Abstract
Purpose
To determine the degree of natural acclimatization and artificially-induced acclimation-related changes during repeated exercise/heat bouts in 7 lean and 7 obese 9- to 12-yr-old boys during summer months.
Methods
Beginning at random times during the summer, subjects underwent a 70-min exercise (30% V˙o2max)/heat exposures (38°C, 50% rh) on six separate days.
Results
On day 1, obese children were less naturally acclimatized as indicated by significantly higher baseline core temperatures (Tc) (obese = 37.62 ± 0.06 vs. lean = 37.41 ± 0.06; P < 0.004). By day 6 vs. 1, significant reductions in baseline Tc were evident in both groups (obese = 37.41 ± 0.04 vs. lean = 37.18 ± 0.04; both P < 0.05). Baseline Tc in obese subjects by day 6 was similar to that of lean subjects on day 1. Daily reductions in exercise Tc were evident in both groups (final exercising Tc day 1 vs. 6; obese = 38.15 ± 0.05 vs. 37.89 ± 0.05, lean = 38.17 ± 0.09 vs. 37.72 ± 0.06°C; both P < 0.001), occurring at a significantly slower rate in obese subjects (final exercise Tc day 6 – 1; obese vs. lean = −0.26 ± 0.04 vs. −0.45 ± 0.08°C; P < 0.05). Significant reductions in exercising heart rate (HR) occurred in the lean but not the obese subjects by day 6 (final exercising HR day 1 vs. 6; obese = 132 ± 3 vs. 131 ± 3; P > 0.05, lean = 138 ± 3 vs. 127 ± 3 bpm; P < 0.001).
Conclusions
During summer months, obese children are less naturally heat-acclimatized and subsequently acclimate at a slower rate.
Keywords: Acclimatization, Acclimation, Children, Thermoregulation, Core Temperature, Body Composition
Introduction
Heat-acclimatization (induced in a natural environment) and acclimation (induced over a shorter period of time, often in a laboratory setting) result from repeated heat exposures which sufficiently increase body core temperature (Tc) and mean skin temperature, and stimulate abundant sweating (38). In response, the body adapts through numerous physiological adjustments such as reductions in day-to-day exercise Tc, heart rate (HR) and mean skin temperature, an increase in sweating rate, earlier onset of sweating with more dilute sweat, and an increase in plasma volume (32). In addition, decreases in morning baseline Tc have been observed following humid heat-acclimation (6). The induction of heat-acclimation during exercise is specific to the duration of exposure, environmental conditions, and intensity of exercise and can be attained in adults in 5–10 days through exercise/heat exposures lasting 1–2 hrs each day (32).
While both children and adults are able to acclimate to exercise in the heat, it has been reported that children acclimate at a slower rate (14) and attain a degree of acclimation that is somewhat lower (37) than adults. Only two studies (12,13) have investigated the responses of obese/overweight vs. lean children to exercise in the heat, with both studies demonstrating no difference in heat tolerance (exercise time in the heat before a Tc of 39.4°C was reached). However, although all subjects in both studies underwent 3 exercise/heat-acclimation sessions prior to the heat tolerance trials, these data were not presented or discussed. Thus, neither the relative ability of obese vs. lean children to acclimate to exercise in the heat nor a comparison of their rates of acclimation has been investigated.
In adults, exposure to summer heat confers some degree of natural acclimatization. During both passive heat stress and exercise in the heat, Tc and HR are lower and sweating is more profuse and dilute in summer compared to winter months (38). Due to this natural acclimatization, full artificially-induced heat-acclimation in a warm environment occurs more rapidly (10). A high degree of fitness also hastens the acclimation process (31). Children indigenous to tropical climates display high sweating rates, and a heat tolerance similar to adults during exercise in the heat (28,29). However, for both obese and lean children residing in more temperate climates, the degree of natural acclimatization incurred during the summer months and its impact on subsequent acclimation-related changes when exposed to regular exercise/heat exposures are unknown.
As exercise is frequently prescribed as a main combatant of the pediatric obesity pandemic and as a greater number of children become more physically active, especially outdoors during the warm summer months, ensuring their physical well-being during every exercise session is important. The degree of heat-acclimatization/acclimation during exercise is one factor which could affect a child’s physical performance, subjective comfort and/or physical well-being during exercise in the heat. The smaller body surface area to mass ratio and increased subcutaneous fat deposits of an obese vs. lean individual may contribute to a slower rate of metabolic heat loss (30) and possible differences in the heat-acclimatization/acclimation responses during exercise. Understanding the heat-acclimatization/acclimation similarities/differences during exercise between lean and obese children has implications for scheduling youth sports games and practices, etc. If obese children are less naturally heat-acclimatized and/or display a slower rate of heat-acclimation during exercise, this might suggest that obese children require additional exercise bouts in the heat in order to achieve a degree of acclimation similar to that of lean children.
The purpose of this study was to determine the degree of initial natural acclimatization and subsequent artificially-induced acclimation-related changes during repeated exercise/heat bouts in 7 lean and 7 obese 9- to 12-yr-old boys during the warm summer months. It was hypothesized that obese children would 1) be less naturally acclimatized to the heat as shown by significantly higher baseline Tc, and 2) display a significantly slower time course for the classic markers of acclimation (e.g., day to day decreases in exercise Tc and HR, elevations in sweating rate) during repeated days of light-to-moderate intensity exercise in a warm, humid environment.
Methods
Subjects
This study was approved by the Institutional Review Board of The Pennsylvania State University. Seven lean and 7 obese 9- to 12-yr-old boys volunteered to participate in this study. Lean and obese were defined as ≤ 20% and ≥ 25% body fat, respectively (18) as measured by whole body dual energy X-ray absorptiometry scan (model QDR 4500W, Hologic, Waltham, MA). Each subject and his parent/guardian were advised of all experimental procedures and associated risks before verbal assent was given by the child and a written informed consent was provided by the parent/guardian. Subjects were recruited via flyers distributed to schools in the Central Pennsylvania region. All subjects were healthy, normotensive, and not taking any medications that could affect their cardiovascular or thermoregulatory responses. Preliminary screening included blood chemistry analysis (CHEM-24, complete blood count and lipid profile, Quest Diagnostics), and resting 12-lead electrocardiogram. During a maximal graded exercise test on a treadmill, subjects began at a self-selected speed to elicit a HR of ~140- to 150-bpm at 0% grade, followed by an increase in slope of 2% until two of the following four criteria were met: 1) a plateau in oxygen uptake (V˙o2) defined as an increase of ≤ 2.0 ml/kg/min; 2) a HR > 195 bpm; 3) a respiratory exchange ratio > 1.0; or 4) subjective indicators of fatigue such as hyperpnea, facial flushing, unsteady gait and refusal of the child to exercise further (11,23). Subjects completed a physical exam during which a clinician determined pubertal status according to the criteria of Tanner (35). Subject characteristics are presented in Table 1.
Table 1.
