Abstract
Individuals who have developed a clinical dependence on drugs and/or alcohol often report that they sought help because they were “sick and tired of being sick and tired.” Quality of life (QOL) remains the missing measurement in the addictions arena. The few studies conducted to date show that QOL is typically poor during active addiction and improves as a function of remission. An intriguing question bears on the role of quality of life in subsequent remission status. Reasoning that higher life satisfaction may `increase the price' of future use and thus enhance the likelihood of sustained remission, this exploratory study tests the hypotheses that quality of life satisfaction prospectively predicts sustained remission, and that motivational constructs mediate the association. Inner city residents (N = 289, 53.6% male, mean age 43) remitting from chronic and severe histories of dependence to crack and/or heroin were interviewed three times at yearly interval beginning in April 2003. Logistic regression findings generally support our hypotheses: Controlling for other relevant variables, baseline life satisfaction predicted remission status one and two years later and the association was partially mediated by motivation (commitment to abstinence) although the indirect effect did not reach statistical significance. Findings underline the importance of examining the role of quality of life satisfaction in remission processes. Limitations of this exploratory study are discussed including the use of a single item global life satisfaction rating; suggestions for future studies are discussed including the need to embrace QOL as a bona fide clinical outcome and to use comprehensive standardized QOL measures that speak to individual dimensions of functioning. Implications are noted, especially the need for the addiction field to continue moving away from the pathology-focused model of care toward a broader model that embraces multiple dimensions of positive health as a key outcomes.
Keywords: Quality of life, remission, recovery, motivation, addiction, processes
1. Introduction
Drug and alcohol abuse are associated with multiple negative consequences in all areas of functioning.1 Substance use disorders are characterized in DSM-IV “as maladaptive patterns of substance use leading to clinically severe impairment or distress” in a broad range of areas of functioning including physical or psychological problems, personal safety, social relations, roles and obligations, work (American Psychiatric Association, 1994). These negative consequences and the hope for a better life, a `normal life', are key reasons substance users cite for wanting to stop using and for seeking help. The broad construct of quality of life (QOL) has assumed increased importance in clinical practice and research. Most areas of biomedical research have made a gradual paradigmatic shift from the traditional pathology-focused model of evaluating interventions by assessing disease-specific outcomes, to one that incorporates or is complemented by outcomes emphasizing QOL. Large-scale biomedical clinical trials now routinely include QOL as primary or secondary measures of outcome (Foster et al., 1999). Quality of life is an important diagnostic and outcome criterion that incorporates the individual's subjective view and illuminates domains not captured by traditional symptom measures (Donovan et al., 2005). Further, there is increasing evidence that QOL is of prognostic value - for instance, in treatment settings, higher pretreatment QOL satisfaction predicts better outcomes in inpatient psychiatric units (longer stay, fewer psychiatric symptoms) independently of baseline psychiatric status and other relevant factors (Russo et al., 1997; also see Lis et al. 2006).
1.1 Quality of life: Conceptualization and assessment
QOL research remains an emerging field; there is no universally accepted definition in biomedical circles (Bonomi et al., 2000; Smith et al., 1999). There is however a broad consensus that QOL is subjective - it cannot be observed by others (Bonomi et al., 2000); it is related to, but broader than perceived health status (Patrick & Erickson, 1988) and it is multidimensional - it captures a broad range of clinical, functional and personal variables (Aaronson, 1990 and 1991). Clinicians, researchers and federal agencies (NIH PROMIS, the U.S. Department of Health and Human Services' Food and Drug Amdinistration, 2006) unanimously regard three domains (dimensions) as key components of QOL: physical, social, and mental health and functioning (Testa & Simonson, 1996). Traditionally, the conceptualization of QOL has mirrored the pathology-based clinical care model and centered on subjective perceptions of the impact of health status on physical, psychological and social functioning and well-being (i.e., limitations in functioning), a concept referred to as “health-related quality of life” (HRQOL). In the last decade, in parallel with the reconceptualization of health as a positive resource rather than the mere absence of symptoms (WHO, 1985), “the goal is longevity with good function, and the challenge to health professionals is not only preventing disease and overcoming it when it occurs, but also helping people to achieve that goal” (Breslow, 2006, p17). A broader conceptualization of QOL has developed, exemplified by the World Health Organization's (WHO) definition of QOL as “an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.” (WHOQOL Group, 1995). This generic or overall conceptualization of QOL encompasses both life satisfaction in general, and satisfaction with specific life domains; in addition to shifting the focus from limitation in functioning to wellness, overall QOL is also conceptualized more broadly than is HRQOL, extending the scope from the three traditional dimensions (social, psychological and physical health) to factors such as environment safety and opportunity for recreation and leisure (i.e., living context). Bonomi et al. (2000), who reported on the US validation of the WHO instrument noted that “these additional factors that are not considered in some QOL instruments, [but] have been found important to individuals, groups and society, and are integral in describing overall QOL” (p. 1).
As summarized in Table 1, the two conceptualizations of QOL are reflected in the way they are measured. HRQOL measures, such as the MOS-Short For surveys (SF) series of instruments such as the SF36 (Ware, 1993), the most widely used instrument in biomedical QOL research, assess “health-limited” function bearing on daily tasks and social functioning - e.g., “has your health limited you in walking one block?” whereas overall “generic' QOL instruments, such as the World Health Organization Quality of Life instrument (WHOQOL-BREF - WHOQOL Group, 1998) assess perceived objective functioning (`how is your memory?') and subjective evaluation of functioning (`how satisfied are you with your memory function?'). The pathology-focused HRQOL approach is informative but limited in usefulness; it says where functioning limitations lie but does not inform on overall well being or satisfaction with life in general. Writing on behalf of the WHOQOL group, Szabo (1996) noted that most HRQOL instruments, “while beginning to provide a measure of the impact of disease, do not measure QOL per se” (p. 355- emphasis added). It is important and of prognostic value (see earlier) for clinical care to know how satisfied people are with important aspects of their life (e.g., social relations, health, living context) and measures of disease alone are insufficient determinants of health status (Bonomi et al., 2000; Skevington et al., 2004).To date, the bulk of QOL research, especially in the addictions, has adopted the HRQOL conceptualization and used corresponding instruments. This may be changing as the addiction field is increasingly recognizing the importance of focusing on positive outcomes (Venner et al., 2006); to wit, three recent European studies have used the WHOQOL-BREF instrument in their work among substance users (Bizarri et al., 2005; DaSilva et al., 2005; Günther et al., 2006) as does the NIAAA-funded COMBINE study (see Cisler et al., 2005), signaling that North American addiction researchers and their funding agencies are increasingly recognizing the usefulness of this area of research.
Table 1.
Prevalent conceptualizations and measurement Quality of life and their clinical implications
| Health-related RQOL | Overall generic QOL | |
|---|---|---|
| Definition | The effects of illness on the physical, mental and social dimensions of the individual's well-being | An individual's perception of their position in life in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns (WHO 1995) |
| Paradigm | Pathology | Wellness |
| Instruments | MOS-SF(6, 12, 36) | WHO-QOL and WHOQOL-BREF |
| Assesses | Health-related limitations | How much, often, completely, good, satisfied |
| Treatment focus | Symptom reduction | Maximized overall functioning and life satisfaction |
1.2 Quality of Life research in the Addictions
In 1990, Fallowfield referred to QOL as the missing measurement in health. Today, virtually no area of medicine is without published studies on QOL (Morgan et al., 2003). In 2008, QOL remains the missing measurement in addiction research. We lag far behind biomedical disciplines as well as behind the mental health field in embracing QOL as an essential outcome domain, especially in the US (Morgan et al., 2003). Systematic use of QOL indicators to monitor outcomes has been scarce in spite of the wide-ranging effects of substance use disorders (SUD) on patient, family and society (Peters & Foster, 2001; Préau et al., 2006).2 Recent reviews of the published literature indicate that a total of fewer than 40 studies have been published on QOL among SUD populations in the past 20 years (e.g., Donovan et al., 2005; Finney et al., 2003; Foster et al., 1999; Morgan et al., 2003; Smith & Larson, 2003; Rudolf & Watts, 2002). Published SUD studies almost all bear on alcohol-dependent persons with fewer than ten published studies examining QOL among illicit drug users (Morgan et al., 2003; Rudolf & Watts, 2002). A few studies have used mixed samples of alcohol and drug dependent individuals to study QOL (e.g., Morgan et al., 2003; Stein et al., 1998). Moreover, QOL studies of drug using populations have been restricted to dually-diagnosed persons and/or opiate users (Bizzarri et al., 2005; Fassino et al., 2004; Puigdollers et al., 2004; Villeneuve et al., 2006; Vorma et al., 2004). We found only one published (cross-sectional) study among crack/cocaine dependent persons (Havassy & Arns, 1998) in spite of crack accounting for 42% of treatment demand in the US while heroin accounts for only 27% of admissions (United Nations Office of Drug Control and Crime Prevention, 2000). There are of course studies that examine non-substance use outcomes but do not include the term QOL as keyword - e.g., studies using the Addiction Severity Index (ASI, Mclellan et al., 1992) encompassing domains such as family and social relations, psychological health and employment). Finney and colleagues (2003) reviewed 30 years of published outcome research on professional interventions for alcohol-dependent persons (1968-1998) and concluded that measures of global functioning were less likely to be included in more recently published studies. Of multigroup studies published between 1990 and 1998, only 38% reported on psychological functioning, the most frequent non-substance use outcome examined; 13% reported on global functioning, 13% on social/marital functioning, 16% on occupational functioning, 12% on physical health.
