Abstract
Purpose
To determine if adolescents who lose Medicaid entitlements when they leave foster care are subsequently able to secure employer-sponsored or student health insurance coverage.
Methods
Two year follow-up of a cohort of 404 adolescents leaving foster care in 8 counties in a Midwestern state. We conducted survival analysis to study predictors of time to first insurance loss, and logistic regression analysis to determine factors associated with insurance reacquisition, among these youth.
Results
A total of 206 adolescents (51%) left foster care during follow up, of whom 138 (67%) lost health insurance coverage within a mean of 3 months of leaving foster care. Those that regained coverage (34; 17% of those leaving foster care) did so after a mean period of 8 months spent without insurance. Hazard of insurance loss was lower for employed adolescents (HR: 0.5; 95% CI: 0.4–0.7; p<0.0001), but only half of all adolescents leaving foster care reported being able to secure employment. Student health insurance did not reduce hazard of insurance loss. Boys had significantly lower odds of regaining insurance compared to girls (OR: 0.2, SE: 0.5, p=0.003).
Conclusions
Most youth leaving the child welfare system seem unable to transition to other forms of health insurance coverage. Even those that do acquire coverage, do so after an inordinate period of time. Enacting existing extensions of Medicaid coverage until age 21 for foster care youth is necessary to provide the resources to address the considerable health and mental health needs among these youth.
Keywords: Child welfare, Medicaid, health insurance, foster care
INTRODUCTION
Health insurance eligibility for children in the child welfare system has been enshrined in policy for several decades.[1] However, federal policymaking to ensure continuity of insurance coverage once these children transition out of the child welfare system is less than a decade old. Continuity of health insurance coverage for older adolescents leaving the child welfare system is critical, given their considerable physical [2–5] and mental health needs [6–8]; these needs often persist after youth leave the child welfare system, and require resources to support continuity of care. Currently, there is no empirical data on the ability of adolescents to successfully secure health insurance coverage once they leave the child welfare system.
Most children have entitlements to Medicaid as long as they are in the child welfare system. States are required to provide Medicaid coverage for all children in foster care for whom states receive federal reimbursement for foster care expenses under Title IV-E of the Social Security Act.[9] States have the option of covering children in foster care who are not Title IV-E eligible, and all do so.[10] Consequently, 99% of all children in foster care are covered under Medicaid.[11] Coverage for children who are on the rolls of a child welfare agency but are maintained within their own homes (“in-home”) is less comprehensive, with an overall Medicaid coverage rate of approximately 84%.[11]
The problem of health insurance coverage arises when adolescents leave the child welfare system, usually between the ages of 18 and 21 years depending upon state policy.[12] In FY 2005, a total of 287,000 children exited foster care of whom over 29,000 (around 10%) were aged 18 years and over.[13] Only about 20% of these adolescents are eligible for public insurance, a phenomenon that causes many of these youth to go over an “insurance cliff.” [14]
This ‘insurance cliff’ exists because most entitlements to which children in the child welfare system are eligible end on their 18th birthday. The usual source of insurance coverage for adolescents in the United States – as dependents on birthparents’ employer-sponsored private health insurance – is largely unavailable for those who leaving foster care. Adolescents between the ages of 18 and 21 years are entitled to Medicaid only if they are either disabled, pregnant, or are parents.[14] Absent entitlements, states have the option to cover these older adolescents, and exercise this option in two ways. First, states can use the “Ribicoff children” option to cover children who meet income criteria for Medicaid, but do not meet other programmatic criteria.[15] Second, states may use Medicaid’s “medically needy” option to cover adolescents with significant health needs between the ages of 18 and 21 years who are otherwise ineligible for Medicaid. Today, the “medically needy” option has become the principal way in which older adolescents are enrolled into Medicaid.[16] However, because these are optional benefits, states do not always choose to cover older adolescents; national surveys reveal that 36% of all individuals between the ages of 18 and 24 years report being uninsured – the highest rate of uninsurance among all age groups.[17]
Recognizing the risk posed by loss of insurance entitlements, Congress passed the Foster Care Independence Act in 1999 (Public Law No. 106–169). Title I of the Act created an option for states to extend Medicaid coverage to adolescents who had been in foster care on their 18th birthday, were under 21 years of age, and met the income eligibility regulations of the state in which they lived.[18] States’ response to the passage of the Act was measured. By 2002 only 7 states had implemented the Act,[19] and as of 2007 only 18 states have implemented these eligibility expansions.[14] Following publication of that report, two states – North Carolina and Missouri – enacted these expansions in 2007. Presumably, one reason why states may be reluctant to expand benefits to older adolescents is the perception that these adolescents may secure other types of coverage, and that such expansions are unnecessary. However, there is no empirical evidence to show whether transitions to other types of health insurance actually occur among adolescents leaving foster care, or whether these youth fall into an insurance gap and remain uninsured.