Subject characteristics by group
| Lean Boys | Obese Boys | |
|---|---|---|
| n | 7 | 7 |
| Age, yr | 11 ± 0.3 | 11 ± 0.2 |
| Height, cm | 152 ± 2 | 155 ± 1 |
| Weight, kg | 42 ± 2 | 54 ± 4* |
| AD, m2 | 1.33 ± 0.03 | 1.50 ± 0.05* |
| AD/mass, m2/kg | 0.032 ± 0.001 | 0.028 ± 0.001* |
| Body fat, % | 18 ± 1 | 33 ± 2* |
| Lean body mass, kg | 32 ± 1 | 33 ± 1 |
| V˙o2max, ml ·kg−1·min−1 | 49 ± 1 | 37 ± 2* |
| V˙o2max, L/min−1 | 2.1 ± 0.1 | 2.0 ± 0.1 |
Values are means ± SE. AD, DuBois surface area; V˙o>2max, maximal aerobic capacity.
Significantly different from lean boys, P < 0.05
A minimum of 8-h before each test, subjects swallowed an ingestible temperature sensor (CorTemp, HQ Inc, Palmetto, Fla) for the measurement of Tc. The sensor is a single-use, pill-shaped electronic device that contains a telemetry system, a microbattery, and a quartz crystal whose frequency of vibration is linearly related to temperature. Each temperature sensor was calibrated by the manufacturer, which provides a serial number that is programmed into a handheld recorder (CT2000), ensuring an accuracy of 0.1°C. Each pill was used within 6 months from the date it was shipped by the manufacturer. During steady state exercise in a warm environment, the temperature and response time of the ingestible temperature sensor falls between that of rectal and esophageal temperatures (22).
Testing Procedures
Subjects were asked to refrain from caffeine consumption on each day of the experiment and reported to the lab at least 2-h after a meal. After providing a urine sample, the subject was instrumented with a Polar® heart rate monitor, belt and pouch to attach the handheld recorder (CT2000) to the subject for continuous Tc measurement and weighed (Seca 770, accuracy ± 50 g) wearing only shorts (all subsequent weights were taken wearing shorts only).
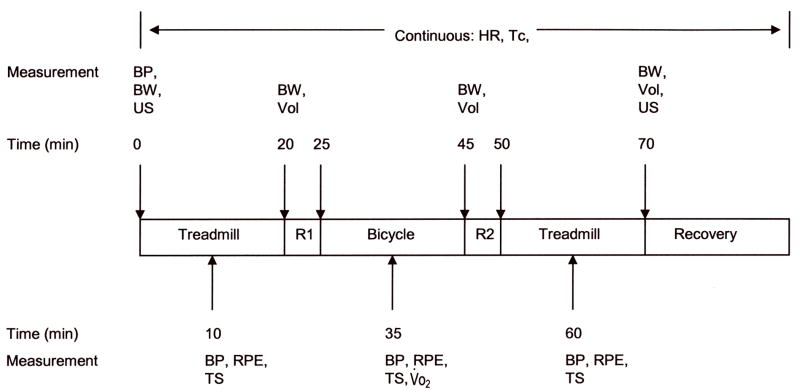
A total of six 70-min acclimation sessions were completed (one session per day) by each subject on separate days. During each trial, 2 subjects were test concurrently, 1 lean and 1 obese, in order to control for early/late summer seasonal and time of day variations. Testing began in the beginning of June and concluded by early September. Local weather for this period averages from 22 to 28°C (71 to 82°F; National Oceanic and Atmospheric Administration (NOAA), 2007). For all experimental trials the time between each scheduled test day was no more than 2 days. Subjects were encouraged to stay well-hydrated the day before each trial. For all experimental trials, subjects wore shorts, socks and sneakers. Since experiments were conducted in the summer months, subjects were partially heat-acclimatized due to routine outdoor activities (38). Thus, baseline Tc in lean and obese children were measured and compared to assess the degree of natural acclimatization. Subsequently, each subject completed 6 acclimation sessions in order to compare physiological responses between lean and obese boys during repeated exercise/heat bouts from the partially heat-acclimatized state. Attainment of acclimation was defined by a similar final Tc for two consecutive sessions and a leveling off of Tc within the last exercise bout (all subjects completed 6 trials). A schematic of the experimental design is diagrammed in Figure 1.
Figure 1.
Schematic of the experimental design for each trial. HR, heart rate; Tc, body core temperature; BP, blood pressure; BW, body weight; US, urine sample; Vol, volume of fluid ingested; RPE, rating of perceived exertion; TS, thermal sensation; V˙o2, oxygen consumption; R1, rest period 1; R2, rest period 2.
During each session, subjects exercised at 30% of maximal aerobic capacity (V˙o2max) alternating between a treadmill (Precor USA C962) and cycle ergometer (Monark Ergomedic 818E) for three 20-min bouts interspersed with 5-min rests. Environmental conditions were held constant at 38°C, 50% relative humidity. During school recess and spontaneous playtime, children spend a majority of the time participating in light-to-moderate intensity activities (26,27); thus this exercise intensity was chosen because it reasonably simulates an intensity typical of a child during spontaneous physical exertion and of heat-acclimation studies. Body weight was measured during each rest period and the subject was given water to maintain body weight by replacing most water lost through sweat. The experiment ended when the subject either completed the protocol, if the Tc exceeded 39°C, if the subject experienced adverse signs (nausea, dizziness, etc.), or if the subject desired to stop. After exiting the chamber at the conclusion of the experiment, a post-experiment urine sample was obtained.
Measurements
All HR, and Tc data were measured continually through the protocol and stored as 1-min averages using computer software (Labview) in conjunction with a data-acquisition system (National Instruments, Austin, TX). Blood pressure by brachial auscultation (sphygmomanometry) was measured 10-min into each exercise bout. To ensure that each subject was working at the desired workload, expired air was measured 10-min into the second exercise bout for 5-min for the determination of V˙o2 (TrueOne 2400 Metabolic Measurement System, ParvoMedics, Salt Lake City, UT). Urine volume was measured with a graduated cylinder and urine color was determined by holding each specimen container next to a validated color scale (3) in a well-lit room. The eight-color scale ranges from very pale yellow (#1) to brownish green (#8). Urine osmolality (freezing point depression, Advanced DigiMatic Osmometer Model 3D2), and specific gravity (Refractometer, Atago A300CL) were determined in triplicate. Sweating rate was calculated from the net change in body weight corrected for fluid consumption and urine excreted.
Subjective ratings
During the preliminary screening, the Physical Activity subscale of the Physical Self Description Questionnaire -- which has been validated for use in adolescents (19,20,21) -- was completed to subjectively determine how “active” each subject perceived himself to be on a daily/weekly basis. Each item is a simple declarative statement, all positively worded, and subjects respond on a 6-point true-false response scale where 1 = “false”, 2 = “mostly false”, 3 = “more false than true”, 4 = “more true than false”, 5 = “mostly true”, and 6 = “true”. The statements to which the subjects responded were, “Several times a week I exercise or play hard enough to breathe hard (to be out of breath)”, “I often do exercise or activities that make me breathe hard”, “I get exercise or do sports activities 3 or 4 times a week that make me breathe hard and last at least 30 minutes”, “I do physically active things (like jogging, dancing, bicycling, aerobics, gym or swimming) at least three times a week”, “I do lots of sports, dance, gym or other physical activities”, and “I do sports, exercise, dance or other activities almost every other day”. During each experiment, ratings of perceived exertion ((RPE), Borg scale (5)) and thermal sensation ((TS), using a 0–8 scale in which 0 = unbearable cold, 4 = thermoneutral, and 8 = unbearably hot (40)) were measured 10-min into each exercise bout.
