Abstract
Objectives
To implement an interactive, Web-based postgraduate course aimed at improving the knowledge, skills, and confidence of health care practitioners with interest in providing pharmaceutical care to people with mental disorders.
Design
The Web-based course was created in which authentic tasks and multiple modes of presentation and problem-solving were used to develop understanding of core concepts. Participants formulated pharmaceutical care plans for authentic case scenarios and cases selected from practice. Participants developed management plans using audiovisual lectures, videotaped demonstration patient interviews, and links to mental health practice tools and the literature. A combination of online discussion, collaborative and individual preparation of care plans, and peer and instructor feedback were used.
Assessment
Responses on postcourse surveys showed that participants' comfort levels with providing pharmaceutical care for common mental disorders increased moderately. Three-quarters of respondents indicated that the course had deepened their understanding and enhanced their mental health practice.
Summary
A Web-based postgraduate course in pharmaceutical care for patients with mental disorders was successfully implemented and resulted in a template which can be used in the development of similar postgraduate courses.
Keywords: psychiatry, pharmacy, postgraduate education, online, mental health
INTRODUCTION
As many as 450 million people worldwide suffer from mental disorders, with 1 in 4 families having at least 1 member with a mental illness.1 In New Zealand, 46.6% of the population may meet criteria for having a mental disorder at some time in their lives.2
Pharmacists are well positioned to contribute to the management of mental illnesses as they are among the most trusted health professionals.3 Among mentally ill patients, pharmacists may be particularly valuable in improving adherence to medication regimens and providing appropriate advice for managing and decreasing medication-related side effects.4 However, pharmacists' provision of information about psychotropic medications may be limited by their lack of training in counselling people with mental illnesses.5 This is not a concern unique to pharmacists. Health professionals in general have identified the management of mental illnesses as among their most challenging therapeutic responsibilities.6-8
Postgraduate and continuing education programs are of vital importance to expanding basic pharmacy education and enhancing the therapeutic management skills of health care professionals, particularly in therapeutic areas where insufficient training has been received or achieved during undergraduate studies. More postgraduate education programs in mental health care are needed and may help health care practitioners to gain increased awareness, understanding, knowledge, and skills in assisting their mental health clients, in particular on issues surrounding pharmacotherapy.9-11 In New Zealand, there are only a few mental health educational programs that are designed to enhance the knowledge and skills of pharmacists in this therapeutic area. Taking all these issues into consideration, the School of Pharmacy at the University of Auckland decided to offer a postgraduate course, Pharmacotherapy in Psychiatry, as an on-campus course starting in 2004. Because course enrolment was low, an online delivery format was considered.
Internet technology is an emerging option for the provision of postgraduate educational programs as it offers practicing professionals the opportunity to continue in the workforce while engaging in an active-learning environment, allowing them to proceed at their own pace and at their convenience. However, in the area of pharmacotherapy in mental health, there are a limited number of teaching and learning models developed for Web-based technology. Consequently, the Pharmacotherapy in Psychiatry course was redesigned as an online course and offered for the first time in 2005.
The design and implementation of this interactive, online postgraduate course aimed at improving the knowledge, skills, and confidence of health care practitioners with interest in providing pharmaceutical care to people with mental disorders are described.
