Abstract
Objectives
To compare PharmD students' and preceptors' perceptions of preceptors' teaching behaviors.
Methods
A 47-item survey instrument was developed and distributed to students and preceptors for rating the frequency and adequacy of each teaching behavior as not done, done but inadequate, and well done and adequate.
Results
Seventy-seven (99%) students and 53 (55%) preceptors responded to the survey. Students were somewhat satisfied with their preceptors' teaching behaviors. In comparison, preceptors overrated their own teaching behaviors as well done and adequate on 9 of 47 (19%; p ≤ 0.05) items, with the majority being in the areas of providing feedback to students and evaluation.
Conclusion
Preceptors tended to overestimate the quality of their performance compared with students' evaluations. These findings suggest the need for a preceptor development program.
Keywords: teaching, perception, PharmD student, preceptor, assessment
INTRODUCTION
Following the adoption of pharmaceutical care (currently referred to as medication therapy management in the United States) as the primary mission for pharmacy practice, the doctor of pharmacy (PharmD) degree was adopted in the United States as the sole entry degree into the profession. The Faculty of Pharmaceutical Sciences at Naresuan University was the first of 14 colleges and schools in Thailand to switch to an all PharmD program (1999). While some faculties offer an optional PharmD degree, Naresuan University is now 1 of only 3 faculties that offer the PharmD degree for all students. At Naresuan University, throughout their final year, students gain experience in medication therapy management from 4 mandatory (medicine, ambulatory care, drug information, and community pharmacy) and 2 elective advanced pharmacy practice experience. These experiences focus on active learning, providing the student with structured practice opportunities, observation of preceptors, and case discussions. These practice-based experiences are designed in the problem-based learning model under the direction of the preceptor. At the completion of 6 advanced pharmacy practice experiences (APPE), students should have the necessary knowledge, skills, abilities, and attitudes to enable them to function effectively as members of an interdisciplinary healthcare team.
A study by Hill et al found that final-year pharmacy students' confidence in their drug knowledge and skills significantly increased after completing advanced pharmacy practice experiences.1 Similarly, in 81.5% of the evaluations, medical students felt that there was at least moderate improvement in their ability to perform selected competencies during the medical practice experiences. By the end of the practice experience, 85.3% of students were confident in performing the competencies most or almost all of the time.2 To achieve this goal, preceptors must assume the role of teacher, mentor, and evaluator by showing students how to apply knowledge learned in their didactic courses to daily practice and to share knowledge and skills with them. They also must assess the students' performance through systematic evaluations to continue to improve their strengths and correct their weaknesses. Although providing effective feedback to learners is an important aspect of clinical teaching, preceptors typically spend most of the time imparting clinical facts and pearls and devote less time to understanding the clinical thinking patterns and learning styles of students,3 possibly because most preceptors were trained to be practitioners rather than educators.
Previous studies have considered preceptorship from individual perspectives, such as that of students,4 teachers, or preceptors.5 The study by Kaviani et al highlightened the importance of formal preceptor preparation, which was shown to enhance teaching and learning opportunities for nursing students and personal and professional development of preceptors.6 For preceptors to take responsibility for improving their teaching skills, they must first develop a greater understanding of their current performance in relationship to professional expectations.7 Given these findings, final-year doctor of pharmacy students were asked to evaluate preceptors' skills in communication, pharmacy practice, teaching, and providing feedback and evaluation to students.
METHODS
In June 2006, a 47-item survey instrument was constructed to evaluate preceptors' teaching skills and behaviors. Several of the survey items were adapted from previously conducted surveys8-15 A pilot survey instrument was sent to students and preceptors who had completed their first advanced pharmacy practice experience and their feedback was used to revise the survey instrument. Naresuan University's investigational review board approval was obtained to conduct the survey.
The revised survey instruments were immediately distributed to 77 students and mailed to 53 preceptors who had participated in a second advanced pharmacy practice experience from May 1, 2006, to June 14, 2006. One follow-up telephone call was made to nonresponders. Survey participants were asked to rate the frequency and adequacy of each teaching skill or behavior on a scale of 1 to 3 on which 1 = not done, 2 = done but inadequate, and 3 = well done and adequate. Participation in the survey was voluntary and anonymous and no compensation was given. Students completed their survey instruments prior to receiving their advanced practice experience grade, which was assigned after the sixth practice experience. Preceptor and student responses were analyzed separately and differences between their perceptions of preceptor teaching skills and behaviors were evaluated. The percentage and median scores rated for each teaching behavior item were calculated and subjected to statistical analysis. The Mann-Whitney rank sum test was used because it allowed the researchers to compare differences between 2 independent samples. The level of significance was set a priori at 0.05. Survey data were analyzed using SPSS Version 11.5 (SPSS Inc, Chicago, IL).
