Abstract
Objectives
To survey pharmacy preceptors regarding experiential education and determine the implications of the findings on colleges and schools of pharmacy.
Methods
An online survey was sent to 4,396 experiential sites. The survey instrument consisted of 41 questions regarding the experiential education environment from the preceptor's perspective (eg, experiential load, time-quality issues, compensation, etc).
Results
One thousand one hundred sixty-three preceptors responded (26.5%) to the survey. Concerning experiential load, 73% took 2 or more students in the past year and almost half of the sites had to turn placements away. Nearly all preceptors felt that the more time they spent with students, the higher quality the experience, and 20% felt they didn't have enough time to provide a quality experience. Thirty-six percent of respondents chose monetary stipend as the form of compensation they valued most.
Conclusions
This study provides insights into the issues that concern volunteer preceptors and the findings could be used to enhance the quality of experiential education in pharmacy.
Keywords: preceptor, experiential education, rotation, clerkship, advanced practice experiences
INTRODUCTION
Experiential education is an integral part of the pharmacy curriculum, constituting at least 30% of the professional curriculum. According to the most recent Accreditation Council for Pharmacy Education (ACPE) Standards and Guidelines, the curriculum must include introductory pharmacy practice experiences (IPPEs) at “not less than 5% curricular length” and advanced pharmacy practice experiences (APPEs) at “not less than 25% curricular length,” which equates to approximately 300 hours of IPPEs and 1,440 hours of APPEs throughout the pharmacy curriculum.1 Previous ACPE Standards did not stipulate a required number of IPPE or APPE hours; thus, most colleges and schools had significantly less than 300 hours of IPPE curriculum requirements. To meet this increased experiential demand, colleges and schools of pharmacy need additional quality preceptors to teach pharmacy students in various pharmacy practice settings.
In addition to the increased experiential education demand within the practice environment, there is also a pharmacist workforce shortage in the United States.2 The 2008-09 Bureau of Labor Statistics Occupational Outlook Handout states that
…excellent opportunities are expected for pharmacists over the 2006-2016 period. Job openings will result from rapid employment growth, and from the need to replace workers who retire or leave the occupation for other reasons. Employment of pharmacists is expected to grow by 22 percent between 2006 and 2016, which is much faster than the average for all occupations. The increasing numbers of middle-aged and elderly people—who use more prescription drugs than younger people—will continue to spur demand for pharmacists throughout the projection period.3
Student enrollments are increasing in existing colleges and schools and several new college and schools of pharmacy are opening. In July 2007, there were 99 accredited colleges and schools according to ACPE, with an additional 3 colleges/schools classified as precandidate status.4 By comparison, there were 87 accredited colleges/schools in 2004. These 12 additional colleges/schools means there are approximately 1,200-1,500 additional students per professional year in the curriculum. The number of graduates has increased by 40% since 2004. As of October 2008, there are 110 accredited colleges/schools of pharmacy in the United States and an additional 4 colleges/schools that have submitted new school applications.5
The increased experiential education requirements, expanding student enrollment in existing colleges/schools, and opening of additional colleges/schools are creating challenges for new and existing colleges and schools. A number of surveys have collected data from colleges and schools about experiential workload challenges6,7; however, information regarding advanced experiential education that conveys volunteer preceptors' perceptions is lacking in the literature. The purpose of this survey was to obtain volunteer preceptor perspectives of their advanced experiential student workload, time-quality issues, and compensation.
METHODS
A survey instrument was created in FrontPage using cross-sectional quantitative methodology.8 Nine colleges/schools (5 private and 4 public) from various regions of the United States, sent the survey instrument to their volunteer preceptors, who represented a cross-section of colleges/schools and preceptor demographics. Experiential education administrators and preceptors from the following colleges/schools participated in the study: Creighton University School of Pharmacy and Health Professions, Drake University College of Pharmacy and Health Sciences, Ohio Northern University College of Pharmacy, The University of Connecticut School of Pharmacy, University of Maryland School of Pharmacy, Nova Southeastern University College of Pharmacy, Xavier University of Louisiana College of Pharmacy, University of California at San Francisco School of Pharmacy, and University of Washington School of Pharmacy. The project was approved by each university's institutional review board.
