OASIS correlated strongly with the major convergent validity measures of anxiety (BSI-18-A), panic (PDSS), social anxiety (SPIN), posttraumatic stress (PCL-C), and generalized anxiety (GADSS). The OASIS also correlated positively with depression (PHQ-9) and disability (SDS), and negatively with mental health (SF-12-M) and quality of life (EQ-5D). Discriminant validity analyses (see Table 4) showed that the OASIS did not correlate with a measure of alcohol use (AUDIT). Its negative correlations with measures of social support (MOS-SSS) and physical health (SF-12-P), while statistically significant in this large sample, were small in magnitude (rs < .25).
Table 4.
Correlations of OASIS with Convergent and Discriminant Validity Measures
| OASIS | BSI-A | PDSS | SPIN | PCL-C | GADSS | PHQ-9 | SF-12-M | SDS | EQ-5D | SF-12-P | MOS-SSS | AUDIT | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OASIS | --- | .50 | .60 | .40 | .49 | .58 | .50 | −.48 | .59 | −.45 | −.23 | −.22 | .05 |
| BSI-A | --- | .68 | .47 | .62 | .63 | .54 | −.52 | .55 | −.55 | −.19 | −.17 | .13 | |
| PDSS | --- | .41 | .60 | .75 | .53 | −.46 | .64 | −.53 | −.23 | −.13 | .06 | ||
| SPIN | --- | .57 | .50 | .47 | −.32 | .49 | −.38 | −.25 | −.16 | .12 | |||
| PCL-C | --- | .67 | .69 | −.51 | .68 | −.51 | −.22 | −.13 | −.04 | ||||
| GADSS | --- | .67 | −.63 | .74 | −.56 | −.22 | −.17 | .05 | |||||
| PHQ-9 | --- | −.63 | .70 | −.59 | −.32 | −.25 | .06 | ||||||
| SF-12-M | --- | −.67 | .41 | −.12 | .25 | −.07 | |||||||
| SDS | --- | −.54 | −.23 | −.26 | .02 | ||||||||
| EQ-5D | --- | .41 | .18 | −.04 | |||||||||
| SF-12-P | --- | .16 | .12 | ||||||||||
| MOS-SSS | --- | −.04 | |||||||||||
| AUDIT | --- |
Note. Correlations in bold are statistically significant at p < .001. Correlations in italics are statistically significant at p < .05. Correlation coefficients were estimated based on varying sample sizes (ns = 125 to 653) as some measures were only administered to participants who endorsed specific diagnoses. OASIS = Overall Anxiety Severity and Impairment Scale. BSI-A = Brief Symptom Inventory – Anxiety Subscale. PDSS = Panic Disorder Severity Scale (self-report version). SPIN = Social Phobia Inventory. PCL-C = Posttraumatic Stress Disorder Checklist –Civilian Version. GADSS = Generalized Anxiety Disorder Severity Scale. PHQ-9 = Patient Health Questionnaire 9 (depression scale). SF-12-M = Short Form Health Survey – Mental Health Subscale. SDS = Sheehan Disability Scale. EQ-5D = EuroQol (quality of life scale). SF-12-P = Short Form Health Survey – Physical Health Subscale. MOS-SSS = Medical Outcomes Survey – Social Support Scale. AUDIT = Alcohol Use Disorders Identification Test.
Discussion
The current study evaluated the psychometric properties of the OASIS, a self-report measure of anxiety severity and impairment. A previous investigation provided evidence for the reliability and validity of the OASIS in a college student sample (Norman et al. 2006); however, conclusions could not be drawn regarding the utility of the OASIS for assessing anxiety in clinical samples or samples more diverse in age and education level. Our study addressed this limitation by evaluating the OASIS in a diverse sample of primary care patients who were referred to an anxiety treatment study. We conclude that the OASIS has good reliability and validity for clinical samples, as well as applicability to a diverse range of anxiety disorders.