1.3 Quality of life among active and remitting substance users
The small body of research currently available on QOL among persons who use or abuse substances has been conducted for the most part, using convenience samples of individuals enrolled in professional treatment services; as is characteristic of emerging fields, the knowledge is base plagued with a number of limitations including a dire lack of prospective work and of long-term follow-ups among the few prospective studies, a lack of uniformity in the instruments used and in the way scores are reported. Available evidence shows that QOL is consistently poorer among active SUD persons and treatment seekers than among cohorts without SUD or chronic psychiatric conditions (for review, Donovan et al., 2005; Foster et al., 1999; Rudolf & Watts, 2002; Smith & Larson, 2003). This is consistent across comparisons of alcohol dependent samples with clinical and non-clinical cohorts (e.g., Daeppen et al., 1998), primary care patients (Johnson et al., 1995; Kraemer et al., 2002; Spitzer et al., 1995; Volk et al., 1997), comparison groups with chronic health or mental health conditions (Foster, Marshall & Peters, 1997 and 2000a; Powell & Crome, 1999), cancer, diabetes and heart failure (Foster et al;, 1997 and 2000b; Stein et al., 1998), and with nonalcoholic healthy groups (Rippeth, 1997; Romeis et al., 1999; Smith & Larson, 2003). For example, Smith and Larson (2003) reported that as measured by the SF-36 (Ware, 1993), SUD treatment clients have significantly lower QOL than the general population, as low or lower than patients with lung disease and diabetes and significantly lower than that of patients awaiting cardiac surgery. In terms of individual substances, the only study including cocaine dependent persons reported lower life satisfaction among primary cocaine users than in matched groups of users of other substances or non-abusers (Havassy & Arns, 1998). Moreover, one study reported that drug use may impair QOL more than does alcohol use (Smith & Larson, 2003) although another group found no difference in QOL between alcohol and drug users (Stein et al, 1998).
Given the low QOL among active users, a number of short-term studies, mostly among alcohol dependent samples, suggest that abstinence is associated with significant gains in QOL, particularly in mental functioning, and that QOL deteriorates among individuals who relapse (Foster et al., 2000a and 2000b; Holcomb et al., 1997; Kraemer et al., 2002; Morgan et al., 2003; Perrotta et al., 1999; Villeneuve et al., 2006; Vorma et al., 2004). The longest study bearing on QOL domains (although not labeled as `quality of life research') among substance dependent individuals followed previously untreated alcoholics at 2- and 10 years post-treatment and assessed physical, mental, social and occupational functioning (Moos et al., 1990). At 2-year follow-up, 49% were remitted (no drinking-related problems or clinical alcohol use in the previous 2 years) and at 10 years, 57% were remitted. At both follow-ups, the remitted group had significantly higher levels of functioning than did the relapsed group in every domain under study. Moreover, compared to a normative sample with no dependence history, the stably remitted group exhibited only a few deficits at 2-year follow-up (in physical and mental health) and functioned normally at 10-year follow-up. On the other hand, the relapsed group had significant deficits in functioning at both follow-ups, compared to both stably remitted and normative individuals. At this writing, the knowledgebase is lacking on QOL status or trajectories among individuals who remit naturally (i.e., without the use of formal or informal resources),
We examined the association between QOL satisfaction and remission duration in the same large sample of formerly poly-drug dependent persons in for the present study. Participants ranged in length of abstinence from one month to over ten years at recruitment (Laudet et al., 2006). In cross-sectional analyses, overall quality of life satisfaction increased gradually from under 6 months to 3 years of remission (i.e., a duration often considered as `stable' remission, Brecht et al., 1987); remission duration was significantly associated with QOL satisfaction, accounting for 9% of the variance explained, a finding that is consistent with prior reports that the role of abstinence on QOL is relative small (e.g., Stein et al., 1998). Subsequently, we reported findings from prospective analyses with the same cohort whereby after controlling for baseline level of QOL satisfaction, baseline abstinence duration predicted higher levels of QOL satisfaction a year later (Laudet et al., 2008). Taken together, emerging findings suggest that QOL is poor in key functioning domains among substance users and that reduced substance use and especially, abstinence, are associated with QOL improvements. Addiction is a chronic condition and treatment gains are often short-lived, especially in the absence of participation in post-treatment recovery promoting activities such as participation in 12-step fellowships (Fiorentine and Hillhouse, 2000; Kelly et al., 2006) or other support groups, and/or establishing a drug-free substance network. Many substance users cycle between abstinence and active use multiple times before (if ever) reaching stable remission (e.g., Dennis et al., 2005) Even among individuals who engage in recommended remission-promoting activities, relapses are not uncommon. This suggests that important factors implicated in sustaining remission remain unidentified.
1.4 Role of quality of life in remission processes
An intuitively appealing and potentially important question is whether QOL satisfaction plays a role in subsequent symptom level. Research on QOL among those with chronic conditions has focused thus far on the unilateral effect of symptom management on QOL -e.g. does symptom reduction lead to improved QOL? The human experience is complex, representing a dynamic interaction among multiple domains (biology, individual characteristics, internal and external resources and stressors, culture) that influence each other and cannot adequately be captured through linear or unidirectional analyses. A few researchers working with chronic disease populations outside of the addiction field have suggested that QOL may influence subsequent symptom status so that the association between QOL and subsequent symptom level may be bidirectional. For example, Youssef and colleagues noted that “Uncontrolled blood pressure alters hypertensive patients' QOL through anxiety and depressive reactions, and poor QOL hampers blood pressure control even with a therapeutic regimen” (Youssef et al., 2005. p.117). In the addictions arena, considering a bidirectional relationship between QOL and remission would translate into asking not only whether substance use affects QOL but also whether level of QOL satisfaction predicts subsequent remission. One of the most important predictors of remission is having something to lose (e.g., friends, health, job) if substance use continues (Costello, 1975; Havassy et al., 1993; Vaillant, 1995). Past consequences of drug use (loss) can also motivate change through the desire to ward off further loss. Behavioral economics and behavior choice theory are useful in elucidating these mechanisms (Bickel et al., 1992; Degrandpre et al., 1994). Drug dependence can be understood in terms of behavior choice - what factors result in the choice of drug over other reinforcers (Bickel et al., 1996). Of particular relevance is the basic principle of demand law whereby consumption decreases as price increases (Allison, 1983). Living drug-free is associated with a significant increase in positive experiences and with improvements in many areas of life (e.g., Laudet & White, 2005); these improvements may `increase the price' of future substance use; in other words, the risk of losing the valued benefits of a drug-free life may sustain motivation for abstinence.
We first identified this theme in qualitative interviews conducted in the sample used for the present study. Speaking of what helped maintain remission (`recovery'), participants made statements such as: “What worked for me is just the thought that I don't wanna go through that madness no more. … See, cause if I was to do that, I probably would lose everything”. Several researchers have alluded to the role of QOL on remission; for example, Blomqvist noted that among remitted substance users, “stability/improvements in several life areas contributed to sustaining the resolution” (2002, p. 149). Rudolf & Priebe (2002) reported that high satisfaction with life at treatment admission predicted subsequent abstinence rates. Conversely, low QOL may heighten the risk of relapse (e.g., Foster et al., 1998); in one study, emotional distress, being with peers who make commitment to abstinence difficult, and difficulties with relationship and finances during the year after baseline predicted relapse 12 months later (Claus et al., 1999; also Hoffmann & Miller, 1993). Thus QOL may be an important prognostic indicator and predictor of remission, yet it has not been examined systematically as such. Elucidating this issue and possible mediating processes has significant implications for service delivery: Intervention strategies focusing on non-substance use outcomes (e.g., housing, education work and social roles, existential well-being and spirituality, recreational activities) may afford clients something valued that they want to retain (something to lose), thus enhancing commitment to recovery. Conversely, QOL decreases including those resulting from general circumstances (e.g., bereavement, illness) may heighten the risk of relapse.
1.5 Study Objectives
The present study is a first step toward elucidating the role of QOL satisfaction in subsequent remission status among formerly drug-dependent persons. We build on our previous reports and use repeated measurements to test the following hypotheses:
Baseline level of quality of life satisfaction prospectively predicts sustained remission one and two years later, after controlling for baseline length of remission.
