Abstract
Purpose
To compare the effect of early versus late intravitreal injection of triamcinolone in patients with macular edema due to branch retinal vein occlusion (BRVO).
Methods
Twenty eyes of 20 patients with macular edema from BRVO, including 10 with duration after onset of ≤3 months and 10 with duration of >3 months, were treated using a single intravitreal triamcinolone injection (4 mg/0.1 ml). Best-corrected visual acuity and foveal thickness by optical coherence tomography were measured 1, 3, and 6 months post-injection.
Results
In patients that received treatment after a disease duration of ≤3 months, visual acuity and foveal thickness significantly improved from baseline over 6 months of follow-up. However, in those with a duration of > 3 months, improvements in visual acuity and foveal thickness, though apparent at 1 month, were not maintained at 3 and 6 months post-triamcinolone.
Conclusions
Intravitreal triamcinolone is more effective in patients with BRVO who are treated earlier.
Keywords: Branch retinal vein occlusion, Intravitreal triamcinolone, Macular edema
A few studies on patients with branch retinal vein occlusion (BRVO) have suggested that intravitreal corticosteroid can reduce macular edema and increase visual acuity.1-3 However, these studies did not evaluate the effectiveness of triamcinolone with respect to the timing of the intravitreal injection. In addition, follow-up periods were inadequate or patients who had undergone multiple injections of intravitreal triamcinolone or combined treatment with laser photocoagulation were included. The purpose of this study was to directly compare the effect of an early versus a late intravitreal triamcinolone as a primary treatment for macular edema due to BRVO.
Patients and Methods
This study had been performed according to the Declaration of Helsinki of the World Medical Association. This retrospective study included 20 eyes of 20 patients who received a single injection of intravitreal triamcinolone (4 mg/0.1 ml) as an only treatment for macular edema from BRVO between July 2004 and June 2005, and who had a post-injection follow-up time of >6 months. Of these 20 patients, 10 had a disease duration from onset to injection of ≤3 months and the other 10 had a duration of >3 months. We designated these as the early treatment and late treatment groups, respectively. Best-corrected Snellen visual acuity (converted to logarithms of the minimal angle of resolution [logMAR]), intraocular pressure (IOP) by Goldmann applanation tonometry, and foveal thickness on optical coherence tomography (Stratus OCT™; Carl Zeiss Meditec Inc., Dublin, CA, USA) were measured at baseline and at 1, 3, and 6 months post-injection. The difference between baseline and postoperative measurements in logMAR visual acuity and foveal thickness were compared in each group, using the two-tailed Student's t test and the chi-square test. Statistical significance was accepted at p<0.05.
The protocol was approved by the Institutional Review Board of Seoul National University Hospital, Seoul, Korea, and informed consent was obtained from the patients.
Results
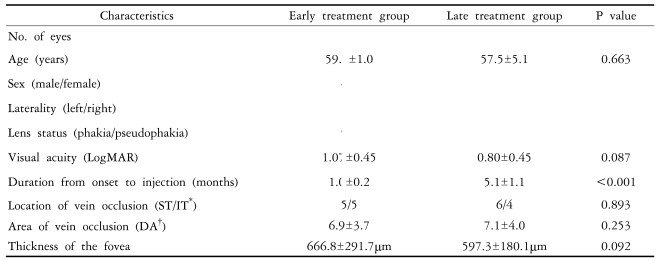
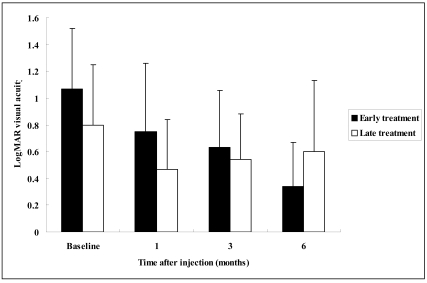
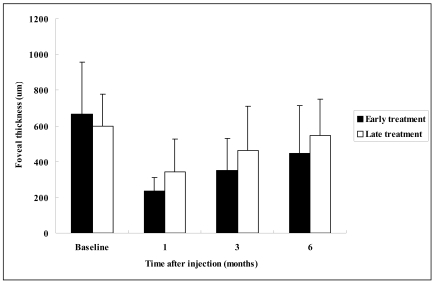
Patient demographics and characteristics of BRVO are shown in Table 1; no statistically significant differences were found between the two groups. In the early treatment group, mean visual acuity significantly improved from a baseline of 1.07±0.45 logMAR units to 0.74±0.51 (p=0.021) at 1 month, 0.63±0.43 (p=0.012) at 3 months, and 0.34±0.33 (p=0.005) at 6 months post-injection. In this group, mean foveal thickness was 666.8±291.7 µm at baseline, and significantly reduced to 233.8±77.2 µm (p<0.001) at 1 month, 351.1±180.8 µm (p=0.026) at 3 months, and 446.2±266.6 µm (p=0.029) at 6 months. However, in the late treatment group, though mean visual acuity significantly improved from baseline 0.80±0.45 to 0.47±0.37 (p=0.039) at 1 month, it did not further improve at 3 months (0.54±0.34, p=0.080) or 6 months (0.60±0.53, p=0.226). Similarly, mean foveal thickness decreased significantly from baseline 597.3±180.1µm to 344.0±183.3 µm (p=0.030) at 1 month, but results did not significantly improve at 3 months (464.0±246.8 µm, p=0.594) or 6 months (545.1±204.6 µm, p=0.952). Comparisons of mean visual acuity and foveal thickness in the two groups are shown in figures 1 and 2, respectively. One patient in the early treatment group and two in the late treatment group experienced an elevated IOP during follow-up, and one in the late treatment group required trabeculectomy.