DESIGN
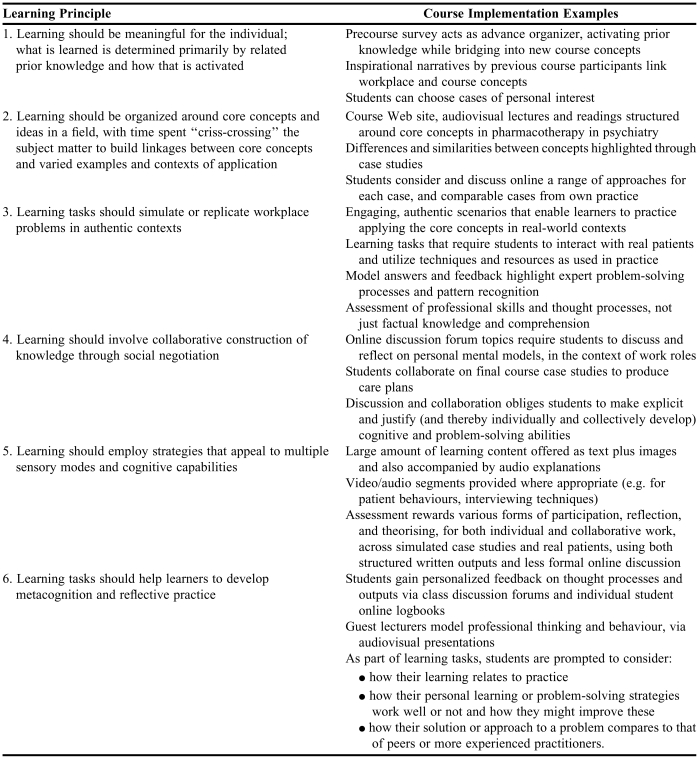
The online Pharmacotherapy in Psychiatry course design was based on the following learning principles:
Learning should be meaningful for the individual; what is learned is determined primarily by related prior knowledge and how that is activated.12
Learning should be organized around core concepts and ideas in a field,13 with time spent “criss-crossing” the subject matter to build linkages between core concepts and varied examples and contexts of application.14
Learning tasks should simulate or replicate workplace problems in authentic contexts.15
Learning should involve collaborative construction of knowledge through social negotiation.16
Learning should employ strategies that appeal to multiple sensory modes and cognitive capabilities.12,17
Learning tasks should help learners to develop metacognition12 and reflective practice.18
The learning design principles and measures to implement them in the Pharmacotherapy in Psychiatry course are outlined in Table 1. The course consists of 5 academic modules: Module 1: Introduction to Mental Health; Module 2: Psychopharmacology; Module 3: Psychosis and Schizophrenia; Module 4: Mood and Anxiety Disorders; Module 5: Mental Health in Special Populations. Module design focused on supporting participants in developing solutions to a range of practice-related problems common to the field.
Table 1.
Learning Design Principles Utilized in Pharmacotherapy in Psychiatry Online Course
A design research approach was utilized for the development and evaluation of the course.19 The steps in the development process consisted of: review of the literature on the latest developments in the teaching and learning of psychiatric pharmacotherapy; design of the content of the course and student material around the learning principles described above to support teaching and learning in a virtual environment; development of the course Web pages and hosting of these within the University's learning management system; liaison with a range of content experts to facilitate creation of audiovisual lectures and other relevant content resources; creation of a course resource CD-ROM to contain the audiovisual lectures and demonstrations of psychiatric patient interviews, to ensure that these large files would be accessible by students with low-bandwidth access to the Internet.
Eleven authentic case scenarios and 2 cases from participants' own practice environments acted as the basis for participants to create pharmaceutical care plans. Asynchronous online threaded discussions served as a forum for participants to discuss, develop, and publish their care plans. Other care plans were developed by participants individually and submitted to a private online logbook journal for marking and feedback from the instructor.
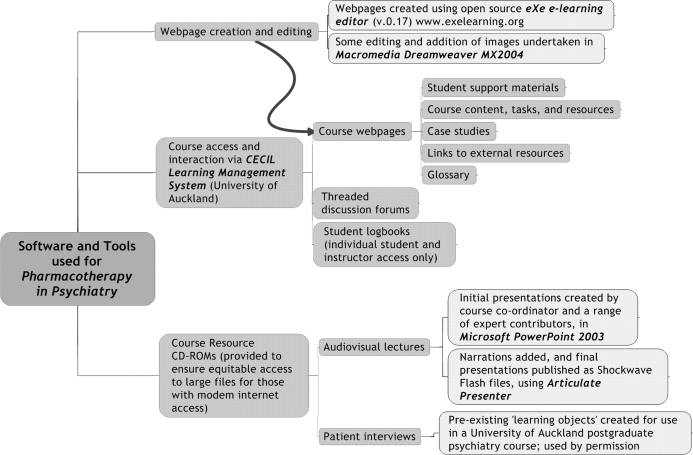
Participants drew upon a range of multimedia resources to complete the various course tasks. Web links to practice tools were provided, as was a link to a library resource site customized for the course with current research articles and links to other publications relevant to the field. The software and tools used for authoring, teaching, learning, and communication are outlined in Figure 1.
