Abstract
Objectives
To create a doctor of pharmacy curricular experience that will decrease students' social barriers to interaction with and treatment of mentally-ill patients.
Design
We created a survey instrument to measure 4 aspects of students' conceptions of schizophrenia and clinical depression: (1) understanding of the medical nature of each disease, (2) understanding of patient behavior, (3) belief in the efficacy of treatment, and (4) social distance. We delivered this instrument before and after a neuropsychiatry curriculum including “peer-level patient presenters” in addition to the traditional first-year pharmacy curriculum.
Assessment
Social-distance scores significantly decreased in first-year pharmacy students who attended peer-level patient presentations, indicating increased willingness to interact with persons with schizophrenia and clinical depression. In addition, students' understanding of the causes of illness, behavior of patients, and most importantly, efficacy of drug counseling for these diseases increased.
Conclusions
Changes to the curriculum including the addition of peer-level patient presentations can quantitatively decrease pharmacy students' social barriers to the treatment of mentally-ill patients.
Keywords: curriculum, mental illness, social distance, schizophrenia, depression
INTRODUCTION
Pharmacists are generally less interactive with and less comfortable providing pharmaceutical care services and medication instructions to mentally ill patients than to patients with most other classically “somatic” illnesses.1-4 This observation is particularly alarming considering the high personal and social cost of mental illness and the historically high rates of medication noncompliance, and continues despite findings that medication counseling and monitoring improves adherence to drug therapy in mentally ill patients.5,6
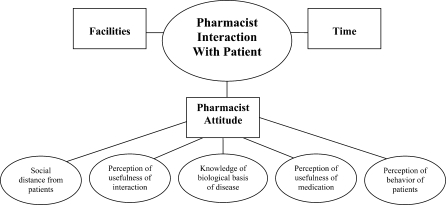
There are several reasons why pharmacists may have lessened interaction with mentally ill patients. These include (1) poor understanding of the biological and chemical nature of the illnesses, (2) poor understanding of the behavior of patients with mental illnesses, (3) an inappropriately low belief in the efficacy of psychiatric medication and thus the importance of stable treatment, and (4) increased social distance from those with mental illnesses.2,7-9
Social distance is a major focus of this study, and was assessed (1) because of its importance in the fields of psychology and sociology as a measure of willingness of a subject to participate in varied relationships with a person belonging to a stigmatized group and (2) because it is believed to correspond to actual behavior.8-12 Social distance toward mentally ill patients has been assessed in first-year pharmacy students, indicating that students with prior relationships with someone with a mental illness exhibited less social distance than those without,11 however, the effect of pharmacy curriculum on reducing social distance has not been studied.
In order to examine these questions, we have quantitatively measured the impact of a teaching technique utilizing student interaction with “peer-level patient presenters,” who are patients with mental illness or family members of these patients.13,14 “Peer-level” indicates that the presenter has what the student perceives as a social status equal to or greater than their own. This form of interaction is different from that achieved in the clinic or pharmacy in which the student is in a position of authority over the patient. Studies have predominantly shown that “peer-level” patient interactions significantly decrease prejudicial attitudes, while clinician-to-patient interactions do not.8,12,13,15,16 In this study, “peer-level” status was achieved by using presenters with graduate-level education or work history as a health care professional.
The objective of this study was to determine whether a teaching technique using peer-level patient presenters would be effective in increasing pharmacy students' perception of the importance of the role of pharmacist counseling in effective treatment of 2 specific mental illnesses and in decreasing classical measures of social distance that might impair pharmacy students' willingness to interact with these patients. These goals correspond to the American Council for Pharmacy Education competency standards 13 and 15, which emphasize core curricular teaching that integrates the elements of knowledge, skills, attitudes, and values, as well as assessment and evaluation of student learning outcomes.17 In addition, in accordance with the Center for the Advancement of Pharmaceutical Education's educational outcomes, our study was designed to promote patient-centered care training to pharmacy students.18 We describe in this report a curricular approach designed to achieve the above stated goals, and quantitative data supporting the effectiveness of this curriculum.