The association between QOL satisfaction and subsequent remission status is mediated by motivational constructs
2. Materials and Method
2.1 Sample
Recruiting was conducted in New York City through media advertisements over a one-year period starting in March 2003.3 Media recruiting has been the method of choice for studying recovered substance users who, by definition, do not present themselves at treatment programs. (e.g., Burman, 1997, Toneatto et al., 1999, Rumpf et al., 2000; for review, see Sobell et al., 2000) as well as persons who had resolved other addictions (e.g., gambling, Hodgins et al., 2000). A study assessing possible selection bias in media recruitment of naturally-recovered alcohol dependent persons compared a media recruited sample with a large random general population sample and concluded that “data do not justify assumption that a serious bias devalues findings from studies using media solicitation” (Rumpf et al, 2000, p. 773). The authors went on to state that “In contrast to snowball sampling, media solicitation avoids a recruitment of closed subcultures and a selection bias that can be minimized through a broad scope in the media.”
Interested parties called a toll-free number and were screened briefly as described in details elsewhere (Laudet et al., 2005). Eligibility criteria for the study were: (1) fulfilling the DSM-IV(TR) criteria for abuse or dependence of any illicit drug for at least one year in one's lifetime, but not in the past month; (2) self-reported abstinence from illicit drugs for at least one month, and (3) not being enrolled in residential treatment.4 Eligible individuals were contacted within a week of screening to schedule an in-person interview. Seven hundred and two unduplicated screenings were conducted. Of those, 440 were eligible and 353 were interviewed during the recruiting period (81% of eligible callers; we closed recruiting once our target sample size was attained). The study was reviewed and approved by NDRI's Institutional Review Board (IRB) and we obtained a certificate of confidentiality from our funding agency. The baseline interview session (BL) started by explaining the voluntary nature of the study, participation requirements and administration of the informed consent procedure. The interview lasted an average of two and a half hours. Each participant was paid $30 for his/her time. In-person interviews were also conducted one- and two-years after baseline. The one- and two-year follow-up interview protocols (F1 and F2) were somewhat shorter (background and historical information was collected at baseline); participants were paid $40 and $50, respectively, for these interviews. Participants were contacted by mail quarterly to maintain updated locator information and to thank them for their continued participation in the project. Three-hundred and seventeen one-year follow-up interviews were conducted on average (mean) 379 days after baseline (St Dev. = 45 days) and 308 F2 interviews were conducted a mean of 361 days after F1 (St. Dev. = 73 days), representing retention rates of 92% and 90% at F1 and F2, respectively). The sample for this study consists of the 289 individuals from whom we obtained both F1 and F2 data (84% of the surviving baseline cohort; 11 died).
Study participants were evenly divided between men and women (53.6% male), most were members of under-served groups (64% African-American, 15.5% non-Hispanic white, and 21.5% of other or mixed ethnic/racial background; 18% were of Hispanic origin) and ranged in age, at baseline, from 19 to 65 years (mean = 43, Std. Dev = 7.8). Educational attainment ranged from 5 to 18 years of schooling (mean = 12 year, Std. Dev = 2). Twenty percent were employed part-time, 22% full time with 60% citing government or other benefits (e.g., Veteran's pension) as primary source of income. Over half (56%) were single, 16% were married and 28% were widowed, separated or divorced. One quarter (24%) reported being seropositive for HIV antibodies, 30.8% had tested positive for Hepatitis C, and 40% had been diagnosed with a mental health disorder at some point in the past. The majority (84.4%) had no involvement with the criminal justice system at entry in the study; 13% were on probation or parole. Lifetime dependence severity measured by the Lifetime Non-alcohol Psychoactive Substance Use Disorders subscale of the Mini International Neuropsychiatric Interview (M.I.N.I, Sheehan et al., 1998) was high, with a mean score of 11.7 (Std. Dev. = 2.4; possible range on the scale is 0 to 14). The majority of participants had used multiple substances. The most frequent primary problem substance was crack cocaine (59.4%) followed by heroin (18.2%). Regular drug use had lasted on average 18.7 years (St.Dev. = 12 years); 86% had received one or more episode of addiction treatment. Length of abstinence at baseline ranged from one month to ten years (mean length of remission = 14 months).
2.2 Measures
The semi-structured instruments consisted of sociodemographics and background measures as well as of the measures described below and summarized in Table 2. We have used most of these instruments previously and where necessary, the items were reworded for ease of understanding at a reading level corresponding to 9th grade in the United States. Unless stated otherwise, higher scores represent a higher level of the construct under study.
Table 2.
Descriptives of key domains at baseline, one- and two-year follow-ups: remission, quality of life satisfaction and motivation for remission (N = 289)
| Baseline | Mean | St.Dev | Scale range |
|---|---|---|---|
| Quality of Life satisfaction | 7.6 | 1.9 | 0 - 10 |
| Commitment to abstinence | 3.1 | .45 | 1 - 4 |
| One-year follow-up | |||
| QOL satisfaction | 7.3 | 2.1 | 0 - 10 |
| Change in life satisfaction | 4.3 | .8.9 | 1 - 5 |
| Commitment to abstinence | 3.0 | .45 | 1 - 4 |
| Remission (% no use past year) | 66.4% | — | — |
| Two-year follow-up | |||
| QOL satisfaction | 7.0 | 2.0 | 0 - 10 |
| Change in life satisfaction | 3.9 | .99 | 1 - 5 |
| Commitment to abstinence | 3.1 | .41 | 1 - 4 |
| Remission (% no drug use past year) | 68.8% | — | — |
| Remission (% no drug since baseline) | 58.4% | — | — |
2.2.1 Baseline length of abstinence from illicit drugs
Alcohol and drug use history was collected using a list of 13 substances included in the Addiction Severity Index (ASI - McLellan et al., 1992).5 For each substance `ever' used once or more, participants provided the last date of use. A variable was computed for clean time at baseline (BL) from each substance ever used; length of abstinence represents time since most recent use of any of the illicit drug ever used, in months (i.e., if participant last used heroin 4 years ago and crack 5 months ago, length of recovery is 5 months).
2.2.2 Sustained remission
This was operationalized as no self-reported drug use in the year preceding each of the follow-up interviews. Dichotomous variables were computed to code whether or not each participant had sustained abstinence from drugs in the year preceding F1 and in the two years preceding F2 (i.e., since baseline). While reduced use may be a remission goal for some, empirical findings obtained both in the US and in Australia suggest that persons with severe histories of polysubstance misuse choose total abstinence as their remission goal (Laudet & Storey, 2006) and previous studies have reported that most failed remission attempts are based on moderation; abstinence proves more successful (Burman, 1997; Maisto, et al., 2002).
2.2.2.1. Corroboration of self-reported substance use
Saliva samples were collected as part of every interview but for budgetary reasons, samples are analyzed for participants who report no substance use since the previous interview because under-reporting is typically more prevalent in this population than is over reporting [neither participants not field staff were told this during data collection so as to minimize bias in self-report and data collection]. Saliva samples are tested for cocaine, opiates, THC and methamphetamines. The laboratory reports results (positive or negative) for each substance and we computed a summary variable (positive/negative for any of the four substances).
2.2.3 Quality of life satisfaction
“In general how satisfied are you with your life?” answered on a visual scale where 1 = `not at all,' and 10 “completely.” This item is one of the four Global satisfaction with life and health items in the World Health Organization Quality of Life instrument (WHOQOL, Bonomi et al., 2000). We used this global measure because we sought to assess participants' overall evaluation of their life satisfaction, taking into account the balance between positive and negative as it was relevant to their individual experience rather than the researcher deciding which life domains are or are not relevant to life satisfaction.
2.2.4 Change in life satisfaction
In addition to the yearly life satisfaction rating, participants rated change in quality of life relative to the previous year: “Looking back on the period [since previous interview], would you say that overall, your life has gotten a little better, much better, a little worse, much worse or stayed about the same? We used a 5 point Likert-type answer scale ranging from 1 (Gotten much worse) to 5 (Gotten much better).
2.2.5 Motivation
We used the Commitment to Abstinence subscale of the Addiction Treatment Questionnaire (Morgenstern & McCrady 1993; Morgenstern et al., 1996); it consists of five items each rated from for level of agreement, ranging from 1 (strongly disagree) to 4 (strongly agree); Cronbach Alpha in this dataset = .72.
2.3 Analytic Plan
Bivariate associations among the key variables were examined as a first step to testing the study hypotheses. The role of QOL satisfaction on subsequent remission status was examined using logistic regressions with baseline length of remission as a control variable. Analyses to test the mediation hypothesis were guided by widely used procedures initially described by Baron and Kenny (1986) and Kenny et al., (1998) and most recently used to test the role of intensive referral to 12-step meetings and of professional treatment on subsequent remission from alcohol use (Timko, Debenedetti & Billow, 2006 and Moos & Moos, 2006, respectively). To establish mediation, first, baseline QOL satisfaction was entered in a regression to predict F1 (or F2) remission status. Second, motivation was entered in a regression to predict subsequent remission, controlling for life satisfaction. If the odds of continued remission are greater among those with higher motivation, the requirements for step 2 are met. Third, life satisfaction was regressed on commitment to abstinence, the hypothesized mediator. Finally, life satisfaction and motivation were entered in a regression together to predict subsequent remission status; we compared the size of the effect of life satisfaction on remission when motivation is absent and present, and conducted a Sobel Z test to assess the significance of the indirect effect (Sobel, 1982). Statistical significance was set at p<.05 for all the analyses reported here.