Table 1.
Patient demographics and characteristics of the retinal vein occlusion in the early and late treatment groups
* ST : Superotemporal, IT : Inferotemporal.
† DA : Disc area.
Fig. 1.
LogMAR visual acuity results in the early and late treatment groups. A significant sustained improvement was evident in the early treatment group throughout the subsequent 6-month follow-up, but in the late treatment group, the initial improvement at 1 month was not sustained at 3 and 6 months.
Fig. 2.
Foveal thickness by optical coherence tomography in the early and late treatment groups. A significant improvement was observed in the early treatment group throughout the 6-month follow-up, but the improvement observed at 1month was not further sustained in the late treatment group.
Discussion
The macular edema due to BRVO may ultimately disappear because the collateral circulation usually bypasses the blockage over a period of 6 to 24 months after BRVO onset.4 However, vision may not improve due to retinal pigment epithelium atrophy, even after the disappearance of macular edema, and thus, an early reduction in macular edema is important if vision is to be restored. Triamcinolone might control macular edema while the collateral circulation is established in BRVO,5 and result in a visual improvement. Our study shows that patients with macular edema from BRVO responded to intravitreal injection of triamcinolone with regard to foveal thickness and visual acuity with the group of a short disease duration showing a greater response. Patients with a disease duration of >3 months did not sustain foveal thickness and visual acuity improvements through a 6-month follow-up, whereas those with a duration of ≤3 months showed continued improvements through follow-up.
The present study has the major limitation that follow-up was conducted over only 6 months. It is possible that the effect of triamcinolone would reduce in the early treatment group with time, because foveal thickness of both groups was increasing after the post-injection one month, while visual acuity was still improving in the early treatment group at the post-injection 6 months.
Thus, further investigation with a longer follow-up is necessary to better ascertain the long-term effect of intravitreal triamcinolone on the degree of macular edema and visual outcome with respect to disease duration. In conclusion, we find that intravitreal triamcinolone is more effective over a 6 month period in BRVO patients who are treated earlier.
References
- 1.Hayashi K, Hayashi H. Intravitreal versus retrobulbar injections of triamcinolone for macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2005;139:972–982. doi: 10.1016/j.ajo.2004.12.087. [DOI] [PubMed] [Google Scholar]
- 2.Chen SD, Lochhead J, Patel CK, Frith P. Intravitreal triamcinolone acetonide for ischaemic macular oedema caused by branch retinal vein occlusion. Br J Ophthalmol. 2004;88:154–155. doi: 10.1136/bjo.88.1.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yepremyan M, Wertz FD, Tivnan T, et al. Early treatment of cystoid macular edema secondary to branch retinal vein occlusion with intravitreal triamcinolone acetonide. Ophthalmic Surg Lasers Imaging. 2005;36:30–36. [PubMed] [Google Scholar]
- 4.Christoffersen NL, Larsen M. Pathophysiology and hemodynamics of branch retinal vein occlusion. Ophthalmology. 1999;106:2054–2062. doi: 10.1016/S0161-6420(99)90483-9. [DOI] [PubMed] [Google Scholar]
- 5.Degenring RF, Kamppeter B, Kreissig I, Jonas JB. Morphological and functional changes after intravitreal triamcinolone acetonide for retinal vein occlusion. Acta Ophthalmol Scand. 2003;81:399–401. doi: 10.1034/j.1600-0420.2003.00084.x. [DOI] [PubMed] [Google Scholar]