Abstract
Purpose
To evaluate the relationship between optic disc and retinal nerve fiber layer (RNFL) measurements obtained with the optical coherence tomography (OCT) and the Heidelberg retina topography (HRT) in normal, normal tension glaucoma (NTG), and high tension glaucoma (HTG).
Methods
Normal, NTG and HTG subjects who met inclusion and exclusion criteria were evaluated retrospectively. One hundred seventy eyes of 170 patients (30 normal, 40 NTG, and 100 HTG) were enrolled. Complete ophthalmologic examination, HRT, OCT, and automated perimetry were evaluated.
Results
Disc area, cup area and cup/disc area ratio measured with HRT were significantly different between NTG and HTG (all p<0.05). Mean RNFL thickness measured by OCT with ascanning diameter of 3.4 mm was larger in NTG than HTG (84.97±24.20 µm vs. 73.53±27.17 µm, p=0.037). Four quadrant RNFL thickness measurements were not significantly different between NTG and HTG (all p>0.05). Mean deviation and corrected pattern standard deviation measured by automated perimetry was significantly correlated with mean and inferior RNFL thickness in both NTG and HTG (Pearson's r, p<0.05). Mean RNFL thickness/disc area ratio was significantly larger in HTG than NTG (35.21±18.92 vs. 31.30±10.91, p=0.004).
Conclusions
These findings suggest that optic disc and RNFL damage pattern in NTG may be different from those of HTG.
Keywords: High tension glaucoma, Normal tension glaucoma, Retinal nerve fiber layer
Glaucomatous optic nerve damage may manifest itself not only as a morphological change in the optic nerve head (ONH) but also as a decrease in the thickness of the retinal nerve fiber layer (RNFL).1 Loss of axonal fibers results in the decreased thickness of the RNFL, and this structural change has been found to precede both any morphological changes of the optic nerve head and functional changes in the visual field.2-13 Thus, measuring the RNFL thickness, along with morphological analysis of the ONH lies at the cornerstone of early glaucoma detection.The development of the Heidelberg Retina Topography (HRT, Heidelberg engineering GmbH, Heidelberg, Germany) has made possible an objective three dimensional topographic analysis of the ONH. A more recent development in the optical coherence tomography (OCT Humphrey Systems, Inc., Dublin, California, USA) utilizes a near infra-red beam to provide cross sectional views of the retina with a remarkable resolution of up to 10 µm. However, it has been reported that not only the RNFL thickness but the size of the ONH has great inter-individual and inter-racial variations.14-17 Also, the thickness of the RNFL has been found to be directly proportional to the size of the ONH.18-20 Therefore, clinical correlation between these two variables should aid each other in the diagnosis of early glaucomatous change. Inter-racial comparisons in the thickness of the RNFL, have to date been largely studied between Caucasians and those of African descent. The authors of this study have attempted to compare high tension and normal tension glaucoma patients for any differences in HRT and OCT measurements in a cohort of Korean patients diagnosed with glaucoma.
Materials and Methods
This study involved retrospective comparison analysis of HRT and OCT variables of the right eye of patients diagnosed with high tension glaucoma (HTG) or normal tension glaucoma (NTG) between January, 2001 and May, 2001. Normal controls were also included in this comparison study. The thirty eyes of normal controls were restricted to those without any ocular morbidity, showing neither glaucomatous optic disc changes nor visual field defects, and whose intraocular pressure (IOP) never exceeded 21 mmHg on repeated measurements. The thirty NTG eyes included in this study were defined as those showing both glaucomatous optic disc changes and corresponding visual field defects but who's IOP never exceeded 21 mmHg on repeated measurements. Subsequently, the one hundred eyes enrolled as HTG group included those as stated above for NTG except whose IOP exceeded 21 mmHg prior to or after initiation of therapy and thus diagnosed as primary open angle glaucoma. The restriction of the study to the right eye of each patient for each group was to facilitate statistical analysis. HRT, OCT and visual field exams were all completed on the same day by one examiner for each of the exams.
Exclusion criteria included any other ocular co-morbidity including high myopia, cataracts and diabetic retinopathy that may interfere with the results. A past history of any central nervous system disease that could influence ONH morphology also warranted exclusion.