Figure 1.
Software and tools used for authoring, teaching and learning, and communication.
One month prior to its implementation, the online version of Pharmacotherapy in Psychiatry was assessed through a structured formative evaluation. Considering that a fully online method of delivering a postgraduate course was entirely new for the School, a thorough evaluation of the course needed to be conducted prior to course implementation. The evaluation was overseen by a member of the Faculty Education Unit who had not been involved in course development. There were 5 participants: 3 staff members of the School who had also been involved in running face-to-face postgraduate courses, a postgraduate student at the School, and a former student from the on-campus, face-to-face Pharmacotherapy in Psychiatry course offered in 2004. The participants in this evaluation had not previously seen the online version of the course, and had relatively high levels of computer literacy. They were all asked to complete a usability questionnaire, the results of which were used to make necessary changes prior to launching the course in the second academic semester of 2005.
Post-implementation, the course was assessed through student precourse and postcourse surveys. The purpose of these surveys was twofold: first, to act as an “advance organizer” by helping the students bring to mind relevant prior knowledge and bridge into new course concepts; and secondly, both the precourse and postcourse surveys helped to assess the impact of the course on the students' confidence and knowledge in the various aspects of psychiatric pharmacotherapy. Both survey instruments consisted of 18 multiple-choice questions divided into 3 broad areas of assessment:
The students' comfort level with the main concepts of pharmaceutical care in the area of mental health was self-assessed and defined as “very comfortable,” “comfortable,” “somewhat comfortable,” or “not comfortable” by answering questions on assessing patients with mental health conditions, designing a therapeutic plan for these patients, interpreting laboratory results and psychiatric testing scales, counselling mental health patients on their medications and other related issues surrounding therapy; and monitoring and following up with these patients.
The students' baseline knowledge on several basic mental health concepts and therapeutics was assessed by answering true or false questions, with each correct answer given a score of 1, for a maximum score of 10.
The students' self-assessment of their learning needs and reasons for taking the course were also surveyed.
The survey was designed to take approximately 5 to 10 minutes to complete. Students were asked to submit it prior to the course and again upon course completion.
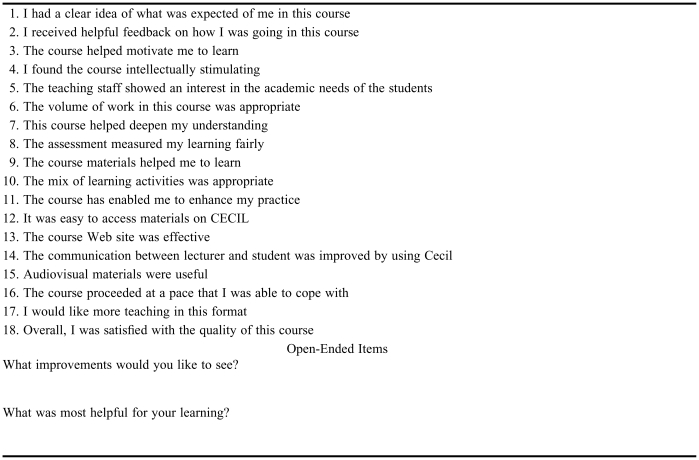
Finally, because Pharmacotherapy in Psychiatry was an elective course offered in the Master of Pharmacy Practice postgraduate program, a standard course evaluation had to be submitted to the Board of Studies. The University of Auckland's standard 11-item course evaluation questionnaire was varied to omit any reference to the physical environment and instead contained 8 additional questions regarding the e-learning format used (Appendix 1). Each question was assessed using a 5-point Likert scale on which 5 = strongly agree, 4 = agree, 3 = neutral, 2 = disagree, and 1 = strongly disagree. This questionnaire evaluated primarily the satisfaction of the students with the course design, content, workload, and assessment in relation to the learning objectives. The feedback provided in this overall course evaluation was also considered important as it provided information on the implications for developing other postgraduate courses that were to be offered by the School in a similar format.