The convergent validity of the OASIS was supported by robust correlations with a well-validated global measure of anxiety (BSI-A) as well as with each of the four disorder-specific measures. The OASIS also showed expected correlations with other constructs that overlap significantly with anxiety. Patients with higher OASIS scores scored lower on mental health and higher on disability. Finally, discriminant validity analyses demonstrated that OASIS scores are not substantially related to scores on measures of other constructs that have minimal overlap with anxiety (e.g., alcohol use).
Overall, our results suggest that the OASIS effectively captures severity and impairment regardless of the specific focus of the anxiety disorder. As noted above, the OASIS displayed salient correlations with measures of generalized anxiety, social anxiety, posttraumatic stress, and panic. In addition, the anxiety disorder identified by the patient as most distressing was not a significant predictor of OASIS scores. In contrast, number of anxiety diagnoses was positively correlated with OASIS score. We view this as supporting the validity of the OASIS, given that prior research has shown that presence of multiple anxiety disorders is associated with greater impairment than presence of a single disorder (Mennin, et al., 2000; Kroenke et al., 2007).
The results regarding the internal consistency and dimensionality of the OASIS were similar to those reported for an undergraduate sample (Norman et al. 2006). We concluded that a single-factor model that accounted for correlated error variance between two items provided the best fit for the data. Therefore, use of a total score (computed by summing the five items) is recommended when the OASIS is used in clinical samples. Statistical analyses to determine an appropriate cut-score for identification of clinically anxious individuals suggested that an OASIS score of 8 or above (which correctly classified 87% of the patients in this sample) would be indicative of a probable anxiety disorder. We did not attempt to statistically determine a cut-score for classifying patients as remitted in the present study, but future investigations that include the OASIS as a treatment outcome measure should address this question.
A common question posed for anxiety scales is how well they can be differentiated from measures of depression. Many well-established anxiety measures correlate significantly with depression scales, and in some cases appear equally sensitive to depression as to anxiety (Moras et al. 1992; Bieling et al. 1998). In this sample (largely comprised of clinically anxious individuals), the OASIS correlated with a measure of depressive symptoms (PHQ-9). The magnitude of this correlation (r = .50) was identical to the correlation between the OASIS and the convergent validity measure of global anxiety symptoms. Hierarchical regression further showed that presence of unipolar mood disorders predicted variance in OASIS scores beyond the variance accounted for by anxiety disorders. In fact, MDD predicted a greater increase in OASIS score than any of the anxiety disorders.
There are several possible explanations for the association between depressive symptoms and more severe profiles on the OASIS. First, having both anxiety and depression may reflect the presence of a more severe diathesis that makes individuals prone to anxiety syndromes of greater severity. Second, presence of more severe anxiety may lead to depression, or conversely presence of depressive symptoms may exacerbate anxiety in some patients. Finally, it is possible that patients do not discriminate well between anxious and depressive symptoms and are considering both when they fill out a questionnaire like the OASIS (i.e., scores are artificially inflated in patients with co-occurring depression).
In practice, the potential influence of depressive symptoms on OASIS scores may cause some patients with mood disorders to score at or above the recommended cut-score of 8, even if they do not meet full criteria for a co-occurring anxiety disorder. As with any self-report scale, the OASIS should not be used in isolation for diagnostic purposes. A “positive” screen on the OASIS should prompt the clinician to inquire about anxiety disorders as well as symptoms of conditions that commonly co-occur with anxiety disorders such as mood disorders. In some cases a mood disorder may be the most appropriate diagnosis for a patient with an elevated OASIS score. This type of clinician-based differential diagnosis, while at times logistically challenging in settings such as primary care, is essential for adequate assessment and treatment planning for patients with anxiety and other psychiatric disorders.
