Abstract
The objectives of this study were to estimate the incidence and identify the temporal patterns of visits to Rhode Island emergency departments (EDs) by adults who were sexually assaulted. Visits to all Rhode Island EDs from January 1995–June 2001 by adults who were sexually assaulted were identified using International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9) codes. Medical records of these visits were reviewed. Frequency distributions of the assault characteristics and patient demographics were generated. Incidence rates (IRs) of ED visits after sexual assault were estimated using 2000 US Census data. Analyses of the temporal patterns of the ED visits after sexual assault were conducted. Of the 823 ED visits, 796 (96.7%) were by females and 27 (3.3%) were by males. The median age for females was 25 years (range, 18–96 years) and was 28 years (range, 18–87 years) for males. Among the female patients, 76.6% sustained a vaginal/anal assault. Among the male patients, 59.3% sustained an anal assault. The average annual IR of ED visits after sexual assault was 30.3/100,000/year for females and 1.2/100,000/year for males, which is a 25-fold greater incidence of these visits for females than males. ED visits after adult sexual assault were more frequent during warmer months and around 5 p.m. There was a gradual 43% increase in the IRs of ED visits after sexual assault over the 6.5-year period. These findings should help direct EDs to maximize supportive services when they are needed most often.
Keywords: Emergency service, Hospital/utilization, Incidence, Rape/statistics & numerical data, Rhode Island/epidemiology, Sexual behavior, Time factors, Rape, Sex offenses
Introduction
A recent national study reported that there were 143,648 emergency department (ED) visits after sexual assaults in the United States during 2001 and 2002.1 Researchers at one United States ED observed that the incidence of sexual assault evaluations at that ED increased by 60% from 1974–1991.2 If a similar trend is occurring elsewhere, an increase in ED visits after sexual assault would indicate a growing need for more medical, psychological, and social supportive services for these patients.
EDs and sexual assault survivor service providers would benefit from knowing the incidence of ED visits for sexual assault in their area and from knowing whether or not the incidence is increasing. Armed with this information, EDs and service providers could plan for an appropriate response to the needs of sexual assault survivors on a state or local level. In addition, understanding the temporal patterns of ED visits after sexual assault would allow EDs and sexual assault advocacy programs to know when to maximize the availability of qualified sexual assault health care providers and ensure access to appropriate services.
We first sought to estimate age and gender-stratified incidence rates (IRs) of ED visits by adults for sexual assault that occurred in an entire state, Rhode Island. Secondly, we aimed to identify temporal patterns for these visits and estimate what times EDs could anticipate when the needs for providing services to these patients would be the greatest.
Methods
Study Design and Setting
We conducted a medical record review of ED visits to all eleven civilian EDs in Rhode Island that provide medical care to adults after sexual assault. These EDs are at five general academic (teaching) hospitals, five community (non-teaching) general hospitals, and one women’s specialty care hospital. The state’s children’s hospital ED was not included in the study. ED visits after adult sexual assault during the 6.5-year period of January 1995 to June 2001 were included. This study was a part of a larger study that examined ED visits for blood or body fluid exposures, including sexual assault, which was conducted prior to the introduction of state-specific and updated federal recommendations on blood or body fluid exposure management.3–5 No studies on this topic have been conducted after this period. At the time of this study, there were no sexual assault nurse examiner (SANE) programs operating in the state. All hospital institutional review boards in the state approved the study.
Data Collection and Processing
Hospital and ED provider billing databases were searched using the following International Classification of Disease, Ninth Revision, Clinical Modification (Department of Health and Human Services, 6th Edition, 2001; ICD-9) codes: V71.5 (observation following rape), V15.41 (history of rape), and 995.83 (adult sexual abuse).
The authors searched for the medical records of all ED visits identified by the ICD-9 code-directed database query. The primary author and a team of trained research assistants reviewed each medical record and extracted the data according to a defined protocol onto a standardized data collection form. ED visits that were for an adult sexual assault were included in the study. For these visits, the age and gender of the patient; type of sexual assault exposure; year, month, and day of the week of the sexual assault ED visit; and hours elapsed from time of sexual assault to ED presentation were recorded on the standardized form. Prior to conducting the medical record review, the research assistants underwent over ten hours of training on how to extract data from the medical records. The primary author directly observed the research assistants during their review of the first fifty medical records, periodically reviewed the accuracy of their data extraction throughout the study, and reviewed each data collection sheet.