ASSESSMENT
Fourteen students, including nurses and pharmacists, took the course during the first 2 years that the online program was available (5 in 2005, and 9 in 2006). The majority of the students were female (71%), pharmacists (71%), and from outside Auckland (71%). Eleven out of the 14 students (79%) completed both the precourse and postcourse surveys. Only 3 students were from Auckland; the remaining 11 students were geographically dispersed throughout the South and the North islands of New Zealand.
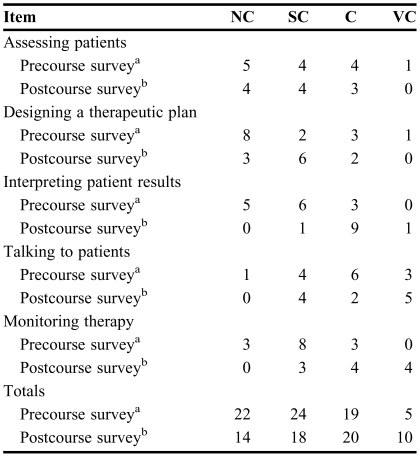
Table 2 presents the survey results regarding the students' comfort level with the main concepts of pharmaceutical care in the area of mental health. There was an overall trend for students' comfort levels with the various components of pharmaceutical care to increase by course completion, with an increase in the number of responses of “comfortable” and “very comfortable” (from 24 to 30), and a decrease in the number of responses of “not comfortable” and “somewhat comfortable” (from 46 to 32).
Table 2.
Students' Comfort Level With Pharmaceutical Care Planning in Mental Health (N = 14)
Abbreviations: NC = not comfortable, SC = somewhat comfortable, C = comfortable, VC = very comfortable
N = 14 students
N = 11 students
Average baseline scores of the students' knowledge of basic mental health concepts and therapeutics as assessed by the true/false nature of the survey questions were high (7 out of 10). The number of correct answers increased from the precourse to the postcourse test (average score 9 out of 10).
Overall, most students indicated the reason for enrolling in the course was because they were currently working with mental health clients and wanted to better understand the mechanism of action of psychotropic medications. At the beginning of the course, students indicated they were most knowledgeable about antidepressants; however, by the end of the course, this response changed to antipsychotics.
Only 8 of the 14 (57%) students who took the online version of Pharmacotherapy in Psychiatry completed the overall course evaluation. Most of the 8 students gave positive responses (agree or strongly agree) to the survey items. Specific findings from the overall course evaluation included:
Approval ratings for volume of work and course pace were only 30% and 33%, respectively.
Responses regarding multimedia delivery and online communication were generally positive, with 80% approving of the course Web site, 73% stating that the CECIL learning management system improved lecturer/student communication, and 65% responding that the audiovisual materials were useful.
Seventy-eight percent of students found the course intellectually stimulating and stated it helped deepen their understanding.
Seventy-five percent of students affirmed that the course had enabled them to enhance their practice, and 78% responded that they would like more teaching in this format.
DISCUSSION
The course Pharmacotherapy in Psychiatry is an example of how postgraduate and continuing education programs can enhance the skills of health care professionals and address limitations in undergraduate curriculums. In the area of mental health, programs like the one described in this paper may improve pharmacists' ability to meet the drug-related needs of the mentally ill. The increased uptake observed when this course was redesigned for online delivery indicates that this mode of delivery is favored compared to similar face-to-face educational programs.
The results of the various evaluations undertaken before and after the implementation of the online course are also indicative of positive learning outcomes. The precourse and postcourse survey results (albeit with a limited number of participants) showed an increase in comfort levels and baseline knowledge. In addition, the course evaluation survey results showed a 63% approval of overall course quality.
The workload and lack of flexibility associated with a paced, collaborative learning model requiring development of care plans across multiple cases may act to de-motivate students. However, this needs to be weighed against the high levels of student engagement and collaboration that were evident when meaningful learning was facilitated in this format.