Approximately 60% of APPEs are taught by volunteer preceptors.7 Thus, the survey instrument was only sent to volunteer preceptors (ie, those not paid by the university to teach students). Faculty members who served as preceptors were not included because precepting APPE students was their primary responsibility and an expected part of their job requirement.
The survey instrument consisted of 41 questions. Experiential workload was evaluated by gathering information from the previous year about the number of students that were precepted, the number of colleges/schools partnered with to take students, the number of placement requests, the number of times preceptors could not take students when requested, and characteristics preceptors use in determining which students to accept when the requests outnumbered the openings available. Preceptors were asked whether student placements had increased, and if so, to rank the reasons for the increase. Preceptors were also asked to rank their top 3 considerations when determining which students to precept when demand was more than they could accommodate.
Preceptors were asked how much time they spent with their students per week, whether the amount of time spent with students increased the quality of the experience, and whether they felt they spent enough time with their students to provide a quality experience. Several questions were also asked to evaluate the compensation of APPE sites for precepting students, such as the most valuable form of compensation, as well as whether compensation was required, amount of compensation, and where the stipend went if one was required.
Preceptor demographics were collected regarding gender, race, terminal degree, number of years in pharmacy practice, number of years at current site, number of years they have precepted students, and the title that best described their role or relationship to pharmacy students. Site characteristics such as state where located, population density, type of pharmacy practice setting, and whether their site was private or public were also collected.
The survey instrument was pilot tested with a representative cross-sectional group of preceptors and changes were made based on the group's feedback. An e-mail containing a link to the online questionnaire was then sent out to 4,396 volunteer preceptors from the 9 participating colleges and schools. Each college's or school's experiential education director/assistant director sent the original e-mail message and 2 follow-up reminders to the volunteer preceptors in their database over a 4-week period in 2006.
Data from the survey instrument were entered into SPSS, version 14.0 (Statistical Package for the Social Sciences, Inc., North Chicago, IL) for analysis. Data were analyzed using reported frequencies and descriptive statistics.
RESULTS
One thousand one hundred sixty-three preceptors responded to the survey (response rate = 26.5%). Thirty-three respondents described themselves as full-time faculty members and therefore their data were excluded from the results.
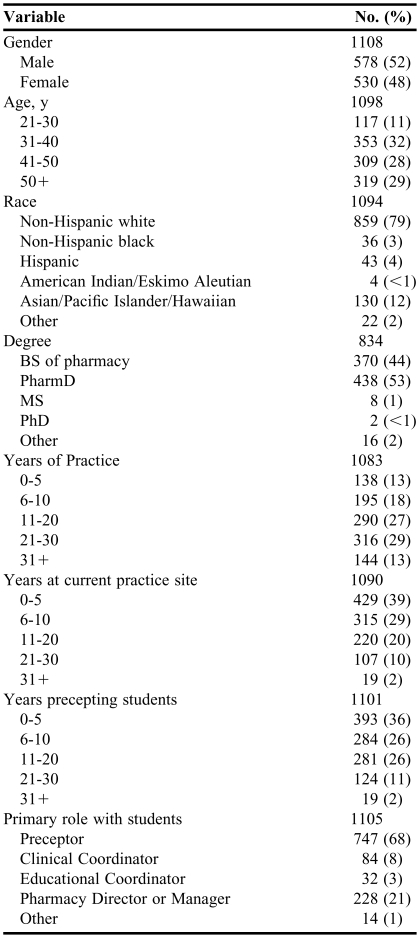
Preceptor demographics are listed in Table 1. The majority of the respondents were more than 30 years of age and males slightly outnumbered females. Nearly 80% of respondents were non-Hispanic white. Approximately half had earned a doctor of pharmacy (PharmD) degree (53%), while 44% held a bachelor of science (BS) degree in pharmacy. The majority (69%) of respondents reported that they had practiced pharmacy for 11 or more years. The number of years working at the current practice site varied. Approximately half (51%) had been precepting students 6 to 20 years. The majority of respondents (68%) indicated that their primary role with students was as a preceptor, followed by 21% as a director/manager, and 11% as a clinical or educational coordinator.