2.4 Attrition analysis
We compared participants included in the analyses (n = 289) with those surviving for whom we did not obtain a full dataset (N = 53) on key individual-level variables: age, gender, race/ethnicity, primary substance, baseline length of recovery and lifetime addiction severity. Differences were assessed using chi-square for categorical variables and t-tests for continuous measures. Participants who provided a full dataset, compared to those who did not, did not differ in lifetime dependence severity, age or primary substance; however they were significantly more likely (p < 0.05) (a) to be older by three years at baseline (mean = 43 vs. 39.8); (b) to have been abstinent for a longer period (32 months vs. 13 months) and (c) to be African-American (86.5 vs. 77.1%, chi sq. = 5.1).
3. Results
3.1 Descriptives
3.1.1 Substance misuse outcomes at one and two-year follow-up
Descriptives of the study domains at each data collection point are presented in Table 2. Two-third of participants (66.4%) reported no drug use since baseline at the one year follow-up (F1), 68.5% reported no use since F1 at F2; overall, 58.4% of participants had no reported drug use since BL at F2, that is, they sustained remission for two years. At F2, 13.8% of the saliva samples were positive for one or more of the four substances,6 representing an 86.2% concordance rate for any substance, a finding that compares favorably with reports from the DATOS study (79% agreement between self-report and urine testing and 80% for hair toxicology for cocaine only -Simpson et al., 2002).
Length of remission at baseline was significantly associated with greater likelihood of sustained remission at F1, F2 and over the two years between baseline and F2. Mean length of remission (abstinence) at baseline among participants who sustained remission at F1 was three and a half years (40.8 months) compared to 15 months for those who reported substance use between baseline and F1 (F = 23.67, p <..001). Participants who reported past year substance use at F2 had a mean of 10 months of abstinence at F1, compared to over four years (52 months) among those who reported no substance use between F1 and F2 (F = 63.09, p <..001). A similar pattern of results emerged with respect to difference between participants who did and did not sustained remission for the full two years between baseline and F2.
3.1.3 Life satisfaction and motivation
Life satisfaction was relatively high throughout the study. Change in life satisfaction at both follow-ups were at the answer level corresponding to 'life has gotten a little better.” Motivation level was steady over the study period, corresponding to the `agree' answer point.
3.2 Hypotheses testing
3.2.1 Does life satisfaction prospectively predict remission?
Bivariate associations among the key domains under study are presented in Table 3. Overall life satisfaction at baseline was significantly associated with subsequent abstinence - i.e., with sustaining abstinence in the year ending at F1, at F2, and over the two years between baseline and F2. In logistic regressions, controlling for baseline length of remission, life satisfaction significantly predicted sustained remission a year later, at F1 (Exp(B) = 1.17, p<.05, CI 95% = 1.01 -1.32), and continuous remission for two years assessed at F2 (Exp(B) = 1.18, p <.05, CI 95% = 1.03 -1.35). Linear regression findings with baseline life satisfaction as the predictor and duration of abstinence at F1 and again at F2 as outcomes also yielded significant results.
Table 3.
Bivariate associations among remission, quality of life satisfaction and motivation for remission: Baseline, one- and two-year follow-ups (N = 289)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | ||||||||||||
| 1. Remission duration | 1.0 | .16** | -.05 | .22*** | .14* | -.02 | .28*** | .21*** | .14* | -.03 | .30*** | .33*** |
| 2. QOL satisfaction | 1.0 | .12* | .35*** | .20*** | .02 | .20*** | .18** | .09 | .09 | .19*** | .22*** | |
| 3. Commitment to abstinence | 1.0 | .08 | .06 | .41*** | .23*** | .06 | .10 | .37*** | .09 | .17* | ||
| One-year follow-up | ||||||||||||
| 4. QOL satisfaction | 1.0 | .58*** | -.10 | .40*** | .36*** | .30*** | .01 | 34*** | .36*** | |||
| 5. Change in satisfaction | 1.0 | .03 | .36*** | .30*** | .26*** | .04 | .32*** | .31*** | ||||
| 6. Commitment to abstinence | 1.0 | .-.03 | -.04 | .02 | .50*** | -.03 | .20*** | |||||
| 7. Remission | 1.0 | .30*** | .32** | .03 | .57*** | .83*** | ||||||
| Two-year follow-up | ||||||||||||
| 8. QOL satisfaction | 1.0 | .63*** | -.10 | .40*** | .41*** | |||||||
| 9. Change in satisfaction | 1.0 | .04 | .40*** | .36*** | ||||||||
| 10. Commitment to abstinence | 1.0 | .01 | .07 | |||||||||
| 11. Remission | 1.0 | .80*** | ||||||||||
| 12. Remission (no use since baseline) | 1.0 |
p<.05
p<.01
p<.001
†p <.1 [trend]; all correlations are two-tailed.
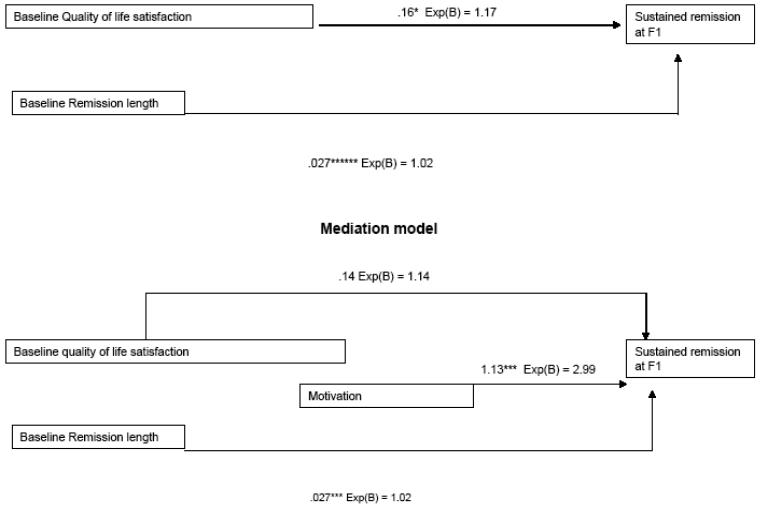
3.2.2 Does motivation mediate the association between life satisfaction and subsequent remission?
In bivariate associations (Table 3) baseline QOL satisfaction was positively associated with motivation measured concurrently; BL motivation was also significantly associated with past year remission at F1 and with past two years remission at F2; as a stricter test, we also examined the association between BL motivation and subsequent remission controlling for BL life satisfaction (not shown in Table 3); the partial correlation coefficient was significant for F1 remission (r = .21, p =.000) and for two year remission at F2 (r = .15, p =.01). Having established that QOL satisfaction significantly predicts remission, that motivation, the hypothesized mediator, predicts remission independently of QOL satisfaction, and that QOL satisfaction predicts motivation, analyses were conducted to test the mediation hypothesis. Logistic regression results with F1 remission as the dependent variable are graphically represented in Figure 1. The analyses controlled for baseline length of abstinence, a known predictor of subsequent abstinence. The figure shows that baseline life satisfaction is significantly associated with greater odds of sustained remission at F1 (Exp(B) = 1.17, p<.05, CI 95% = 1.01 -1.32) and that when baseline motivation is entered in the analyses, the association between QOL satisfaction and subsequent remission weakens (p = .058) and baseline motivation significantly increases the odds of sustained remission at F1 (Exp(B) = 2.99, p<.001, CI 95% = 1.69 - 5.68). Including motivation in the regression equation predicting F1 remission reduced the beta estimating the effect of QOL satisfaction from .16 (p < .05) to .14 (ns), indicating that motivation mediated about 13% of the influence of QOL satisfaction on F1 remission. However, the indirect effect of QOL satisfaction on subsequent remission via motivation did not reach statistical significance according to the Sobel test (Z = .24, p>.05). Similar patterns resulted when the analyses were repeated with past two years remission at F2 as the dependent variable (not shown in Figure1) - baseline QOL satisfaction predicted past two years remission at F2 (Exp(B) = 1.18, p<.01, CI 95% = 1.04 - 1.35), that association weakened but remained statistically significant when BL motivation was entered in the analyses (Exp(B) = 1.17, p <.05), and baseline motivation was significantly associated with greater likelihood of F2 remission (Exp(B) = 2.3, p<.001, CI 95% = 1.29 - 4.17). Taken together, findings lend partial support to the study hypotheses that QOL satisfaction prospectively predicts subsequent remission and that this association is partially mediated by motivational processes.
figure 1.