RESULTS
Seventy-six students (99% response rate) and 29 (55% response rate) preceptors completed the survey. Most of preceptors had been assigned 1 to 2 students during the pharmacy practice experience.
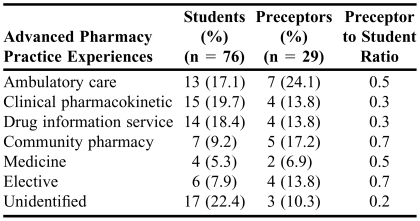
The number of respondents that participated in individual advanced pharmacy practice experiences and the ratio of preceptors to students are shown in Table 1. The ratio of preceptors to student response rates were 0.7, 0.7, 0.5 and 0.5 in community pharmacy, elective, ambulatory care, and medicine practice experiences, respectively. However, the numbers of students and preceptors involved in each practice setting were too small, so differences of perceptions between students and preceptors in specific settings could not be compared.
Table 1.
Students and Preceptors Divided by Types of Advanced Pharmacy Experience
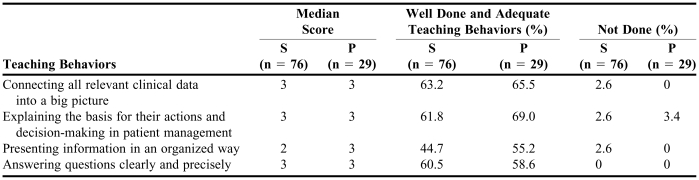
The student assessment of preceptor teaching behaviors and preceptors' assessment of themselves are summarized in Table 2, 3, and 4. Most students rated their preceptors' teaching behaviors as well done and somewhat satisfied.
Table 2.
Median Scores and Percentage of Rated Teaching Behaviors as Perceived by Students and Preceptors in Preceptor Communication Skills Domain
P = preceptors; S = students
ap < 0.05
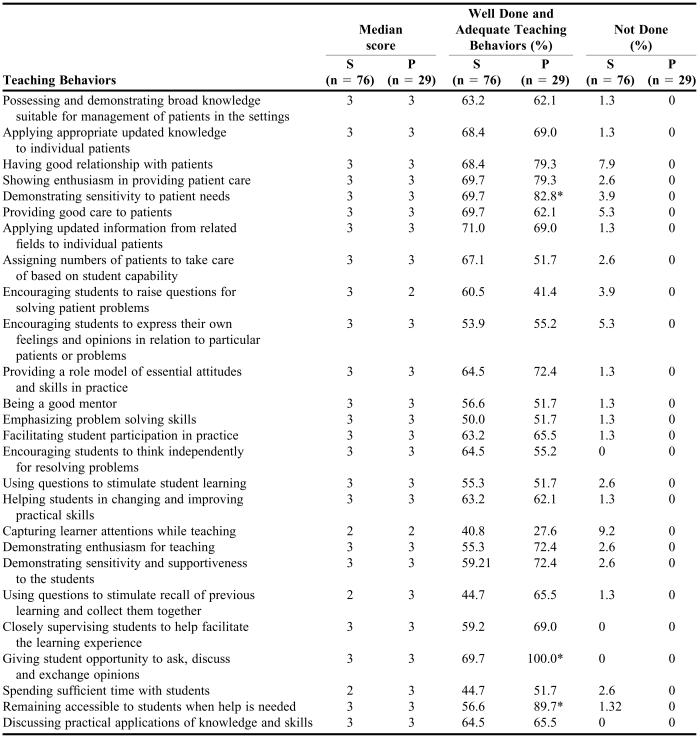
Table 3.