Statistical Analyses
A repeated measures analysis of covariance was used to fit a model to the data by SAS PROC MIXED. This linear mixed model took into account the correlated nature of the repeated measures. Group was treated as a fixed effect and subjects were treated as random effects. The independent variables were group, time and day (where appropriate) and the dependent variable was the measured physiological response. When making multiple comparisons, Bonferroni adjustments were used. Results were considered significant at P < 0.05.
During exercise in the heat, whereas metabolic heat production is a reflection of absolute intensity, heat loss mechanisms are a function of relative intensity. Thus, heat storage and the subsequent rise in Tc is dependent to some degree upon both absolute and relative intensities (17). In the present study, work at the same relative intensity was the logical choice in order to investigate differences in heat loss mechanisms between lean and obese boys. However, to investigate the impact of absolute vs. relative intensity, 4 lean and 3 obese subjects repeated the first heat-acclimation trial which matched the absolute and relative workloads of the lean and obese groups (i.e. decreasing the workload for the lean group to match the obese group and increasing the workload for the obese group to match the lean group). The time between the completion of the 6th heat-acclimation trial and the repeat heat-acclimation trial was > 2 months.
Results
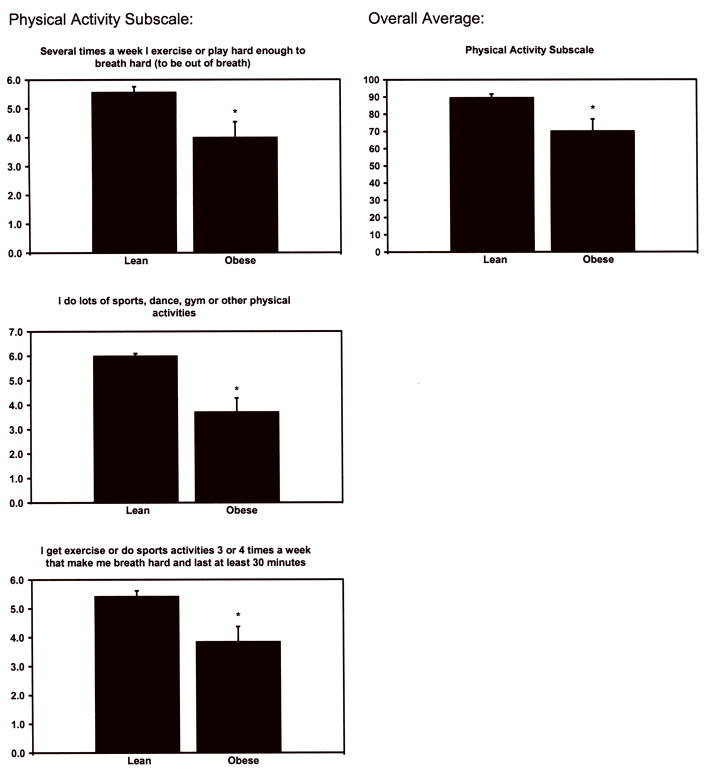
Responses to the Physical Activity subscale of the Physical Self Description Questionnaire are presented in Figure 2. Compared to lean subjects, obese subjects perceived themselves to be significantly less active (P < 0.03) as determined by significantly lower ratings to the following questions: “Several times a week I exercise or play hard enough to breath hard (to be out of breath)” (P < 0.03), “I get exercise or do sports activities 3 or 4 times a week that make me breath hard and last at least 30 minutes” (P < 0.02), “I do lots of sports, dance, gym or other physical activities” (P < 0.003).
Figure 2.
Responses to the Physical Activity subscale of the Physical Self Description Questionnaire on a 6-point true-false scale where 1 = “false”, 2 = “mostly false”, 3 = “more false than true”, 4 = “more true than false”, 5 = “mostly true”, and 6 = “true”. Only statements yielding significant effects are presented. The subscale was comprised of 6 statements and the average of the 6 scores represents the overall average for that subscale. *Significant group difference at P < 0.05.
Six lean and 2 obese subjects were classified as pre-pubertal (Tanner stage 1), 5 obese subjects were classified as mid-pubertal (Tanner stage 2–4) and 1 lean subject was classified as late-pubertal (Tanner stage 5). As expected, obese subjects weighed more, had a higher body surface area, a lower body surface area to mass ratio, higher percent body fat, and a lower V˙o2max (all P < 0.05; Table 1). Body fatness ranged from 14 to 20% in the lean subjects and from 28 to 45% in the obese subjects. The measured exercise intensity ranged from 27.6 ± 0.5% to 35.3 ± 1.0% for the lean subjects and 27.5 ± 1.2% to 35.5 ± 0.5% for the obese subjects across trials (P > 0.05).
Baseline, final exercise and change in Tc per trial by day of acclimation are presented in Table 2. On day 1, obese subjects were less naturally acclimatized as indicated by a significantly higher baseline Tc (P < 0.004). By day 6 compared to day 1, significant reductions in baseline Tc were evident in both groups (both P < 0.05), occurring at a similar rate (baseline Tc day 6 – day 1; P > 0.05). Obese subjects continued to have significantly higher baseline Tc on days 2 through 6 (all P < 0.05). Baseline Tc in obese subjects by day 6 was similar to that of lean subjects on day 1 (P > 0.05).
Table 2.
Baseline, final exercise and change in Tc by day of acclimation
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 6 – Day 1 | |
|---|---|---|---|---|---|---|---|
| Baseline Tc, °C | |||||||
| Lean | 37.41 ± 0.06 | 37.28 ± 0.06 | 37.35 ± 0.04 | 37.30 ± 0.06 | 37.22 ± 0.04† | 37.18 ± 0.04† | −0.23 ± 0.04 |
| Obese | 37.62 ± 0.06* | 37.44 ± 0.08* | 37.47 ± 0.10* | 37.47 ± 0.08* | 37.45 ± 0.05* | 37.41 ± 0.04*† | −0.21 ± 0.06 |
| Final Exercise Tc, °C | |||||||
| Lean | 38.17 ± 0.09 | 37.99 ± 0.06† | 37.95 ± 0.05† | 37.87 ± 0.06† | 37.78 ± 0.07† | 37.72 ± 0.06† | −0.45 ± 0.08 |
| Obese | 38.15 ± 0.05 | 38.19 ± 0.08 | 38.06 ± 0.06 | 38.07 ± 0.07 | 37.96 ± 0.05† | 37.89 ± 0.05† | −0.26 ± 0.04* |
| Δ Tc per trial, °C | |||||||
| Lean | 0.77 ± 0.08 | 0.72 ± 0.06 | 0.60 ± 0.04 | 0.58 ± 0.02† | 0.56 ± 0.04† | 0.54 ± 0.02† | −0.23 ± 0.09 |
| Obese | 0.53 ± 0.07 | 0.76 ± 0.12 | 0.58 ± 0.10 | 0.61 ± 0.11 | 0.51 ± 0.06 | 0.48 ± 0.08 | −0.05 ± 0.07 |
Values are means ± SE for 7 lean and 7 obese subjects. Tc, body core temperature; ΔTc = Final Exercise Tc − Baseline Tc.