Table 1.
Pharmacy Preceptor Demographicsa
The number of respondents varied due to missing data for the different items
Abbreviations: BS = bachelor of science; PharmD = doctor of pharmacy; MS = master of science; PhD = doctor of philosophy
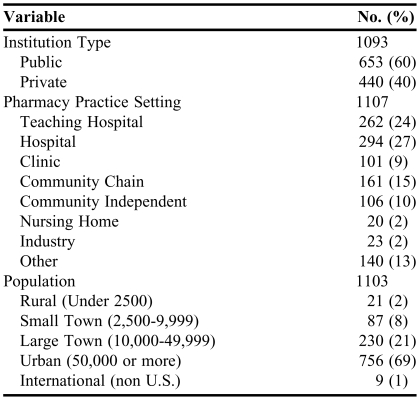
The site demographics are listed in Table 2. Sixty percent of the respondents were affiliated with public institutions and 40% were affiliated with private institutions. Approximately half worked in hospitals and a fourth worked at community sites.
Table 2.
Preceptor Site Featuresa
The number of respondents varied due to missing data for the different items
Nearly all of the respondents (90%) precepted at sites located in urban areas or large towns. Respondents represented 46 states, plus the District of Columbia. The states with the most respondents were California (15%), Washington (10%), Florida (10%), and Maryland (9%).
The majority of sites had precepted more than 1 student during the previous year. Forty-three percent of respondents (485/1126) indicated they had precepted 2-5 students in the last year. This was followed by 19% precepting 6-10 students (214/1126) and 16% (179/1126) precepting only 1 student in the past year.
More than half of the sites surveyed were working with 2 or more colleges/schools for student placements. Fifty percent (563/1126) of respondents indicated that they had accepted students from 2-5 different colleges/schools in the past year.
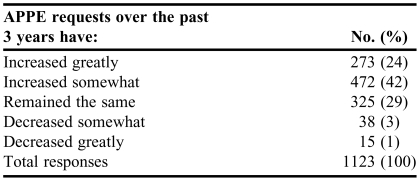
Two thirds of respondents indicated that requests for student placement/APPE positions had increased either “somewhat” or “greatly” over the past 3 years, and about 30% of respondents indicated that the number of requests was the same (Table 3). The highest ranked reason for the increase in number of student requests for APPEs was increased enrollment in existing colleges and schools of pharmacy, followed by increased number of new colleges and schools of pharmacy, and decreased sites available that could offer quality experiences.
Table 3.
Advanced Pharmacy Practice Experience (APPE) Requests
Forty-seven percent (408/871) of site preceptors responded that they had to deny placement of 1 or more students in the past year; however, 53% (463/871) stated that they did not turn any students away. The most common reason for turning students away was pharmacy staff workload (31%), followed by an increase in requests (22%).
When demand for student placements was high, “local school commitment” (47%) and “first-come, first-served” (46%) were most frequently ranked highest as considerations for determining whether or not they would take students.
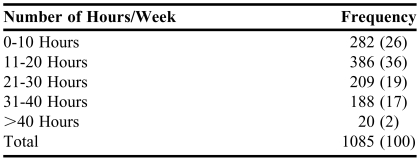
Time spent with rotation students varied among the respondents. Thirty-six percent indicated they spent 11-20 hours/week with their APPE students, while 26% spent 0-10 hours/week with their APPE students (Table 4).
Table 4.
Time Spent with Advanced Pharmacy Practice Experience Students, No. (%)
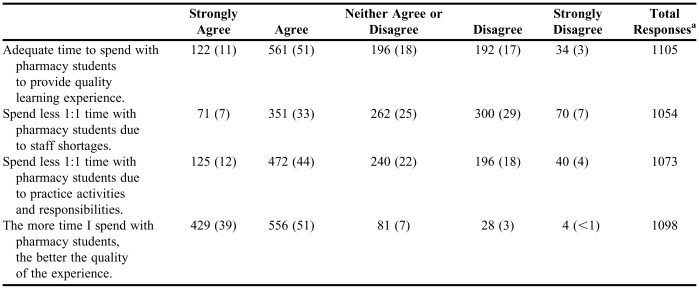
Preceptors were asked to respond to several questions regarding time and quality issues in the experiential environment (Table 5). Ninety percent of respondents stated they strongly agreed or agreed that the more time they spent with students, the higher quality the experience. Sixty-two percent strongly agreed or agreed that they had adequate time to spend with students to provide a quality experience.