DESIGN
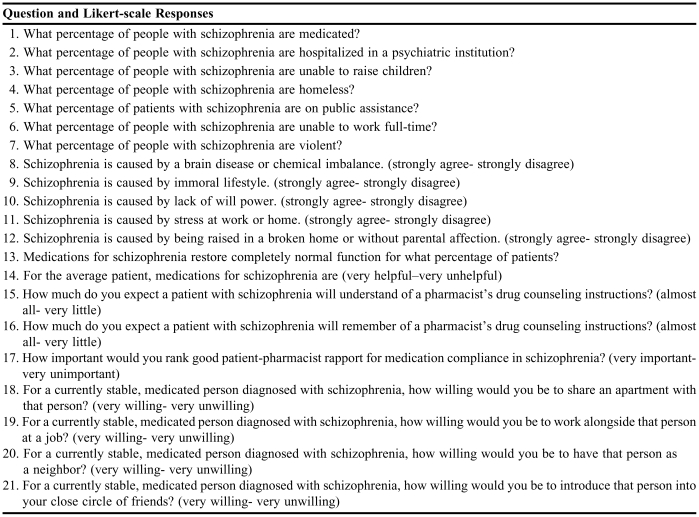
To determine whether the technique of peer-level patient presentation decreases pharmacy students' social distance from patients with mental illness and/or increases their perception of the importance of pharmacist counseling for these patients, we chose to investigate the effect of peer-level patient presentations for 2 commonly encountered mental illnesses with significant social stigma: schizophrenia and clinical depression. A questionnaire was designed to specifically measure first-year pharmacy students' perception of 5 items that we hypothesized may impact pharmacists' attitudes toward patients suffering from schizophrenia and clinical depression (Figure 1). This questionnaire was administered twice, before and after pharmacy students completed the curriculum on psychiatric and neurologic illnesses, and data were analyzed to quantify which measures were changed by students' exposure to the peer presenters.
Figure 1.
Proposed factors impacting pharmacists' interaction with mentally-ill patients
As there was no established survey instrument that addressed all of the measures we wished to investigate, a unique instrument was created from established sources as well as our experience.19 The social distance questions used were a 4-item derivation of the classic Social Distance Scale20 as used by Bell8 and Angermeyer.21 The Bogardus social distance scale was designed to study race relations and includes several questions probing openness to immigration of differing groups as well as personal relationships. This scale has been modified to analyze perceptions about members of differing national, religious, and political affiliations,10 the physically handicapped,22 and the mentally ill.11 The questions included in this study were chosen to represent varying levels of personal relationship (roommate, friend, coworker, and neighbor) involving social comfort, while excluding previously used questions that could reflect conceptions of the competency or reliability of the patient, such as willingness to allow a patient to babysit one's children.8
The patient behavior and usefulness of medication questions were derived from those utilized in a study of British medical students and practitioners.7 The causes of schizophrenia and clinical depression questions were derived from those utilized in a German study of public perception of the causal attributions of schizophrenia.21
First-year students enrolled in the Pacific University School of Pharmacy were asked to voluntarily complete during class time a 42-item questionnaire at the beginning and at the end of their curriculum on psychiatric and neurologic illnesses. Questions were designed to measure students' perception of the behavior of patients with schizophrenia and clinical depression (7 questions each); causes of schizophrenia and clinical depression (5 questions each); usefulness of medication (2 questions each); usefulness of pharmacist interaction (3 questions each); and social distance from patients with schizophrenia and clinical depression (4 questions each). A modified version of the survey is provided in Appendix 1. At the end of the curriculum, students were also invited to complete an open-ended question evaluating the use of our peer-level patient presenter on clinical depression.
The Pacific University School of Pharmacy uses a modified-block format in which courses are presented sequentially, 3 days per week, for 6 hours per day. This allows total immersion in one didactic topic at a time. Additionally, 1 day every other week, first-year students attend a professional-skills seminar, and 1 day every other week they attend early experiential clinical rotations as pharmacy technicians. As part of our course CNS: Pharmacology and Medicinal Chemistry with Clinical Correlates, we presented five 6-hour days of curriculum on neuropsychiatric disorders. During this section we covered several neuropsychiatric disorders including generalized anxiety disorder, clinical depression, bipolar disorder, phobia, and schizophrenia. Our instructional techniques included (1) standard didactic presentation of current neurophysiological theories of mental illness and pharmacology, (2) presentations by a clinical psychiatrist, and (3) peer-level patient/family presenters.