Significant group difference at P < 0.05.
Significantly different from day 1 within group at P < 0.05.
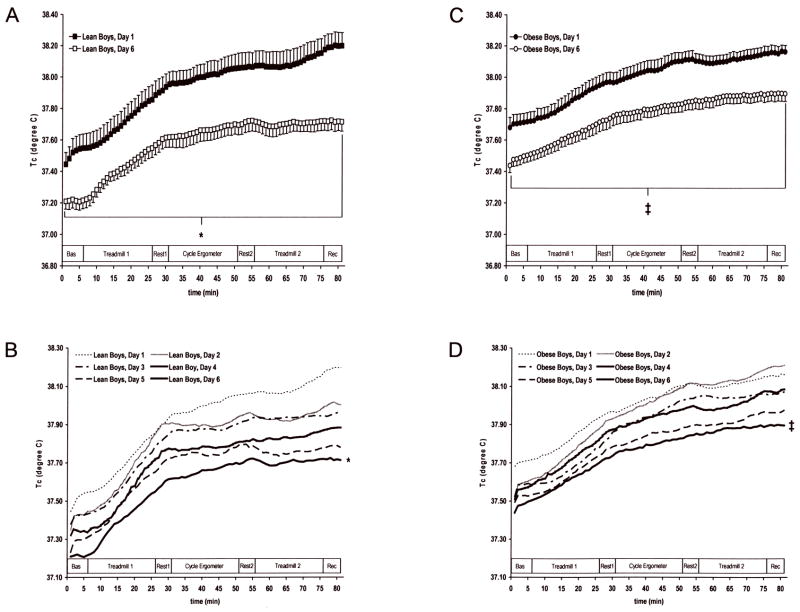
Compared to day 1, significant reductions in exercising Tc throughout the entire protocol were evident by day 6 in both groups (Figure 3; both P < 0.001), occurring at a significantly slower rate (final exercise Tc day 6 – day 1) in obese vs. lean subjects (Table 2, P < 0.05). The change in Tc per trial (ending – beginning Tc) was significantly lower in lean subjects on day 5 and 6 compared to day 1 (Table 2; P < 0.05) but not in obese subjects (P > 0.05). For both groups, there were no significant differences in Tc between day 5 and 6 (final Tc during exercise day 5 vs. day 6; obese = 37.96 ± 0.05 vs. 37.89 ± 0.05, lean = 37.78 ± 0.07 vs. 37.72 ± 0.06°C P > 0.05), suggesting attainment of heat-acclimation according to the operationally defined criteria of a similar final Tc for two consecutive sessions and a clear plateau in Tc during the last exercise bout (Figure 3).
Figure 3.
Time course of mean Tc response of 7 lean and 7 obese 9- to 12-yr-old boys during repeated exercise-heat bouts in the summer months. Exercise at 30% V˙o2max alternated between a treadmill and bike for 3 20-min bouts interspersed with 5-min rest periods at 38°C and 50% rh. Values are means ± SE. Bas, Baseline; Rec, Recovery. A (lean boys Tc, day 1 and day 6) and B (lean boys Tc, all 6 days): *P < 0.001 between day 1 and day 6 for lean boys. C (obese boys Tc, day 1 and day 6) and D (obese boys Tc, all 6 days): ‡P < 0.001 between day 1 and day 6 for obese boys.
The Bland-Altman approach to measuring agreements for repeated measures was used to determine the agreement of Tc between the first (relative exercise intensity) and repeated (absolute exercise intensity) heat-acclimation trials using ± 0.3°C as the physiological threshold for assessment. This threshold takes into account the anticipated standard deviation for Tc measurement in boys of this age (4). The mean difference between the two trials was 0.01°C and the standard deviation of the difference between the two trials was 0.08°C. The 95% limits of agreement were −0.1503 to 0.1621. Therefore, when matched for absolute and relative exercise intensity, the difference in Tc was within acceptable limits and considered marginal. This suggests that other factors independent of exercise intensity contribute to significant differences observed in the present study.
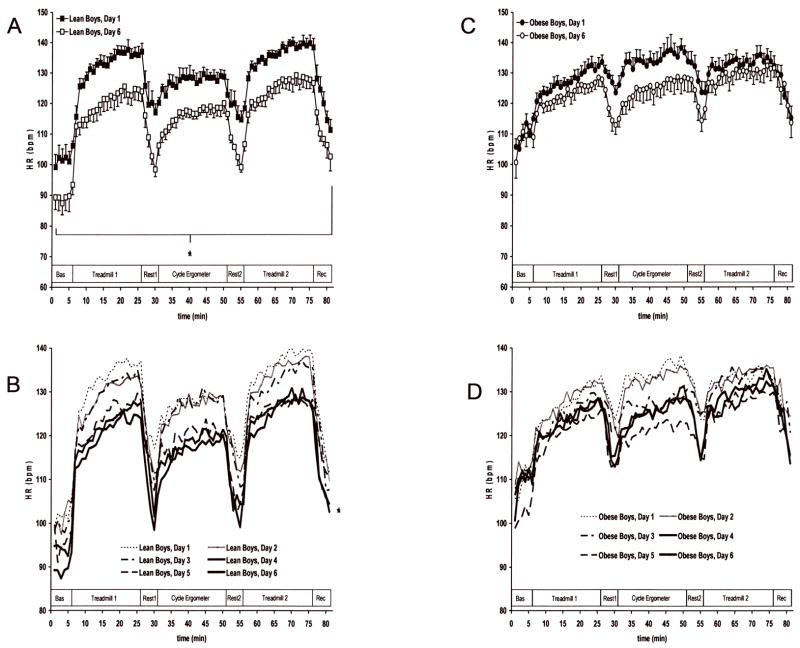
A significant reduction in HR from day 1 to day 6 occurred in the lean (P < 0.001) but not the obese subjects (Figure 4). The change in HR per trial (ending –beginning Tc) was significantly different between groups within each trial (P < 0.01), but not between-day within each group (change in HR day 1 vs. 6; obese = 26 ± 4 vs. 31 ± 6, lean = 39 ± 5 vs. 37 ± 3). Obese subjects had a significantly lower relative (ml·m−2·h−1) but not absolute (ml·h−1) sweating rate compared to lean subjects across all days (Table 3; P < 0.01). No urine variable was significantly different between groups.
Figure 4.