The results of the various formal course evaluations, combined with the anecdotal observations of student online discussions, collaboration, and coursework submitted, also provide an opportunity to consider the validity of the learning principles underpinning the course design and the effectiveness of the strategies employed to implement them. The first learning principle stated that learning should be meaningful for the individual; what is learned is determined primarily by related prior knowledge and how that is activated. The applicability and value of this principle was evidenced by the students' engagement in online discussions, often evolving into discussion of students' own patients and workplace practices; also an increase in students' postcourse comfort and knowledge levels across the areas of practice with which scenarios and patient cases dealt; and the high student ratings of the intellectual stimulation, deepening of understanding, and enhancement of practice afforded by the course.
The course resources and case scenarios were structured around 5 core areas of mental health practice. Through development of care plans for multiple case scenarios in each area, discussion of alternative approaches with peers, review of model care plans provided, and instructor feedback on care plans completed individually, students engaged in varied and frequent tasks around the core concepts. All of these were in line with the principles that learning should be organized around core concepts and ideas in a field, with time spent “crisscrossing” the subject matter to build linkages between core concepts and varied examples and contexts of application; and that learning tasks should simulate or replicate workplace problems in authentic contexts. Support for the value of these principles for learning was provided by an increase in students' postcourse comfort levels across the areas of practice addressed by the scenarios and patient cases, and the high student ratings of the intellectual stimulation, deepening of understanding, and enhancement of practice that the course provided. However, the students' low approval ratings for volume of work and course pace indicated that the depth of engagement that the multiple case studies required was somewhat onerous.
The principle that learning should involve collaborative construction of knowledge through social negotiation underpinned learning activities throughout the course. These prompted online discussion of care plan formulation by students, and collaboration during the final module to produce a care plan for 1 of 2 cases. The readiness of students to engage with one another online regarding practice issues, and their fairly high rating of the ability of the university learning management system to improve communication, suggest that this principle is one that is important to student learning at this level. However, adopting the paced, collaborative course design model that this principle requires does mean some loss of flexibility; students cannot work through learning activities entirely at a pace that suits them, as reflected in low student ratings for course workload and pace.
The multimodal nature of information representation and pathways for student engagement built into the course reflects the application of the principle that learning should employ strategies that appeal to multiple sensory modes and cognitive capabilities. The high student approval ratings for the course Web site, the learning management system communication functions, and the audiovisual materials provided suggest that this principle was significant for the student learning experience. In addition, over three quarters of students responded that they would like to take more courses taught in this format.
The principle that learning tasks should help learners to develop metacognition and reflective practice was implemented through the audiovisual presentations by experts in the field of psychiatric pharmacotherapy, who modelled professional modes of thinking and problem solving in the mental health field. The requirement for students to articulate and justify their own approaches to care plan formulation, and the alternative perspectives provided across a large number of real and simulated cases by model care plans, together with peer and instructor feedback, acted to promote student reflection on their problem-solving strategies and professional practice. The value of this principle was demonstrated by high student ratings for deepening of understanding and enhancement of practice, along with increases in student comfort and knowledge levels across the areas of practice addressed by the course.
In terms of the design research approach we adopted, the findings above must be seen as tentative early steps in the process of theory construction. Data collected and observations made were insufficient to determine the relative significance for learning of each of the principles used to guide the course design, or the extent to which they are interdependent. It is reasonable also to assume that particular strategies employed to implement each principle must have influenced student engagement and learning outcomes.
SUMMARY
Flexible delivery courses may be an ideal way of reaching pharmacists interested in learning more about mental health care. The preliminary findings discussed above suggest that the online Pharmacotherapy in Psychiatry course provided the environment for a “community of practice” to develop between geographically dispersed mental health professionals.
Pharmacotherapy in Psychiatry was designed as a Web-based course structured around 6 core learning principles. Further research is required to clarify the role that the learning principles utilized are playing, individually and collectively, and the effects on learning of using alternative approaches to implement them.
The course was systematically implemented using formative evaluations, usability testing, and various forms of student feedback. The initial results indicate that this process achieved a good quality product and established a suitable template for future courses.
Course Evaluation Questionnairea
REFERENCES
- 1.Investing in Mental Health. The World Health Organization; Geneva, 2003. Available at: http://www.who.int/mental_health/media/investing_mnh.pdf. Accessed September 30, 2007.