Clinician presentations on both clinical depression and schizophrenia utilized a case-study approach, discussing real patients and their therapeutic and clinical histories in order to portray the wide variability in patient cognition, emotional response to pharmacotherapy, and response to pharmaceutical treatment. The clinical presenter also described how to positively interact with patients who many health care workers find disconcerting to work with.
Peer-level patient/family presenters spoke for both topics; a patient presenter spoke on clinical depression while a second speaker discussed a family history of schizophrenia. The peer-level patient presenter on clinical depression spoke with startling honesty for 1.5 hours on the symptomology of the disease, familial and cultural barriers she faced in accepting diagnosis and treatment, her medication history, and how she was able to overcome her illness enough to raise a family, continue her education, and run a business, while still suffering from recurrent bouts of depression. Using this technique of self-portrayal, the speaker attempted to bring a sense of reality and humanity to the illness. The students continued this dialog by asking formal questions for 30 minutes, and several students joined in a personal conversation with her during the following break. The family member speaking on schizophrenia discussed her relationship with her schizophrenic family member, and how the family was affected by the illness on a day-to-day basis. Students responded with many questions ranging from symptomology to personal impact, including a tentative question on whether the lecturer was concerned about a genetic predisposition toward schizophrenia in her children. This question resulted in a dialog in which students could address their own fears and attitudes toward mental illness in their families and friends.
The questionnaire was presented in online form utilizing Web Course Tools (WebCT), and students were given in-class time to complete it. All students in our program are required to bring a WebCT compatible laptop to class each day, and all first-year students had online access to the questionnaire. The questionnaire was presented twice, once before their curriculum on psychiatric and neurologic illnesses and once after.
Data including personal identifiers was downloaded from the WebCT base into a Microsoft Excel spreadsheet. Within this spreadsheet, students' responses on the pre- and post-intervention survey instruments were coded and paired to allow for anonymous analysis. Student data for the questions on schizophrenia or clinical depression were subdivided according to their response to a question asking whether they had attended the speaker presentations for that topic. In order to quantitate changes, data for each 4- or 5-point Likert-scale question was transformed from verbal descriptions to a numerical scale on which 1 equaled higher percentage, more agreement, or more willing, and 4 or 5 equaled lower percentage, less agreement, or least willing. Changes in group means are presented in pretest mean/posttest mean ratio form where 3.74/4.24 indicates a mean change toward lower percentage, or less agreement. Data for each question was analyzed using a paired, two-tailed t test, to identify differences between pre- and post-intervention answers. Statistical significance was defined as p < 0.05, and only significant changes are reported in this manuscript.
IRB approval was sought and granted by the Pacific University Institutional Research Board for the completion of this study.
ASSESSMENT
Forty-eight students completed both the pre-intervention and post-intervention survey. Thirty-four of the 48 students had attended the presentations on clinical depression and 14 had not, and 42 had attended the presentations on schizophrenia and 6 had not.
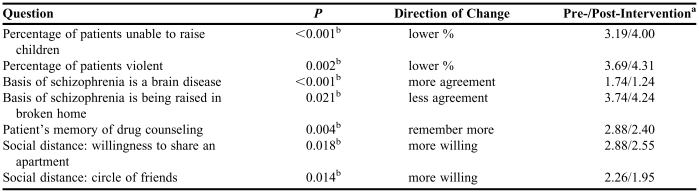
Students who attended the peer-level family-member presentation on schizophrenia (n = 42) were less likely to believe that patients with schizophrenia would be unable to raise children than they were before completing the curriculum (p < 0.001; pre-curriculum score/ post-curriculum score = 3.19/4.00), Students also were less likely to believe that patients with schizophrenia are violent than they were before completing the curriculum (p = 0.002; 3.69/ 4.31; Table 1). They indicated significantly more agreement with the statement that “schizophrenia is caused by a brain disease or chemical imbalance” (p < 0.001; 1.74/1.24). Students showed significantly less agreement that schizophrenia is caused by “being in a broken home or without parental affection” (p = 0.020; 3.74/4.24) and although not significant, students trended to indicate less agreement with statements that it was caused by immoral lifestyle, lack of willpower, or stress at work or home.
Table 1.