In the present study we examine discontinuities in health insurance coverage from a 2-year follow-up study of adolescents leaving foster care in a Midwestern state that, at the time of this study, had not implemented provisions of the Foster Care Independence Act. We describe the magnitude and duration of insurance coverage after leaving foster care, and identify the effects of sociodemographic characteristics, maltreatment history, placement, need, and occupational status on insurance loss and reacquision among this cohort. We use survival analysis to test the hypotheses that (a) securing a job will significantly reduce time to first insurance loss, and (b) college or university student status will significantly reduce time to first insurance loss among these adolescents. Through these analyses, we attempt to provide policymakers with data that could inform legislation regarding Medicaid expansions to former foster care adolescents in their states.
METHODS
Study Design and Sample
This study recruited a cohort of participants aged 17 years in the custody of the child welfare agency in 8 counties in a Midwestern state between December 2001 and May 2003. Each participant was re-contacted every 3 months for a total study duration of 2 years. Further details regarding the study are available elsewhere [20, 21]. This study was approved by our university’s Institutional Review Board.
Of a total of 450 adolescents eligible to participate in the study, 406 (90%) were interviewed. Of these, 404 had complete data and formed the study sample. Of these, 148 were excluded from the analyses because they remained in foster care throughout the 2-year follow-up duration. Another 50 were left-truncated, i.e. no information was available on them once they left foster care and, consequently, we were unable to determine if these youth had any “exposure” to insurance coverage before they lost coverage. The remaining 206 youth (51%) left foster care, 138 (67%) lost insurance after leaving foster care, and 34 youth (17%) regained insurance coverage during follow-up.
Measures and Variables
Sociodemographic characteristics
Adolescents self-reported their age; interviewers recorded their gender as observed at first interview. Because our sample was predominantly white and Black, we aggregated all non-white adolescents into a single ‘youth of color’ category in multivariate analyses. Adolescents self-reported their place of residence at first interview, which was grouped into 5 categories – living in a foster home, living in a congregate care environment such as a group home, living independently, living with birthparents, or living with another relative. In multivariate analysis, we aggregated living situation into two categories – in-home (living with birthparents, or another relative), or out-of-home.
Maltreatment History
History of physical abuse and physical neglect were elicited from responses to the Childhood Trauma Questionnaire (CTQ) administered at first interview. The CTQ is a 28-item self-report instrument that elicits lifetime histories of maltreatment [22, 23]. We used cut-off scores provided by the developers for moderate and severe maltreatment to develop binary indicator variables for these types of maltreatment [24]. A third category of sexual abuse was elicited from questions asking about past experiences of being touched on one’s own – or being forced to touch another’s – private parts; and forcible vaginal, anal, or oral sex. Variables were coded such that adolescents could report more than one type of maltreatment concurrently.
Mental health need
Interviewers used the Diagnostic Interview Schedule [25] to obtain past-year diagnoses of major depressive disorder (MDD), posttraumatic stress disorder (PTSD), attention deficit/hyperactivity disorder (ADHD), manic episode, oppositional defiant disorder, conduct disorder, and substance dependence among participants at first interview. The DIS is a structured interview designed for use by lay interviewers, and its prior versions have been found to have good reliability and validity [26, 27]. We developed a binary variable indicating whether or not the adolescent had a mental health diagnosis based on the presence or absence of these disorders.
Health Insurance Transitions
Youth leaving the foster care system were asked about their insurance status at each follow-up wave. Lacking a direct measure of employer-sponsored or student health insurance coverage, we constructed proxies for each of these constructs. Participants self-reported their number of work hours per week at each wave of the study, from which we constructed a proxy for eligibility for employer sponsored health insurance coverage. Because we lacked data on whether the hours worked were all worked in a single job, we used any number of hours worked as potential eligibility for employer-sponsored coverage. This proxy measures potential eligibility for, and not actual take-up of, employer-sponsored health insurance. However, the former is the more policy-relevant metric of determining whether or not the option of securing an alternative source of health insurance exists, which could inform decision-making around Medicaid expansions.