- 2.Wells JE, Oakley Browne MA, Scott KM, McGee MA, Baxter J, Kokaua J. Te Rau Hinengaro: The New Zealand Mental Health Survey: overview of methods and findings. Aust N Z J Psychiatry. 2006;40:835–44. doi: 10.1080/j.1440-1614.2006.01902.x. [DOI] [PubMed] [Google Scholar]
- 3.Nurses, pharmacists and doctors rated most ethical and honest professions eleventh year in a row: Roy Morgan Research, Sydney 2004. Available at: http://www.roymorgan.com/news/polls/2004/3809/. Accessed September 30, 2007.
- 4.Bullman DC, Svarstad BL. Effects of pharmacist monitoring on patient satisfaction with antidepressant therapy. J Am Pharm Assoc. 2002;2:36–43. doi: 10.1331/108658002763538053. [DOI] [PubMed] [Google Scholar]
- 5.Phokeo V, Sproule B, Raman-Wilms L. Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55:1434–6. doi: 10.1176/appi.ps.55.12.1434. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J, Struening EL. Opinions about mental illness in the personnel of two large mental hospitals. J Abnorm Social Psychol. 1964;64:349–60. doi: 10.1037/h0045526. [DOI] [PubMed] [Google Scholar]
- 7.Howard MO, Chung SS. Nurses' attitudes toward substance misusers, II. Experiments and studies comparing nurses to other groups. Substance Use Misuse. 2000;35:503–32. doi: 10.3109/10826080009147470. [DOI] [PubMed] [Google Scholar]
- 8.The Mental Health and General Practice Investigation Research Group. General practitioners' perceptions of barriers to their provision of mental health care. N Z Med J. 2005;118:1222. Available at: http://www.nzma.org.nz/journal/118-1222/1654/. Accessed September 30, 2007.
- 9.Awad AG. Integrating a clinical review process with postgraduate training in clinical psychopharmacology. Qual Rev Bull. 1987;13:279–82. doi: 10.1016/s0097-5990(16)30145-2. [DOI] [PubMed] [Google Scholar]
- 10.Martin L, Saperson K, Maddigan B. Residency training: Challenges and opportunities in preparing trainees for the 21st Century. Can J Psychiatry. 2003;48:225–31. doi: 10.1177/070674370304800405. [DOI] [PubMed] [Google Scholar]
- 11.Clinton M, Hazelton M. Scoping mental health nursing education. Aust N Z J Ment Health Nurs. 2000;9:2–10. doi: 10.1046/j.1440-0979.2000.00155.x. [DOI] [PubMed] [Google Scholar]
- 12.Driscoll MP. Psychology of Learning for Instruction. 3rd ed. Boston: Allyn & Bacon; 2005. [Google Scholar]
- 13.Bransford J, Brown A, Cocking RR. How People Learn: Brain, Mind, Experience, and School. Expanded ed. Washington: National Academy Press; 2000. [Google Scholar]
- 14.Spiro RJ, Feltovich PJ, Jacobson MJ, Coulson RL. Cognitive flexibility, constructivism, and hypertext: random access instruction for advanced knowledge acquisition in ill-structured domains. In: Steffe LP, Gale J, editors. Constructivism in Education. Hillsdale, NJ: Erlbaum; 1995. pp. 85–107. [Google Scholar]
- 15.Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. New York: Cambridge University Press; 1991. [Google Scholar]
- 16.O'Donnell AM. The role of peers and group learning. In: Alexander PA, Winne PH, editors. Handbook of Educational Psychology. 2nd ed. Mahwah, NJ: Erlbaum; 2006. pp. 781–802. [Google Scholar]
- 17.Mayer R. The promise of multimedia learning: using the same instructional design methods across different media. Learn Instruction. 2003;13:125–39. [Google Scholar]
- 18.Schön DA. Educating the Reflective Practitioner. San Francisco: Jossey-Bass; 1987. [Google Scholar]
- 19.Reeves TC, Herrington J, Oliver R. Design research: a socially responsible approach to instructional technology research in higher education. J Computing Higher Educ. 2005;16:96–115. [Google Scholar]