Time course of mean HR response of 7 lean and 7 obese 9- to 12-yr-old boys during repeated exercise-heat bouts in the summer months. Exercise at 30% V˙o2max alternated between a treadmill and bike for 3 20-min bouts interspersed with 5-min rest periods at 38°C and 50% rh. Values are means ± SE. Bas, Baseline; Rec, Recovery. A (lean boys HR, day 1 and day 6) and B (lean boys HR, all 6 days): *P < 0.001 between day 1 and day 6 for lean boys. C (obese boys HR, day 1 and day 6) and D (obese boys HR, all 6 days): No significant differences between days.
Table 3.
Sweating rate during repeated exercise/heat bouts by day of acclimation
| Sweating Rate, ml·h−1 |
Sweating Rate, ml·m−2·h−1 |
|||
|---|---|---|---|---|
| Lean | Obese | Lean | Obese | |
| Day 1 | 316 ± 44 | 312 ± 37 | 238 ± 33 | 207 ± 22* |
| Day 2 | 332 ± 40 | 334 ± 71 | 249 ± 30 | 218 ± 41* |
| Day 3 | 363 ± 50† | 348 ± 31 | 271 ± 34 | 231 ± 18* |
| Day 4 | 396 ± 70† | 361 ± 28† | 296 ± 51† | 240 ± 19* |
| Day 5 | 411 ± 79† | 379 ± 36† | 303 ± 54† | 250 ± 17*† |
| Day 6 | 424 ± 56† | 416 ± 44† | 316 ± 36† | 277 ± 29*† |
Values are means ± SE for 7 lean and 7 obese subjects.
Significant group difference at P < 0.01.
Significantly different from day 1 within group at P < 0.05.
Subjective responses to the exercise in the heat bouts on days 1 through 6 are presented in Table 4. At all time points on days 3 through 6, RPE were significantly higher in obese subjects. In lean subjects, a significant reduction in RPE occurred at min 35 and 60 on day 6 compared to day 1 and in TS at all time points on days 3 through 6.
Table 4.
Subjective responses to repeated exercise/heat bouts by day of acclimation
| RPE
|
TS
|
|||
|---|---|---|---|---|
| Lean | Obese | Lean | Obese | |
| Day 1 | ||||
| 10 min | 9 ± 1.0 | 10 ± 0.8 | 5.9 ± 0.2 | 5.4 ± 0.2 |
| 35 min | 12 ± 1.4 | 12 ± 1.1 | 6.2 ± 0.3 | 6.2 ± 0.3 |
| 60 min | 13 ± 1.5 | 13 ± 0.8 | 6.3 ± 0.4 | 6.3 ± 0.1 |
| Day 2 | ||||
| 10 min | 9 ± 1.0 | 10 ± 0.8 | 5.3 ± 0.3 | 5.1 ± 0.3 |
| 35 min | 11 ± 1.4 | 13 ± 1.1* | 5.7 ± 0.4 | 5.9 ± 0.2 |
| 60 min | 11 ± 1.7 | 14 ± 1.1* | 5.9 ± 0.4 | 6.6 ± 0.3* |
| Day 3 | ||||
| 10 min | 9 ± 1.3 | 11 ± 1.1* | 5.0 ± 0.3† | 5.1 ± 0.2 |
| 35 min | 11 ± 1.6 | 13 ± 1.1* | 5.6 ± 0.4† | 5.9 ± 0.3 |
| 60 min | 11 ± 1.8 | 14 ± 1.2* | 5.9 ± 0.4 | 6.0 ± 0.3 |
| Day 4 | ||||
| 10 min | 9 ± 1.2 | 12 ± 1.0* | 5.1 ± 0.3† | 5.1 ± 0.3 |
| 35 min | 10 ± 1.5 | 12 ± 1.1* | 5.6 ± 0.4† | 5.8 ± 0.3 |
| 60 min | 11 ± 1.7 | 14 ± 1.1* | 5.9 ± 0.4 | 6.1 ± 0.3 |
| Day 5 | ||||
| 10 min | 9 ± 1.3 | 11 ± 1.1* | 5.1 ± 0.3† | 5.3 ± 0.3 |
| 35 min | 10 ± 1.4 | 13 ± 1.1* | 5.5 ± 0.4† | 5.9 ± 0.2* |
| 60 min | 10 ± 1.4† | 13 ± 1.0* | 5.6 ± 0.4† | 6.1 ± 0.3* |
| Day 6 | ||||
| 10 min | 9 ± 1.1 | 11 ± 0.9* | 5.1 ± 0.3† | 5.4 ± 0.3 |
| 35 min | 9 ± 1.2† | 12 ± 1.2* | 5.3 ± 0.3† | 5.6 ± 0.2† |
| 60 min | 10 ± 1.3† | 13 ± 1.4* | 5.6 ± 0.3† | 6.1 ± 0.4* |
Values are means ± SE for 7 lean and 7 obese subjects. RPE, rating of perceived exertion; TS, thermal sensation.
Significant group difference at P < 0.05.
Significantly different from day 1 within group at P < 0.05.
Discussion
The main findings from this study are that during the summer months, obese (compared to lean) 9- to 12-yr-old boys 1) are less naturally heat-acclimatized as indicated by significantly higher baseline Tc, and 2) display a significantly slower rate of decrease in exercise Tc and less of an elevation in sweating rate during repeated bouts of light-to-moderate exercise at a similar relative intensity (30% V˙o2max) in a warm, humid environment. After 6 days of artificial heat-acclimation, baseline Tc in obese children reached that of lean children on day 1, whereas by day 6 lean children acclimated to a new baseline Tc. Since obese children started at a higher baseline Tc, and acclimate at a slower rate, this suggests that they require additional exercise/heat bouts in order to achieve a degree of acclimation similar to that of lean children. Therefore, obese children may require more attention and close monitoring to ensure their safety during exercise in the heat.
Beneficial effects of natural acclimatization
Adults exposed to warm summer weather attain some degree of natural acclimatization. Tc and HR are lower and sweating is more profuse and dilute in the summer compared to winter months during both a passive heat stress and exercise in the heat. (38). Experimental heat-acclimation occurs at a faster rate in both acclimatized (10) and more fit (31) adults. Physically fit adults during exercise in the heat display traits similar to that of heat-acclimatized adults (25). Pandolf et al. (24) showed that V˙o2max before acclimation was directly related to the rate of drop in exercising Tc over the course of heat-acclimation. Responses such as lower Tc and HR, and higher sweating rates during exercise in the heat are similar for adults residing in tropical climates and those who are artifically-acclimated, compared to unacclimated controls (38).