A proxy for student health insurance eligibility was constructed from variables that asked whether the participant was attending college or university at each wave of the study. College-enrolled students have several pathways into health insurance coverage. A quarter of public universities and almost all private universities and colleges require that students have health insurance as a condition of enrollment; at least 3 states have enacted legislation requiring that students have health insurance in order to enroll; half of all full-time students reportedly receive health insurance through their parents’ plans; and a fifth have coverage through college and university plans.[28] Given the strong associations between college/university attendance and insurance coverage, participants reporting full time college or university student status were classified as being eligible for student health insurance.
Data Analyses
Because adolescents in the sample were closely clustered around 17 years of age, we did not use age in the analyses. We also followed the mental health services literature on child welfare populations to determine selection of variables for statistical analysis [20, 29–31].
For bivariate analyses, we present descriptive data on the original cohort (N=404); on those that left foster care and for whom insurance data were available (N=206); and on those that lost insurance coverage after leaving foster care (N=138). All descriptive analyses were conducted using bivariate chi-square tests of proportion.
For multivariate survival analysis, we used the cohort of 206 adolescents leaving foster care, and counted the number of waves until such time participants first reported becoming uninsured. We use a wave-based unit of time to insurance loss rather than calendar time because the exact time of insurance loss is interval-censored. A total of 34 individuals (17%) regained coverage at subsequent waves; given this small number and because the mean duration of time spent uninsured was 8 months, we right-censored adolescents at the time of their first insurance loss. A total of 61 adolescents in the sample had a missing value in the wave immediately preceding the wave in which insurance loss reportedly occurred. For these adolescents, we assumed that the first observed uninsurance wave was also the first wave at which insurance loss occurred. This is a conservative assumption, the effect of which is to lengthen the true time to insurance loss among this sample of children.
We then estimated a survival (event history) analysis using our predictors to identify variables that were associated with hazard of first insurance loss among these youth. A total of 28 youth (14% of those leaving foster care) had missing data at at least one wave. We compared estimates obtained from complete case as well as imputed data analyses using the method of Imputation by Chained Equations [32, 33]. There were no differences in estimates obtained from imputed and unimputed analyses (not shown), and results of complete case analyses are presented. We also conducted a logistic regression analysis to examine variables associated with reacquisition of insurance. All analyses were conducted in version 9 of Stata [34].
RESULTS
Sample Characteristics
The overall sample had a slightly higher percentage of females (56%); around half (51%) were African-American and 44% were white (Table 1). Physical abuse (46%) and neglect (46%) were the dominant forms of maltreatment. Most of these youth (42%) lived in a group home or other congregate care facility at first interview, while less than a third (29%) were in family foster care. A tenth (11%) lived independently or in their own homes. Under half (45%) of these adolescents met DSM criteria for a past year mental disorder at first interview. Summed across waves, 30% reported being employed, and 13% reported attending a college or university.
Table 1.