Questionnaire on Schizophrenia by Students Attending Presentations
A 4 or 5-point Likert scale was used on which 1 = higher percentage, more agreement, or more willing, and 4 or 5 = lower percentage, less agreement, or least willing. Absolute change in score is presented as a pre-test mean/post-test mean ratio
indicates a p < 0.05 on a two-tailed, paired t test
Students who attended the peer-level family member presentation on schizophrenia indicated an increased expectation that patients with schizophrenia would remember drug counseling instructions compared to their pre-intervention expectations (p = 0.004; 2.88/2.40).
All 4 social distance measures decreased among students who attended the peer-level family member presentation on schizophrenia, with significant decreases in the 2 indicators of closest social interaction: students became more willing to share an apartment with a person with schizophrenia (p = 0.018; 2.88/2.55) or introduce a person with schizophrenia to their close circle of friends (p = 0.014; 2.26/1.95).
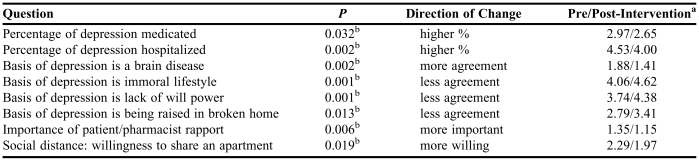
Students who attended the peer-level patient presentation on clinical depression (n = 34) showed increased perception of the severity of the disorder. They were more likely to believe that patients with depression would be medicated (p = 0.032; 2.97/2.65) or hospitalized (p = 0.002; 4.53/4.00) than they were before completing the curriculum (Table 2). They indicated significantly more agreement with the statement “schizophrenia is caused by a brain disease or chemical imbalance” (p = 0.002; 1.88/1.41), and less agreement that it is caused by an immoral lifestyle (p = 0.001; 4.06/4.62), lack of willpower (p = 0.001; 3.74/4.38), or “being raised in a broken home or without parental affection” (p = 0.013; 2.79/3.41).
Table 2.
Questionnaire on Clinical Depression by Students Attending Presentations
A 4 or 5-point Likert scale was used on which 1 = higher percentage, more agreement, or more willing, and 4 or 5 = lower percentage, less agreement, or least willing. Absolute change in score is presented as a pre-test mean/post-test mean ratio
indicates a p < 0.05 on a two-tailed, paired t test
After attending the peer-level patient presentation on clinical depression, students ranked “good patient-pharmacist rapport for medication compliance” as more important than they had in the pre-intervention survey (p = 0.006; 1.35/1.15).
Students attending the peer-level patient presentation on clinical depression showed a significant decrease in the first social distance measure, responding with more willingness to share an apartment with a person with clinical depression (p = 0.019; 2.29/1.94) and trended toward decreased social distance in 2 of the 3 other measures.
Students who did not attend the peer-level patient/family presentations on schizophrenia (n = 6) or clinical depression (n = 14) showed significant changes only in measures of perception of the biological basis of the diseases, and not in measures of belief of the pharmacists' importance or social distance. The 3 measures that showed significant change for this student group were increased agreement that the basis of schizophrenia is a brain disease (p = 0.042; 2.00/1.17), increased agreement that the basis of clinical depression is a brain disease (p = 0.013; 1.86/1.36), and less agreement that clinical depression is due to a lack of willpower (p = 0.019; 4.21/4.57).
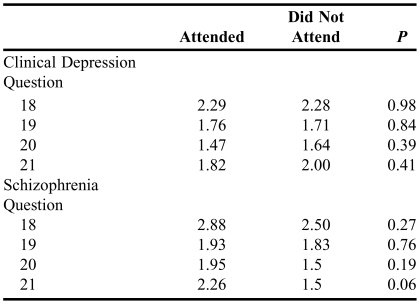
In order to rule out the possibility that students attending the presentations did so because of an initially more positive or accepting attitude toward mental illness, we compared the pre-intervention social distance scores of students in the attending group with those of students in the groups not attending. There was no significant difference in any initial social distance measure between these groups as measured by Student's t test (Table 3).
Table 3.
Pre-Curriculum Social Distance Scores Compared Between Student Groups Who Attended or Did Not Attend Peer-Level Patient/Family Presentations
Lower scores indicate less social distance, higher scores indicate greater social distance
Student feedback to an open-ended question on the clinical depression presentation indicated that the presentation was extremely helpful. Several students emphasized that although the didactic curriculum had taught about the biological basis of disease, the peer-level patient presentation cemented the idea that mental illness could happen to “anyone” and enhanced their feelings of empathy toward patients with mental illnesses.
