Abstract
Purpose
To evaluate the protective effects of epigallocatechin gallate (EGCG) against UV irradiation of cultured human lens epithelial cells.
Methods
We irradiated cultured human lens epithelial cells with a 30-second pulse from a UV lamp with an irradiance of 0.6 mW/cm2. Five minutes and 1 hour after UV irradiation, we administered 0, 5, 10, 15, 25, 50, or 100 uM EGCG. The cell number was measured with a microscopic counting chamber and cell viability was evaluated using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay.
Results
Compared to untreated cells, the total number of cultured human lens epithelial cells was markedly higher after UV irradiation. In a dose-dependent manner, viability was also higher in EGCG-treated cells.
Conclusions
EGCG increased the cell count and cell viability after UV irradiation of cultured human lens epithelial cells, indicating that EGCG can protect lens epithelium against UV damage.
Keywords: Cell viability; Cultured human lens epithelial cells; Epigallocatechin gallate (EGCG); 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay; UV irradiation
INTRODUCTION
Ocular light injury is caused by several mechanisms, in particular, by short wavelength ultraviolet light. Ultraviolet light is divided into three categories: UVC (200-290 nm), UVB (290-320 nm) and UVA (320-400 nm).1 The ultraviolet light between 200 nm and 300 nm is absorbed into the cornea, but ultraviolet light between 300 nm and 400 nm penetrates the cornea and is absorbed into the lens.2,3 The mechanistic cause of cataracts is complicated, but they can arise as a result of systemic diseases like diabetic mellitus, ultraviolet light, heat, hormone abnormalities, and smoking.4-6 Epidemiological reports and experiments indicate that ultraviolet light may be a primary cause of cataracts.4-6 The exact mechanism of UV-induced cataract formation is not fully understood. Cataract formation results from the accumulation of UV-induced DNA damage, changes in membrane transport and permeability, and changes in the biochemistry and physiology of the lens by reactive oxygen species such as hydrogen peroxide (H2O2), superoxide anion (O2-), singlet oxygen (1O2), and hydroxyl radical (HO-).7,8 Flavonoids are a class of natural biological products that have evolved to protect plants from oxidative damage induced by chronic exposure to ultraviolet light.9 Flavonoids have many physiological health benefits, including protection from cardiovascular disease and cancer, and most of these beneficial effects are thought to stem from their potent antioxidant and free radical-scavenging properties, as well as their abilities to modulate many cellular enzyme functions.9 The toxicities of most effective flavonoids are low. These include the dietary flavonoids such as fisetin, luteolin, quercetin, eriodictyol, baicalein, galangin, and EGCG, as well as synthetic flavonoids such as 3, 6-dihydroxy flavonol, and 3, 7-dihydroxy flavonol. (-)-epigallocatechin-3-gallate (EGCG) is the major polyphenolic constituent found in green tea.10,11 Several other polyphenolic compounds, known as catechins, are also found in green tea, though to a lesser degree. In addition to EGCG, the catechins include (-)-epicatechin-3-gallate (ECG), (-)-epigallocatechin (EGC), (-)-epicatechin (EC), and (+)-catechin. More than 50% of the tea catechin mass is composed of EGCG, and a vast body of scientific research suggests that EGCG (and the other catechins) are responsible for the majority of the potential health benefits attributed to green tea consumption.12 However, few studies have assessed the protective effects of EGCG after UV irradiation ofhuman lens epithelial cells.
To evaluate the protective effects of EGCG against UV irradiation of cultured human lens epithelial cells we treated the cells with different concentration of EGCG. Five minutes and 1 hour after irradiation, we measured the effects on cell survival and viability. We choose these time points with future in vivo experiments in mind, in particular those that would evaluate green tea absorption and the protective effects of EGCG on the lens epithelium. Specifically, most people drink green tea indoors from 5 minutes to 1 hour after outdoor UV exposure. After another 24-hour incubation, the total cell count was measured and cell activity was evaluated using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay. The aim of this study was to determine whether EGCG can protect human lens epithelial cells from UV-induced damage, and to develop a new in vivo model of UV protection for human lenses using epigallocatechin gallate (EGCG).