Quality of life satifaction as predictor of subsequent remission
4. Discussion
This exploratory study set out to examine the association between overall quality of life satisfaction and subsequent remission from SUD. We hypothesized that the predictive role of QOL satisfaction on subsequent remission would be mediated by motivational processes. Findings partially supported the hypotheses in this large sample of inner city participants with long and severe histories of dependence to “hard drugs” (crack and heroin). One of the key benefits of mediational analyses is that they help specify the processes through which important health outcomes occur (Finney & Moos, 1995). Motivation has long been recognized as critical to behavior change processes. Attaining and maintaining abstinence from drugs and alcohol, especially in the context of severe dependence, is a challenging process. Successfully remitted individuals report that to stay in recovery, `you have to want it' (Laudet & White, 2004). Recovery is most often experienced as an ongoing process (e.g., Burman, 2003; Flynn et al., 2003) that requires consistent work and focus. Staying motivated to do this work is therefore critical. Present findings indicate that controlling for duration for baseline abstinence, a strong predictor of subsequent remission status, greater levels of overall QOL satisfaction are associated with enhanced likelihood of remaining in remission (abstinent) one and two years later. This association is partially mediated by motivation. These findings suggest that having satisfying life conditions (`a better life') may represent something valued that could be lost if substance use resumes and therefore acts as a deterrent to returning to substance misuse by “raising the price” of doing so. Thus QOL satisfaction may play a critical role in longitudinal remission processes - enhancing the likelihood of sustained remission as shown here, but also conversely, possibly increasing vulnerability to relapse if QOL satisfaction decreases, regardless of the causes of this decrease- be it substance use, depression or external events such as an accident or illness, stress, bereavement, or job loss to name only a few.
As discussed earlier, the addiction field has thus far neglected to recognize the importance of life quality in remission processes; this is in stark contrast with other biomedical fields where several thousands QOL studies are published annually bearing on a wide range of chronic and acute physical and mental `conditions' and population subgroups. There are, in all likelihood, multiple reasons for this. Among them may be the fact that a large number of substance misusers are members of socially and economically disenfranchised minority subgroups who do not have a `voice' with service providers, insurers and other stakeholders. In clinical practice (and research) in biomedical fields, patients have come to expect that quality of life issues taken into account when discussing alternative therapeutic regimens and other clinical interventions (e.g, Lev et al., 2004). In contrast, substance misuse has until recently been regarded and addressed as a social ill; the clinical outcomes deemed critical may have been determined at least as much by society's concerns as by the needs of the individuals being treated. To date, treatment and research have focused mostly on symptom reduction (i.e., substance use) outcomes. This is understandable and probably reflects the expectations of stakeholders groups (e.g., service payers, the general public) who are most likely to assess the effectiveness of treatment in terms of substance misuse and related threats to public health and safety (i.e., crime and infectious disease transmission). However, addressing these symptoms only is unlikely to serve well either the service clients themselves or other stakeholders. Rather, present findings suggest that fostering opportunities for improved functioning and satisfaction in key areas (psychosocial, education and work, physical and mental health, drug-free leisure activities, living context), in addition to reducing substance use, may significantly enhance the likelihood of sustained remission and thus constitute the best investment of taxpayer dollars in the long run. This is consistent with recommendations recently made by McLellan and colleagues (2005) who wrote “Typically, the immediate goal of reducing alcohol and drug use is necessary but rarely sufficient for the achievement of the longer-term goals of improved personal health and social function and reduced threats to public health and safety—i.e. recovery” (p. 448 - emphasis added).
The ultimate goal of clinical practice is to improve patients' lives. When addressing substance use disorders that are regarded as chronic and where for many, multiple episodes of professional treatment appear to be required for remission to be attained (e.g., Dennis et al., 2005), present findings suggesting that QOL satisfaction may help foster remission emphasize the need to broaden the clinical goal to functioning outcomes that contribute to enhance life satisfaction rather than solely reducing impairments. Correspondingly, researchers should broaden the scope of evaluation outcome domains to include standardized quality of life measures as part of their instrument battery (for discussion, see Cisler et al., 2005). On a broader level, these recommendations suggest that the addiction field needs to make a paradigmatic shift from the traditional pathology-focused model of evaluating interventions by assessing disease-specific outcomes, to one that incorporates or is complemented by outcomes emphasizing positive functioning and the cumulative development of “recovery capital” (Granfield & Cloud, 2001; Laudet et al., 2006). As previously noted, most other biomedical fields have gradually achieved this shift and now embrace measures of life expectancy and QOL as bona fide outcome domains; the addiction field is gradually moving in that direction (e.g, Venner et al., 2006). A final implication of our findings is the potential value of post-treatment recovery support services (e.g., Scott et al., 2005) that are strength-based, focus on the enhancement of broad areas of life functioning and are consistent with the `process' experience of recovery that unfolds over time. The ability of such professionally-directed or peer-based services to foster and sustain remission and corresponding benefits to the individual by increasing quality of life warrants focused attention.
Researchers rarely address specifically the ethical issue of collecting data among individuals who may not directly benefit from participating in our studies. Procedures such as informed consent partially address the issue in stating the risk and benefits of participation for the individual and for society. The current study is unique in a number of ways: we interviewed participants yearly at four time points (an unusually long follow-up period) and participants were media recruited from the community (in contrast with most research where participants are recruited in treatment programs). Therefore we were particularly interested in learning of participants' experiences in this project as we planned to conduct studies with a similar design in the future. We developed the study instruments in collaboration with persons in recovery and emphasized throughout the project that we were interested in participants' experiences, `good or bad.' Our follow-up rate (90% of the surviving cohort at the two-year follow-up) is encouraging. We also conducted a three-year follow-up interview where we asked a series of questions about overall experience with the study including personal usefulness of participation and level of interest in participating in similar studies in the future. The preponderance of participants reported benefiting from taking part in the study (e.g. “It kept me aware of what's going on and how far I've gotten” - 82% said participation was “very useful”, 15% `somewhat useful' - other options: `not at all' and not really useful') and 93% said they would “definitely” be interested in participating in a similar study in the future (other options: “not at all” and “may be interested”). These findings suggest that long-term research among community-based persons in recovery from substance misuse is feasible and may even benefit the individuals themselves by providing a forum where to reflect on past experiences, in addition to contributing greatly to empirical knowledge that can aid in guiding clinical intervention, training and funding decisions.
4.1 Limitations
In addition to focusing on a important yet neglected topic -the role of quality of life in addiction recovery, -the study has a number of strengths including a relatively large sample of members of a population that remains under-investigated (persons in recovery), a long-term follow-up with repeated measurements and excellent retention rates, and the assessment of continuous abstinence rather than the typical practice of asking about “past 30 or 90 days prior to the follow-up interview.” This is the first large scale study designed to explore the prospective role of quality of life satisfaction and mediating processes on SUD remission among illicit-drug dependent persons. As such, it represents an important first step in a potentially critical yet neglected area. As in most exploratory studies, several limitations must be taken into consideration in interpreting findings. First, we used a single-item, global assessment of life satisfaction. The study was conducted to examine the role on long-term remission of domains previously identified as predictors of short-term abstinence (e.g., 12-step affiliation, social supports, motivation); QOL had not been identified among hypothesized predictors of stable remission because of the dearth of published findings in the area especially in the early 2000's when the instruments were being developed (note that the bulk of the QOL research in the addiction field discussed. here has been published very recently). Qualitative analyses identified quality of life satisfaction as critical to sustaining remission and led us to examine the issue in quantitative analyses. The questionnaire protocol included a single item measure used in the WHOQOL that we used in this study. While global assessments can be reliable indicators of how a person feels (US Department of Health and Human Services, 2000) and are useful prognostic clinical indicators (e.g, Reid et al., 2006), they are of limited value. Perhaps most importantly, they do not speak to the multidimensionality of QOL - i.e., to specific areas of functioning that have been identified as critical by QOL researchers (physical, social, emotional, living environment) but rather provide a global rating of how satisfied the individual feels with his/her life. Future studies should use more comprehensive (multidimensional) standardized measures of QOL such as the SF-12 or SF-36 or preferably the WHOQOL-BREF to be able to compare findings across subpopulations and over time in individual functioning areas.
A second limitation concerns the study sample; participants were members of urban, typically underserved minorities and characterized by a long and severe history of poly-substance use. Findings may not apply to members of other groups, such as persons with lower problem severity, individuals whose primary dependence is to alcohol or individuals who had high levels of pre-recovery resources (job, family, education, support system) and/or whose QOL was not as severely affected by substance use as is typically the case in severely dependent populations. Finally, the study design using one-year follow-up intervals may not be well-suited to examine some change processes. It is likely that the association between life satisfaction and motivation is proximal rather than distal. In bivariate associations, we obtained significant findings between QOL satisfaction and motivation measured concurrently but the association between QOL satisfaction at a given time and motivation a year later was not significant; however, present findings whereby QOL satisfaction appears to influence remission status emphasize the need to elucidate the association, including the role of specific functioning QOL domains on sustaining remission. Future studies should plan the timing of follow-up assessments to be more sensitive to the associations among QOL, motivation and substance use to elucidate the question further.
