Abstract
We report a case of recurrent occlusion of laser iridotomy (LI) sites after a Visian ICL (Implantable contact lens version 4, Staar Surgical AG, Nidau, Switzerland) implantation. A 45-year-old woman had bilateral ICL implantation after placement of two peripheral LI sites in each eye to prevent pupillary block. At one month after the operation, severe narrowing or occlusion of four LI sites occurred. After this, although she received four additional LIs at postoperative months 1, 6, 9 and 10 in both eyes, the narrowing or occlusion recurred. Mild chronic anterior chamber inflammation was observed intermittently throughout the follow-up period. We performed clear lens extraction in both eyes (at postoperative month 11 in the left eye and month 26 in the right eye) due to recurrent occlusion of the LI sites and excess trabecular meshwork pigment deposition presumably caused by the four repeated LIs. Recurrent obstruction of LI sites can occur after ICL implantation. These problems were unresolvable despite four repeated laser iridotomies. The risks associated with anterior uveitis must be considered when planning an ICL implantation.
Keywords: Anterior uveitis, ICL implantation, Laser iridotomy
Recently, ICL implantation has received attention for its excellent and rapid visual and refractive results in eyes with high myopia but there are still concerns about complications such as anterior capsule opacity cataracts,1,2 pupillary block glaucoma,3,4 chronic inflammation,5 pigmentary dispersion syndrome,6,7 and pigmentary glaucoma.8 We report an interesting case of recurrent narrowing or obstruction of laser iridotomy (LI) sites despite four repeated procedures of LI.
Case Report
A 45-year-old woman, with refraction of -7.5 Dsph in the right eye (RE) and -9.25 Dsph -1.2 Dcyl×80° in the left eye(LE) presented as a good candidate for ICL implantation. With a thin central cornea thickness (450 µm), a sufficient anterior chamber depth (3.32 mm), a white-to-white diameter of 11.2 mm, a wide iridocorneal angle with light trabecular meshwork (TM) pigmentation, and no ocular disease such as cataracts, glaucoma, or uveitis, she was well within all indications for the procedure. She had mild dry eye symptoms and a history of occasional injection in both eyes that had improved spontaneously. She had no systemic disease such as diabetes.
After obtaining informed consent, two peripheral LIs were performed superiorly, approximately 90 degrees apart in each eye to prevent pupillary block. An argon green laser was used to make a definite and sufficiently sized opening (more than 500 µm in diameter) for the LI site. Also to prevent regrowth of the iris pigmented epithelium and to remove residual radial iris strands, an Nd: YAG laser was applied (1 mJ, average of 5 pulses). Patent sites and adequate sizes were confirmed 1 day after LI and every follow-up day after that with Goldmann 3 mirrors with 25x magnification. To reduce inflammation after the LI, 0.1% fluorometholone was administered four times daily for 3 days. Seven days after LI, a Visian ICL (ICM115V4 -11.00 diopter) was implanted in the RE and a -13.50 diopter lens of the same design was implanted in the LE. Two weeks after surgery, the uncorrected visual acuity (UCVA) was 25/20 with refraction of -0.25 Dcyl×172° in the RE and -0.25 Dsph in the LE.
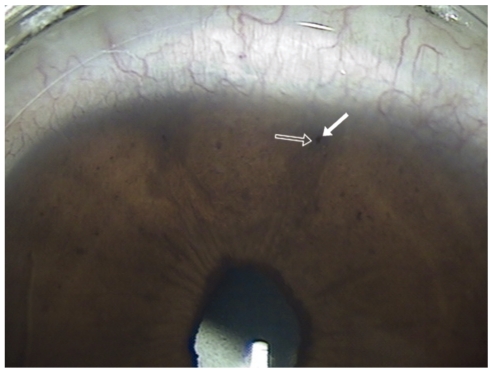
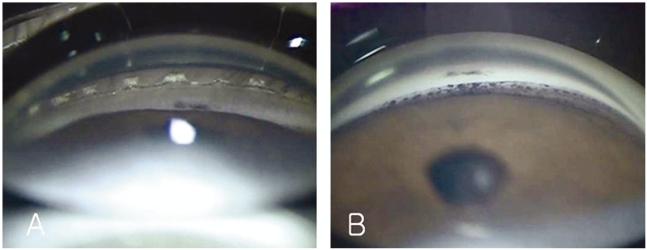
At postoperative 1 week, moderate inflammatory cells (+2) were found in the anterior chamber and vaulting (from the -125% of the central corneal thickness (CCT) in both eyes. To control the inflammation, 0.1% fluorometholone was administered every 2 hours in both eyes. Unfortunately, the inflammatory cells of the anterior chamber did not resolve. As time passed, the iris pigments of the ICL and vaulting increased progressively. At one month postoperative, 70% narrowing or obstruction of all the 4 peripheral LI sites was observed in both eyes (Fig. 1). Inflammatory cells (+1) persisted in the anterior chamber despite the administration of 0.1% fluorometholone four times per day. The iridocorneal angle narrowed to less than 10 degrees and vaulting increased to approximately 250% of CCT in RE and 300% of CCT in LE. Intraocular pressure was 12 mmHg in RE and 10 mmHg in LE. After additional laser treatment, the angle width increased to 40 degrees and vaulting returned to 100% (Fig. 2). Although 0.1% fluorometholone was administered four times daily for 7 days after LI, mild cells (+1) remained in the anterior chamber. When the more potent 1% prednisolone acetate was used, anterior