The type of sexual assault exposure was classified according to the parts of the body affected during the assault: anal or vaginal penetration, genital touching only, or oral sex. This classification also indicates the potential severity of a blood or body fluid exposure and consequent need for prophylaxis, based upon body location and type of exposure. All assaults classified as “anal or vaginal penetration” involved penile penetration. Assaults in which assailants used fingers or other objects to touch or penetrate the genitalia were classified as “genital touching only”. “Oral sex” exposures involved oral–genital contact; however, the direction of the sexual act could not be determined from the medical records. Patients whose medical record did not have any details of the sexual assault were designated as “not stated”, and those patients who could not recall or did not know the details of their sexual assault were classified as “not recalled”.
Two trained research assistants independently entered every form into an Epi Info 2002 (Centers for Disease Control and Prevention, 2002) database, and then performed a data comparison analysis to verify that all forms were entered correctly. Incorrect entries were corrected, and subsequent analyses were performed on this verified database. The database was transferred to STATA 8.2 (Stata Corporation, College Station, TX) for analysis.
Data Analysis
The data analysis included calculating summary statistics of the demography of the assaulted patients and characteristics of the sexual assault (type of sexual exposure and time elapsed from sexual assault to ED visit). IRs of ED visits after adult sexual assault stratified by age and gender were estimated by Poisson regression modeling. IRs were expressed as the number of ED visits per 100,000 persons by age group categories and gender using 2000 US Census figures for Rhode Island.6 The average IR over the 6.5-year period was calculated using the 2000 US Census as a base year. Census figures for intercensal years were estimated from available US Census data and were used in the calculations for trends over time. Corresponding 95% confidence intervals (CIs) for IRs were calculated using recommended methods.7 Plots of IRs by year for males and females and for females only were created. Tests of trend using Poisson regression were conducted to assess increases in the IRs of ED visits after sexual assault over the 6.5-year period. Plots and tests of trend of ED visits for males only were not performed due to the small number of cases.
To identify temporal patterns for ED visits, plots of the unadjusted frequency of ED visits after sexual exposures by month of the year, day of the month, day of the week, and hour of the day were created using the statistical software program R 2.5.1 (http://www.r-project.org/). Peak and nadir times for visits were identified from the plots. Temporal data from missing cases were not imputed since these data could not be inferred from the medical records. The Walter & Elwood (W&E) seasonality test was used to assess the existence of cyclic patterns in ED visits over time.8 Goodness of fit Χ2 testing was employed to evaluate the strength of the evidence for these patterns. These two tests were performed to determine whether or not the peak and nadir times identified in the plots reflected true recurring temporal patterns. All tests were considered statistically significant at the α = 0.05 level.
Results
Study Population
The ICD-9 code search identified 1,009 ED patient visits. Of these, 968 (95.9%) visits had medical records that were available for review; and of these, 823 (85.0%) were confirmed as ED visits after an adult sexual assault. The remainder constituted errors in ICD-9 coding. Of the 823 ED visits after adult sexual assault, 796 (96.7%) were by females and 27 (3.3%) were by males. The median age for the females was 25 years (range: 18–96 years) and was 28 years (range: 18–87 years) for the males. The majority (63.2%) of ED visits after adult female sexual assault occurred at the state’s women’s hospital, 25% were at the five community hospitals, and 11.8% were at the five academic hospitals. For males, 66.7% of the visits were at the academic hospitals and 33.3% at the community hospitals.