Table 5.
Preceptors' Responses to Survey Questions Regarding Time Spent With Students and Quality of Advanced Pharmacy Practice Experiences, No. (%)
The number of preceptors responding to each item varied
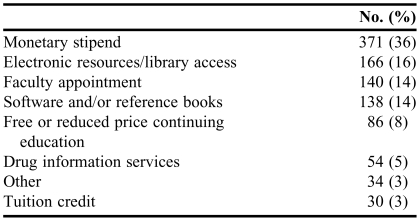
Several questions were asked regarding compensation for precepting students. Fifty-six percent (608/1085) indicated that they accepted compensation, but only 10% (99/1025) indicated that they required compensation. When asked what form of compensation was most valuable to them, approximately a third ranked monetary stipend highest (Table 6).
Table 6.
Forms of Compensation Considered Most Valuable (N = 1019)
Respondents were instructed to answer additional compensation questions only if they required compensation (n = 99); however, not all respondents in this category answered all of the questions. In addition, with regard to the colleges/schools participating in sending this survey to their preceptors, one college/school pays all of their experiential sites, some colleges/schools do not pay any of their sites, and the majority of the colleges/schools have the ability to pay a stipend depending on the situation.
Preceptors who required compensation for APPEs (n = 99) were asked to report the required dollar amount and 83% (n = 82) responded. The median amount was $500 (range = $75 to $2,000) per student APPE. The mean amount was $486 (standard deviation ±$268).
Only 7% (6/90) of respondents started requiring stipends in the past year and 33% (68/204) of respondents indicated they required a stipend to compensate for the additional workload created by precepting students along with other job responsibilities. Thirty-six percent (32/88) indicated that the stipend went into pharmacy development funds for preceptor use, 25% (22/88) indicated that it went into the pharmacy administration budget, 11% (10/88) into the general hospital budget, and 10% (9/88) directly to the preceptor as cash. Sixty-eight percent (38/56) indicated they would not precept students without a monetary stipend, and 32% (18/56) indicated they would.
DISCUSSION
Preceptor demographics, such as gender and years of practice, were similar to demographics reported in the AACP Pharmacy Preceptor Survey for 2007.9 Therefore; the authors believe that the preceptor population was well-represented in this survey. Also, preceptors responded from all regions within the United States, representing an adequate cross-section of respondents. California was the most highly represented state in the survey because several of the colleges/schools that participated in this study had APPE agreements with California sites.
Experienced quality preceptors are a valuable asset to colleges and schools. Most of the respondents were experienced and had been at their practice sites for several years, with the majority having more than 11 years of experience and approximately 50% having been at their current sites for 6 or more years. Reasons for this may be that some states require a minimum number of years in practice or post graduation prior to allowing pharmacists to serve as preceptors and/or younger pharmacists are establishing themselves and may not feel comfortable becoming preceptors immediately. Pharmacy education leaders should take a look at other health professions, such as physical therapy, which have an accreditation standard that requires students to learn to teach as part of the professional curriculum. With that type of model, students are equipped with the skills needed to precept and are capable of serving as preceptors sooner after graduation. Colleges/schools and residency programs should seriously consider this when evaluating what is important to include in the pharmacy curriculum. This practice would also lay a solid foundation for additional preceptor development and professional growth post graduation.
Half of the respondents were from hospital settings and the other half were divided among various other types of practice sites. Colleges/schools have typically emphasized hospital practice, especially since the advent of the first professional degree PharmD curriculum. Despite the focus on hospital and acute care patient management within the curriculum, the majority of pharmacy graduates practice in community-based settings. Academia has been charged with helping to lead the advancement of community practice to incorporate additional medication therapy management services and patient-care-oriented programs. Colleges and schools need to evaluate the emphasis on hospital practice and consider shifting some resources to ambulatory-based and community practice programs.