Materials and Methods
1. Cell culture
The human lens epithelial line CRL-1142 (HLE-B3) (ATCC, USA) was used for this study. These cells were cultured in Dulbecco's Modified Eagle's Medium (DMEM) (Sigma, St Louis, MO, USA), supplemented with 10% fetal bovine serum (FBS), 100 U/ml penicillin, 100 u/ml streptomycin, and 25 ug/ml nystatin, and were cultured at 37℃ in humidified atmosphere, containing 5% CO2.
2. Ultraviolet Irradiation
Human lens epithelial cells were irradiated for 30 seconds with an irradiance of 0.6 mW/cm2 after removal of serum-free growth medium. UV irradiance was modulated by adjusting UV lamp (FS-20 T12-UVB, National Biological Corp.) output, which was calibrated with a UV sensor. The UVB spectrum was between 280 nm and 320 nm with peak irradiance at 312 nm. The total UVB exposure volume was 18 mJ/cm2.
3. Experimental Protocol and Groups
Human lens epithelial cells were cultured for 1 day and the experiments were performed on 3 groups: the normal control group, which was not exposed to UV lights (Group I); the second group exposed to UV lights without administration of EGCG (Sigma, St Louis, MO, USA) (Group II); and the third group exposed to UV lights with administration of EGCG (Sigma, St Louis, MO, USA) (Group III). Group III was treated with 5, 10, 15, 25, 50, or 100 µM EGCG (Sigma, St Louis, MO, USA), 5 minutes or 1 hour after UV irradiation.
4. Cell count and MTT assay
24 hours after UV incubation, the cell count was measured using a microscopic counting chamber, and cell viability was evaluated using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay. In this assay, MTT is reduced to purple formazan in the mitochondria of living cells. A solubilization solution is added to dissolve the insoluble purple formazan product into a colored solution. The MTT assay was carried out using a standard protocol, and optical density was measured at 570 nm using a spectrophotometer.
5. Statistical analysis
To increase the reliability of the data, all experiments were repeated 5 times and average values were calculated. SPSS for Windows Version 10.1 was used to compute routine statistics. The data were analyzed for significance using repeated measures two-way ANOVA, followed by a Duncan's multiple range test of post hoc tests, and were expressed as a mean percentage of the control value plus S.E.M. P values < 0.05 were considered significant.
Results
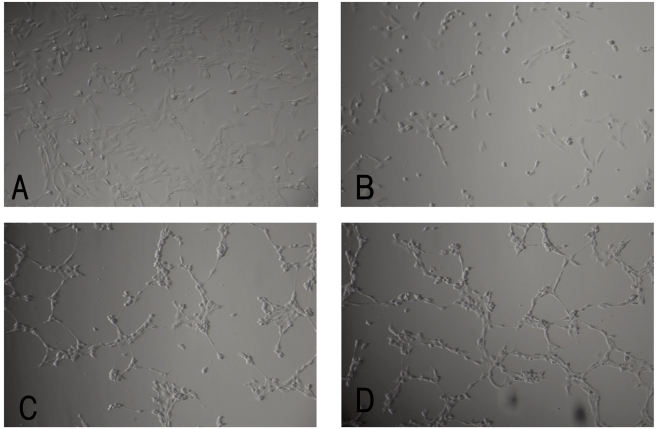
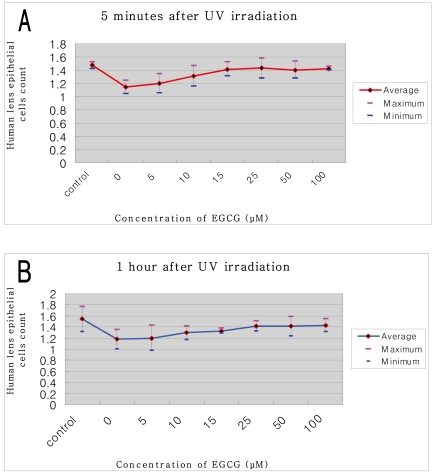
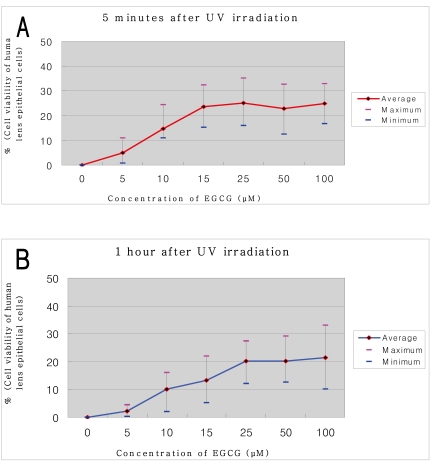