Characteristics of the Sexual Assaults
Table 1 provides a description of the types of sexual exposures sustained during the sexual assaults. The majority of sexual assaults involved anal and/or vaginal exposures from penile penetration. Except for two female–female assaults, all assailants were male. The assailant gender was not recorded or not recalled in 7.8% of the visits. The time elapsed from assault to ED presentation was available for 786 patients. The range of time elapsed was <1 to 275 h for females (interquartile range: <1 to 1 h) and <1 to 8 h (interquartile range: <1 to 2 h) for males. Among females, 92.8% presented within 96 h and among males, 85.7% presented within 96 h of their assault. Time elapsed from assault to ED presentation could not be calculated for 28.6% for the males and 4.1% of the females since the time of the assault was either unknown or not stated in the medical record. For these 786 patients, 89.2% presented within 72 h.
Table 1.
Characteristics of the sexual assaults
| Male (n = 27)% | Female (n = 796)% | |
|---|---|---|
| Type of sexual assault exposure | ||
| Vaginal/anal | 59.3 | 76.6 |
| Vaginal only | N/A | 46.9 |
| Anal only | 55.6 | 1.3 |
| Vaginal/anal | N/A | 6.7 |
| Vaginal/oral | N/A | 14.9 |
| Anal/oral | 3.7 | 0.6 |
| Vaginal/anal/oral | N/A | 6.3 |
| Oral only | 22.2 | 3.6 |
| Genital touching only | 3.7 | 4.9 |
| Not recalled | 14.8 | 12.8 |
| Not stated | 0 | 2.0 |
| Time elapsed from sexual assault to ED presentationa | (n = 21 %) | (n = 765 %) |
| <24 h | 33.3 | 52.8 |
| 25–48 h | 23.8 | 27.7 |
| 49–72 h | 19.1 | 9.9 |
| >72 h | 23.8 | 9.5 |
aTime elapsed was not recorded or known for all patients
Incidence Rates of ED Visits after Sexual Assault
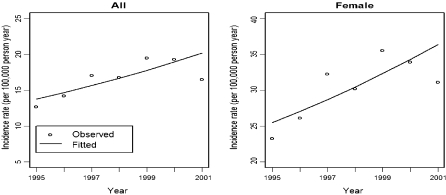
IRs after ED visits after sexual assault generally decreased with age (Table 2). For females, IRs were highest among 18–24-year-olds. IRs were greater for those under age 35 than for those 35 years of age and older (males: 2.2 [1.9–2.5] vs. 0.7 [0.4–1.1]; females: 73.1 [68.4–78.0] vs. 10.3 [9.2–11.5]). IRs for ED visits were 25-fold greater for females than males (30.3 vs. 1.2/100,000 persons). Figure 1 shows a plot of the IRs of ED visits over the study years for males and females (all) and for females only. Poisson regression modeling demonstrated that there was a gradual 43% increase in the IRs of ED visits for males and females after sexual assault over the 6.5-year period (test of trend: p ≤ 0.03). There was a marginally statistically significant trend for a 44% increase in the IRs of ED visits for females only (test of trend: p ≤ 0.05).
Table 2.
Incidence of ED visits after sexual assault per 100,000 persons in the Rhode Island population
| Male | Female | |||||||
|---|---|---|---|---|---|---|---|---|
| Total assaults | Average # assaults/yr | Census 2000 | Assault incidence per 100,000 | Total assaults | Average # assaults/yr | Census 2000 | Assault incidence per 100,000 | |
| 18 to 24 years | 9 | 1.38 | 52,873 | 3.1 (1.6–5.8) | 377 | 58 | 53,734 | 130 (117.6–143.9) |
| 25 to 29 years | 7 | 1.08 | 31,792 | 2 (1.4–6.2) | 112 | 17.2 | 32,940 | 46.5 (38.7–56.0) |
| 30 to 34 years | 1 | 0.2 | 36,821 | 0.4 (0.1–2.9) | 107 | 16.5 | 38,773 | 42.0 (34.8–50.8) |