Approximately 90% of sites in the survey were from urban or large population areas. Most colleges and schools of pharmacy are located in areas with larger populations. Thus, the majority of preceptor sites are located in close proximity to the schools. College/school leaders should explore opportunities to reach out to rural areas for additional sites. In addition to meeting the need for additional experiential sites for colleges/schools, such relationships would expose students to pharmacy practice in rural areas where larger pharmacy workforce shortages exist.10
National volunteer preceptor data concerning workloads has not been published in previous studies, so it is important to note that 73% of sites took 2 or more students in the past year. Experiential office faculty members are striving to meet quality assurance standards as well as preceptor development needs. Logistically, it may be more efficient to assign more students (scheduled throughout the year) to each site, which would also give experiential office faculty members fewer sites to oversee and opportunity to interact more frequently. Also, by having more students on a routine basis rather than intermittently, preceptors would gain valuable experience that would make them better educators. It would also be easier for preceptors to effectively integrate students into practice activities if students are at the site consistently throughout the year. Another advantage to consistently having students present is that it would allow others at the practice to better understand why the students are there and what they should be doing. Over time, the preceptor and other staff members would come to expect and depend on student participation in site activities.
Standards regarding ideal student-to-preceptor ratio do not exist and remain to be developed. This is an issue that warrants additional attention as experiential program administrators continue to struggle with the challenges of ensuring quality sites and preceptors while still being able to offer a variety of experiences to students.
More than half of the site representatives completing the survey instrument indicated that they took students from more than 1 college/school. This means that the majority of sites are dealing with students from various colleges/schools and, thus, various educational backgrounds, which may be challenging when determining appropriate teaching level. Regional experiential faculty groups are organizing and meeting regularly to standardize such things as learning objectives, forms, schedules, etc, in an attempt to simplify the process for sites and preceptors. This should continue to be a priority since the overlap will continue to increase as more new colleges and schools of pharmacy are opening and enrollments at existing colleges and schools are increasing. Standardization of student evaluation forms and procedures may decrease the complications of having students from different colleges/schools.
Two thirds of preceptors indicated that requests had increased over the past few years and almost half had to decline to accept students for courses/experiences in the past year. Colleges and schools of pharmacy are increasingly placing higher demands on sites to precept students and many are forced to turn students away. Experiential program administrators need to work closely with managers and preceptors at new and potential sites to determine how to accommodate increasing demands. Development of best practice models for precepting and streamlining administrative responsibilities associated with precepting, such as the use of a universal student evaluation form, could help preceptors work more efficiently with students and colleges/schools.
Most sites were precepting several students per year, therefore preceptor education that teaches personnel at these sites how to balance teaching with their other practice responsibilities is important. Accepting students from local colleges/schools and on a “first-come, first-served” basis were cited by preceptors as the most common ways of prioritizing the acceptance of students for APPEs when demand was more than they could accommodate. Schools in close proximity (local) typically have an advantage over distance sites because there is a higher probability that many of the local site's preceptors are alumni for that school and therefore more familiar with the program. The increasing number of programs with multiple campuses and distance-based elements creates challenges for local colleges/schools as they compete for sites and preceptors. Colleges/schools whose APPE needs overlap with those of other colleges/schools should work together to accommodate their needs.
“First-come, first-served” as a way of prioritizing student placement encourages colleges/schools to contact sites earlier in the scheduling process to secure APPE placements. Scheduling too far in advance creates challenges for both parties as experiential administrators are busy working with their students who are currently completing their APPEs, and sites are unsure of future availability due to ever-changing staffing and workload issues that impact their ability to place students. Schools should not get into a race for site scheduling, which may happen as competition continues to increase.