The possible influence of depressive symptoms on OASIS scores may be considered a limitation of the measure, albeit one that applies to many other anxiety assessment tools (see Table 4 for examples). In the current study we were not able to investigate the most appropriate manner to differentiate presence of anxiety disorders from presence of mood disorders on the OASIS for two reasons. First, the number of patients with mood disorders in the absence of anxiety disorders was low (n = 43). Second, this small sample was likely heavily biased toward cases of “anxious depression” given that the patient’s physician perceived enough anxiety symptoms to refer the patient to an anxiety treatment study. Therefore, it would be invalid to estimate OASIS norms for patients with mood disorders using this sample. Future studies using samples that are not predetermined to have an increased risk of anxiety disorders should evaluate the ability of the OASIS to differentiate anxiety disorders from mood disorders and other conditions.
Several limitations of this study must be noted. First, convergent validity measures consisted solely of other self-report inventories. Therefore, some of the relationships observed between the OASIS and other measures of anxiety may have been attributable to method effects. Future studies should attempt to demonstrate meaningful relationships between the OASIS and measures of anxiety severity that do not rely on self-report. Second, demographic information was only available for participants who were enrolled in the larger CALM study. Because this information is unknown for participants who were ineligible or refused, we cannot assume that the subsamples used for the convergent and discriminant validity analyses were representative of the total sample. Third, the format of the OASIS is such that each response option is linked to 1–3 short sentences describing a certain level of symptoms or impairment. The need to read through these response options may sometimes be burdensome to patients or clinicians interpreting the measure. However, an alternative view is that this format promotes more thoughtful responses on the part of the patient and provides more informative details to the clinician.
In summary, the present investigation suggests that the OASIS is a reliable and valid instrument for measurement of anxiety severity and impairment in clinical samples. These results build upon those of a prior study supporting use of the OASIS for assessment of anxiety in non-clinical samples (Norman et al. 2006). To the best of our knowledge, this is the only available measure that captures severity and impairment across anxiety disorders. The combination of its broad applicability and brevity enhance the utility of the OASIS as an assessment tool for primary care, outpatient psychiatric, and other settings that require broad and efficient assessment (e.g., community-based research). In particular, the fact that the OASIS demonstrated a favorable balance of sensitivity and specificity with just five items suggests that the OASIS could be a highly efficient and effective screening tool. In addition to identifying patients with probable anxiety disorders, the OASIS provides valuable information to the clinician regarding severity of symptoms and impairment related to the patient’s anxiety.
Finally, the OASIS also may prove a useful tool for clinical assessment of treatment outcome, especially for patients with multiple anxiety disorders who would otherwise need to complete multiple self-report inventories that might be difficult to integrate and/or prioritize. The recent emergence of behavioral treatments that can be applied to multiple anxiety disorders (Barlow et al. 2004; Sullivan et al. 2007) also suggests a need for assessment tools that capture severity and impairment across a variety of anxiety-related problems. Given its applicability to a wide range of anxiety disorders, the OASIS appears to be a promising measure for evaluating the effects of interventions aimed broadly at anxiety rather than one specific anxiety diagnosis.
Acknowledgments
This work was supported by the following National Institute of Mental Health grants: U01 MH070018 to RAND (Dr. Sherbourne), U01 MH058915 to University of California Los Angeles (Dr. Craske), U01 MH057835 to University of California San Diego (Dr. Stein), U01 MH057858 to University of Washington (Dr. Roy-Byrne), U01MH070022 to University of Arkansas for Medical Sciences (Dr. Sullivan), MH065324 to Dr. Roy-Byrne and MH64122 to Dr. Stein. The authors wish to thank Bernadette Benjamin for her help with data preparation and management.
Footnotes
Five cases were excluded from this calculation because they were extreme outliers.