| 35 to 39 years | 6 | 0.9 | 41,812 | 2.2 (1.0–4.9) | 98 | 15.1 | 43,552 35.3 | (29.0–43.0 |
| 40 to 44 years | 1 | 0.2 | 41,452 | 0.3 (0.1–2.8) | 53 | 8.2 | 43,494 | 20.3 (15.5–26.5) |
| 45 to 49 years | 0 | 0 | 36,702 | 0 ( 0–3.7) | 17 | 2.6 | 38,727 | 7.4 (4.6–12.0) |
| 50 to 54 years | 0 | 0 | 32,660 | 0 (0–4.5) | 11 | 1.7 | 33,774 | 5.8 (3.2–10.4) |
| 55 to 59 years | 1 | 0.2 | 24,024 | 0.7 (0.1–5.3) | 5 | 0.8 | 25,958 | 3.4 (1.4–8.2) |
| 60 to 64 years | 1 | 0.2 | 18,298 | 0.9 (0.1–6.58) | 3 | 0.5 | 20,709 | 2.4 (0.8–7.4) |
| 65 to 69 years | 0 | 0 | 16,408 | 0 (0–7.1) | 2 | 0.3 | 19,615 | 1.4 (0.4–5.8) |
| 70 to 74 years | 0 | 0 | 16,143 | 0 (0–7.4) | 2 | 0.3 | 21,518 | 1.4 (0.3–5.5) |
| 75 to 79 years | 0 | 0 | 13,637 | 0 (0–9.2) | 1 | 0.2 | 20,439 | 0.8 (0.1–5.4) |
| 80 to 84 years | 0 | 0 | 8,392 | 0 (0.1–15.4) | 1 | 0.2 | 15,353 | 1.0 (0.1–7.3) |
| 85 years or more | 1 | 0.2 | 5,422 | 2.9 (0.4–23.5) | 7 | 1.1 | 15,475 | 7.2 (3.5–15.2) |
| Total | 27 | 4.2 | 376,436 | 1.2 (0.8–1.7) | 796 | 122.5 | 424,061 | 30.3 (28.3–32.5) |
FIGURE 1.
ED visits after sexual assault by year, 1995 through mid-2001.
Temporal Patterns of ED Visits after Sexual Assault
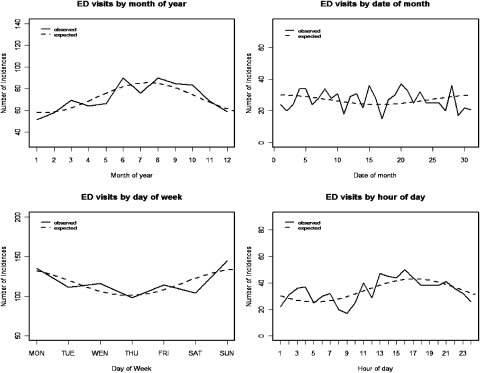
As shown in Figure 2, ED visits after sexual assault were more frequent during the summer months, and demonstrated a peak in August and a nadir in January/February (W&E seasonality test: p ≤ 0.01). There was a peak in visits on Saturday/Sunday and a nadir on Thursdays (W&E seasonality test: p ≤ 0.02). Visits were more frequent in the evening, with a peak at 5 p.m. and a nadir at 5 a.m. (W&E seasonality test: p ≤ 0.01). There were no cyclic patterns by day of the month (W&E seasonality test: p ≤ 0.09). Although the W&E seasonality tests indicated cyclic variations by month, week, and hour of the day, goodness of fit testing suggested that the available data only supported the presence of variations by month and hour of the day.
FIGURE 2.
Temporal patterns of ED visits after sexual assault.
Discussion
Most of the patients evaluated in the ED after sexual assault in Rhode Island were female and presented to EDs at an approximately 25-fold greater incidence than males. Incidence of visits generally decreased with age and the highest incidence was among young adult women. These results indicate that EDs should anticipate that the majority of patients who will present for sexual assault will be young adult women, and therefore EDs must be able to offer appropriate services from the ED for this demographic group, such as emergency contraception for dispensing from the ED.
Analysis of temporal patterns indicated peak times for these visits in the summer months and the evening hours. The data also show that the incidence of ED visits after sexual assault has been increasing. These results help inform EDs and sexual assault survivor service providers to expect that this trend will likely continue, and provide direction on when to expect ED visits after sexual assault. The temporal patterns can be used to plan for the provision of medical, psychological, and social services for these patients when they are needed most. For example, in areas where sexual assault nurse examiner programs are available, staffing could be maximized during the peak times identified in these analyses.