Whether the amount of one-on-one time preceptors spend with students equates to a higher quality learning experience remains unknown. Nearly all preceptors in the survey responded that they thought that the more time they spent with students the better the quality of the APPE. Contrasting that with the actual time they indicated they were spending with students revealed a gap/shortfall that should be of concern to experiential program administrators. Approximately 20% of respondents felt they were not able to spend enough time with students to provide a quality experience. In some instances, a concerted effort to contact preceptors to discuss time-quality balance to ensure a valuable educational experience may be required. Colleges/schools should also be collaborating to explore best-practice precepting models. Models that provide balance among quantity of preceptor one-on-one student time, quality interactions that facilitate self-directed student learning, and student contribution (value-added services) to sites would be useful for both sites and schools. Preceptor development opportunities are needed to determine, facilitate, and maintain a balance that is mutually beneficial to all.
Over half of the time that students were at their experiential sites was not spent directly with the preceptor, so schools need to ensure that patient safety is a priority during the unsupervised times and that the students are gaining the experience necessary to become competent pharmacists. There may be a difference among various pharmacy practice settings regarding the most appropriate amount of supervision. For example, more supervision may be needed at sites where dispensing is a primary responsibility (eg, community and hospital) compared to sites where the student is given instructions and then expected to identify and collect information from various resources. This is another area where preceptor development regarding potential student APPE activities may benefit the relationship and the quality of the learning experience. School administrators need to be able to verify with confidence that students completed the appropriate full-time equivalent hours and are eligible to sit for the board licensing examination. Preceptors need to spend adequate time with students to clearly define expectations, supervise patient care activities, and provide routine feedback to improve the student's pharmacy practice skills. However, other responsibilities, staff shortages, and heavy workloads often are a higher priority for pharmacist preceptors. Experiential administrators should work closely with preceptors to better understand the environmental constraints preceptors face and to develop workload balance solutions that are win-win for both parties.
One third of the respondents who answered the compensation questions indicated that the reason they required compensation was for the additional precepting workload. When asked where the monetary stipend went, 36% indicated it went to administration and 36% indicated it went into a pharmacy development fund that preceptors could use. For some pharmacists, precepting students may mean that they are getting less practice-related work done at their site, while for others, it may mean that they are spending additional time at work. This information should be discussed between experiential office administrators and site managers so that if the pharmacists are actually putting in extra time, then they benefit from the resources through preceptor development, whether it is support for attending national meetings or additional resource availability on site. Otherwise, if precepting means that the pharmacist is unable to cover all of his/her staffing responsibilities, having the compensation go to administration may be warranted.
All survey respondents were asked to select the form of compensation that was most valuable to them, regardless of whether they currently required a monetary stipend or other form of compensation. It is no surprise to the authors that over a third of respondents indicated that a monetary stipend was most valuable to them. This was followed by library and electronic resource access. Many schools do not have the funds available, or do not allocate a portion of students' tuition or fees, to pay a stipend to experiential sites for their services. The level of compensation to preceptors may more significantly impact state colleges/schools than private since their budgets are often impacted by national and state fiscal and political climates. In contrast, private colleges/schools have more flexibility in determining and setting tuition rates.
According to the 2003-2004 AACP Professional Affairs Committee Report, financial support for experiential programs varied among schools from 1% to 27% (total cost as percent of school's expense budget).11 When the report was published, the experiential component of pharmacy education was at least 25% of the curricula. The information in this survey should be presented to administrative officials in colleges/schools to assure appropriate support and to determine what types of resources can be made available to preceptors. If a preceptor is providing a quality experience, which is a service that the schools need, it is important to work together to cultivate a supportive and long-lasting relationship. Compensation can take many forms, including the value that students add to a site through the contributions of their daily activities and the site's ability to showcase themselves as a potential future employer. Compensation is a way of rewarding the site for playing an integral part in the education of future pharmacy professionals and therefore may be a key piece necessary to ensure the best overall experiences. In order to effectively support experiential education, which now comprises 30% of the pharmacy curricula, a comparable portion of the college's/schools' budget must be allocated to this area.
There are some limitations that have been identified throughout the study. Due to financial and time constraints, the survey was available only electronically; thus, preceptors without Internet or e-mail access were excluded.