Median Scores and Percentage of Rated Teaching Behaviors as Perceived by Students and Preceptors in Preceptor Skills in Practice and Teaching Domain
P = preceptors; S = students
ap < 0.05
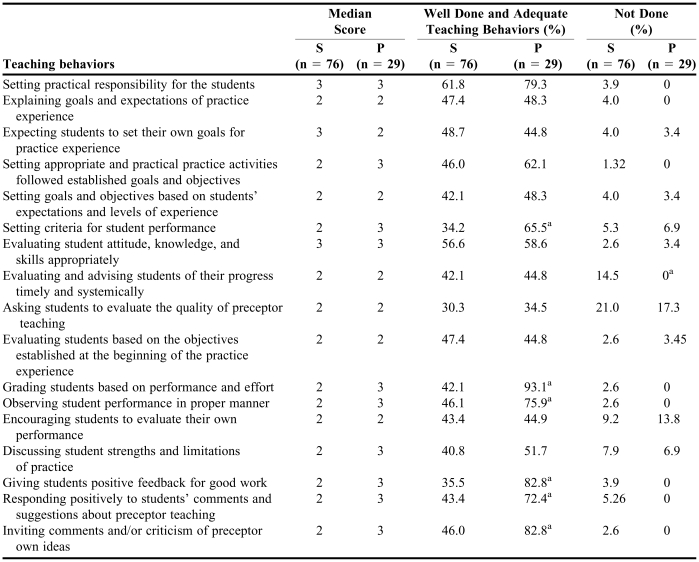
Table 4.
Median Scores and Percentage of Rated Teaching Behaviors as Perceived by Students and Preceptors in Preceptor Feedback and Evaluation Domain
P = preceptors; S = students
p < 0.05
Compared to students' ratings, preceptors did not overrate their teaching behaviors in any of the 4 items in the area of preceptor communication skills (Table 2). However, they did overrate their teaching behaviors in comparison to the students' evaluations for well done and adequate teaching behaviors in 3 of 26 (12 %) items in the domain of skills in practice and teaching, and 6 of 17 (35 %) in the domain of feedback and evaluation, respectively (p ≤ 0.05). In the domain of well done and adequate teaching behaviors, the items on which preceptors overrated themselves in comparison to student evaluations were in their ability to demonstrate sensitivity to patient needs; giving the student the opportunity to ask questions and discuss and exchange opinions; and remaining accessible to students when help was needed. In the domain of feedback and evaluation, preceptors thought that their behaviors were more adequate than did students in setting criteria for student performance; grading students based on performance and effort; observing student performance in a proper manner; giving students positive feedback for good work; responding positively to students' comments and suggestions about preceptor teaching; and inviting comments and/or criticism of preceptors' own ideas (p ≤ 0.05).
In the area of preceptor skills in practice and teaching (Table 3), only 27.6 % of preceptors thought they captured their student's attention well while teaching, although the rest stated that they did not do this well enough. However, 41% of the students rated their preceptors' performance as well done and adequate on this item. All preceptors stated that they did well in giving their student(s) opportunities to ask, discuss, and exchange opinions, but only 70% of students indicated this was done well by their preceptor. Another discrepancy occurred between students' and preceptors' perceptions concerning evaluation and advising. While preceptors believed they evaluated and advised students of their progress in a timely and systemic manner, 14.5% of students stated their preceptors did not complete these teaching behaviors at all.
Seventeen behaviors were assessed in the area of feedback and evaluation of students. In the area of preceptor teaching (Table 4), about one third of students and preceptors thought preceptors asked students to evaluate the quality of preceptor teaching; however, 21.0% of students and 17.2 % of preceptors, respectively, said preceptors did not ask students to evaluate the quality of their teaching. Fourteen percent of preceptors indicated they never encouraged students to evaluate their preceptor's performance, while students gave more credit to their preceptors.
The teaching behavior items with which both students and preceptors agreed were that preceptors answered questions clearly and precisely; encouraged students to think independently when resolving problems; closely supervised students to help facilitate the learning experience; gave students the opportunity to ask, discuss, and exchange opinions; and discussed practical applications of knowledge and skills. Ratings on all 17 items can be seen in Table 4.
DISCUSSION
The overall results of this 47-item survey used to evaluate the core teaching principles in the area of communication, practice, teaching, and feedback and evaluation showed general agreement between students and preceptors on 35 of the 47 behaviors evaluated. Students' and preceptors' opinions were significantly different on only 8 items, which were noted in the results above and will be discussed here. However, there are some limitations to the study that should be elucidated. First, quality and adequacy of preceptor teaching behaviors were assessed by subjective perceptions rather than objective measures. Second, preceptor recall bias may have occurred since some preceptors sent the survey instrument back a month after students finished the second APPEs. The response rate among preceptors was less than that among students, probably because students were required to complete the survey instrument in a classroom setting after completion of the APPE, while preceptors' participation in the survey was self-motivated and optional. Third, the items in the survey instrument did not include all possible behaviors, ie, there may be other behaviors that could have been included. Thus, study conclusions may not be applicable to other groups of preceptors and caution should be used in applying these findings to all preceptors.