Participants who were not eligible or who did not enroll in the CALM treatment study did not complete the convergent and discriminant validity measures.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Antony MM, Orsillo SM, Roemer L. Practitioner’s guide to empirically based measures of anxiety. Kluwer Academic/Plenum Publishers; New York, NY: 2001. [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Towards a unified treatment for emotional disorders. Behav Ther. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory manual. Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Bieling PJ, Antony MM, Swinson RP. The State-Trait Anxiety Inventory, Trait version: Structure and content reexamined. Behav Res Ther. 1998;36:777–788. doi: 10.1016/s0005-7967(98)00023-0. [DOI] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): Validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56:423–432. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Carter RM, Wittchen HU, Pfister H, Kessler RC. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depress Anxiety. 2001;13:78–88. doi: 10.1002/da.1020. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR, Churchill LE, Sherwood A, Foa E, Weisler RH. Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. Brit J Psychiatry. 2000;176:379–386. doi: 10.1192/bjp.176.4.379. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, scoring, and procedures manual. NCS Pearson, Inc; Minneapolis, MN: 1993. [Google Scholar]
- Gorsuch RL. Factor analysis. 2. Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- Grice JW. Computing and evaluating factor scores. Psychol Methods. 2001;6:430–450. [PubMed] [Google Scholar]
- Houck PR, Spiegel DA, Shear MK, Rucci P. Reliability of the self-report version of the panic disorder severity scale. Depress Anxiety. 2002;15:183–185. doi: 10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- Jaccard J, Wan CK. LISREL approaches to interaction effects in multiple regression. Sage Publications; Thousand Oaks, CA: 1996. [Google Scholar]
- Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006;63:415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. Am J Psychiatry. 2000;157:669–682. doi: 10.1176/appi.ajp.157.5.669. [DOI] [PubMed] [Google Scholar]
- Moras K, Di Nardo PA, Barlow DH. Distinguishing anxiety and depression: Reexamination of the reconstructed Hamilton scales. Psychol Assess. 1992;4:224–227. [Google Scholar]
- Muthén LK, Muthén BO. Mplus 3.0 [Computer software] Author; Los Angeles: 1998. [Google Scholar]
- Norman SB, Hami-Cissell S, Means-Christensen AJ, Stein MB. Development and Validation of an Overall Anxiety Severity and Impairment Scale (OASIS) Depress Anxiety. 2006;23:245–249. doi: 10.1002/da.20182. [DOI] [PubMed] [Google Scholar]
- Rabin R, de Charro F. EQ-5D: A measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychol Med. 2008;38:15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen J, Jacobi F, Cox BJ, Belik SL, Clara I, Stein MB. Disability and poor quality of life associated with comorbid anxiety disorders and physical conditions. Arch Intern Med. 2006;166:2109–2116. doi: 10.1001/archinte.166.19.2109. [DOI] [PubMed] [Google Scholar]
- Shear K, Belnap BH, Mazumdar S, Houck P, Rollman BL. Generalized Anxiety Disorder Severity Scale (GADSS): A preliminary validation study. Depress Anxiety. 2006;23:77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. Int Clin Psychopharmacol. 1996;11(Suppl 3):89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS Social Support Survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. Manual for the Stait-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- Stein MB, Roy-Byrne PP, Craske MG, Bystritsky A, Sullivan G, Pyne JM, Katon W, Sherbourne CD. Functional impact and health utility of anxiety disorders in primary care outpatients. Med Care. 2005;43:1164–1170. doi: 10.1097/01.mlr.0000185750.18119.fd. [DOI] [PubMed] [Google Scholar]
- Sullivan G, Craske MG, Sherbourne C, Edlund MJ, Rose RD, Golinelli D, Chavira DA, Bystritsky A, Stein MB, Roy-Byrne PP. Design of the Coordinated Anxiety Learning and Management (CALM) study: Innovations in collaborative care for anxiety disorders. Gen Hosp Psychiatry. 2007;29:379–387. doi: 10.1016/j.genhosppsych.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch MJ, Schmidt NB, Jaimez TL, Jacquin KM, Harrington PJ. Impact of cognitive-behavioral treatment on quality of life in panic disorder patients. J Consult Clin Psychol. 1995;63:823–830. doi: 10.1037//0022-006x.63.5.823. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Huska JA, Keane TM. The PTSD Checklist-Civilian Version. National Center for PTSD; Boston, MA: 1994. [Google Scholar]