Visual fields were obtained by Humphrey automated perimetry (Allergan- Humphrey, Inc., San Leandro, USA) central 30-2 program. Obtained visual field indices for statistical analysis included mean deviation (MD), and corrected pattern standard deviation (CPSD). The HRT exam immediately followed the visual field exam by creating a mean topograph from 3 images with image size of 15 degrees. In all subjects the ONH border was drawn just inside the inner boundary of the scleral ring of Elschnig by a single examiner. All ONH measurement variables made by the HRT were calculated from this manually drawn ONH border and an automatically set standard reference plane. The twelve ONH measurement variables calculated by the HRT included disc area, rim area, cup area, cup/disc ratio, cup volume, rim volume, mean cup depth, maximum cup depth, cup shape measure, height variation contour, mean RNFL thickness and RNFL cross sectional area.
OCT examinations were the last to be completed in the series. All globes were internally fixated by asking the examinee to fixate on the built-in flashing light. The peripapillary retina was scanned at diameters of 2.3 mm and 3.4 mm centered on the center of the disc to obtain RNFL thickness measurements. RNFL thickness was measured for each of the 4 quadrants surrounding the disc and a mean value was calculated. In addition, the OCT values for the mean and inferior RNFL thickness from the two glaucomatous groups were divided by nasal RNFL thickness and disc area, in an attempt to compare values between the two groups.
All twelve measurement variables calculated by the HRT and the five measurement variables obtained with the OCT were compared amongst the normal controls, NTG and HTG groups. Between the two glaucoma groups the MD and CPSD obtained from automated perimetric testing were also compared. Comparison between the two glaucoma groups was done with the 3.4 mm scanning diameter values, as this location has previously been reported as showing a significant difference between thetwo glaucoma groups.21,22
Statistical analyses were done with the SPSS/PC program to differentiate between the Pearson correlation test, linear regression test, analysis of variance (ANOVA) and the Student ttest. A p-value of less than 0.05 was set for statistical significance.
Results
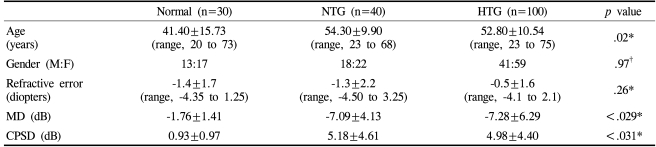
Demographic data shown in Table 1 for each of the three groups show a tendency for the normal control group to have been younger than either of the two glaucomatous groups, but statistically show no significant difference. Gender and refractive error showed no statistical difference amongst the three groups. As expected, MD and CPSD values were significantly higher for the normal control group when compared to the two glaucoma groups.
Table 1.
Patients' demographics
CPSD=corrected pattern standard deviation on visual field; dB=decibels; F=female; HTG=high tension glaucoma M=male; MD=mean deviation on visual field; NTG=normal tension glaucoma; Values given as means±standard deviations; *By analysis of variance; †By Chi-square test.
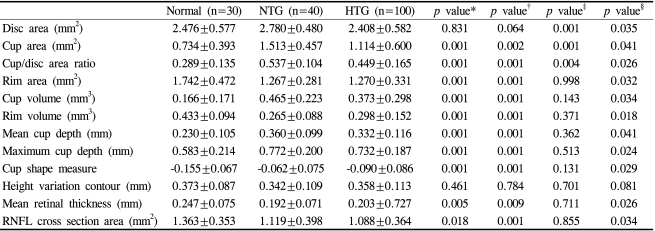
Comparisons of HRT parameters among three study groups were shown in Table 2. According to ANOVA, height variation contour was the only value which was similar among all three study groups. Cup area and cup/disc area ratio had different values in three groups.
Table 2.
HRT parameters in normal, normal tension glaucoma, and high tension glaucoma
HTG=high tension glaucoma; NTG=normal tension glaucoma; RNFL=retinal nerve fiber layer; Values given as means±standard deviations; *Corresponding pairs: normal and NTG, Student t test; †Corresponding pairs: normal and HTG, Student t test; ‡Corresponding pairs: NTG and HTG, Student t test; §Corresponding: normal, NTG, and HTG, analysis of variance.
Disc area was significantly different only between NTG and HTG but not between normal vs. NTG and normal vs. HTG. Rim area, cup volume, rim volume, maximum cup depth, cup shape measure, mean retinal thickness, and RNFL cross section area were different between normals vs. NTG/HTG.