The reason for the rise in incidence of ED visits for sexual assault is not known, given national data supporting a decrease in the occurrence of sexual assault. The rise might then be a sign that more sexual assault survivors are seeking medical treatment and forensic evaluations. This observation might reflect the success of community education, sexual assault advocacy, and law enforcement efforts that emphasize the reporting of sexual assault and the accompanying medical evaluation.
It is important to note that most female patients presented within 72 h of their assault. This finding indicates that time-dependent interventions, such as post-exposure prophylaxis for HIV, sexually transmitted diseases, and pregnancy, as well as the collection of evidence for the forensic examination, could be considered and conducted when appropriate for the majority of female patients. It is concerning that fewer of the male patients presented within 72 h. EDs should assist with community education programs, sexual assault advocacy groups, and law enforcement officials to ensure that survivors of sexual assault present as soon as possible for a medical and forensic examination after an assault.
National estimates of the incidence of sexual assault in the US are available through the Bureau of Justice’s National Crime Victimization Survey (NCVS), which includes sexual assault whether or not it was reported to police or evaluated in a medical setting. Data from the 2000 NCVS agree with our observation that the incidence of sexual assault reported in this survey is greater for those under age 35 than above age 359 and has a peak incidence between age 20–34.10 In regard to gender, the NCVS estimated that there were ten and 210 rapes/sexual assaults per 100,000 males and females, respectively, of age 12 and greater in 2000.9 Using the NCVS figures for 2000, we calculate that for males and females of age 18 and greater these estimates would be 7.7 and 172 per 100,000 persons, respectively. According to NCVS estimates, 54.4% of female sexual assault survivors received their medical care from a hospital after sexual assault.11 Using data from the 1998 National Violence Against Women (NVAW) Survey, Tjaden and Thoennes found that 35.6% of women sought medical care following rape and 50% of these were evaluated in an ED.12 It is important to note that, in general, NCVS estimates are believed to be lower for intimate partner violence than NVAW estimates due to survey methodology.13 The NCVS queries survey respondents about sexual assault in the context of a crime committed against them, while the NVAW asks respondents about any sexual encounter that is without consent, uses or threatens force, and involves penetration of the anus, mouth, or vagina. As a result, respondents might be more likely to report a sexual assault in the NVAW. If, as according to Tjaden and Thoennes,12 only 17.8% of sexual assaults are evaluated in EDs, then our estimates of the average annual incidence of sexual assault evaluated in Rhode Island EDs of 1.1 and 28.9 per 100,000 males and females, respectively, are reasonable. However, if the NCVS estimates that 34.8% of sexual assaults are evaluated in EDs are correct, then our estimates are half of the expected incidence for Rhode Island. We believe that our estimates for the incidence of ED visits for sexual assault are an underestimate, given that this was a retrospective study that employed ICD-9 codes to identify cases. However, it is more likely that the underestimate was small and not a 50% reduction. Therefore, we suggest that the 17.8% ED visit rate for sexual assault is probably reasonable for our state.
A few published studies exist on the frequency of sexual assault on a statewide level, but none are ED-based studies. In November 2002 to February 2003, Masho et al. conducted a cross-sectional telephone survey of women age 18 and older in Virginia on the prevalence of sexual assault.14 Due to its design, this study could not provide incidence estimates. Alexander et al. estimated the incidence of sexual assault among women in the workplace in Washington from 1980–1989.15 The authors utilized ICD-9 codes to search for sexual assault cases using the state’s worker’s compensation database. The study’s findings were specific to women in this setting. Roberto and Teaster recorded the nature of sexual abuse sustained by adult women under the care of Adult Protective Services in Virginia 1996–2001.16 The data are essentially a case series on sexual assault of women living in an assisted setting.
