Abstract
Purpose
To present a case of peripheral infiltrative keratitis mimicking infectious keratitis on the flap margin and limbus, which appeared on the first postoperative day after the laser in situ keratomileusis (LASIK).
Methods
A 36-year-old woman who underwent uneventful bilateral simultaneous LASIK developed multiple round infiltrate along the flap margin reaching to limbus from the 11 o'clock to 6 o'clock area in both eyes.
Results
The flap was lifted and irrigation was performed with antibiotics. but infiltration seemed to appear again. The infiltrate was more concentrated at the periphery and was extended to the limbus. Direct smear and culture for bacteria and fungus were negative. Topical prednisolone acetate 1% eye drops was added, infiltrative condition was resolved.
Conclusions
LASIK induced peripheral infiltrative keratitis, in which infectious origin was ruled out, is reported
Keywords: DLK, LASIK, topical corticosteroid
Laser in situ keratomileusis (LASIK) has been shown to be an effective treatment for myopia, hyperopia, and astigmatism. As with any surgical procedure, complications can arise that threaten best spectacle-corrected visual acuity. When a diffuse infiltrate enclosed in the interface appears within 2 to 6 days postoperatively without anterior chamber reaction or epithelial defect, it can be diagnosed as diffuse lamellar keratitis (DLK). It emanates intermittently or in clumps throughout a broad area.1
Possible etiologies are included oil, wax, metallic fragments, silicates, bacterial endotoxins, epithelial defects, and laser / contaminant interaction, a contaminant in the lamellar interface introduced at the time of surgery. It showed response to topical steroids. Treatment, however, largely rests on the different stages of DLK.1-3
This is a report of multiple round peripheral infiltrate developed following the flap margin and limbus mimicking infectious keratitis on the first day after LASIK.
Case Report
A 36 year old woman went through routine bilateral simultaneous LASIK on March 23, 2006, for a refractive error of -4.00 D sphere -1.00 D cylinder axis 180 in both eyes with the NAVEX SYSTEM (Nidek Advanced Visual Excimer, NIDEK, USA) in local eye clinic. The whole operation progressed unremarkably without signs of bleeding from the flap edge before or after the surgery.
0.5% Moxifloxacin eye drops and 0.1% fluorometholone eye drops were prescribed 4 times a day. The day after the operation, the patient complained watering, severe photophobia, bilateral redness and whitish changes in the cornea.
As the infiltration grew worse, she was transferred to our hospital's department of ophthalmology. Visual acuity came out 20/25 in both eyes with correction.
Both Intraocular pressure is 11 mmHg by non-contact tonometry. Through a slit-lamp examination, both lids appeared normal without any indications of meibomitis or blepharitis. Mild congestion was found in the conjunctiva. Numerous round infiltrate could be seen along the flap margin (Fig. 1), diffused from the 11 o'clock to 6 o'clock direction.
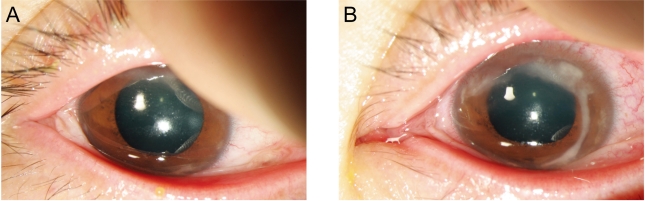
Fig. 1.
White multiple corneal infiltrates in the periphery along the lamellar flap margin were noted in the first day after LASIK on both eyes (A: right eye, B: left eye)
The infiltrate was more concentrated at the periphery and faded out centrally while the center of the flap was left unaffected. There were no distinguishable epithelial defects. Also, the anterior chamber showed neither cells nor flare. Because the shape of the infiltration was diffusely round, we could not rule out the infection.