inflammatory cells disappeared. Although she received three additional LIs (at postoperative months 6, 9 and 10) in both eyes, the narrowing or occlusion of the LI sites recurred. Mild inflammatory cells (+1) were observed transiently throughout the follow-up period. Pigment deposits on the ICL were observed and pigmentation of TM increased to Grade 3 or 4 by the semi-quantitative method (Grade 0-4) due to the four repeated LIs. The pupil was distorted toward the LI site but posterior synechia was not observed. Finally, we removed the ICL and performed clear lens extraction (CLE) at postoperative month 11 in the LE and month 26 in the RE. After CLE, good UCVA (20/20) and normal intraocular pressure (12 mmHg) were well maintained but the distortion of the iris toward the LI sites remained. There was no evidence of pigment dispersion syndrome or pigmentary glaucoma.
Fig. 1.
Laser iridotomy (LI) sites at 9 months after ICL surgery. Pinpoint openings (solid arrow) of LI sites with regeneration of dark-brown iris pigment epithelium (hollow arrow) were observed. The Iris was distorted toward LI sites due to repeated LI. 25 ×, Goldmann 3 mirrors.
Fig. 2.
Width of iridocorneal angle at 9 months after ICL surgery. (A) Peripheral iris was very steep and convex. Iridocorneal angle was narrowed because of the obstruction of LI sites. (B) After additional LI, although the angle width increased, trabecular pigment also increased. 25 ×, Goldmann 3 mirrors.
Discussion
The aim of this report is to illustrate that recurrent obstruction of LI sites can be induced by ICL implantation and that these complications were unresolvable despite four repeated LI treatments.
LI is very important for the prevention of pupillary block. Because Asians have thicker and more heavily pigmented irises, formation of the LI site must be performed with a combined technique (using argon to make the initial bore and the Nd:YAG laser to complete the perforation)9 and the size of LI sites must be larger than those in Caucasians. Ophthalmologists who do not have much experience with Asian patients may not know about the more consistent structure of this iris type, therefore performing LI on this population can be complicated.
It is not certain whether ICL implantation itself might provoke anterior uveitis or if the patient had undiagnosed anterior uveitis in the past and it simply recurred after ICL implantation. We posit that the ICL was implanted during a quiescent period but the chronic irritation of the posterior iris surface by the ICL disrupted the anterior blood aqueous barrier, inducing anterior chamber inflammation. As a result, the iris pigment epithelium regenerated and occluded LI sites.
There is convincing evidence found by ultrasound biomicroscopy that contact between the ICL and the posterior iris surface occurred in all cases. Jimenez-Alfaro et al. reported that the aqueous flare can increase by 49.19% in the first postoperative month relative to preoperative values, then decrease and subsequently remain above preoperative values for 24 months.5 There are many reports about subclinical inflammation after implantation of anterior chamber phakic IOLs.10 However, subclinical inflammation after ICL implantation has not been as problematic as the decrease of lens transmission.5 It is now necessary to focus our attention on the chronic rubbing of the posterior iris surface by the ICL and on subclinical inflammation, because chronic inflammation can induce cataracts, obstruction of LI sites, synechia, or cystoid macular edema. Therefore, it must be considered as a possibility even if inflammatory cells in anterior chamber are undetectable by the slitlamp, because flare and increased permeability of the blood-aqueous barrier can be detected with a laser flare-cell meter or by fluorophotometry. Determining the exact ICL size is crucial for the prevention of rubbing of the posterior surface of the iris with the ICL. The white-to-white distance was measured with a caliper and rechecked with ORBSCAN to be 11.2 mm. So the ICL was implanted with a horizontal length of 11.5 mm. Because the vault was 100% of CCT at postoperative week 1, the size of the ICL seemed appropriate.
The inflammation of the anterior chamber and the obstruction of LI sites occurred in both eyes nearly simultaneously with similar features. After CLE, the inflammation of the anterior chamber disappeared at 1 month postoperative and the size of the LI sites remained constant. Given these results, it would seem that the cause of the anterior uveitis in this patient was the ICL combined with a predisposition toward inflammation.