RNFL thickness measurements by OCT with the 3.4 mm and 2.3 mm diameter scan were tabled in Table 3. First of all, according to ANOVA, RNFL thickness of nasal peripapillary quadrant was similar in three groups with both scan diameters. With 3.4 mm scan diameter, mean RNFL thickness showed a significant difference among all three groups. The normal control group showed the thickest RNFL while the HTG group showed the thinnest. Comparison of the four peripapillary quadrants among the three groups showed the normal control group to have the highest RNFL thickness values except for the nasal quadrant when compared against the two glaucoma groups. RNFL thickness for each quadrant between the two glaucoma groups showed no significant difference. For the 2.3 mm diameter scan, although the normal control group showed the highest value of mean RNFL thickness, a difference between the two glaucoma groups was not found. Measurements for the four peripaillary quadrants showed the similar tendency as with the 3.4 mm diameter scan.
Table 3.
Retinal nerve fiber layer thickness measured by OCT in normal, normal tension glaucoma, and high tension glaucoma (µm)
NTG=normal tension glaucoma; HTG=high tension glaucoma; Values given as means±standard deviations; *Corresponding pairs: normal and NTG, Student t test; †Corresponding pairs: normal and HTG, Student t test; ‡Corresponding pairs: NTG and HTG, Student t test; §Corresponding: normal, NTG, and HTG, analysis of variance.
In the normal control group, OCT measurements for mean RNFL thickness and foreach of the peripapillary quadrants except the nasal quadrant significantly correlated with disc from the HRT showed a significant association with mean, superior and temporal quadrant RNFL thickness measurements with the OCT. Among the OCT measurements, the superior RNFL thickness measurement showed the most association with calculated HRT parameters.
For the NTG group, associative analysis between OCT and HRT variables showed the inferior RNFL thickness measurement to be significantly correlated with HRT parameters cup volume, cup/disc ratio, rim area and cup shape measure. Also, the mean RNFL thickness measurement showed significance when associated with rim area and cup shape measure. Two visual field indices MD and CPSD showed significant correlation with mean and inferior quadrant RNFL thickness measurements on OCT. In association with visual field testing, the inferior quadrant RNFL thickness showed a high correlation with MD and CPSD. In addition, the thinner the RNFL was, the further the MD and CPSD fluctuated from the normals.
In the HTG group, HRT parameters associated with mean RNFL thickness were cup area, cup/disc ratio and cup shape measure. Of note, the cup shape measure showed significant association with all RNFL thickness measurements except the nasal quadrant RNFL. Inferior quadrant RNFL thickness showed the most correlations with HRT parameters including cup area, cup/disc ratio, rim area, cup area, rim volume, cup shape measure, mean RNFL thickness and RNFL cross sectional area.
Both MD and CPSD showed correlation with the mean and inferior quadrant RNFL thickness measurements with a higher correlation for the inferior RNFL thickness. The thinner the RNFL the further the MD and CPSD drifted from normal. This trend was consistent for both glaucoma groups.
The two glaucoma groups were compared by taking the mean and inferior quadrant RNFL thickness measurements by OCT, which incidentally showed a significant association with MD and CPSD, and dividing these measurements by the nasal quadrant RNFL thickness and disc area measured and calculated by the HRT and OCT respectively. The ratio of the mean and inferior RNFL thickness to the nasal quadrant RNFL thickness did not show a significant difference between NTG and HTG groups (all p>0.05). The ratio of the mean RNFL thickness to disc area for the two glaucoma groups was 35.21±18.92 for NTG and 31.30±10.91 for HTG, showing a significant difference between the two groups (p=0.004) however the ratio of inferior quadrant RNFL thickness to disc area reached no significant level between the two glaucoma groups (p>0.05).
Discussion
HRT and OCT are relatively recent developments to combat these problems. HRT provides a quantitative value for various parameters by taking three dimensional measurements of the ONH and peripapillary retina. The high reproducibility of HRT has already been reported.23 OCT utilizes a light source in the near infra red spectrum to take tomographic sections of tissue just like a B-scan ultrasonograph, enabling direct measurements of RNFL thickness.
However, RNFL thickness and ONH morphology are known to have wide inter-individual and inter-racial variations.14-17 Tsai et al.14 have reported that the disc area of Oriental people is larger than Caucasians but smaller than people of African descent. They also remarked on the high inter-individual differences. In light of these differences and the fact that the incidence of NTG is reported to be much higher in Asians than Caucasians, the unbiased use of Western data in an attempt at diagnosis and detection of progression of glaucoma can give erroneous results. The compilation of data for Korean people in the analysis of ONH morphology by HRT and the measurements of RNFL thickness by OCT in normal subjects have already been published.24-28 However, comparisons with glaucomatous eyes have not yet been studied. The authors of this study attempted to analyze, compare and find any association in HRT and OCT parameters in normal Korean subjects and those already diagnosed with NTG or HTG.