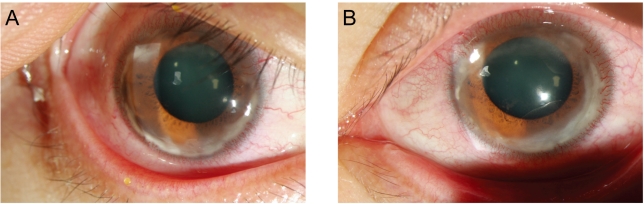
During flap lifting and antibiotics irrigation, bacterial and fungal culture were obtained. 0.5% moxifloxacin eye drops and fortified vancomycin 50 mg/ml eye drops were given in each eye for 4 times a day. The infiltration seemed to improve, but on the 2nd day after operation, the infiltrate had developed to involve the flap edge from the 2 o'clock to 11 o'clock direction and also involved the limbus in both eyes. Direct smear and culture for bacteria and fungus were negative. Blood tests were performed for human immunodeficiency disease, hepatitis B surface antigen, hepatitis C antigen, rheumatoid factor, and C-reactive protein, but they all turned out negative also. But the infiltrate did not advance centrally, alone with topical antibiotics, its margin appearing clear (Fig. 2). We started administrating 1% topical prednisolone acetate eye drops every 3 hours.
Fig. 2.
Peripheral flap infiltration was progressed into the limbus in second day after flap lifting with antibiotics irrigation. (A: right eye, B: left eye)
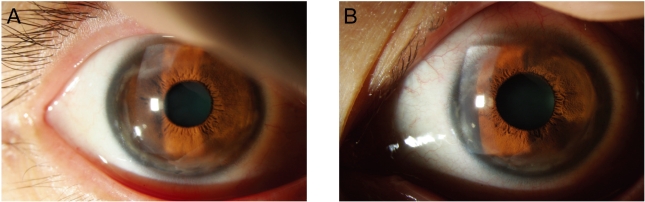
On the 6th day after operation, the symptoms showed improvement. The infiltrate in the peripheral area decreased significantly, with the fogginess in the interface also diminished remarkably (Fig. 3). Refraction was -0.25 -2.00×10 in the right eye and -1.25 -1.75×150 in the left eye, the visual acuity improved to 20/20. The IOP in both eyes was 10 mmHg.
Fig. 3.
After adding topical prednisolone acetate along with topical antibiotics, decreased infiltration was the lamellar flap and the corneal limbus 6th day after flap lifting with antibiotics irrigation. (A: right eye, B: left eye)
Discussion
Corneal infiltrations after LASIK are relatively uncommon complications. Because corneal infiltrates represent a nonspecific accumulation of inflammatory cells, several possible causes should be considered. Probably the most important complication is infectious keratitis. An infection after LASIK can be rapidly progressive and potentially vision threatening. If an infection has been ruled out, other etiologies can be entertained.
Generally, peripheral corneal infiltrates can be associated with several etiologies, including blepharitis-related, staphylococcus hypersensitivity infiltrates, Terrien's marginal degeneration, Mooren's ulcer, and peripheral ulcerative keratitis associated with autoimmune or collagen vascular disease.4,5
Singhal et al.6 reported one case in likeliness with our case. Young man developed a thick band of infiltrate between the flap margin and limbus extending from 2 o'clock to 9 o'clock in both eyes. The infiltrate was more concentrated at the periphery and faded centrally and progressed diffusely into the interface leading to typical diffuse lamellar keratitis. The infiltrate responded to topical prednisolone acetate 1% eye drops
Ambrosio et al.7 Lahner et al.5 also reported respectively 2 cases of sterile peripheral infiltration after LASIK which showed good response to topical steroid therapy.
The patient concerned in the present case showed no clinical or serologic signs of connective tissue disorder. There was no evidence of meibomitis or blepharitis, and there was no history of Staphylococcal marginal keratitis as well. Although the surgery was routine, she displayed acute symptoms one day after the operation. The infiltrate appeared in multiple round shapes following the flap margin without any epithelial defects. These findings could not rule out the possibility of infectious keratitis. The patient had been using 0.5% moxifloxacin eye drops before she was asked for our consult. The patient did not seem to respond to the antibiotic so we immediately performed flap lifting and antibiotics irrigation but infiltration soon appeared again and progressed to the limbus outside of flap. We added topical steroids into the treatment starting from the second day after the operation and the patient showed a response.