Ruggiero and Kilpatrick of the National Violence Against Women Prevention Research Center extrapolated data from the National Women’s Survey and the NVAW Survey to estimate the lifetime prevalence of forcible rape among adult women by state. Using 2000 census estimates for Rhode Island, they estimated that one out of eight adult women in Rhode Island had experienced forcible rape in their lifetime.17 However, the incidence of sexual assault cannot be determined from the study. The US Bureau of Justice calculates crime statistics for all states using crimes reported to the police. Using Bureau of Justice figures for Rhode Island and the 2000 Rhode Island Census population estimates, we calculated that there was an average of 33.9 reported forcible rapes per 100,000 females per year in Rhode Island from 1995–2001.18 In comparison, we estimated that the average annual incidence of ED visits for sexual assaulted females was 28.9/100,000 persons/year. Our estimates appear to be in concordance with the Federal Bureau of Investigation figures for reported rape in Rhode Island.
Limitations
There are several limitations to this study. First, this was a retrospective review of medical records. Not all medical records were available for review and some were incomplete, although the percentage of missing and incomplete records was relatively small. Further, using ICD-9 codes to identify cases has its limitations.19–23 Errors in coding, errors in the billing data base, and failure of the ED clinician to indicate a diagnosis of a sexual assault, are a few reasons why cases would not have been captured by this study. Further, we did note that there were differences across hospitals in which ICD-9 codes were more frequently used to designate a sexual assault. We purposely cast a wide net with the ICD-9 codes searched so to overcome these differences across institutions. However, given the high percentage of records available and the large sample obtained, we believe that we were able to describe the population reasonably well. Second, the data are from 1995 to 2001. Even though the data may seem dated, we believe the temporal patterns of when assaults occur during the day, week, month, and time of year are not likely to have changed. Future research can assess if the temporal patterns are in fact stable over time and if the increasing trend in ED visits for sexual assault is continuing. Third, information about the perpetrator of the assault was not consistently available in the medical records, so this information could not be evaluated in the context of the study. The relationship of the perpetrator to the survivor of the assault might influence when and where the survivor sought medical care, which would affect the estimates in this study. We are unable to assess the impact of this factor. Future studies can evaluate the impact of relationship of perpetrator and survivor on when and where survivors seek medical care in EDs. Fourth, ED visits undoubtedly underestimate the frequency of sexual assault in the population since a significant proportion of sexual assault survivors do not seek medical attention. At the minimum, however, our results are useful for ED planning for these patients. Lastly, since this study was based on ED visits in Rhode Island, generalization to other states might not be applicable in all cases. However, we believe that sexual assault incidence is not likely to vary significantly across states and know of no reason why temporal patterns of ED visits would vary by state. Other states can review their ED sexual assault data and assess if similar patterns are apparent.
Conclusions
In conclusion, this study assists in the establishment of a better understanding of the incidence and temporal patterns of ED visits for adults evaluated after sexual assault in an entire state. With this information we now have some direction in helping to guide statewide medical and social provisions for these patients, as well as a time frame to optimize scheduling of qualified sexual assault health care providers available to provide timely care and treatment for sexual assault survivors.
Acknowledgements
The preliminary findings of this study were presented at the American College of Emergency Physicians Research Forum, Washington, DC, September 27, 2005.
Dr. Merchant was supported by a National Institutes of Health training grant through the Division of Infectious Diseases, Brown Medical School, The Miriam Hospital, from the National Institute on Drug Abuse, 5 T32 DA13911. This study was supported in part by grants from the National Institutes of Health to the Brown/Lifespan/Tufts Centers for AIDS Research (P30 AI42853), the Rhode Island Foundation, and the Elizabeth Glaser Pediatric AIDS Foundation.