Characteristics of adolescents aging out of foster care
| Overall sample | Left foster care during 3-year follow-up | Lost insurance coverage after leaving foster care | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| TOTALS | 404 | 100 | 206 | 51.0 | 138 | 67.0 |
| Gender | ||||||
| Male | 178 | 44.1 | 81 | 39.3 | 58 | 42.0 |
| Female | 226 | 55.9 | 125 | 60.8 | 80 | 58.0 |
| Race/ethnicity | ||||||
| African-American | 206 | 51.0 | 88 | 42.7 | 59 | 42.8 |
| White | 178 | 44.1 | 111 | 53.9 | 74 | 53.6 |
| Hispanic | 1 | 0.25 | 0 | 0 | 0 | |
| Other | 19 | 4.65 | 7 | 3.4 | 5 | 3.6 |
| Maltreatment history | ||||||
| Physical abuse | 186 | 46.0 | 97 | 47.1 | 62 | 44.9 |
| Sexual abuse | 141 | 34.9 | 82 | 39.8 | 51 | 37.0 |
| Neglect | 186 | 46.0 | 87 | 42.2 | 54 | 39.1 |
| Placement | ||||||
| In family foster care | 116 | 28.7 | 53 | 25.7 | 33 | 23.9 |
| Placed with relatives | 74 | 18.3 | 39 | 18.9 | 27 | 19.6 |
| Lives in group home | 168 | 41.6 | 80 | 38.8 | 52 | 37.7 |
| Lives alone | 13 | 3.2 | 7 | 3.4 | 5 | 3.6 |
| Lives in own home | 33 | 8.2 | 27 | 13.1 | 21 | 15.2 |
| Mental health need | ||||||
| Any mental health diagnosis | 181 | 44.8 | 103 | 50.0 | 69 | 50.0 |
| Occupational status | ||||||
| Currently working | 115 | 28.5 | 112 | 54.4 | 66 | 47.8 |
| Education status | ||||||
| Currently attending college | 52 | 12.9 | 23 | 11.2 | 12 | 8.7 |
A total of 206 youth (52% of the original sample) left foster care during the 2-year follow-up, and 148 youth remained. Most of those that left foster care were white (N=111, 54%), while those that remained were largely youth of color (N=105, 71%; p<0.0001) (not shown). A smaller percentage of youth who remained were living in a group home or in family foster care (65% versus 76%, p=0.025), and a higher percentage reported being sexually abused (40% versus 32%, p=0.12). Finally, while 3 (2%) of those that remained reported working, 112 (54%) of those who left foster care found employment.
Of the 206 youth that left foster care, 138 (67% of those leaving foster care) lost health insurance coverage at some point during follow-up. Adolescents who lost coverage after leaving foster care did not differ significantly from those who managed to secure coverage after leaving foster care (not shown).
Loss and Reacquisition of Insurance Coverage after Leaving Foster Care
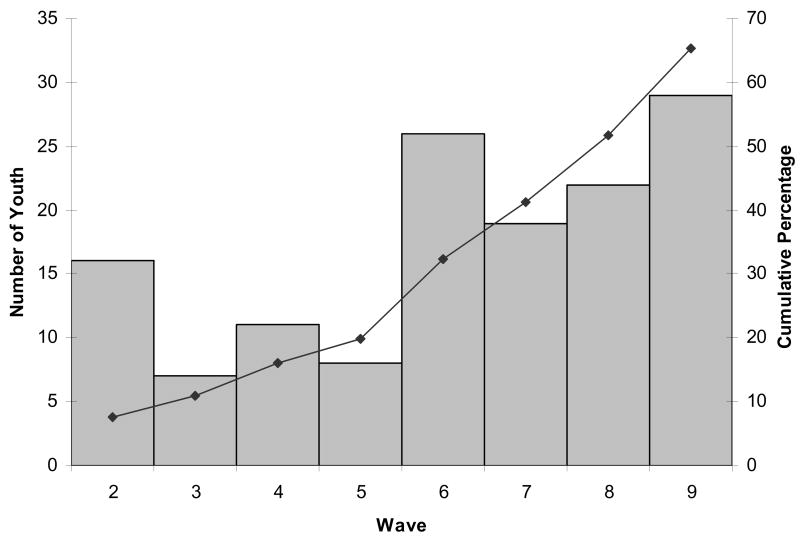
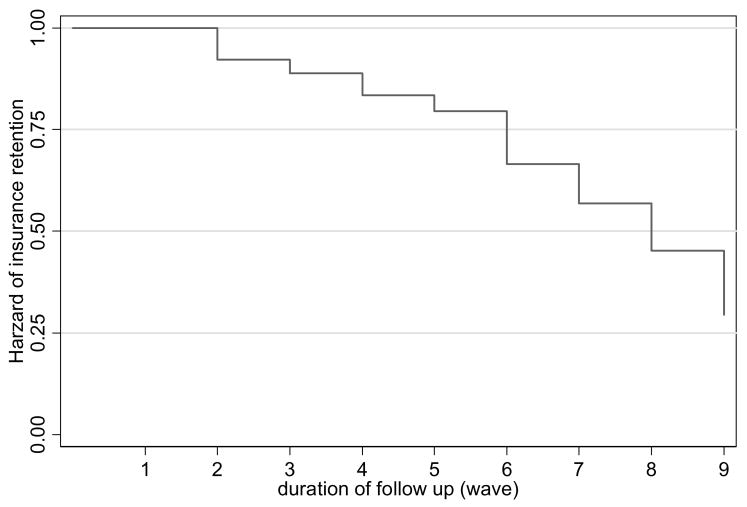
The number of youth who reported being uninsured varied by wave (Figure 1). At Wave 2 (3-month) follow up 16 youth (8% of those who left foster care) reported being uninsured. This percentage decreased to 3% over the next three quarters (waves), but reached 28% by the time of the final wave. Cumulative percentages of adolescents losing insurance rose steadily with duration of follow-up. As shown in the Kaplan-Meier curve (Figure 2), the hazard of insurance retention decreased (i.e. risk of becoming uninsured increased) throughout the duration of follow-up.