Several points suggest sterile infiltrate: the absence of conjunctival injection or ciliary flush, the absence of epithelial defects or surrounding edema, the absence of anterior chamber reaction, and the response to steroids. The infiltrate showed response to intensive topical corticosteroid therapy, which cleared completely except for a mild but negligible regression in the both eyes in the last follow-up.
As in the case of the other study, we also achieved good results in our case with topical steroid therapy.
From the fact that the symptoms improved after additional steroid therapy, immune reaction or inflammatory reaction seems to be the most acceptable cause, but infection could not be ruled out completely because wide-range antibiotics were continuously being used.
Although the exact mechanism of this complication remains unclear, recognition of this entity and its differentiation from infectious keratitis is essential to the management of these patients. Appropriate and early management usually results in a rapid disappearance of the infiltrates without affecting the final outcome. Nevertheless, it is important to maintain a high degree of suspicion for infectious keratitis because the management is very different and the potential outcome much worse if the keratitis is due to an infectious etiology. One could perform a culture and treat these cases empirically as infectious for the first 24 to 36 hours. If the cultures come back negative, one could start topical and systemic steroids.8
In conclusion, to look out the confusion between infectious keratitis and sterile keratitis, this case can be addressed as LASIK-induced bilateral peripheral infiltrative keratitis.
Footnotes
* This study was presented as a poster at the 96th annual meeting of the Korean Ophthalmologic Society in November, 2006.
References
- 1.Linebarger EJ, Hardten DR, Lindstrom RL. Diffuse lamellar keratitis : Diagnosis and management. J Cataract Refract Surg. 2000;26:1072–1077. doi: 10.1016/s0886-3350(00)00468-5. [DOI] [PubMed] [Google Scholar]
- 2.Linebarger EJ, Hardten DR, Lindstrom RL. Diffuse lamellar keratitis: identification and management. Int Ophthalmol Clin. 2000;40:77–86. doi: 10.1097/00004397-200007000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Blustein JN, Hitchins VM, Woo EK. Diffuse lamellar keratitis, endotoxin, and ophthalmic sponges. J Cataract Refract Surg. 2004;30:2027–2028. doi: 10.1016/j.jcrs.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Lifshitz T, Levy J, Mahler O, Levinger S. Peripheral sterile corneal infiltrates after refractive surgery. J Cataract Refract Surg. 2005;31:1392–1395. doi: 10.1016/j.jcrs.2004.12.057. [DOI] [PubMed] [Google Scholar]
- 5.Lahner WJ, Hardten DR, Lindstrom RL. Peripheral keratitis following laser in situ keratomileusis. J Refract Surg. 2003;19:671–675. doi: 10.3928/1081-597X-20031101-10. [DOI] [PubMed] [Google Scholar]
- 6.Singhal S, Sridhar MS, Garg P. Bilateral peripheral infiltrative keratitis after LASIK. J Refract Surg. 2005;21:402–404. doi: 10.3928/1081-597X-20050701-18. [DOI] [PubMed] [Google Scholar]
- 7.Ambrosio R, Periman LM, Netto MV, Wilson SE. Bilateral marginal sterile infiltrates and diffuse lamellar keratitis after laser in situ keratomileusis. J Refract Surg. 2003;19:154–158. doi: 10.3928/1081-597X-20030301-11. [DOI] [PubMed] [Google Scholar]
- 8.Holzer MP, Solomon KD, Vroman DT, et al. Diffuse lamellar keratitis: evaluation of etiology, histopathologic findings, and clinical implications in an experimental animal model. J Cataract Refract Surg. 2003;29:542–549. doi: 10.1016/s0886-3350(02)01691-7. [DOI] [PubMed] [Google Scholar]