There were varying response rates to individual questions resulting in missing data that may have affected some questions more than others. Additionally, respondents were asked to skip the majority of the compensation questions if they answered that they did not require compensation. A better picture of compensation issues in the experiential environment may have been captured if all respondents had been asked to answer all of the questions. Not all of the authors agree that the data collected in the compensation section of the survey instrument truly reflect their personal experience with preceptors in the practice environment.
There is also potential for a sampling bias. The low response rate of 26.5% may not have been representative of the entire population of preceptors. Furthermore, the study used a convenience sampling rather than a randomized, stratified sampling. However, the overall sample size was large and a cross-section of private and public colleges/schools from different regions of the United States surveyed their preceptors. Because of these limitations, caution should be exercised when trying to generalize the information to the entire population of preceptors. Nevertheless, since this is the first national volunteer preceptor survey of its kind to be published, the findings could be used as a foundation for future nationwide preceptor studies.
CONCLUSIONS
A national survey of volunteer pharmacy preceptors found that requests for student placements have increased over the past few years. Almost half of the preceptors responding had to turn away students because they could not place them. Most sites were precepting students from more than one school. Almost all preceptors felt that the more time they spend with APPE students, the better the overall experience, yet one fifth said they do not have enough time to spend with students to provide a quality experience. Monetary stipend was the form of compensation preceptors considered most valuable.
This description of the current experiential environment and preceptor perceptions concerning APPEs should assist college/school leaders and experiential administrators in understanding current preceptor workload issues and needs. With the increase in enrollment of existing schools and the addition of new schools of pharmacy, these challenges are important to address when securing quality preceptors and sites and to further enhance experiential education.
ACKNOWLEDGEMENT
The authors acknowledge Dr. Amy M. Haddad, PhD, Director of the Center for Health Policy and Ethics at Creighton University, for her guidance in getting this project off the ground.
REFERENCES
- 1.Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Chicago, IL: Accreditation Council for Pharmacy Education: 2006. Available at: http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed October 6, 2008.
- 2.Pharmacy Manpower Project, Inc. Aggregate Demand Index for Pharmacists. Available at http://www.pharmacymanpower.com. Accessed October 6, 2008.
- 3.Bureau of Labor Statistics. 2008-09 BLS Occupational Outlook Handbook. Available at: http://www.bls.gov/oco/ocos079.htm. Accessed October 6, 2008.
- 4.American Association of Colleges of Pharmacy. Academic Pharmacy's Vital Statistics. Alexandria, Va: Available at: http://aacp.org/Docs/MainNavigation/InstitutionalData/8855_2008.pdf Accessed October 6, 2008.
- 5.Accreditation Council for Pharmacy Education. Accredited Professional Programs of Colleges and Schools of Pharmacy. Available at: http:/acpe-accredit.org/deans/schools.asp Accessed October 6, 2008.
- 6.Plaza CM, Draugalis JR. Implications of advanced pharmacy practice experience placements: a 5-year update. Am J Pharm Educ. 2005;69(3) Article 45. [Google Scholar]
- 7.Harralson AF. Financial, personnel, and curricular characteristics of advanced practice experience programs. Am J Pharm Educ. 2003;67(1) Article 17. [Google Scholar]
- 8.Salant P, Dillman DA. How to Conduct Your Own Survey. 1st ed. New York, NY: John Wiley and Sons Inc; 1994. [Google Scholar]
- 9.Pharmacy Preceptor Survey Summary Report, 2007. Alexandria, VA: American Association of Colleges of Pharmacy. Available at: http://aacp.org/site/page.asp?TRACKID=&VID=1&CID=1572&DID=9409. Accessed on October 6, 2008.
- 10.Gadkari A, Mott D, Kreling D, Bonnarens J. Characteristics of unmet demand for pharmacists: a survey of rural community pharmacies in Wisconsin. J Am Pharm Assoc. 2008;48:598–609. doi: 10.1331/JAPhA.2008.07039. [DOI] [PubMed] [Google Scholar]
- 11.Littlefield LC, Haines ST, Harralson AF, et al. Academic Pharmacy's Role in Advancing Practice and Assuring Quality in Experiential Education: Report of the 2003-2004 Professional Affairs Committee. Am J Pharm Educ. 2004;68(3) Article S8. [Google Scholar]