In children, very little is known regarding the beneficial effects of natural acclimatization. Children indigenous to tropical climates display high sweat rates and a heat-tolerance similar to adults during exercise in the heat (28,29). Although the American Academy of Pediatric guidelines (1) state that children should not perform physical activity if the wet-bulb globe temperature (WBGT) is greater than 29°C, heat-acclimatized 11- to 14-yr old girl athletes are able to tolerate exercise in conditions of higher heat and humidity (WBGT = 31.9 ± 1.5°C) (9). Girls of similar aerobic capacity, hydration status, and degree of heat-acclimatization as adult women display a stable HR, stroke index and cardiac index while cycling at 60% V˙o2max until fatigue in a hot and humid environment (WBGT = 29.9 ± 0.2°C) (29). Collectively, these studies suggest that children who are naturally acclimatized to tropical climates are able to effectively tolerate exercise in the heat. The present study indicates that both lean and obese children residing in more temperate climates who vary in their degree of acclimatization to the heat during the summer months are also able to tolerate exercise in the heat. On day 1, the obese boys were less naturally acclimatized as indicated by a significantly higher baseline Tc compared to lean boys. Although the Physical Activity subscale of the Physical Self Description Questionnaire in the present study did not differentiate between indoor and outdoor activity, it is likely that the higher baseline Tc on day 1 in the obese subjects was due to less outdoor physical activity and thus, less natural exercise/heat exposure compared to the lean subjects.
Heat-acclimation
In adults, significant reduction in resting Tc following acclimation to humid heat for 7 days have been observed (6). The present study demonstrates that children show similar physiological adaptations to 6 days of humid heat-acclimation. The reduction in baseline Tc in adults ranged from −0.1 to −0.5°C (6), while children tested here also fell within this range (reduction in baseline Tc: obese = −0.21 ± 0.06, lean = −0.23 ± 0.04). Interestingly, baseline Tc in the obese children on day 6 was similar to that of lean children on day 1, whereas lean children by day 6 acclimated to a new baseline Tc. This suggests that with regards to heat-acclimation during the summer months, the obese children in our sample were approximately 6 acclimation days behind the lean children. Therefore, for obese vs. lean children, additional heat exposures may be needed to match the degree of acclimation, even during warm summer months.
Heat-acclimation is most effectively induced through a combination of repeated exercise/heat bouts and is essential to minimize the associated thermal and cardiovascular stress. In adults, Buskirk et al. (8) reported that during a 10-day exercise/heat-(temperatures = 46°C dry bulb; 27°C wet bulb) acclimation protocol, overweight women compared to their lean counterparts were repeatedly unable to complete three 20-min walks interspersed with 20-min rests. In contrast, both lean and obese men tolerated the exercise/heat exposures well and were able to complete all experimental trials without incident. Lean 8- to 10-yr-old children were able to tolerate and complete repeated (7-days) acclimation bouts (temperatures = 43°C dry bulb; 24°C wet bulb), resulting in reduced cardiovascular and thermal strain (15). Only two studies (12,13) have investigated the response of an obese/overweight vs. lean child to exercise in the heat. Both studies reported no difference in heat tolerance (exercise time in the heat before a Tc of 39.4°C was reached) between lean and obese 9- to 12-yr-old children. However, although all subjects were able to complete 3 acclimation sessions (temperature range = 32 – 50°C dry bulb; 18 – 27°C wet bulb) prior to the heat tolerance trials, no acclimation data were provided. The present study indicates that although both groups were able to incur acclimation-related changes, obese children display a significantly slower rate of decrease in exercise Tc and less of an elevation in sweating rate during repeated bouts of exercise in a warm, humid environment. Although both groups began the study with different degrees of natural acclimatization, this still suggests that during the summer months, additional exercise in the heat-acclimation bouts may be necessary in order for obese children to obtain a degree of acclimation similar to that of lean children.
Numerous factors may account for the slower rate of heat-acclimation during exercise in obese vs. lean children in the present study. Due to the increase in subcutaneous body fat deposits, a larger obese individual, with a smaller body surface area/mass ratio, loses metabolic heat generated during exercise at a slower rate than a smaller lean individual (30) thus resulting in greater heat storage. Since adipose tissue has a lower specific heat of stored lipid (0.40 kcal·kg−1·°C−1 adipose tissue vs. 0.82 kcal·kg−1·°C−1 entire human body) storing the same amount of heat would induce a greater rise in temperature in adipose vs. lean tissue (7). Thus, the combination of a smaller body surface area/mass ratio and greater subcutaneous fat deposits may result in greater heat storage in an obese compared to lean child. Previous research has suggested that the degree of heat-acclimatization is related to body heat storage: the greater the amount of heat stored in the body, the higher the degree of heat-acclimatization (34). Others have suggested that there may be a “ceiling effect” or an optimal rate of heat storage above or below which a slower rate of acclimatization will occur (15). Although heat storage was not calculated in the present study, it is possible that the “ceiling effect” combined with the possible impaired heat dissipation mechanisms in obese vs. lean individuals discussed below contributed to the slower rate of heat-acclimation during exercise in obese vs. lean subjects in the present study.
Increases in body surface area cause inverse changes in sweat gland density but not in the total number, since the number of eccrine sweat glands in an individual does not change after 2 years of age (16). Thus the capacity for evaporative cooling in an obese child may be reduced. In the warm/humid environment of the present study, the evaporation of sweat was the primary means of heat dissipation and likely depends on the optimal sweating rate for a given unit of metabolic heat production and surface area. The lower sweating rates per body surface area in the obese vs. lean subjects in the present study may have been insufficient to maintain the evaporative heat loss necessary to match metabolic heat production, resulting in greater heat storage. However, previous research in children has reported no difference in sweating rate per body surface area, in 9- to 12-yr-old lean vs. obese boys during four exercise in the heat tolerance tests at a similar absolute intensity after partial heat-acclimation (13), which is at odds with the present study. The same study also reported higher evaporative rates per kilogram of weight in lean vs. obese boys. Due to the differing environmental conditions and exercise intensities (absolute vs. relative) between studies, it is difficult to explain the above discrepancies and addition research is warranted.
One hallmark of heat-acclimation is a reduction in day-to-day exercising HR. It is likely that not one but a combination of several mechanisms contributes to this improvement in cardiovascular function, including expansion of plasma volume, increase in venous tone from cutaneous and noncutaneous beds, and a reduction in Tc (38). In the present study, significant reductions in exercising HR by day 6 occurred in the lean but not the obese children. Since no prior study had addressed changes in cardiovascular function during heat-acclimation in obese children, it is difficult to speculate reasons for their lack of change in HR. However, previous findings in obese adults may provide some insight. Plasma volume expansion is most likely mediated via the influx of protein from cutaneous interstitial space to vascular compartments (33). Forearm blood flow during exercise in the heat is attenuated in obese compared to lean adults (36). Thus, obese subjects may be less able to flush proteins into the vascular compartments, resulting in a lower amount of fluid shifting from the intra- to the extracellular compartments, less plasma volume expansion and subsequently, less of a reduction in HR during repeated exercise/heat bouts compared to their lean counterparts. In addition, the cardiovascular system may be compromised in an obese adult, as demonstrated by left ventricular hypertrophy accompanied by systolic or diastolic dysfunction, increased cardiac output and stroke volume both at rest and during exercise (7). In adults during acclimatization in a hot, humid environment, HR is significantly correlated with both stroke volume and Tc, suggesting that both an increase in stroke volume and decrease in Tc independently are associated with the decrease in HR (39). Thus, if stroke volume was significantly higher on day 1 in obese subjects, then they may have less reserve to further increase stroke volume which would result in an attenuated decrease in HR.