Fig 1.
Number and cumulative percentages of uninsured adolescents leaving foster care
Fig 2.
Hazard rates of insurance loss over time
Adolescents were insured for a median duration of approximately 3 months (mean duration of approximately 6 months) after leaving foster care before they reported becoming uninsured. On survival analysis of time to first insurance loss (Table 2), securing employment was associated with a lower hazard of insurance loss (HR: 0.5; 95% CI: 0.3, 0.7; p<0.0001). College or university student status was not associated with hazard of insurance loss.
Table 2.
Sociodemographic predictors of insurance loss among adolescents aging out of foster care
| Hazard Ratio | 95% CI | P value | |
|---|---|---|---|
| Gender | |||
| Male | 1.10 | (0.76–1.61) | 0.61 |
| Female | 1.0 | ||
| Race/ethnicity | |||
| Of color | 0.79 | (0.56–1.11) | 0.18 |
| White | 1.0 | ||
| Maltreatment history | |||
| Physical abuse | 1.14 | (0.77–1.69) | 0.53 |
| Sexual abuse | 0.86 | (0.59–1.27) | 0.86 |
| Neglect | 0.90 | (0.62–1.32) | 0.59 |
| Placement | |||
| In family foster care, placed with relatives, or in group home | 1.0 | ||
| In own home | 0.76 | (0.53–1.09) | 0.13 |
| Mental health need | |||
| Any mental health diagnosis | 1.01 | (0.71–1.45) | 0.80 |
| Occupational status | |||
| Works >=37.5 hours/week | 0.49 | (0.34–0.69) | <0.0001 |
| Education status | |||
| attending college | 0.93 | (0.51–1.70) | 0.80 |
N=206, number of failures = 138, total time at risk = 1433 waves. Model overall LR chi-square (9 df) = 21.05, p = 0.01.
A total of 34 adolescents (17% of those leaving foster care) regained coverage after losing it; these youth spent a mean of 8 months without insurance before being able to reacquire coverage. On logistic regression, male adolescents had 80% lower odds of regaining coverage when compared to female adolescents (OR: 0.2, SE: 0.5, p=0.003) (not shown).
DISCUSSION
In this local cohort of youth leaving foster care, we found that two-thirds (67%) of youth leaving foster care lost health insurance coverage, and were insured only for a median duration of around 3 months before loss of coverage. Only 1 in 6 youth who loses coverage regains it, but this happens after a mean duration of 8 months spent uninsured. Consistent with our hypothesis, employment status delayed onset of insurance loss; however, transitions to college or university student status occurred in relatively few youth. For a significant majority of adolescents leaving foster care there is, indeed, an “insurance cliff”[14] in that the majority of adolescents quickly lose insurance coverage once the insurance entitlements of foster care end, few regain coverage after losing it, and even those that do spend considerable periods of time without insurance.
Our finding that employment delays the onset of insurance loss is not necessarily a demonstration of the ability of these adolescents to secure employer-sponsored insurance coverage. First, only a quarter of adolescents leaving foster care reported working 40 hours or more per week. Because part-time positions are rarely associated with employer-sponsored insurance coverage [35], it is unlikely that the adolescents in our sample would be able to obtain employer sponsored insurance. Second, over half of those that reported working full-time equivalent hours reported being insured under Medicaid. Taken together, this suggests that not only are adolescents leaving foster care unable to secure the kinds of jobs that come with employer-sponsored coverage, but also that many of these adolescents face significant challenges in securing any type of job at all.
Most adolescents in the United States today are covered as dependents on their parents’ employer-sponsored health plans.[36] For adolescents leaving foster care, this avenue to coverage is likely largely closed. Furthermore, since 2000 a declining number of individuals have reported being covered under employer-sponsored health insurance – a situation resulting from higher rates of unemployment, fewer employers offering an insurance benefit and, among those that do, requiring that employees bear a larger share of the premium dollar.[37] These changes in the employer-sponsored health insurance market particularly affect low-income workers, from which population children arrive into the child welfare system. Such market-driven changes limit the ability of parental employer-sponsored health insurance to be a viable source of coverage for adolescents leaving foster care.