Quantitative comparisons showed a significantly larger disc area for the NTG group than the HTG group (p=0.001). This was in accord with the results published by Yang et al.25 but contradicted the report by Park.26 Also, average disc area was larger for the NTG group when compared to controls but did not reach a significant level (p=0.064). Cup area showed statistically different values for each of the three groups with NTG having by far the largest area. This was also in contradiction to the report made by Park.26 As in reports made by Fazio29 and Yang26 comparison of rim area showed no difference between the two glaucoma groups but showed a larger area for normal controls as expected. However, previous reports made by Park26 showed larger rim areas for the NTG group, as reports by Caprioli,30 Yamagami,31 and Eid32 postulated smaller rim areas for the NTG group. Caprioli,30 Yamagami,31 and Fazio29 all used ONH stereophotogaphs or the Rodenstock ONH analyzer to compare amongst the groups and thus their methods differed from this present study. However, a recent study by Lester, Mikelberg et al.33 used the HRT to compare one hundred and thirty two HTG patients with fifty NTG patients and found no significant difference in any HRT parameter between the two groups.
In light of the present results, rim area in the two glaucoma groups show a high association with the superiorand the inferior RNFL thickness. The mean and inferior RNFL thickness showed a significant association with cup shape measure. This observation leads to the hypothesis that the change in the mean and the inferior RNFL thickness is more responsible for glaucomatous optic nerve head change than any other quadrant. Unlike in the normal control group, disc area showed no significant correlation with RNFL thickness in the two glaucoma groups, leading to the idea that, a decrease in RNFL thickness in glaucoma does not affect disc size. Also, inferior peripapillary RNFL thickness was the only quadrant to have a significant association with cup/disc ratio in the two glaucoma groups. The association of the mean and inferior peripapillary quadrant RNFL with visual field indices MD and CPSD is worthy of note. The normal ONH is known to have a double-hump pattern with a dual prominence at the superior and inferior borders. This double-hump pattern is known to be preferentially lost with superior and inferior RNFL flattening in glaucomatous eyes.34 However, the present study shows that the peripapillary RNFL thickness to have the most association with glaucomatous visual field changes is the inferior quadrant rather than the superior quadrant, irrespective of the level of IOP.
Previous reports made by Jonas19 and Quigley18 confirm the findings of our study, in that the bigger the disc area, the thicker the mean and inferior RNFL thickness measurements in normal controls. Therefore, the ratio of the mean/inferior RNFL thickness to disc area can be an objective parameter in the two glaucoma groups. This study used in its analysis, the mean RNFL thickness rather than the superior quadrant thickness due to the mean RNFL's association with visual field indices.
In a comparison between the two glaucoma groups, the mean RNFL thickness/disc area ratio showed a significantly lesser value for NTG despite the fact that absolute values for mean RNFL thickness and disc area was larger for NTG. The authors of this study propose that the mean RNFL thickness/disc area ratio can be an aiding factor in distinguishing between the two glaucoma types.
The primary limitation of this study lies in the different number of patients recruited for each comparison group. Namely, the HTG group had a larger number of recruits than either the NTG or the normal control group. This discrepancy in the number of recruits largely resulted from the high cost of the various exams employed in this study, since in the normal control group, OCT and HRT exams were performed only on those patients willing to take on the economic burden and such patients were difficult to find. Secondly, the nature of the present study was retrospective. Subjects were selected for their similarity in glaucoma severity measured by visual field indices. Thus, a comparative analysis between subgroups classified according to graded glaucoma severity was not possible with this study design. A prospective study based on a graded glaucoma severity scale between the two glaucoma groups should be addressed in the future.
The traditional triad of visual field, optic disc cupping, and RNFL defects can now be augmented by the analyses of direct RNFL thickness measurements and ONH morphology through OCT and HRT, respectively. Such augmentation should be able to aid in the early diagnosis and early detection of progression of glaucoma even before signs are evident in the traditional triad. Also, OCT and HRT can aid in the differential diagnosis between NTG and HTG allowing early intervention for the clinician. In this regard, the authors of this study conclude that OCT in conjunction with associated HRT variables, not only acts as an adjunct to the traditional triad of visual field, RNFL photography and ONH morphologic studies, but can also be a most useful tool in research analysis of Korean eyes with glaucoma, such as in the differentiation of NTG and HTG.