Subjective ratings
In lightly-clothed adults, repeated exercise in the heat-acclimation bouts at a given relative intensity decrease RPE and TS, possibly reflecting a decrease in physiological (Tc and HR) strain (2). Very little is known regarding how perceived physical effort and/or thermal comfort change in response to an exercise/heat-acclimation protocol in children. Bar-Or and Inbar (4) found a significant reduction in RPE after a 5-day exercise in the heat-acclimation protocol in 8- to 10-yr-old lean boys. Findings from the present study, which demonstrates in lean children a significant reduction in RPE at min 35 and 60 on day 6 compared to day 1, supports this previous research. The significant reduction in TS at all time points on days 3 through 6 compared to day 1 in lean children also suggests improved thermal comfort. In response to the heat-acclimation protocol in the present study neither RPE nor TS (except for day 6 min 35) significantly decreased in obese subjects. This might suggest that obese children require additional exercise/heat-acclimation bouts in order to achieve a similar degree of improvement in effort perception and thermal comfort as lean children (although it is possible that the obese children may not be able to achieve this due to their obese condition). In addition, the present study indicates that obese compared to lean children have significantly higher RPE values during repeated exercise/heat bouts at all time points on days 3 through 6. It is difficult to postulate factors which may have contributed to the higher RPE values (i.e. increases in ventilation, metabolic rate, HR, mean skin temperature, Tc, acidity, etc.) and to differentiate the magnitude of their impact. It is interesting to note that the obese children had significantly higher RPE values 10-min into the exercise bout. The significantly higher effort perception during exercise in the heat in obese vs. lean children in the present study, could mean that obese children may require enhanced encouragement and support while exercising in the heat.
Limitations
An ingestible temperature sensor was used to measure Tc in the present study. One of the limitations of this procedure is that the position of the pill in the intestinal tract cannot be confirmed. Therefore, it is possible that if the same position is not achieved in each test, this could influence Tc measurement. However, for all 6 heat-acclimation trials, prior to each experiment the time at which the subject swallowed the ingestible temperature sensor was standardized (with the minimum being 8-h before each test). In addition, the time of day in which the subject was tested was standardized for all 6 heat-acclimation trials.
In summary, during the summer months, obese (compared to lean) 9- to 12-yr-old boys are less naturally heat-acclimatized as indicated by significantly higher baseline Tc. In addition, obese children display a significantly slower rate of decrease in exercise Tc and less of an elevation in sweating rate during repeated bouts of light-to-moderate exercise in a warm, humid environment compared to their lean counterparts. This suggests that obese children may require additional exercise bouts in the heat in order to achieve a degree of acclimation similar to that of lean children.
Acknowledgments
We are grateful to the children for their participation in this study and to the parents for supporting them. The technical assistance of Randy McCullough, Doug Johnson, and Jane Pierzga and data collection assistance of Allison Palaio, Matt Kenney, John Jennings, Samantha Wollman, Dave Nhan and Kristin Wielkiewicz is greatly appreciated. We thank the General Clinical Research Center nursing staff for their medical support. Results of the present study do not constitute endorsement by the American College of Sports Medicine.
GRANTS
This study was supported by National Institute of Health Grants R01-AG-07004-14 (W. L. Kenney), M01-RR-10732 (General Clinical Research Center), the Graduate Student Research Endowment from the College of Health and Human Development, The Pennsylvania State University (K. A. Dougherty), and by the Carl V. Gisolfi Memorial Research Fund from the American College of Sports Medicine Foundation (K. A. Dougherty)
Reference List
- 1.American Academy of Pediatrics: Committee on Sports Medicine and Fitness. Climatic heat stress and the exercising child and adolescent. American Academy of Pediatrics. Committee on Sports Medicine and Fitness. Pediatrics. 2000;106(1 Pt 1):158–159. [PubMed] [Google Scholar]
- 2.Aoyagi Y, McLellan TM, Shephard RJ. Interactions of physical training and heat acclimation. The thermophysiology of exercising in a hot climate. Sports Med. 1997;23(3):173–210. doi: 10.2165/00007256-199723030-00004. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong LE, Maresh CM, Castellani JW, Bergeron MF, Kenefick RW, LaGasse KE, Riebe D. Urinary indices of hydration status. Int J Sport Nutr. 1994;4(3):265–279. doi: 10.1123/ijsn.4.3.265. [DOI] [PubMed] [Google Scholar]
- 4.Bar-Or O, Inbar O. Relationship between perceptual and physiological changes during heat acclimatization in 8–10 year old boys. In: Lavallee H, Shephard R, editors. Frontiers of Activity and Child Health: Proceedings of the VIIth International Symposium of Paediatric Work Physiology. Ottawa, Canada: Editions du Pelican; 1977. pp. 205–214. [Google Scholar]
- 5.Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2(2):92–98. [PubMed] [Google Scholar]
- 6.Buono MJ, Heaney JH, Canine KM. Acclimation to humid heat lowers resting core temperature. Am J Physiol. 1998;274(5 Pt 2):R1295–R1299. doi: 10.1152/ajpregu.1998.274.5.R1295. [DOI] [PubMed] [Google Scholar]
- 7.Buskirk ER, Bar-Or O, Kollias J. Physiological effects of heat and cold. In: Wilson NL, editor. Obesity. Philadelphia: Davis; 1969. pp. 119–139. [Google Scholar]
- 8.Buskirk ER, Lundegren H, Magnusson L. Heat acclimatization patterns in obese and lean individuals. Ann N Y Acad Sci. 1965;131(1):637–653. doi: 10.1111/j.1749-6632.1965.tb34827.x. [DOI] [PubMed] [Google Scholar]
- 9.Cabrera-Davila Y, Rivera-Brown A, Berrios L, Frontera-Cantero J, Gonzalez J. Incidence of heat-related symptoms in acclimatized girl athletes during a training session in the heat. Med Sci Sports Exerc. 2006;38(5):S357. [Google Scholar]