Our hypothesis that former foster care youth would secure student health insurance was not confirmed in this study because only a tenth of youth leaving foster care reported attending college or university – a trend that is in keeping with previously reported literature [12]. Only two-thirds of former foster care youth had completed their high school diplomas, and less than a tenth were taking college courses, in the 12–18 month period after leaving the child welfare system in Wisconsin.[38] This rate of college attendance is a fourth of that of the US general population. At the far end, a lack of college-level education prejudices benefits-rich employment in a competitive labor market; at the near end, not being in college also removes a source of health insurance coverage. Consequently, youth leaving foster care are especially vulnerable to insurance discontinuities.
Policymaking may be able to mitigate this risk. Because the adolescents leaving foster care face seem unable to secure alternate insurance coverage, Medicaid and child welfare policymakers should consider the option of extending Medicaid eligibility to all youth transitioning out of foster care at least until age 21 years. This can be accomplished in several ways. Enacting the provisions of the Foster Care Independence Act is perhaps the most direct way to extend coverage to all of these at-risk youth. Other existing Medicaid mechanisms may also serve this purpose. First, in only 19 states are adolescents below the age of 21 years eligible for insurance coverage under either the “Ribicoff children” or “medically needy” options.[14] States could eliminate age limits on optional coverage regulations. Second, over 8 states have sought and obtained Section 1115 waivers (research and demonstration project waivers) to expand Medicaid eligibility to older adolescents; such waiver mechanisms may serve to cover adolescents leaving foster care.[39] On the other hand, 5 states end all Medicaid coverage at age 19 years, 10 require a means test for Medicaid eligibility, and 5 states do not have any regulations under which older adolescents can qualify for Medicaid (authors’ analyses of state Medicaid regulations). Such restrictive policies have serious consequences for these youth who leave foster care with great needs for services.
These policy recommendations should be viewed in the light of some limitations of our study. First, our decision to censor youth at the time of first insurance loss may upwardly bias estimates of the total magnitude of insurance losses among youth leaving foster care since some of these youth might later on regain coverage with increasing duration of follow-up. The magnitude of this bias in our sample is minimized by the fact that in 2 years of follow-up only 34 youth regained insurance coverage; however, because youth were censored when the study ended, the true magnitude of insurance reacquisition cannot be estimated. This is why we focus on first loss of insurance coverage and do not attempt to provide overall estimates of insurance loss and reacquisition among this cohort. Second, our approach to estimating these transitions is based solely on eligibility for employer-sponsored health insurance or school health insurance. We do not measure actual enrollment (or take-up) into these types of coverage. Finally, these data are based on a geographically limited local cohort with a relatively small sample size. These factors limit this study’s generalizability, and preclude our ability to make broader estimates of the magnitude of the problem.
Despite these limitations, our study provides the first empirical assessment of health insurance discontinuities over a 2-year period as adolescents transition from a system that guarantees coverage to one in which insurance is seen as discretionary. Deploying policies that seamlessly ensure continuity of coverage is a necessary first step in ensuring that the considerable health needs of these adolescents are adequately resourced during their difficult transition from foster care to independent adulthood.
Acknowledgments
The authors thank Akeiisa Coleman for assistance with state Medicaid web site analyses. This study was supported by the National Institute of Mental Health (R01 MH 61404) to Dr McMillen, and the HHS/Administration for Children and Families (90PH0013) to Dr Raghavan.