Epigallocatechin gallate (EGCG) protected cultured human lens epithelial cells from oxidative-stress-induced cytotoxicity with excellent efficacy. Compared with unirradiated cells (Fig. 1A), exposure to UV irradiation without administration of EGCG resulted in significant cell loss (Fig. 1B). With administration of 100 µM EGCG, both 5 minutes (Fig. 1C) and 1 hour (Fig. 1D) after UV irradiation, the cell count increased to those seen in unirradiated cells. The cell count of cultured human lens epithelial cells after UV irradiation markedly increased upon EGCG administration (Fig. 2). There was no significant relationship between the time to EGCG administration and cell loss (P=0.719). Cell viability after UV irradiation increased in a dose-dependent manner upon treatment with EGCG, as determined by the MTT assay (Fig. 3). Also, there were significant differences in viability between cells treated with 5 or 10 µM (P=0.000) and 10 or 15 µM EGCG (P=0.000). There was no significant difference between cells treated with 0 or 5 µM EGCG (P=0.233) or between cells treated with 15, 25, 50, or 100 µM EGCG (P=0.166). Compared with untreated cells, viability increased by approximately 24.8% or 21.5% in cells treated with 100 µM of EGCG, after 5 minutes or 1 hour after UV irradiation, respectively. There was no significance between the time to the administration of EGCG and the survival rate of cells (P=0.129).
Fig. 1.
Lens epithelial cell loss after UV irradiation. (A) Control without UV irradiation. (B) After UV irradiation without administration of Epigallocatechin gallate (EGCG). (C) 5 minutes after UV irradiation with administration of 100 µM EGCG. (D) 1 hour after UV irradiation with administration of 100 µM EGCG. The photographs were taken by inverted microscope. (×200)
Fig. 2.
Lens epithelial cell count after UV irradiation. Cell count of cultured human lens epithelial cells after UV irradiation was markedly increased with Epigallocatechin gallate (EGCG) administrationgroup, compared with non- administration group. Control was group without UV irradiation. There was no significant relationship between the time to administration EGCG and the lossof cells (P=0.719). (A) 5 minutes after UV irradiation, (B) 1 hour after UV irradiation.
Fig. 3.
Lens epithelial cell viability after UV irradiation. Cell viability of cultured human lens epithelial cells after UV irradiation was markedly increased with Epigallocatechin gallate (EGCG) administration group and was increased dose-dependent way. Basis (0) was group with UV irradiation without administration of EGCG. There was no significance between the time to administration of EGCG and the survival rate of cells (P=0.129). (A) 5 minutes after UV irradiation, (B) 1 hour after UV irradiation.