- 10.Eichna LW, Bean WB, Ashe WF, Nelson N. Performance in relation to environmental temperature. Reactions of normal young men to hot, humid (simulated jungle) environment. Bull Johns Hopkins Hosp. 1945;76:25–58. [Google Scholar]
- 11.Goran M, Fields DA, Hunter GR, Herd SL, Weinsier RL. Total body fat does not influence maximal aerobic capacity. Int J Obes Relat Metab Disord. 2000;24(7):841–848. doi: 10.1038/sj.ijo.0801241. [DOI] [PubMed] [Google Scholar]
- 12.Haymes EM, Buskirk ER, Hodgson JL, Lundegren HM, Nicholas WC. Heat tolerance of exercising lean and heavy prepubertal girls. J Appl Physiol. 1974;36(5):566–571. doi: 10.1152/jappl.1974.36.5.566. [DOI] [PubMed] [Google Scholar]
- 13.Haymes EM, McCormick RJ, Buskirk ER. Heat tolerance of exercising lean and obese prepubertal boys. J Appl Physiol. 1975;39(3):457–461. doi: 10.1152/jappl.1975.39.3.457. [DOI] [PubMed] [Google Scholar]
- 14.Inbar O. Acclimatization to dry and hot environment in young adults and children 8–10 years old [dissertation] Columbia University; 1978. p. 170. [Google Scholar]
- 15.Inbar O, Bar-Or O, Dotan R, Gutin B. Conditioning versus exercise in heat as methods for acclimatizing 8- to 10-yr-old boys to dry heat. J Appl Physiol. 1981;50(2):406–411. doi: 10.1152/jappl.1981.50.2.406. [DOI] [PubMed] [Google Scholar]
- 16.Kawahata A. Sex differences in sweating. In: Yoshimura H, Ogata K, Itoh S, editors. Essential Problems in Climatic Physiology. Kyoto: Nankodo; 1960. pp. 169–184. [Google Scholar]
- 17.Kenney WL. Thermoregulation at rest and during exercise in healthy older adults. Exerc Sport Sci Rev. 1997;25:41–76. [PubMed] [Google Scholar]
- 18.Lohman TG. The use of skinfold to estimate body fatness on children and youth. J Phys Edu Rec Dance. 1987;58(9):98–102. [Google Scholar]
- 19.Marsh HW. The importance of being important: theoretical models of relations between specific and global components of physical self-concept. J Sport Ex Psychol. 1994;16:306–325. [Google Scholar]
- 20.Marsh HW. Construct validity of physical self-description questionnaire responses: relations to external criteria. J Sport Ex Psychol. 1996;18:111–131. [Google Scholar]
- 21.Marsh HW, Richards GE, Johnson S, Roche L, Tremayne P. Physical self-description questionnaire: psychrometric properties and a multitrait-multimethod analysis of relations to existing instruments. J Sport Ex Psychol. 1994;16:270–305. [Google Scholar]
- 22.O’Brien C, Hoyt RW, Buller MJ, Castellani JW, Young AJ. Telemetry pill measurement of core temperature in humans during active heating and cooling. Med Sci Sports Exerc. 1998;30(3):468–472. doi: 10.1097/00005768-199803000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Owens S, Gutin B. Exercise testing of the child with obesity. Pediatr Cardiol. 1999;20(1):79–83. doi: 10.1007/s002469900405. [DOI] [PubMed] [Google Scholar]
- 24.Pandolf KB, Burse RL, Goldman RF. Role of physical fitness in heat acclimatisation, decay and reinduction. Ergonomics. 1977;20(4):399–408. doi: 10.1080/00140137708931642. [DOI] [PubMed] [Google Scholar]
- 25.Piwonka RW, Robinson S, Gay VL, Manalis RS. Preacclimatization of men to heat by training. J Appl Physiol. 1965;20(3):379–383. doi: 10.1152/jappl.1965.20.3.379. [DOI] [PubMed] [Google Scholar]
- 26.Ridgers ND, Stratton G, Fairclough SJ. Assessing physical activity during recess using accelerometry. Prev Med. 2005;41(1):102–107. doi: 10.1016/j.ypmed.2004.10.023. [DOI] [PubMed] [Google Scholar]
- 27.Ridgers ND, Stratton G, Fairclough SJ. Physical activity levels of children during school playtime. Sports Med. 2006;36(4):359–371. doi: 10.2165/00007256-200636040-00005. [DOI] [PubMed] [Google Scholar]
- 28.Rivera-Brown AM, Gutierrez R, Gutierrez JC, Frontera WR, Bar-Or O. Drink composition, voluntary drinking, and fluid balance in exercising, trained, heat-acclimatized boys. J Appl Physiol. 1999;86(1):78–84. doi: 10.1152/jappl.1999.86.1.78. [DOI] [PubMed] [Google Scholar]
- 29.Rivera-Brown AM, Rowland TW, Ramirez-Marrero FA, Santacana G, Vann A. Exercise tolerance in a hot and humid climate in heat-acclimatized girls and women. Int J Sports Med. 2006;27(12):943–950. doi: 10.1055/s-2006-923863. [DOI] [PubMed] [Google Scholar]
- 30.Robinson S. The effect of body size upon energy exchange in work. Am J Physiol. 1942;36:363–368. [Google Scholar]
- 31.Robinson S, Turrell SE, Belding HS, Horvath SM. Rapid acclimatization to work in hot climates. Am J Physiol. 1943;140:168–176. [Google Scholar]
- 32.Sawka MN, Wenger CB, Pandolf KB. Thermoregulatory responses to acute exercise-heat stress and heat acclimation. In: Fregly MJ, Blatteis CM, editors. Section 4: Environmental Physiology. I. New York: Oxford University Press; 1996. pp. 157–185. [Google Scholar]
- 33.Senay LC, Mitchell D, Wyndham CH. Acclimatization in a hot, humid environment: body fluid adjustments. J Appl Physiol. 1976;40(5):786–796. doi: 10.1152/jappl.1976.40.5.786. [DOI] [PubMed] [Google Scholar]
- 34.Shvartz E, Saar E, Meyerstein N, Benor D. A comparison of three methods of acclimatization to dry heat. J Appl Physiol. 1973;34(2):214–219. doi: 10.1152/jappl.1973.34.2.214. [DOI] [PubMed] [Google Scholar]
- 35.Tanner JM. Growth at Adolescence. Oxford: Blackwell Science; 1962. The development of the reproductive system; pp. 28–39. [Google Scholar]
- 36.Vroman NB, Buskirk ER, Hodgson JL. Cardiac output and skin blood flow in lean and obese individuals during exercise in the heat. J Appl Physiol. 1983;55(1 Pt 1):69–74. doi: 10.1152/jappl.1983.55.1.69. [DOI] [PubMed] [Google Scholar]
- 37.Wagner JA, Robinson S, Tzankoff SP, Marino RP. Heat tolerance and acclimatization to work in the heat in relation to age. J Appl Physiol. 1972;33(5):616–622. doi: 10.1152/jappl.1972.33.5.616. [DOI] [PubMed] [Google Scholar]
- 38.Wenger CB. Human heat acclimatization. In: Pandolf KB, Sawaka MN, Gonzalez RR, editors. Human Performance Physiology and Environmental Medicine at Terrestrial Extremes. Carmel: Cooper Publishing Group; 1988. pp. 153–197. [Google Scholar]
- 39.Wyndham CH, Rogers GG, Senay LC, Mitchell D. Acclimization in a hot, humid environment: cardiovascular adjustments. J Appl Physiol. 1976;40(5):779–785. doi: 10.1152/jappl.1976.40.5.779. [DOI] [PubMed] [Google Scholar]
- 40.Young AJ, Sawka MN, Epstein Y, Decristofano B, Pandolf KB. Cooling different body surfaces during upper and lower body exercise. J Appl Physiol. 1987;63(3):1218–1223. doi: 10.1152/jappl.1987.63.3.1218. [DOI] [PubMed] [Google Scholar]