References
- 1.Tuulonen A, Airaksinen PJ. Initial glaucomatous optic disc and retinal nerve fiber layer abnormalities and their progression. Am J Ophthalmol. 1991;111:485–490. doi: 10.1016/s0002-9394(14)72385-2. [DOI] [PubMed] [Google Scholar]
- 2.Quigley HA, Katz J, Derick RJ, et al. An evaluation of optic disc and nerve fiber layer examinations in monitoring progression of early glaucoma damage. Ophthalmology. 1992;99:19–28. doi: 10.1016/s0161-6420(92)32018-4. [DOI] [PubMed] [Google Scholar]
- 3.Quigley HA, Addicks EM, Green WR. Optic nerve damage in human glaucoma. III. Quantitative correlation of nerve fiber loss and visual field defect in glaucoma, ischemic neuropathy, papilledema, and toxic neuropathy. Arch Ophthalmol. 1982;100:135–146. doi: 10.1001/archopht.1982.01030030137016. [DOI] [PubMed] [Google Scholar]
- 4.Tuulonen A, Lehtola J, Airaksinen PJ. Nerve fiber layer defects with normal visual fields. Do normal optic disc and normal visual field indicate absence of glaucomatous abnormality? Ophthalmology. 1993;100:587–597. doi: 10.1016/s0161-6420(93)31598-8. [DOI] [PubMed] [Google Scholar]
- 5.Sommer A, Miller NR, Pollack J, et al. The nerve fiber layer in the diagnosis of glaucoma. Arch Ophthalmol. 1977;95:2149–2156. doi: 10.1001/archopht.1977.04450120055003. [DOI] [PubMed] [Google Scholar]
- 6.Quigley HA, Dunkelberger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989;107:453–464. doi: 10.1016/0002-9394(89)90488-1. [DOI] [PubMed] [Google Scholar]
- 7.Sommer A, Katz J, Quigley HA, et al. Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol. 1991;109:77–83. doi: 10.1001/archopht.1991.01080010079037. [DOI] [PubMed] [Google Scholar]
- 8.Airaksinen PJ, Alanko HI. Effect of retinal nerve fiber loss on the optic nerve head configuration in early glaucoma. Greafes Arch Clin Exp Ophthalmol. 1983;220:193–196. doi: 10.1007/BF02186668. [DOI] [PubMed] [Google Scholar]
- 9.Tuulonen A, Airaksinen PJ, Montagna A, Nieminen H. Screening for glaucoma with a non-mydriatic fundus camera. Acta Ophthalmol (Copenh) 1990;68:445–449. doi: 10.1111/j.1755-3768.1990.tb01674.x. [DOI] [PubMed] [Google Scholar]
- 10.Quigley HA, Miller NR, George T. Clinical evaluation of nerve fiber layer atrophy as an indicator of glaucomatous optic nerve damage. Arch Ophthalmol. 1980;98:1564–1571. doi: 10.1001/archopht.1980.01020040416003. [DOI] [PubMed] [Google Scholar]
- 11.Quigley HA, Addicks EM. Quantitative studies of retinal nerve fiber layer defects. Arch Ophthalmol. 1982;100:807–814. doi: 10.1001/archopht.1982.01030030811018. [DOI] [PubMed] [Google Scholar]
- 12.Sommer A, Quigley HA, Robin AL, et al. Evaluation of nerve fiber layer assessment. Arch Ophthalmol. 1984;102:1766–1771. doi: 10.1001/archopht.1984.01040031430017. [DOI] [PubMed] [Google Scholar]
- 13.Tsai CS, Zangwill L, Gonzalez C. Ethnic differences in optic nerve head topography. J Glaucoma. 1995;4:248–257. [PubMed] [Google Scholar]
- 14.Armaly MF. Genetic determination of cup/disc ratio of the optic nerve. Arch Ophthalmol. 1967;78:35–43. doi: 10.1001/archopht.1967.00980030037007. [DOI] [PubMed] [Google Scholar]
- 15.Varma R, Tielsch JM, Quigley HA, et al. Race, age, gender and refractive error related differencesin the normal optic disc. Arch Ophthalmol. 1994;112:1068–1076. doi: 10.1001/archopht.1994.01090200074026. [DOI] [PubMed] [Google Scholar]