Students were somewhat satisfied with their own teaching behaviors. Preceptors tended to overestimate their performance compared with student evaluations of their performance, although most of these differences in ratings did not reach statistical significance. Preceptors rated themselves significantly higher on 9 of 47 survey items compared with students' ratings of their preceptor. Most preceptors overrated themselves on their provision of evaluation and feedback to their students, especially on setting criteria, grading, observing, giving positive feedback, and responding positively to students' comments and suggestions. A small number of students and preceptors agreed that preceptors did not ask students to evaluate the quality of their teaching, encourage students to evaluate their own performance, or discuss student strengths and limitations of practice. One problem that preceptors apparently had was capturing the student's attention when teaching.
Students appeared to be less satisfied with their preceptor's performance, especially in the area of preceptors providing feedback and evaluation. Perhaps students wanted to improve their performance to complete preceptors' objectives. However, students might not insist on getting feedback and evaluation when they did not have one. For learners to grow and improve their skills, they need to know what they are doing well, as well as where they need to improve. As clinical teachers, preceptors should provide ongoing feedback. Effective evaluation also helps a learner assess his or her strengths and weaknesses, identify strategies for improvement, and continue professional growth and development. Schultz and colleagues reported that 95.6% of 1,529 medical students and residents surveyed believed that feedback was important for learning.15 Learners ranked “gives constructive feedback” as second in importance and “gives timely feedback” as sixth out of 37 preferred preceptor behaviors.15 In a study of 82 internal medicine practice experience students, Torre and colleagues reported that “high-quality feedback” was the learning activity most strongly associated with learners' perceptions of high-quality teaching.16 In contrast, only 32.7% of third-year medical students rated that receiving feedback from the preceptor on their performance was a helpful curriculum component.2 One observational study found that giving feedback was provided in only 9.4% of community-based preceptors for a family and community medicine practice experience.17 The feedback tended to be positive; however, 52% of ambulatory care preceptors did provide feedback as observed by medical students.18 In the final evaluation sessions, Huang et al found that preceptors often discussed the medical students' skills and performances (75%), but the students were less frequently allowed to discuss the preceptor's performance (25%).17 This study also found that feedback was not often provided in most medical teaching encounters18,19 Dobbie et al recommended to give learner feedback, be clear about when, where, and how preceptor plan to give feedback, acknowledge potential gender differences in giving and receiving feedback, give feedback orally and/or in written format, and give privately negative or constructive feedback when required.20 If preceptors provide feedback and evaluation, students are more likely to give them better evaluations and be more satisfied with the teaching process.
Our study found that preceptors were mostly rated lowest on their provision of feedback to students, while preceptors were rated higher on skills of communication, both in practice and while teaching. Educators have the responsibility to anticipate and lead change in pharmacy practice. Thus, student input is important to help colleges and schools identify areas in which preceptors need improvement and the level of emphasis of these skills to prepare preceptors being better teachers. The program needs to provide opportunities for preceptors to guide discussions, encourage students, model self-reflective behavior, value student self-assessment, and provide feedback on students' reflections. Studies have demonstrated that preceptor can learn to be effective teachers.21,22 After a set of three 90-minute faculty development seminars scheduled 1 week apart, giving feedback to learners by teachers in ambulatory setting was increased from 17% to 22% (p = 0.09), and feedback was more likely to be specific (9% vs. 15%; p = 0.02).19 After the workshops, preceptors reported that they were better at letting the students reach their own conclusion (p = 0.001) and at evaluating the learners (p = 0.03).19
CONCLUSION
This survey identified the perceptions of students and preceptors about 47 preceptor teaching behaviors in the areas of communications, practicing and teaching, and giving feedback and evaluation to students.
To improve the quality of experiential education, we must teach preceptors and create programs to guide them in their development and encourage their continual development. We must also make students aware of their right to get feedback and evaluation from preceptors since these are essential to students achieving curriculum goals.
This survey was a good start in identifying areas where preceptor development is needed and which teaching behaviors should be continued and which need improvement. Furthermore, a formal preceptor development program is needed to resolve the teaching problems identified by this survey.
ACKNOWLEDGEMENT
The author wishes to express her sincere gratitude to Professor Gary H. Smith, PharmD, FASHP, FCCP, for his expert advice and immeasurable editorial assistance on this manuscript.