Discussion
The exact mechanism of UV-induced cataract formation is not yet fully understood. However UV-induced cataract formation does result from the accumulation of UV-induced DNA damage, changes in membrane transport and permeability, and changes in biochemical and physiology of lens epithelium by reactive oxygen species. Increasing interest in the health benefits of tea has led to the inclusion of tea extracts in dietary supplements and functional foods. While green tea contains a number of bioactive chemicals, it is particularly rich in catechins. Although a number of in vitro and in vivo studies have shown EGCG acts as an antioxidant and anti-apoptotic agent, the actual mechanism of its action as an antioxidant remains unclear.13-17 Importantly, total plasma antioxidant activity has been shown to increase following significant intake of green tea in laboratory studies.18,19 Moreover, an increase in plasma catalase activity and a decrease in nitric oxide levels occurred, suggesting that catechins have both direct antioxidant effects and indirect influences to increase the activity of other antioxidants or enzymes.20 It has been suggested that catechins, like EGCG, elicit antioxidant effects in a number of ways.21 However, few reports have demonstrated the protective effects of EGCG after UV irradiation on human lens epithelium. Therefore, we evaluated the effects of EGCG treatment on human lens epithelial cells after UV-induced damage. We also aimed to develop a new in vitro model of UV protection using epigallocatechin gallate (EGCG) for human lenses. In our study, the total cell count of cultured human lens epithelial cells after UV irradiation markedly increased upon EGCG treatment, compared with untreated cells. Also, cell viability markedly increased in a dose-dependent fashion upon EGCG administion, as determined by the MTT assay.
In conclusion, we have shown that EGCG increases cell count and cell viability after UV irradiation of cultured human lens epithelial cells, indicating the protective effects of EGCG against UV damage in cultured human lens epithelial cells. Future in vivo and in vitro studies examining mitochondria damage, nucleic acid damage, and phagocyte activity after UV exposure of human lens epithelial cells are needed.
Footnotes
This study was supported by grant from 2007 Chosun University Research Fund.
References
- 1.McCarty CA, Taylor HR. Recent developments in vision research: light damage in cataract. Invest Ophthalmol Vis Sci. 1996;37:1720–1723. [PubMed] [Google Scholar]
- 2.Norren DV, Vos JJ. Spectral transmission of the human ocular media. Vision Res. 1974;14:1237–1244. doi: 10.1016/0042-6989(74)90222-3. [DOI] [PubMed] [Google Scholar]
- 3.Margrain TH, Boulton M, Marshall J, et al. Do blue light filters confer protection against age-related macular degeneration. Prog Retin Eye Res. 2004;23:523–531. doi: 10.1016/j.preteyeres.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Worgul BV, Merriam GR, Jr, Medvedovsky C. Cortical cataract development-an expression of primary damage to the lens epithelium. Lens Eye Toxicity Res. 1989;6:559–571. [PubMed] [Google Scholar]
- 5.Taylor HR, West SK, Rosenthal FS, et al. Effect of ultraviolet radiation in cataract formation. N Engl J Med. 1998;319:1429–1433. doi: 10.1056/NEJM198812013192201. [DOI] [PubMed] [Google Scholar]
- 6.Zigman S, Vaughan T. Near-ultraviolet light effects on the lenses and retinas of mice. Invest Ophthalmol Vis Sci. 1974;13:462–465. [PubMed] [Google Scholar]
- 7.Spector A, Garner WH. Hydrogen peroxide and human cataract. Exp Eye Res. 1981;33:673–681. doi: 10.1016/s0014-4835(81)80107-8. [DOI] [PubMed] [Google Scholar]