4.2 Conclusions
Maintaining remission from drug and alcohol dependence is a multi-determined, complex process that remains poorly understood. Our findings suggest that QOL satisfaction, a domain that has been all but neglected in the addictions field, may play a critical role in sustaining remission. These findings, taken together with results from a small empirical body of work showing that substance use influences quality of life, suggest that the relationship between QOL satisfaction and substance use is likely to be reciprocal rather than unidirectional (i.e., changes in substance use affecting quality of life). More research is needed to elucidate these complex processes toward guiding clinical practice, program development and the allocation of scare heath services resources. We plan to continue investigating these critical issues and hope that this study encourages others to do so as well.
Acknowledgements
This work was supported in part by NIDA Grant R01 DA14409 and by a grant from the Peter McManus Charitable Trust to the first author to whom correspondence should be directed.
The authors gratefully acknowledges the contribution of the men and women who shared their experiences, strength and hope with our staff for this project.
Footnotes
We note that studies by “rational addiction” researchers and theorists challenge the prevalent belief that substance misuse carries only negative consequences; for example, for the active user, substance misuse may be experienced as positive at the time in the short-term (e.g., Vuchinich & Heather, 2003). Indeed, some substance misusers report positive effects of drug or alcohol use, mostly short-term consequences: such as feeling self-confident and more competent, becoming more sociable and being able to cope with mental complaints, e.g. reducing anxiety (e.g., Rudolf & Priebe, 2002). This study focuses on elucidating remission processes and is conducted among individuals who have come to the conclusion that for them, the consequences of substance misuse are negative so that they seek to maintain remission.
An anonymous reviewer suggested mention be made of the possible iatrogenic effects of professional SUD treatment. For example, Moos (2005) reviewed relevant studies and found that between 7% and 15% of patients who participate in psychosocial treatment for substance use disorders may be worse off subsequent to treatment than before. Moos concluded that safety standards and monitoring procedures are needed to identify such occurrences and that researchers should strive to elucidate the specific causes of iatrogenic effects as well as identify strategies to counteract any such effects.
Sample text of recruiting ad: “Have you successfully overcome a drug problem? NDRI is interested in interviewing anyone in NYC who used to have a serious problem with drugs and is no longer using. Your experiences can provide valuable information to help people with similar problems. Confidentiality is strictly maintained. Participants compensated for time. We do not provide treatment. Call Pathways toll free (800) xxx-xxxx”
This study is a naturalistic investigation of the role of psychosocial factors on long-term recovery, we wanted to be able to assess the role of baseline community-related factors on subsequent outcome.
Alcohol, cannabis, heroin, street or illegal Methadone (to get high), other opiates/Analgesics (e.g., morphine, codeine), downers or depressants (e.g., sedatives, barbiturates, or tranquilizers), crack, non-crack cocaine, methamphetamine or other amphetamines/stimulants, PCP or other hallucinogens, inhalants/Solvents (Glue, gasoline), ecstasy, any other drug including over-the-counter.
11.5% for cocaine, 2.3% for opiates, none for THC or methamphetamines..
References
- Aaronson NK. Quality of life research in cancer clinical trials: A need for common rules and language. Oncology. 1990;4(5):59–66. [PubMed] [Google Scholar]
- Aaronson NK. Methodologic issues in assessing the quality of life of cancer patients. Cancer. 1991;67(Suppl No 3):844–850. doi: 10.1002/1097-0142(19910201)67:3+<844::aid-cncr2820671416>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Allison J. Behavioral economics. Praeger Publishers; New York: 1983. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;(51):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bickel WK, DeGrandpre RJ. Basic psychological science speaks to drug policy: Drug cost and competing reinforcement. In: Bickel WK, DeGrandpre RJ, editors. Drug policy and human nature: Psychological perspectives on the control, prevention and treatment of illicit drug use. Plenum Press; New York: 1996. pp. 31–52. [Google Scholar]
- Bickel WK, Hughes JR, DeGrandpre RJ, Higgins ST, Rizzuto P. Behavioral economics of drug self-administration. IV. The effects of response requirement on the consumption of and interaction between concurrently available coffee and cigarettes. Psychopharmacology (Berl) 1992;107(23):211–6. doi: 10.1007/BF02245139. [DOI] [PubMed] [Google Scholar]
- Bizzarri J, Rucci P, Vallotta A, Girelli M, Scandolari A, Zerbetto E, Sbrana A, Lagher C, Ellantonio E. Dual diagnosis and quality of life in patients in treatment for opioid dependence. Subst Use Misuse. 2005;40(12):1765–76. doi: 10.1080/10826080500260800. [DOI] [PubMed] [Google Scholar]
- Blomqvist J. Recovery with and without treatment: A comparison of resolutions of alcohol and drug problems. Addiction Research and Theory. 2002;10(2):119–158. [Google Scholar]
- Bonomi AE, Patrick DL, Bushnell DM, Martin M. Validation of the United States' version of the World Health Organization Quality of Life (WHOQOL) instrument. J Clin Epidemiol. 2000;53(1):13–7. doi: 10.1016/s0895-4356(99)00123-7. [DOI] [PubMed] [Google Scholar]
- Brecht ML, Anglin MD, Woodward JA, Bonett DG. Conditional factors of maturing out: Personal resources and preaddiction sociopathy. The International Journal of the Addictions. 1987;21(1):55–69. doi: 10.3109/10826088709027413. [DOI] [PubMed] [Google Scholar]
- Breslow Health Measurement in the Third Era of Health. Am J of Public Health. 2006;96(1):17–19. doi: 10.2105/AJPH.2004.055970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burman S. The challenge of sobriety: Natural recovery without treatment and self-help programs. Journal of Substance Abuse. 1997;9:41–61. doi: 10.1016/s0899-3289(97)90005-5. [DOI] [PubMed] [Google Scholar]
- Burman S. Cognitive Processes: Their influence on varying pathways to recovery. Journal of Social Work Practice in the Addiction. 2003;3(3):21–39. [Google Scholar]
- Cisler RA, Kivlahan DR, Donovan D, Mattson ME. Assessing nondrinking outcomes in combined pharmacotherapy and psychotherapy clinical trials for the treatment of alcohol dependence. J Stud Alcohol Suppl. 2005;(15):110–8. doi: 10.15288/jsas.2005.s15.110. discussion 92-3. [DOI] [PubMed] [Google Scholar]
- Claus R, Mannen K, Schicht W. Treatment career snapshots: Profiles of first treatment and previous treatment clients. Addictive Behaviours. 1999;24:471–479. [PubMed] [Google Scholar]
- Costello RM. Alcoholism treatment and evaluation, II: Collation of Two Year Follow-up studies. International Journal of Addictions. 1975;10:857–867. doi: 10.3109/10826087509027344. [DOI] [PubMed] [Google Scholar]
- da Silva Lima A, Fleck M, Pechansky F, de Boni, Sukop P. Psychometric properties of the World health Organisation quality of life instrument (WHOQoL-BREF) in alcoholic males- a pilot study. Quality of Life Research. 2005;14:473–478. doi: 10.1007/s11136-004-5327-1. [DOI] [PubMed] [Google Scholar]
- Daeppen J, Krieg M, Burnand B, Yersin B. MOS-SF-36 in evaluating health-related quality of life in alcohol dependent patients. American Journal of Alcohol and Drug Abuse. 1998;24:685–694. doi: 10.3109/00952999809019617. [DOI] [PubMed] [Google Scholar]
- DeGrandpre RJ, Bickel WK, Higgins ST, Hughes JR. A behavioral economic analysis of concurrently available money and cigarettes. J Exp Anal Behav. 1994;61(2):191–201. doi: 10.1901/jeab.1994.61-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Scott C, Funk R, Foss M. The duration and correlates of addiction and treatment careers. Journal of Substance Abuse Treatment. 2005;28(Suppl 1):51–62. doi: 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Donovan D, Mattson M, Cisler R, Longabaugh R, Zweben A. Quality of life as an outcome measurement in alcoholism treatment research. Journal of Studies on Alcohol. 2005;(Supplement July 15):119–139. doi: 10.15288/jsas.2005.s15.119. [DOI] [PubMed] [Google Scholar]
- Fallowfield L. The quality of life: the missing measurement in healthcare. Souvenir press; London: 1990. [Google Scholar]