Dr. Raghavan is an investigator with the Center for Mental Health Services Research, at the George Warren Brown School of Social Work, Washington University in St. Louis; through an award from the National Institute of Mental Health (5P30 MH068579).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Small MA. Obstacles and advocacy in children’s mental health services: managing the Medicaid maze. Behav Sci Law. 1991 Spring;9(2):179–188. doi: 10.1002/bsl.2370090207. [DOI] [PubMed] [Google Scholar]
- 2.Schor EL. The foster care system and health status of foster children. Pediatrics. 1982 May;69(5):521–528. [PubMed] [Google Scholar]
- 3.Halfon N, Mendonca A, Berkowitz G. Health status of children in foster care. The experience of the Center for the Vulnerable Child. Arch Pediatr Adolesc Med. 1995 Apr;149(4):386–392. doi: 10.1001/archpedi.1995.02170160040006. [DOI] [PubMed] [Google Scholar]
- 4.Halfon N, Klee L. Health services for California’s foster children: current practices and policy recommendations. Pediatrics. 1987 Aug;80(2):183–191. [PubMed] [Google Scholar]
- 5.Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics. 2000 Oct;106(4 Suppl):909–918. [PubMed] [Google Scholar]
- 6.Pilowsky D. Psychopathology among children placed in family foster care. Psychiatr Serv. 1995 Sep;46(9):906–910. doi: 10.1176/ps.46.9.906. [DOI] [PubMed] [Google Scholar]
- 7.Burns BJ, Phillips SD, Wagner HR, et al. Mental health need and access to mental health services by youths involved with child welfare: a national survey. J Am Acad Child Adolesc Psychiatry. 2004 Aug;43(8):960–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- 8.Landsverk J, Garland AF, Leslie LK. Mental health services for children reported to Child Protective Services. In: Myers JEB, Berliner L, Briere J, et al., editors. APSAC Handbook on Child Maltreatment. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 9.U.S. Department of Health and Human Services. Centers for Medicare and Medicaid Services. Medicaid eligibility: Mandatory eligibility groups. 2006. [cited 1/3/08]; Available from: www.cms.hhs.gov/MedicaidEligibility/03_MandatoryEligibilityGroups.asp#TopOfPage.
- 10.Geen R, Sommers A, Cohen M. Medicaid spending on foster children. Washington, D.C: Urban Institute; 2005. [Google Scholar]
- 11.Libby AM, Kelleher KJ, Leslie LK, et al. Child welfare systems policies and practices affecting Medicaid health insurance for children: A national study. Journal of Social Service Research. 2007;33(2):39–49. [Google Scholar]
- 12.Courtney ME, Heuring DH. The Transition to Adulthood for Youth “Aging Out” of the Foster Care System. In: Osgood DW, Foster EM, Flanagan C, et al., editors. On your own without a net: The transition to adulthood for vulnerable populations. Chicago, IL: University of Chicago Press; 2005. pp. 27–67. [Google Scholar]
- 13.U.S. Department of Health and Human Services AfCaF, Children’s Bureau. AFCARS Report - Preliminary Estimates for FY 2005. 2007. [cited 1/4/08]; Available from: http://www.acf.hhs.gov/programs/cb/stats_research/afcars/tar/report13.htm.
- 14.Fox HB, Limb SJ, McManus MA. The public health insurance cliff for older adolescents, Fact Sheet No. 4. April 2007. [cited 1/4/08]; Available from: http://www.incenterstrategies.org/jan07/factsheet4.pdf.
- 15.Mann C, Rowland D, Garfield R. Historical Overview of Children’s Health Care Coverage. The Future of Children. 2003 Spring;13(1):30–53. [PubMed] [Google Scholar]
- 16.Crowley J. Medicaid Medically Needy Programs: An Important Source of Medicaid Coverage. 2003. [cited 1/4/08]; Available from: http://www.kff.org/medicaid/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=14325.
- 17.National Center for Health Statistics (U.S.) Health, United States, 2006. Hyattsville, Md: Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2006. [Google Scholar]
- 18.U.S. Congress. Foster Care Independence Act of 1999 1999. [cited 1/7/08]; Available from: http://thomas.loc.gov/cgi-bin/query/F?c106:4:./temp/~c106HbJlA8:e3992.