DISCUSSION
We presented and tested a teaching plan designed to enhance not only students' didactic knowledge, but also their future professional interaction with patients with mental illnesses. While the use of patient speakers has been reported in general pharmacy education, we have found no literature describing its use in mental illness education or quantitating its effect on social distance measures.14
Our use of peer-level patient/family presenters increased students' qualitative self-reported sense of empathy toward mentally ill patients. Our quantitative data similarly suggest that our curriculum achieved the stated goal of increasing pharmacy students' perception of the importance of the role of pharmacist counseling in effective treatment of these disorders, and in decreasing classical measures of social distance that might impair their willingness to interact with these patients. Based on student feedback, interaction with peer-level patient presenters appeared to be an important component of the successful change in their attitudes toward mental illness.
Students' perception of the degree of social impairment caused by/resulting from schizophrenia decreased as a result of completing the curriculum, while their perception of the degree of social impairment caused by depression increased. We believe that these opposing changes reflect the misconceptions that students brought to the classroom, as they showed a higher initial perception of social impairment for schizophrenia than for depression. These results may reflect an increased awareness of the seriousness of depression, as well as a new understanding that there are many high-functioning persons with schizophrenia
We initially anticipated that there would be pronounced changes in social distance scores, but upon analysis we found significant changes only for those measures for which high social distance (over 2.0) was indicated in the initial questionnaire. These items were those which measured closer social relationships, ie, roommate or friend as opposed to coworker or neighbor. These results are consistent with prior studies on social distance that report significant change only on items describing close relationships and not on items describing more distant social relationships.23
Lastly, while students actually showed less belief in the usefulness of medications for these diseases (possibly due to patient and clinician discussions of drug-refractory cases), they showed more belief in the overall importance of patient/pharmacist rapport and the ability of patients to understand and remember drug counseling. While students recognized the clinical limitations of these drugs, they believed more strongly in the role of the pharmacist in treating these patients. We do not know whether these attitudinal changes will translate into successful changes in patient care. It would be of interest to follow these students postgraduation and administer questionnaires to measure self-reported comfort with mentally ill patients and average time spent on drug-counseling with these patients.
One of the major barriers to the use of peer-level patients in the curriculum is the identification of appropriate speakers. Local offices of major national disease associations have been helpful in recruiting patient presenters for schizophrenia, depression, bipolar disorder, and Parkinson's disease. The local chapter of the National Alliance for the Mentally Ill (NAMI) has been particularly helpful and has an established program of patient-presenters.
SUMMARY
A curricular approach using peer-level patient/family presenters in addition to traditional didactic methods increased pharmacy students' empathy toward mentally-ill patients, decreased social distance, and increased students' belief in the overall importance of the patient/pharmacist relationship in successfully treating mental illness.
ACKNOWLEDGEMENTS
This study was supported in part by the 2006 Ortho-McNeil Janssen Scientific Affairs – AFPE – AACP New Investigator Grant for Pharmacy Faculty.
The authors would like to acknowledge the invaluable participation of Dr. Kevin Smith and Ms. Gayathri Ramprasad. We also would like to thank Dr. Erika Kleinknecht for study design suggestions and Dr. Joe Bonnarens for valuable comments on the manuscript.