- Fassino S, Abbate Daga G, Delsedime N, Rogna L, Boggio S. Quality of life and personality disorders in heroin abusers. Drug and Alcohol Dependence. 2004;76:73–80. doi: 10.1016/j.drugalcdep.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Finney JW, Moos RH. Entering treatment for alcohol abuse: A stress and coping model. Addiction. 1995;90:1223–1240. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- Finney JW, Moyer A, Swearingen CE. Outcome variables and their assessment in alcohol treatment studies. Alcsm Clin. and Experimental research. 2003;27:1671–1679. doi: 10.1097/01.ALC.0000091236.14003.E1. [DOI] [PubMed] [Google Scholar]
- Fiorentine R, Hillhouse M. Drug treatment and 12-step program participation: The additive effects of integrated recovery activities. Journal of Substance Abuse Treatment. 2000;18(1):65–74. doi: 10.1016/s0740-5472(99)00020-3. [DOI] [PubMed] [Google Scholar]
- Flynn P, Joe G, Broome K, Simpson D, Brown B. Looking back on cocaine dependence: Reasons for recovery. American Journal on Addictions. 2003;12:398–411. [PubMed] [Google Scholar]
- Foster JH, Marshall EJ, Peters TJ. Comparison of the Quality of Life of Cancer Patients and Alcohol Dependents. Quality of Life Research. 1997;6:646. [Google Scholar]
- Foster JH, Marshall EJ, Peters TJ. Predictors of relapse to heavy drinking in alcohol dependent subjects following alcohol detoxification-the role of quality of life measures, ethnicity, social class, cigarettes and drug use. Addiction Biology. 1998;3:333–343. doi: 10.1080/13556219872146. [DOI] [PubMed] [Google Scholar]
- Foster JH, Powell JE, Marshall EJ, Peters TJ. Quality of Life in Alcohol Dependent Subjects - A Review. Quality of Life Research. 1999;8:255–261. doi: 10.1023/a:1008802711478. [DOI] [PubMed] [Google Scholar]
- Foster JH, Marshall EJ, Peters TJ. Quality of Life measures and outcome in alcohol dependent men and women. Alcohol. 2000a;22:45–52. doi: 10.1016/s0741-8329(00)00102-6. [DOI] [PubMed] [Google Scholar]
- Foster JH, Marshall EJ, Peters TJ. Application of a Quality of Life measure, the Life Situation Survey (LSS) to alcohol dependent subjects in relapse and remission. Alcoholism Clinical and Experimental Research. 2000b;24:1687–1192. [PubMed] [Google Scholar]
- Granfield R, Cloud W. Social context and “natural recovery”: The role of social capital in the resolution of drug-associated problems. Substance Use and Misuse. 2001;36:1543–1570. doi: 10.1081/ja-100106963. [DOI] [PubMed] [Google Scholar]
- Günther O, Roick C, Angermeyer M, K¨onig H. The EQ-5D in alcohol dependent patients: Relationships among health-related quality of life, psychopathology and social functioning, Drug and Alcohol Dependence. 2006. doi:10.1016/j.drugalcdep.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Havassy B, Arns P. Relationship of cocaine and other substance dependence to well-being of high-risk psychiatric patients. Psychiatric Services. 1998;49:935–940. doi: 10.1176/ps.49.7.935. [DOI] [PubMed] [Google Scholar]
- Havassy B, Wasserman D, Hall S. Research Monograph # 135. National Institute on Drug Abuse; Rockville, MD: 1993. Relapse to cocaine use: conceptual issues in cocaine treatment: Research & clinical perspectives. [PubMed] [Google Scholar]
- Hodgins D, El-Guebaly N. Natural and treatment assisted recovery from gambling problems: A comparison of resolved and active gamblers. Addiction. 2000;95(5):777–789. doi: 10.1046/j.1360-0443.2000.95577713.x. [DOI] [PubMed] [Google Scholar]
- Hoffmann N, Miller N. Perspectives of effective treatment for alcohol and drug disorders. Psychiatric Clinics of America. 1993;16:127–140. [PubMed] [Google Scholar]
- Holcomb WR, Parker JC, Leong GB. Outcomes of inpatients treated on a VA psychiatric unit and a substance abuse treatment unit. Psychiat. Serv. 1997;48:699–704. doi: 10.1176/ps.48.5.699. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Spitzer RL, Williams JBW, Linzer M, DeGruy F, Kroenke K, Brody D, Hahn S. Psychiatric comorbidity, health status, and functional impairment associated with alcohol abuse and dependence in primary care patients: Findings of the PRIME MD-1000 study. J. Cons. Clin. Psychol. 1995;63:133–140. doi: 10.1037//0022-006x.63.1.133. [DOI] [PubMed] [Google Scholar]
- Kelly J, Stout R, Zywiak W, Schneider E. A 3-Year Study of Addiction Mutual-help Group Participation Following Intensive Outpatient Treatment. Alcoholism: Clinical and Experimental Research. 2006;30:1381–1392. doi: 10.1111/j.1530-0277.2006.00165.x. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. In: Gilbert DT, Fiske ST, Lindzey G, editors. The Handbook of Social Psychology. 4th Ed Vol. 1. McGraw Hill; Boston, MA: 1998. pp. 233–265. [Google Scholar]
- Kraemer KL, Maisto SA, Conigliaro J, McNeil M, Gordon AJ, Kelley ME. Decreased alcohol consumption in outpatient drinkers is associated with improved quality of life and fewer alcohol-related consequences. J. Gen. Intern. Med. 2002;17:382–386. doi: 10.1046/j.1525-1497.2002.10613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A, White W. Recovery Capital as Prospective Predictor of Sustained Recovery, Life satisfaction and Stress among former poly-substance users. Substance use and Misuse. 2008;43:27–54. doi: 10.1080/10826080701681473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A, Storey G. A comparison of the recovery experience in the US and Australia: Toward identifying `universal' and culture-specific processes. Poster presented at the International NIDA Research Forum; Scottsdale, AZ. June.2006. [Google Scholar]
- Laudet A, Morgen K, White W. The role of Social Supports, Spirituality, Religiousness, Life Meaning and Affiliation with 12-step Fellowships in Quality of Life Satisfaction among Individuals in Recovery from Alcohol and Drug Use, Alc. Treatment Quarterly. 2006;24():33–74. doi: 10.1300/J020v24n01_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet A, White W, Morgen K. What does recovery mean to you? Definition, goals, and experiences from the recovering community. 133rd Annual Meeting of the APHA; Philadelphia. December 2005. [Google Scholar]
- Laudet A, White W. The role of spirituality, faith and life meaning in the addiction recovery process. 28th Congress of the World Federation for Mental Health (WFMH); Cairo, Egypt. 2005, September. [Google Scholar]
- Laudet A, White W. An exploration of relapse patterns among former poly-substance users. Presented at the 132nd Annual Meeting of the Amer.; Public Health Association, Washington DC. 2004. [Google Scholar]
- Lev EL, Eller LS, Gejerman G, et al. Quality of life of men treated with brachytherapies for prostate cancer. Health Qual Life Outcomes. 2004;2:28. doi: 10.1186/1477-7525-2-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lis CG, Gupta D, Granick J, Grutsch JF. Can patient satisfaction with quality of life predict survival in advancedcolorectal cancer? Support Care Cancer. 2006;14(11):1104–10. doi: 10.1007/s00520-006-0100-3. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Longabaugh R, Beattie M. The relationship between abstinence for one year following pretreatment assessment and alcohol use and other functioning at two years in individuals presenting for alcohol treatment. J Stud Alcohol. 2002;63(4):397–403. doi: 10.15288/jsa.2002.63.397. [DOI] [PubMed] [Google Scholar]
- McLellan A, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinatti H, et al. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100(4):447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos B. Protective resources and long-term recovery from alcohol use disorders. Durg and Alcohol Dependence. 2007;86(1):46–54. doi: 10.1016/j.drugalcdep.2006.04.015. [DOI] [PubMed] [Google Scholar]
- Moos RH. Iatrogenic effects of psychosocial interventions for substance use disorders: prevalence, predictors, prevention. Addiction. 2005;100:595–604. doi: 10.1111/j.1360-0443.2005.01073.x. [DOI] [PubMed] [Google Scholar]
- Moos RH, Finney JW, Cronkite RC. Alcoholism Treatment: Context. Process. And Outcome. Oxford University Press; New York: 1990. [Google Scholar]
- Morgan TJ, Morgenstern J, Blanchard KA, Labouvie E, Bux DA. Health-related quality of life for adults participating in outpatient substance abuse treatment. Am J Addict. 2003;12(3):198–210. [PubMed] [Google Scholar]
- Morgenstern J, Kahler C, Frey R, Labouvie E. Modeling therapeutic responses to 12-step treatment: Optimal responders, non-responders, and partial responders. Journal of Substance Abuse. 1996;8:45–59. doi: 10.1016/s0899-3289(96)90079-6. 1996. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, McCrady BS. Cognitive Processes and Change in Disease-Model Treatment. In: McCrady B, Miller WR, editors. Research on Alcoholics Anonymous, Opportunities and Alternatives. Alcohol Research Documentation, Inc., Rutgers University; New Brunswick, NJ: 1993. pp. 153–166. [Google Scholar]