REFERENCES
- 1.Hill LH, Kirkwood CK. Student and preceptor perception of performance in advance pharmacy practice experiences. Am J Pharm Educ. 2005;69:467–74. [Google Scholar]
- 2.Brody DS, Ryan K, Kuzma MA. Promoting the development of doctoring competencies in clinical settings. Fam Med. 2003;36:S105–9. [PubMed] [Google Scholar]
- 3.Lucas J, Baxley E, Witherspoon P. Walking the balance BEAM: the art and science of becoming a successful clinical teacher. Fam Med. 2002;34:498–9. [PubMed] [Google Scholar]
- 4.Earnshaw GJ. Mentorship: the students' views. Nurse Educ Today. 1995;15:274–9. doi: 10.1016/s0260-6917(95)80130-8. [DOI] [PubMed] [Google Scholar]
- 5.Dibert C, Goldenberg D. Preceptors' perceptions of the benefits, rewards, supports and commitment to the preceptor role. J Adv Nurs. 1995;21:1144–51. doi: 10.1046/j.1365-2648.1995.21061144.x. [DOI] [PubMed] [Google Scholar]
- 6.Kaviani N, Stillwell Y. An evaluative study of clinical preceptorship. Nurse Educ Today. 2000;20:218–26. doi: 10.1054/nedt.1999.0386. [DOI] [PubMed] [Google Scholar]
- 7.Sachdeva AK. Preceptorship, mentorship, and the adult learner in medical and health sciences education. J Cancer Educ. 1996;11:131–6. doi: 10.1080/08858199609528415. [DOI] [PubMed] [Google Scholar]
- 8.CDC travel information. Effective preceptor. Atlanta (GA): Centers for Disease Control and Prevention. Available at: http://www.mtn.ncahec.org/pdp. Accessed May 20, 2006.
- 9.CDC travel information. The one-minute preceptor. Atlanta (GA): Centers for Disease Control and Prevention. Available at: http://www.mtn.ncahec.org/pdp. Accessed May 20, 2006.
- 10.CDC travel information. Feedback. Atlanta (GA): Centers for Disease Control and Prevention. Available at: http://www.mtn.ncahec.org/pdp. Accessed May 20, 2006.
- 11.CDC travel information. Setting expectations. Atlanta (GA): Centers for Disease Control and Prevention. Available at: http://www.mtn.ncahec.org/pdp. Accessed May 20, 2006.
- 12.CDC travel information. Evaluation: Making it works. Atlanta (GA): Centers for Disease Control and Prevention. Available at: http://www.mtn.ncahec.org/pdp. Accessed May 20, 2006.
- 13.Langlois JP, Thach SB. Bringing faculty development to community-based preceptors. Acad Med. 2003;78:150–5. doi: 10.1097/00001888-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Administrative Clinical Clerkship Coordination Committee. Pharmaceutical Care Clerkship Manual 2006. 7th ed. Phisanuloke Naresuan University 2006.
- 15.Schultz KW, Kirby J, Delva D, et al. Medical students' and residents' preferred site characteristics and preceptor behaviors for learning in the ambulatory setting: a cross-sectional survey. BMC Med Educ. 2004;4:12. doi: 10.1186/1472-6920-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Torre DM, Sebastian JL, Simpson DE. Learning activities and high-quality teaching: perceptions of third-year IM clerkship students. Acad Med. 2003;78:812–4. doi: 10.1097/00001888-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Huang WY, Monteiro FM. Teaching behaviors used by community-based preceptors for a family and community medicine clerkship. Fam Med. 2000;32:678–80. [PubMed] [Google Scholar]
- 18.Kernan WN, Holmboe E, O'Connor PG. Assessing the teaching behaviors of ambulatory care preceptors. Acad Med. 2004;79:1088–94. doi: 10.1097/00001888-200411000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Salerno SM, O'Malley PG, Pangaro LN, Wheeler GA, Moores LK, Jackson JL. Faculty development seminars based on the one-minute preceptor improve feedback in the ambulatory setting. J Gen Intern Med. 2002;17:799–87. doi: 10.1046/j.1525-1497.2002.11233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dobbie A, Tysinger JW. Evidence-based strategies that help office-based teachers give effective feedback. Fam Med. 2005;37:617–9. [PubMed] [Google Scholar]
- 21.White CB, Bassali R, Heery LB. Teaching residents to teach. An instructional program for training pediatric residents to percept third-year medical students in the ambulatory clinic. Arch Pediatr Adolesc Med. 1997;151:730–5. doi: 10.1001/archpedi.1997.02170440092016. [DOI] [PubMed] [Google Scholar]
- 22.Furney SL, Orsini AN, Orsetti KE, Stern DT, Gruppen LD, Irby DM. Teaching the one-minute preceptor. A randomized controlled trial. J Gen Intern Med. 2001;16:620–4. doi: 10.1046/j.1525-1497.2001.016009620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]