- 16.Poinoosawmy D, Fontana L, Wu JX, et al. Variation of nerve fibrelayer thickness measurements with age and ethnicity by scanning laser polarimetery. Br J Ophthalmol. 1997;81:350–354. doi: 10.1136/bjo.81.5.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quigley HA, Coleman AL, Dorman-Pease ME. Larger optic nerve heads have more nerve fibers in normal monkey eyes. Arch Ophthalmol. 1991;109:1441–1443. doi: 10.1001/archopht.1991.01080100121056. [DOI] [PubMed] [Google Scholar]
- 18.Jonas JB, Schmidt AM, Muller-Bergh JA, et al. Human optic nerve fiber count and optic disc size. Invest Ophthalmol Vis Sci. 1992;33:2012–2018. [PubMed] [Google Scholar]
- 19.Varma R, Skaf M, Barron E. Retinal nerve fiber layer thickness in normal human eyes. Ophthalmology. 1996;103:2114–2119. doi: 10.1016/s0161-6420(96)30381-3. [DOI] [PubMed] [Google Scholar]
- 20.Schuman JS, Hee MR, Puliafito CA, et al. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995;113:586–596. doi: 10.1001/archopht.1995.01100050054031. [DOI] [PubMed] [Google Scholar]
- 21.Lichter PR. Variability of expert observers in evaluating the optic disc. Trans Am Ophthalmol Soc. 1976;74:532–572. [PMC free article] [PubMed] [Google Scholar]
- 22.Weinreb RN, Dreher AW, Bille JF. Quantitative assessment of the optic nerve head with the laser tomographic scanner. Int Ophthalmol. 1989;13:25–29. doi: 10.1007/BF02028633. [DOI] [PubMed] [Google Scholar]
- 23.Lee DW, Jung WJ, Roh SH. Topographic Measurement of the Optic Nerve Head with HeidelbergRetina Tomograph (HRT) in Normal Korean. J Korean Ophthalmol Soc. 1999;40:2224–2231. [Google Scholar]
- 24.Yang JG, Park KH. A comparison of optic nerve topography in primary open-angle glaucoma and normal-tension glaucoma in Korea. Korean J Ophthalmol. 1997;11:79–83. doi: 10.3341/kjo.1997.11.2.79. [DOI] [PubMed] [Google Scholar]
- 25.Park HJ, Choi BG. The Quantitative Evaluation of Optic Nerve Head of NormalTension Glaucoma. J Korean Ophthalmol Soc. 2000;41:1203–1209. [Google Scholar]
- 26.Kim MK, Park KH, Kim DM. Normal-tension Glaucoma and Nerve Fiber Layer Atrophy. J Korean Ophthalmol Soc. 1999;40:1339–1345. [Google Scholar]
- 27.Lee JH, Ahn CS, Lee DY. Quantification of Retinal Nerve Fiber Layer Thickness in the Normal Subjects Using Optical Coherence Tomography. J Korean Ophthalmol Soc. 1999;40:2804–2815. [Google Scholar]
- 28.Fazio P, Krupin T, Feitl ME, et al. Optic disc topography in patients with low-tension and primary open angle glaucoma. Arch Ophthalmol. 1990;108:705–708. doi: 10.1001/archopht.1990.01070070091042. [DOI] [PubMed] [Google Scholar]
- 29.Caprioli J, Spaeth GL. Comparison of visual field defects in the low-tension glaucomas with those in the high-tension glaucomas. Am J Ophthalmol. 1984;97:730–737. doi: 10.1016/0002-9394(84)90505-1. [DOI] [PubMed] [Google Scholar]
- 30.Yamagami J, Araie M, Shirato S. A comparative study of optic nerve head in low and high tension glaucomas. Graefes Arch Clin Exp Ophthalmol. 1992;230:446–450. doi: 10.1007/BF00175931. [DOI] [PubMed] [Google Scholar]
- 31.Eid TE, Spaeth GL, Moster MR, Augsburger JJ. Quantitative differences between the optic nerve head and peripapillary retina in low-tension and high-tension primary open angle glaucoma. Am J Ophthalmol. 1997;124:805–813. doi: 10.1016/s0002-9394(14)71698-8. [DOI] [PubMed] [Google Scholar]
- 32.Iester M, Swindale NV, Mikelberg FS. Sector-based analysis of optic nerve head shape parameters and visual fields indices in healthy and glaucomatous eyes. J Glaucoma. 1997;6:370–376. [PubMed] [Google Scholar]
- 33.Caprioli J, Ortiz-Colberg R, Miller JM, Tressler C. Measurements of peripapillary nerve fiber layer contour in glaucoma. Am J Ophthalmol. 1989;108:404–413. doi: 10.1016/s0002-9394(14)73308-2. [DOI] [PubMed] [Google Scholar]