- 8.Ramachandran S, Morris SM, Devamanoharan P, et al. Radio-isotopic determination of hydrogen peroxide in aqueous humor and urine. Exp Eye Res. 1991;53:503–506. doi: 10.1016/0014-4835(91)90167-d. [DOI] [PubMed] [Google Scholar]
- 9.Middleton E, Kandaswami C, Theoharides TC. The effects of plant flavonoids on mammalian cells: Implicationsfor inflammation, heart disease and cancer. Pharmacol Rev. 2000;52:673–751. [PubMed] [Google Scholar]
- 10.Bettuzzi S, Brausi M, Rizzi F, et al. Chemoprevention of human prostate cancer by oral administration of green tea catechins in volunteers with high-grade prostate intraepithelial neoplasia: a preliminary report from a one-year proof-of-principle study. Cancer Res. 2006;66:1234–1240. doi: 10.1158/0008-5472.CAN-05-1145. [DOI] [PubMed] [Google Scholar]
- 11.Demeule M, Michaud-Levesque J, Annabi B, et al. Green tea catechins as novel antitumor and antiangiogenic compounds. Curr Med Chem Anticancer Agents. 2002;2:441–463. doi: 10.2174/1568011023353930. [DOI] [PubMed] [Google Scholar]
- 12.Nagle DG, Ferreira D, Zhou YD. Epigallocatechin-3-gallate (EGCG): Chemical and biomedical perspectives. Phytochemistry. 2006;67:1849–1855. doi: 10.1016/j.phytochem.2006.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buttemeyer R, Philipp AW, Schlenzka L, et al. Epigallocatechin gallate can significantly decrease free oxygen radicals in the reperfusion injury in vivo. Transplant Proc. 2003;35:3116–3120. doi: 10.1016/j.transproceed.2003.10.055. [DOI] [PubMed] [Google Scholar]
- 14.Morley N, Clifford T, Salter LA, et al. The green tea polyphenol (-)-epigallocatechin gallate and green tea can protect human cellular DNA from ultraviolet and visible radiation-induced damage. Photodermatol Photoimmunol Photomed. 2005;21:15–22. doi: 10.1111/j.1600-0781.2005.00119.x. [DOI] [PubMed] [Google Scholar]
- 15.Nagai K, Jiang MH, Hada J. (-)-Epigallocatechin gallate protects against NO stress-induced neuronal damage after ischemia by acting as an anti-oxidant. Brain Res. 2002;956:319–322. doi: 10.1016/s0006-8993(02)03564-3. [DOI] [PubMed] [Google Scholar]
- 16.Xie D, Liu G, Zhu G, et al. (-)-Epigallocatechin-3-gallate protects cultured spiral ganglion cells from H2O2-induced oxidizing damage. Acta Otolaryngol. 2004;124:464–470. doi: 10.1080/00016480410018278. [DOI] [PubMed] [Google Scholar]
- 17.Mandel S, Weinreb O, Amit T, Youdim MB. Cell signaling pathways in the neuroprotective actions of the green tea polyphenol (-)-epigallocatechin-3-gallate: implications for neurodegenerative diseases. J Neurochem. 2004;88:1555–1569. doi: 10.1046/j.1471-4159.2003.02291.x. [DOI] [PubMed] [Google Scholar]
- 18.Skrzydlewska E, Ostrowska J, Farbiszewski R, Michalak K. Protective effect of green tea against lipid peroxidation in the rat liver, blood serum and the brain. Phytomedicine. 2002;9:232–238. doi: 10.1078/0944-7113-00119. [DOI] [PubMed] [Google Scholar]
- 19.Yokozawa T, Nakagawa T, Kitani K. Antioxidative activity of green tea polyphenol in cholesterol-fed rats. J Agric Food Chem. 2002;50:3549–3552. doi: 10.1021/jf020029h. [DOI] [PubMed] [Google Scholar]
- 20.Negishi H, Xu JW, Ikeda K, et al. Black and green tea polyphenols attenuate blood pressure increases in stroke-prone spontaneously hypertensive rats. J Nutr. 2004;134:38–42. doi: 10.1093/jn/134.1.38. [DOI] [PubMed] [Google Scholar]
- 21.Sutherland BA, Rahman RM, Appleton I. Mechanisms of action of green tea catechins, with a focus on ischemiainduced neurodegeneration. J Nutr Biochem. 2006;17:291–306. doi: 10.1016/j.jnutbio.2005.10.005. [DOI] [PubMed] [Google Scholar]