- 19.English A, Morreale MC, Larsen J. Access to health care for youth leaving foster care: Medicaid and SCHIP. The Journal of adolescent health. 2003 Jun;32(6 Suppl):53–69. doi: 10.1016/s1054-139x(03)00071-5. [DOI] [PubMed] [Google Scholar]
- 20.McMillen JC, Scott LD, Zima BT, et al. Use of mental health services among older youths in foster care. Psychiatric Services. 2004 Jul;55(7):811–817. doi: 10.1176/appi.ps.55.7.811. [DOI] [PubMed] [Google Scholar]
- 21.McMillen JC, Zima BT, Scott LD, Jr, et al. Prevalence of psychiatric disorders among older youths in the foster care system. Journal of the American Academy of Child and Adolescent Psychiatry. 2005 Jan;44(1):88–95. doi: 10.1097/01.chi.0000145806.24274.d2. [DOI] [PubMed] [Google Scholar]
- 22.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American journal of psychiatry. 1994 Aug;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 23.Bernstein DP, Ahluvalia T, Pogge D, et al. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child and Adolescent Psychiatry. 1997 Mar;36(3):340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Bernstein DP, Fink L. Child Trauma Questionnaire: A Retrospective Self-Report. San Antonio, Texas: The Psychological Corporation; 1998. [Google Scholar]
- 25.Robins LN, Cottler L, Bucholz KK, et al. Diagnostic Interview Schedule for DSM-IV (DIS-IV) St. Louis, MO: Washington University; 2000. [Google Scholar]
- 26.Erdman HP, Klein MH, Greist JH, et al. A comparison of two computer-administered versions of the NIMH Diagnostic Interview Schedule. Journal of psychiatric research. 1992 Jan;26(1):85–95. doi: 10.1016/0022-3956(92)90019-k. [DOI] [PubMed] [Google Scholar]
- 27.Blouin AG, Perez EL, Blouin JH. Computerized administration of the Diagnostic Interview Schedule. Psychiatry research. 1988 Mar;23(3):335–344. doi: 10.1016/0165-1781(88)90024-8. [DOI] [PubMed] [Google Scholar]
- 28.Collins SR, Schoen C, Kriss JL, et al. Rite of Passage? Why Young Adults Become Uninsured and How New Policies Can Help (Issue Brief) 2006. [cited 1/22/08]; Available from: http://www.commonwealthfund.org/usr_doc/Collins_riteofpassage2006_649_ib.pdf?section=4039. [PubMed]
- 29.Raghavan R, Zima BT, Andersen RM, et al. Psychotropic medication use in a national probability sample of children in the child welfare system. J Child Adolesc Psychopharmacol. 2005 Feb;15(1):97–106. doi: 10.1089/cap.2005.15.97. [DOI] [PubMed] [Google Scholar]
- 30.Raghavan R, Leibowitz AA, Andersen RM, et al. Effects of Medicaid managed care policies on mental health service use among a national probability sample of children in the child welfare system. Children and Youth Services Review. 2006 Dec;28(12):1482–1496. [Google Scholar]
- 31.Zima BT, Bussing R, Crecelius GM, et al. Psychotropic medication treatment patterns among school-aged children in foster care. J Child Adolesc Psychopharmacol. 1999;9(3):135–147. doi: 10.1089/cap.1999.9.135. [DOI] [PubMed] [Google Scholar]
- 32.Royston P. Multiple imputation of missing values: Update. Stata Journal. 2005;5(2):188–201. [Google Scholar]
- 33.Royston P. Multiple imputation of missing values: Update of ice. Stata Journal. 2005;5(4):527–536. [Google Scholar]
- 34.StataCorp. Stata Statistical Software: Release 9. College Station, TX: StataCorp LP; 2005. [Google Scholar]
- 35.Kronick R, Olsen LC. A needle in a haystack? Uninsured workers in small businesses that do not offer coverage. Health services research. 2006 Feb;41(1):40–57. doi: 10.1111/j.1475-6773.2005.00467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fox HB, McManus MA, Reichman MB. Private health insurance for adolescents: is it adequate? Journal of Adolescent Health. 2003;32(6 Supplement 1):12–24. doi: 10.1016/s1054-139x(03)00070-3. [DOI] [PubMed] [Google Scholar]
- 37.Fronstin P. Sources of Health Insurance and Characteristics of the Uninsured: Analysis of the March 2007 Current Population Survey (Issue Brief No. 310). 2007. [cited 1/24/08]; Available from: http://www.ebri.org/pdf/briefspdf/EBRI_IB_10a-20071.pdf. [PubMed]
- 38.Courtney ME, Piliavin I, Grogan-Kaylor A, et al. Foster youth transitions to adulthood: A longitudinal view of youth leaving care. Child Welfare Journal. 2001 Nov-Dec;80(6):685–717. [PubMed] [Google Scholar]
- 39.Patel S, Roherty M. Medicaid Access for Youth Aging Out of Foster Care. 2007. [cited 1/15/2008]; Available from: http://www.aphsa.org/Home/Doc/Medicaid-Access-for-Youth-Aging-Out-of-Foster-Care-Rpt.pdf.