- Patrick D, Erickson P. Assessing health-related quality of life for clinical decision making. In: Walker SR, Rosser RM, editors. Quality of life: Assessment and applications. MTP Press Ltd.; Lancaster, England: 1988. pp. 9–13. [Google Scholar]
- Perrotta C, Kraemer K, Maisto S, Conigliaro J, McNeil M, Kelly M. Impact of alcohol consumption on quality of life in outpatient problem drinkers. J. Gen. Intern. Med. 1999;14:63A. doi: 10.1046/j.1525-1497.2002.10613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters TJ, Foster JH. In: Quality of Life in Alcohol-Misusing Subjects in Alcohol and Health. Agarwal, Saitz, editors. Marcel Dekker; New York: 2001. p. 12. [Google Scholar]
- Powell J, Crome IB. Quality of Life (QoL) treatment outcome instruments in alcohol misusers demonstrating the effect of treatment? Addict. Biol. 1999;4:240–241. [Google Scholar]
- Préau M, Protopopescu C, Spire B, Sobel A, Dellamonica P, Moatti JP, Carrieri MP. Drug and Alcohol Dependence. 2006. Health related quality of life among both current and former injection drug users who are HIV-infected. (2006) doi:10.1016/j.drugalcdep.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Puigdollers E, Domingo-Salvany A, Brugal MT, Torrens M, Alvaros J, Castillo C, Magri N, Martin S, Vasquez JM. Characteristics of heroin addicts entering methadone maintenance treatment: quality of life and gender. Subst. Use Misuse. 2004;39(9):1353–1368. doi: 10.1081/ja-120039392. [DOI] [PubMed] [Google Scholar]
- Ried LD, Tueth MJ, Handberg E, Nyanteh H. Validating a self-report measure of global subjective well-being to predict adverse clinical outcomes. Quality of Life Research. 2006;15(4):675–86. doi: 10.1007/s11136-005-3515-2. [DOI] [PubMed] [Google Scholar]
- Rippeth J. Factors influencing health-related quality of life in alcoholics and stimulant abusers. Dissertation Abstracts International: Section B: The Sciences & engineering. 1997;58(Sept 3B):1544. [Google Scholar]
- Romeis JC, Waterman B, Scherrer JF, Goldberg J, Eisen SA, Health AC, Bucholz KK, Slutske WS, Lyons MJ, Tsuang MT, True WR. The impact of sociodemographics, comorbidity and symptom recency on health-related quality of life in alcoholics. Journal of Studies on Alcohol. 1999;60(5):653–662. doi: 10.15288/jsa.1999.60.653. [DOI] [PubMed] [Google Scholar]
- Rudolf H, Priebe S. Subjective quality of life and depressive symptoms in women with alcoholism during detoxification treatment. Drug Alcohol Dependence. 2002;66(1):71–6. doi: 10.1016/s0376-8716(01)00183-1. [DOI] [PubMed] [Google Scholar]
- Rudolf H, Watts J. Quality of life in substance abuse and dependency. International Review of Psychiatr. 2002;14:190–197. [Google Scholar]
- Rumpf H, Bischof G, Hapke U, meyer C, John U. Studies on natural recovery from alcohol dependence: sample selection by media solicitation? Addiction. 2000;95(5):765–775. doi: 10.1046/j.1360-0443.2000.95576512.x. [DOI] [PubMed] [Google Scholar]
- Russo J, Roy-Byrne P, Jaffe C, Ries R, Dagadakis C, Avery D. Psychiatric status, quality of life, and level of care as predictors of outcomes of acute inpatient treatment. Psychiatr Serv. 1997;48:1427–1434. doi: 10.1176/ps.48.11.1427. [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML, Foss MA. Utilizing Recovery Management Checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug Alcohol Dependence. 2005;78(3):325–38. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, et al. The Mini International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Broome KM. A national 5-year follow-up of treatment outcomes for cocaine dependence. Archives of General Psychiatry. 2002;59:538–544. doi: 10.1001/archpsyc.59.6.538. [DOI] [PubMed] [Google Scholar]
- Skevington SM, Lotfy M, O'Connell K. The World Health Organization's WHOQOL-BREF quality of life assessment:psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13(2):299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- Smith JA, Hughes ICT, Budd RJ. Non-compliance with anti-psychotic depot medication: Users views on advantages and disadvantages. Journal of Mental Health. (U.K.) 1999;8(3):287–296. [Google Scholar]
- Smith K, Larson M. Quality of life assessments by adult substance abusers receiving publicly funded treatment in Massachusetts. American Journal of Drug and Alcohol Abuse. 2003;29(2):323–335. doi: 10.1081/ada-120020517. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. Jossey-Bass; San Francisco: 1982. pp. 290–312. [Google Scholar]
- Sobell L, Ellingstad T, Sobell M. Natural recovery from alcohol and drug problems: methodological review of the research with suggestions for future directions. Addiction. 2000;95(5):749–764. doi: 10.1046/j.1360-0443.2000.95574911.x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JBW, deGruy FV, Brody D, Davies M. Health-related quality of life in primary care patients with mental disorders: results from the PRIME MD-1000 study. JAMA. 1995;274:1511–1517. [PubMed] [Google Scholar]
- Stein MD, Mulvey KP, Plough A, Samet JH. The functioning and well being of persons who seek treatment for drug and alcohol use. J. Subst. Abuse. 1998;10:75–84. doi: 10.1016/s0899-3289(99)80142-4. [DOI] [PubMed] [Google Scholar]
- Szabo S. The World Health Organization Quality of Life Assessment Instrument. In: Spiker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2nd edition Lippincott-Paven; Philadelphia, PA: 1996. pp. 355–362. [Google Scholar]
- Testa MA, Simonson DC. Assessment of quality-of-life outcomes. New Eng. J. Med. 1996;334:835–840. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- Timko C, Debenedetti A, Billow R. Intensive referral to 12-Step self-help groups and 6-month substance use disorder outcomes. Addiction. 2006;101(5):678–88. doi: 10.1111/j.1360-0443.2006.01391.x. [DOI] [PubMed] [Google Scholar]
- Toneatto T, Sobell LC, Sobell MB, Rubel E. Natural recovery from cocaine dependence. Psychology of Addictive Behaviors. 1999;13(4):259–268. [Google Scholar]
- U.S. Department of Health and Human Services . Understanding and Improving Health and Objectives for Improving Health. 2nd ed. 2 vols. U.S. Government Printing Office; Washington, DC: Nov, 2000. Healthy People 2010. [Google Scholar]
- U.S. Department of Health and Human Services: Food and Drug Administration Guidance for Industry Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. U.S. Department of Health and Human Services author. 2006 doi: 10.1186/1477-7525-4-79. accessed at http://www.fda.gov/cder/guidance/index.htm. [DOI] [PMC free article] [PubMed]
- United Nations Office of Drug Control and Crime Prevention . World Drug Report. Oxford University Press; Oxford New York: 2000. accessed April 12, 2006 at http://www.unodc.org/pdf/world_drug_report_2000/report_2001-01-22_1.pdf. [Google Scholar]
- Vaillant G. The Natural History of Alcoholism Revisited. Harvard University Press; Cambridge, MA: 19831995. [Google Scholar]
- Venner KL, Matzger H, Forcehimes AA, Moos RH, Feldstein SW, Willenbring ML, Weisner C. Course of recovery from alcoholism. Alcohol Clin Exp Res. 2006;30(6):1079–90. doi: 10.1111/j.1530-0277.2006.00121.x. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villeneuve P, Challacombe L, Strike C, Myers T, Fischer B, Shore R, Hopkins S, Millson P. Change in health-related quality of life of opiate users in low-threshold methadone programs. Journal of Substance Use. 2006;11(2):137–149. [Google Scholar]
- Volk R, Cantor S, Steinbauer J, Cass A. Alcohol use disorders, consumption patterns, and health-related quality of life of primary care patients. Alcoholism Clinical and Experimental Research. 1997;21:899–905. [PubMed] [Google Scholar]
- Vorma H, Naukkarinen H, Sarna S, Kuoppasalmi K. Symptom severity and quality of life after benzodiazepine withdrawal treatment in participants with complicated dependence. Addict Behav. 2004;29(6):1059–65. doi: 10.1016/j.addbeh.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Vuchinich RE, Heather N, editors. Choice, Behavioral Economics and Addiction. Pergamon; New York: 2003. [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. New England Medical Center Health Institute; Boston, MA: 1993. [Google Scholar]
- The WHOQOL Group The World Health Organization Quality of Life Assessment (WHOQOL): Position paper from the World Health Organization. Social Science and Medicine. 1995;41(10):1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- WHOQOL Group Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28:551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Basic Documents. 35th ed. WHO; Geneva, Switzerland: 1985. [Google Scholar]
- Youssef RM, Moubarak II, Kamel MI. Factors affecting the quality of life of hypertensive patients. Eastern Mediterranean Health Journal. 2005;11(12):109–118. [PubMed] [Google Scholar]