The pupil was distorted toward the LI sites due to multiple laser treatments and high energy transmission (Fig. 1). In our case, surgical pigment vacuum iridectomy11 was considered before CLE because a dry vitrector with viscoelastics can be used under topical anesthesia. However, CLE was indicated due to the trabecular hyperpigmentation and chronic inflammation. The ICL was removed without any difficulty at postoperative months 11 (LE) and 26 (RE) because the ICL did not adhere to its surroundings despite multiple pigments on the ICL and repeated laser therapies. From these findings, collamer, the material constituting the ICL, seems to be biocompatible.12
Recurrent obstruction of LI sites can be induced by ICL implantation by either the trauma of the surgery or by reactivation of quiescent anterior uveitis. We therefore recommend that the size of LI sites for ICL implantation be slightly larger than conventional LI sites, especially in Asian irises. The risk of anterior uveitis should always be considered. Lastly a detailed review of the past medical history and examination of the anterior chamber looking for inflammation must be performed.
Footnotes
Presented at the XXIV Congress of the European Society of Cataract & Refractive Surgeons, London, England, September 2006.
References
- 1.Gonvers M, Bornet C, Othenin-Girard P. Implantable contact lens for moderate to high myopia-relationship of vaulting to cataract formation. J Cataract Refract Surg. 2003;29:918–924. doi: 10.1016/s0886-3350(03)00065-8. [DOI] [PubMed] [Google Scholar]
- 2.Sanchez-Galeana CA, Smith RJ, Sanders DR, et al. Lens opacities after posterior chamber phakic intraocular lens implantation. Ophthalmology. 2003;110:781–785. doi: 10.1016/s0161-6420(02)01973-5. [DOI] [PubMed] [Google Scholar]
- 3.Bylsma SS, Zalta AH, Foley E, et al. Phakic posterior chamber intraocular lens pupillary block. J Cataract Refract Surg. 2002;28:2222–2228. doi: 10.1016/s0886-3350(02)01303-2. [DOI] [PubMed] [Google Scholar]
- 4.Smallman DS, Probst L, Rafuse PE. Pupillary block glaucoma secondary to posterior chamber phakic intraocular lens implantation for high myopia. J Cataract Refract Surg. 2004;30:905–907. doi: 10.1016/j.jcrs.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 5.Jimenez-Alfaro I, Benitez del Castillo JM, Garcia-Feijoo J, et al. Safety of posterior chamber phakic intraocular lenses for the correction of high myopia: anterior segment changes after posterior chamber phakic intraocular lens implantation. Ophthalmology. 2001;108:90–99. doi: 10.1016/s0161-6420(00)00403-6. [DOI] [PubMed] [Google Scholar]
- 6.Brandt JD, Mockovak ME, Chayet A. Pigmentary dispersion syndrome induced by a posterior chamber phakic refractive lens. Am J Ophthalmol. 2001;131:260–263. doi: 10.1016/s0002-9394(00)00606-1. [DOI] [PubMed] [Google Scholar]
- 7.Abela-Formanek C, Kruger AJ, Dejaco-Ruhswurm I, et al. Gonioscopic changes after implantation of a posterior chamber lens in phakic myopic eyes. J Cataract Refract Surg. 2001;27:1919–1925. doi: 10.1016/s0886-3350(01)01229-9. [DOI] [PubMed] [Google Scholar]
- 8.Sanchez-Galeana CA, Zadok D, Montes M, et al. Refractory intraocular pressure increase after phakic posterior chamber intraocular lens implantation. Am J Ophthalmol. 2002;134:121–123. doi: 10.1016/s0002-9394(02)01414-9. [DOI] [PubMed] [Google Scholar]
- 9.Chun YS, Lee JH, Lee JM, Park IK. IOP and Gonioscopic Changes after Implantable Contact Lens Implantation in Myopic Eyes. J Korean Ophthalmol Soc. 2005;46:336–344. [Google Scholar]
- 10.Perez-Santonja JJ, Iradier MT, Benitez del Castillo JM, et al. Chronic subclinical inflammation in phakic eyes with intraocular lenses to correct myopia. J Cataract Refract Surg. 1996;22:183–187. doi: 10.1016/s0886-3350(96)80216-1. [DOI] [PubMed] [Google Scholar]
- 11.Hoffer KJ. Pigment vacuum iridectomy for phakic refractive lens implantation. J Cataract Refract Surg. 2001;27:1166–1168. doi: 10.1016/s0886-3350(01)00845-8. [DOI] [PubMed] [Google Scholar]
- 12.Khan AJ, Percival SP. 12 year results of a prospective trial comparing poly(methyl methacrylate) and poly(hydroxyethyl methacrylate) intraocular lenses. J Cataract Refract Surg. 1999;25:1404–1407. doi: 10.1016/s0886-3350(99)00199-6. [DOI] [PubMed] [Google Scholar]