Appendix 1. Questions on schizophrenia included in a survey instrument to determine knowledge of disease and attitudes toward persons with mental illness. An identical set of questions was included for clinical depression
REFERENCES
- 1.Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55:1434–6. doi: 10.1176/appi.ps.55.12.1434. [DOI] [PubMed] [Google Scholar]
- 2.Vainio KK, Airaksinen MS, Hyykky TT, Enlund KH. Effect of therapeutic class on counseling in community pharmacies. Ann Pharmacother. 2002;36:781–6. doi: 10.1345/aph.1A374. [DOI] [PubMed] [Google Scholar]
- 3.Kirking DM. Pharmacists' perceptions of their patient counseling activities. Contemp Pharm Pract. 1982;5:230–8. [PubMed] [Google Scholar]
- 4.Cates ME, Burton AR, Woolley TW. Attitudes of pharmacists toward mental illness and providing pharmaceutical care to the mentally ill. Ann Pharmacother. 2005;39:1450–5. doi: 10.1345/aph.1G009. [DOI] [PubMed] [Google Scholar]
- 5.Greenall P. The barriers to patient-driven treatment in mental health: why patients may choose to follow their own path. Int J Health Care Quality Assurance. 2006;19(1):xi–xxv. doi: 10.1108/13660750610643822. [DOI] [PubMed] [Google Scholar]
- 6.Bultman DC, Svarstad BL. Effects of pharmacist monitoring on patient satisfaction with antidepressant medication therapy. J Am Pharm Assoc. 2002;42:36–43. doi: 10.1331/108658002763538053. [DOI] [PubMed] [Google Scholar]
- 7.Mukherjee R, Fialho A, Wijetunge A, Checkinski K, Surgenor T. The stigmatisation of psychiatric illness; the attitudes of medical students and doctors in a London teaching hospital. Psychiatric Bull. 2002;26:178–81. [Google Scholar]
- 8.Bell JS, Johns R, Chen TF. Pharmacy students' and graduates' attitudes towards people with schizophrenia and severe depression. Am J Pharm Educ. 2006;70((4)) doi: 10.5688/aj700477. Article 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lauber C, Nordt C, Falcato L, Rossler W. Factors influencing social distance toward people with mental illness. Community Ment Health J. 2004;40:265–74. doi: 10.1023/b:comh.0000026999.87728.2d. [DOI] [PubMed] [Google Scholar]
- 10.Payne MC, York CM, Fagan J. Changes in measured social distance over time. Sociometry. 1974;37:131–6. [Google Scholar]
- 11.Crismon ML, Jermain DM, Torian SJ. Attitudes of pharmacy students toward mental illness. Am J Hosp Pharm. 1990;47:1369–73. [PubMed] [Google Scholar]
- 12.Jermain DM, Crismon ML. Students' attitudes toward the mentally ill before and after clinical rotations. Am J Pharm Educ. 1991:5545–8. [Google Scholar]
- 13.Couture SM, Penn DL. Interpersonal contact and the stigma of mental illness: a review of the literature. J Mental Health. 2003;12:291–305. [Google Scholar]
- 14.Chisholm MA, Wade WE. Using actual patients in the classroom to develop positive student attitudes toward pharmaceutical care. Am J Pharm Educ. 1999;63:296–9. [Google Scholar]
- 15.Neumann M, Elizur A, Bawer A. Changing medical students' attitudes and professional behavior toward mental patients as a function of psychiatric clerkship. Israel J Psychiatry Related Sci. 1984;21:235–46. [PubMed] [Google Scholar]
- 16.Hicks JM, Spaner FE. Attitude change and mental hospital experience. J Alzheimer's Dis. 1962;65:112–20. [Google Scholar]
- 17.Accreditation Council for Pharmacy. Accreditation Standards. Available at: http://www.acpe-accredit.org/Pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.Pdf. Last Accessed: February 01, 2008.
- 18.American Association of Colleges of Pharmacy Center for the Advancement of Pharmaceutical Education. Educational Outcomes, revised version 2004. Available at: http://www.aacp.org/docs/mainnavigation/resources/6075_CAPE2004.Pdf. Last accessed: February 01, 2008.
- 19.Poirier T, Crouch M, Hak E, MacKinnon G, Mehvar R, Monk-Tutor M. Guidelines for manuscripts describing instructional design or assessment: the IDEAS format. Am J Pharm Educ. 2004;68((4)) doi: 10.5688/aj730355. Article 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bogardus ES. Measuring social distance. J Applied Sociol. 1925;9:299–308. [Google Scholar]
- 21.Angermeyer MC, Beck M, Matschinger H. Determinants of the public's preference for social distance from people with schizophrenia. Can JPsychiatry. 2003;48:663–8. doi: 10.1177/070674370304801004. [DOI] [PubMed] [Google Scholar]
- 22.Bowman JT. Attitudes toward disabled persons: social distance and work competence. J Rehabil. 1987;53:41–4. [Google Scholar]
- 23.Mino Y, Yasuda N, Tsuda T, Shimodera S. Effects of a one-hour educational program on medical students' attitudes to mental illness. Psychiatry Clin Neurosci. 2001;55:501–7. doi: 10.1046/j.1440-1819.2001.00896.x. [DOI] [PubMed] [Google Scholar]