References
- 1.Saltzman LE, Basile KC, Mahendra RR, Steenkamp M, Ingram E, Ikeda R. National estimates of sexual violence treated in emergency departments. Ann Emerg Med. 2007;49(2):210–217 doi:10.1016/j.annemergmed.2006.10.015. [DOI] [PubMed]
- 2.Magid DJ, Houry D, Koepsell TD, Ziller A, Soules MR, Jenny C. The epidemiology of female rape victims who seek immediate medical care: temporal trends in the incidence of sexual assault and acquaintance rape. J Interpers Violence. 2004;19(1):3–12 doi:10.1177/0886260503259046. [DOI] [PubMed]
- 3.Sexually transmitted diseases treatment guidelines 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51(RR-6):1–78. [PubMed]
- 4.Merchant RC, Mayer KH, Browning CA. Nonoccupational HIV post-exposure prophylaxis: guidelines for Rhode Island from the Brown University AIDS Program and the RI Department of Health. Med Health R I. 2002;85(8):244–248. [PubMed]
- 5.Updated US. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001;50(RR-11):1–52. [PubMed]
- 6.US Census Bureau. Census 2000 Data for the State of Rhode Island.
- 7.Breslow NE, Day NE. Statistical methods in cancer research. Volume II—The design and analysis of cohort studies. IARC Sci Publ. 1987;(82):1–406. [PubMed]
- 8.Walter SD, Elwood JM. A test for seasonality of events with a variable population at risk. Br J Prev Soc Med. 1975;29(1):18–21. [DOI] [PMC free article] [PubMed]
- 9.Rennison CM. Criminal Victimization, 2000. Washington, DC: US Department of Justice; 2001.
- 10.Catalano SM. Criminal Victimization, 2003. Washington, DC: US Department of Justice; 2004.
- 11.Rennison C. Rape and Sexual Assault: Reporting to Police and Medical Attention, 1992–2000. Washington, DC: US Department of Justice; 2002.
- 12.Tjaden P, Thoennes N. Prevalence, Incidence, and Consequences of Violence Against Women: Findings From the National Violence Against Women Survey. Washington, DC: US Department of Justice; 1998.
- 13.Tjaden P, Thoennes N. Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women. Washington, DC: US Department of Justice; 2000.
- 14.Masho SW, Odor RK, Adera T. Sexual assault in Virginia: a population-based study. Womens Health Issues. 2005;15(4):157–166 doi:10.1016/j.whi.2005.04.001. [DOI] [PubMed]
- 15.Alexander BH, Franklin GM, Wolf ME. The sexual assault of women at work in Washington State, 1980 to 1989. Am J Public Health. 1994;84(4):640–642. [DOI] [PMC free article] [PubMed]
- 16.Roberto KA, Teaster PB. Sexual abuse of vulnerable young and old women: a comparative analysis of circumstances and outcomes. Violence Against Women. 2005;11(4):473–504 doi:10.1177/1077801204274329. [DOI] [PubMed]
- 17.Ruggiero KJ, Kilpatrick DG. Rape in Rhode Island: A Report to the State. Charleston: National Violence Against Women Prevention Research Center, Medical University of South Carolina; 2003.
- 18.Federal Bureau of Investigation. Crime in the United States, 2003: Uniform Crime Reports. Washington, DC: US Department of Justice; 2004.
- 19.Berman MF, Stapf C, Sciacca RR, Young WL. Use of ICD-9 coding for estimating the occurrence of cerebrovascular malformations. AJNR Am J Neuroradiol. 2002;23(4):700–705. [PMC free article] [PubMed]
- 20.Chewning SJ, Nussman DS, Griffo ML, Kiebzak GM. Health care information processing: how accurate are the data. J South Orthop Assoc. 1997;6(1):8–16. [PubMed]
- 21.Dixon J, Sanderson C, Elliott P, Walls P, Jones J, Petticrew M. Assessment of the reproducibility of clinical coding in routinely collected hospital activity data: a study in two hospitals. J Public Health Med. 1998;20(1):63–69. [DOI] [PubMed]
- 22.Campbell SE, Campbell MK, Grimshaw JM, Walker AE. A systematic review of discharge coding accuracy. J Public Health Med. 2001;23(3):205–211 doi:10.1093/pubmed/23.3.205. [DOI] [PubMed]
- 23.Schwartz RJ, Nightingale BS, Boisoneau D, Jacobs LM. Accuracy of e-codes assigned to emergency department records. Acad Emerg Med. 1995;2(7):615–620. [DOI] [PubMed]