Abstract
We report the clinical course of photodynamic therapy (PDT) in a patient with drusenoid pigment epithelium detachment (PED). A patient with drusenoid PED underwent PDT follow-up was carried out at one week, one month, three months, six months and one year after treatment. Fundus exam, optical coherence tomography (OCT) and fluorescein angiography were performed. After the PDT, drusen and PED were gradually diminished over one year. However, pure serous PED eventually developed at the same location of the drusenoid PED. The results of the PDT, on drusenoid PED, were initially effective, but not completely successful. Therefore, PDT may be considered as an alternative treatment option for drusenoid PED.
Keywords: Drusenoid pigment epithelium detachment, Photodynamic therapy
A variety of different types of pigment epithelium detachment (PED) have been identified in the medical literature. These types of PED can be classified as fibrovascular PED, serous detachment of RPE, hemorrhagic detachment of RPE and drusenoid RPE detachment.1 Verteporfin photodynamic therapy (PDT) has been used to safely reduce the risk of loss of vision in patients with choroidal neovascularization (CNV) in age-related macular degeneration.2 We performed PDT on a patient with drusenoid PED and here report the clinical course.
Case Report
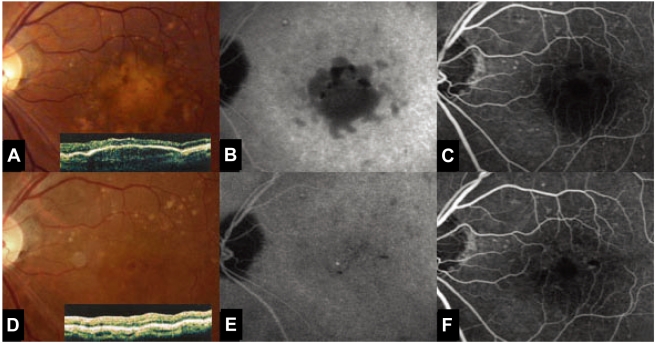
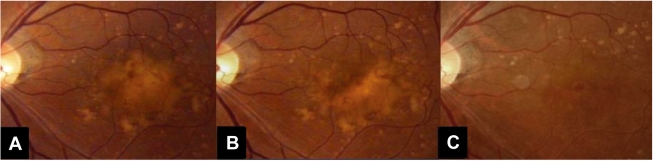
A 68-year-old man presented with decreased visual acuity in his left eye for several months. His corrected vision in the left eye was 20/40. There was no abnormality observed in the anterior segment. On fundus examination of the left eye, one disk diameter sized PED, with diffuse coalesced soft drusen was noted at the macula. At the first examination, fluorescein angiography revealed delayed, regular hyperfluorescence without leakage and the OCT showed multiple pigment epithelium detachments. There was no evidence of CNV (Fig. 1A, B, C). PDT was performed at the PED site and around 1,000 µm2. Fifteen days after PDT, the corrected vision for the left eye was 20/40. On the fundus examination, there was no interval change (Fig. 2A). Five months after PDT, the fundus examination showed a decreased size of the soft drusen (Fig. 2B). Ten months after PDT, the corrected vision of the left eye was improved to 20/25. On fundus examination and OCT, the number of soft drusen was markedly decreased (Fig. 2C). ICG showed that the drusenoid PED diminished in size (Fig. 1D, E, F).
Fig. 1.
(A, B, C) Fundus photography and optical coherence tomography (OCT) at the first examination showed multiple pigment epithelium detachments. Fluorescein angiography revealed delayed, regular hyperfluorescence without leakage. There was no evidence of choroidal neovascularization (CNV). (D, E, F) Ten months after photodynamic therapy (PDT), fundus photography, OCT and ICG showed that the drusenoid PED diminished in size.
Fig. 2.
(A) Fifteen days after PDT, there was no interval change, on the fundus examination. (B) Five months after PDT, the fundus examination showed a decreased size of the soft drusen. (C) Ten months after PDT, the corrected vision of the left eye was improved to 20/25. On fundus examination, the number of soft drusen was markedly decreased.
Discussion
Drusenoid PED has been distinguished from other types of injury by its better prognosis. This avascular PED typically develops slowly and causes minimal complaints of blurred vision. The natural history usually follows a progression to persistent drusenoid RPE detachment, geographic atrophy and neovascularisation.3 The effect of PDT on drusenoid PED has not been confirmed, but the effect of a grid laser on drusen has been reported.4
The effects of PDT can be divided into the photochemical effect of verteporfin and the effect of the 689 nm nonthermal laser itself. As previously reported, vertiporfin has a very broad absorption spectrum, but only the far-red peak at 688-691 nm is typically used in clinical practice. A beam of red laser light (689 nm diode laser) is applied to the retina via a slit lamp irradiating a spot of about 1 mm in diameter, with light intensity of 600 mW/cm2, for 83 seconds, resulting in a total radiant exposure of 50 J/ cm.2,5 Closure of abnormal (leaking) blood vessels occurs for approximately 6-12 weeks in most patients.
We suspect that direct laser treatment of drusen may accelerate their removal by phagocytes, and that RPE proliferation induced by laser photocoagulation might reduce the amount of debris per cell and enhance the phagocytic capacity of the RPE.6 Indirect effects of the laser may alter the characteristics of the lipids which cause Bruch's membrane impairment, so that the soft drusen material escapes.7
In our case, PDT was effective for reducing the drusenoid PED. The effect was observed ten months after the PDT we thought the effect was caused by the laser, not the verteporfin. The efficacy of 689 nm diode laser on drusenoid PED has not been reported; the long term efficacy of the conventional PDT treatment is not known. Further studies are therefore warranted.
References
- 1.Ryan SJ. Retina. 4th ed. Vol. 2. Philadelphia: Elsevier mosby; 2006. p. 1083. [Google Scholar]
- 2.Photodynamic therapy of subfovealchoroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials-TAP report. Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study Group. Arch Ophthalmol. 1999;117:1329–1345. [PubMed] [Google Scholar]
- 3.Roquet W, Roudot-Thoraval F, Coscas G, Soubrane G. Clinical features of drusenoid pigment epithelial detachment in age related macular degeneration. Br J Ophthalmol. 2004;88:638–642. doi: 10.1136/bjo.2003.017632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho AC, Maguire MG, Yoken J, et al. Laser-induced drusen reduction improves visual function at 1 year. Ophthalmology. 1999;106:1367–1374. doi: 10.1016/s0161-6420(99)00735-6. [DOI] [PubMed] [Google Scholar]
- 5.Verteporfin In Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization-verteporfin in photodynamic therapy report 2. Am J Ophthalmol. 2001;131:541–560. doi: 10.1016/s0002-9394(01)00967-9. [DOI] [PubMed] [Google Scholar]
- 6.Frennesson C, Nilsson SE. Prophylactic laser treatment in early age related maculopathy reduced the incidence of exudative complications. Br J Ophthalmol. 1998;82:1169–1174. doi: 10.1136/bjo.82.10.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pauleikhoff D, Löffert D, Spital G, et al. Pigment epithelial detachment in the elderly. Clinical differentiation, natural course and pathogenetic implications. Graefe's Arch Clin Exp Ophthalmol. 2002;240:533–538. doi: 10.1007/s00417-002-0505-8. [DOI] [PubMed] [Google Scholar]