Abstract
Purpose
Current hospital and health-system participation in and the future capacity for experiential education for pharmacy students was investigated.
Methods
An online survey of ASHP members identified as U.S. pharmacy directors was conducted to assess their current and future involvement in partnering with colleges and schools to meet the experiential education requirements for doctor of pharmacy students and the current status of the student learning experiences. Questionnaire items examined the factors on which expanded involvement in experiential education would depend, the nature of support provided by colleges and schools, the types of experiences available for students, respondents' perceptions of factors influencing the quality of experiential education, the value of experiential education to the sites, respondents' challenges and concerns about experiential education, and respondents' current capacity and projections for introductory and advanced experiences through 2012.
Results
Data from 549 respondents were analyzed. Most respondents indicated that they had conducted advanced experiences for their 2007 graduates and anticipated that they would continue to do so. Among the top challenges identified regarding advanced experiences were concerns about time to serve and be trained as preceptors and a lack of standardization and coordination among colleges and schools. Hospitals forecasting their future capacity to accommodate students indicated that their projections were highly dependent on the number of pharmacists at their hospitals. Many respondents noted that their capacity projections were tied to their ability to expand clinical services at their hospitals.
Conclusion
A survey of pharmacy directors suggested an ability of U.S. hospitals to conduct advanced experiential education opportunities for pharmacy students through 2012 and to expand introductory experiences.
Keywords: curriculum, data collection, education, pharmaceutical, pharmacy, institutional, hospital, pharmacy
Addressing the quality and capacity in experiential education for doctor of pharmacy students has been a leadership priority for both the American Association of Colleges of Pharmacy (AACP) and the American Society of Health-System Pharmacists (ASHP) for some time. Collaborative and individual organizational efforts have resulted in resources for members—faculty and practitioners—who are partners in conducting experiential education. One such effort was the Summit to Advance Experiential Education in Pharmacy, convened by AACP in 2005.1 ASHP members and staff participated in planning and as stakeholder invitees to the summit. The purpose of the summit was to bring together key stakeholders from the practice, regulatory, and education communities to identify strategies and develop resources to increase the capacity and enhance the quality, efficiency, and effectiveness of pharmacy experiential education.
The summit called for collaboration between academic pharmacy and professional organizations to improve the quality of experiential education, to recruit and train qualified experiential education preceptors, and to address the need to increase the quantity of exemplary experiential education sites across the country. The summit was the catalyst that led ASHP and AACP to jointly conduct a study investigating current hospital and health-system participation in and the future capacity for experiential education. Several other important initiatives resulted from the summit as well.2-4
BACKGROUND
The mission of pharmacy education is to prepare graduates who provide patient-centered care that ensures optimal medication therapy outcomes and provides a foundation for specialization in specific areas of pharmacy practice; to participate in the education of patients, other health care providers, and future pharmacists; to conduct research and scholarly activity; and to provide service and leadership to the community.5
To be accredited by the Accreditation Council for Pharmacy Education (ACPE), doctor of pharmacy degree programs of colleges and schools of pharmacya must provide knowledge, practice skills, professional attitudes, and values to prepare graduates to enter pharmacy practice in any setting.6 The degree programs must address biomedical and pharmaceutical sciences and social, behavioral, administrative, and clinical competencies.7 With the primary aim of developing practice competency, colleges and schools are required to incorporate into their curricula both introductory and advanced pharmacy practice experiences in various practice settings.8
The ACPE accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree, implemented in July 2007, stipulate that introductory pharmacy practice experiences constitute at least 5% (i.e., 300 contact hours) of the overall curriculum and advanced pharmacy practice experiences constitute at least 25% (i.e., 1440 contact hours) of the overall curriculum.8 The 5% requirement in 2007 for introductory experiences represented an expansion in the requirements and was the first quantified requirement of this nature in the ACPE standards,b although many colleges and schools conducted introductory experiences prior to the 2007 standards.9 Throughout the remainder of this report, these experiences are termed introductory and advanced experiences.
Introductory experiences occur during the first three professional years of the curriculum. They must permit students, under appropriate supervision and as permitted by state practice regulations, to assume direct patient care responsibilities. Introductory experiences must occur in a progressive fashion, leading to entry into advanced experiences.10 Together, these experiences are “designed to develop the practice skills, judgment, professional behavior, attitudes and values, confidence, and personal responsibility needed for each student to embark on an independent and collaborative practice.”11 Introductory experiences may use various formats, including shadowing practitioners or students on advanced experiences, interviews with patients, service learning, and experiences in pharmacies. Introductory experiences may be brief (e.g., one day or less) observational experiences in a practice setting with accompanying explanation by pharmacist preceptors. However, some colleges and schools conduct introductory experiences in a longitudinal fashion over periods of weeks. It has been reported that “the implementation of [introductory experiences] in pharmacy curricula has been met with a wide range of interpretation.”9 It is important to note that the requirements for introductory experiences changed with the implementation of revised ACPE standards in July 2007.
Advanced experiences typically occur in the final year of the professional curriculum under the supervision and monitoring of pharmacist preceptors. Most of the time spent by students in advanced experiences should involve direct patient care.12 Students must participate in hospital or health-system pharmacy, inpatient or acute care general medicine, ambulatory care (e.g., as conducted in a hospital-based clinic), and community pharmacy.12 Social, behavioral, administrative, and clinical competencies are especially developed and honed during experiential education. Advanced experiences typically are full-time (40 hours per week) and conducted over four to six weeks. Elective advanced experiences may occur in patient care or other pharmacy services, such as drug information, informatics, management, home infusion, outpatient dispensing, and investigational drug services.
An increased volume of prescription drug products and their usage, a growing demand for pharmacists' clinical services to meet the needs of the aging population (especially in hospitals and other multidisciplinary health systems), and the resultant substantial expansion of health-care facilities and pharmacies have contributed to a chronic shortage of pharmacists.13-15 In order to address work-force demands, existing colleges and schools have responded by expanding enrollments, establishing branch campuses, and developing distance-learning pathways to increase accessibility to doctor of pharmacy degree programs. In addition, new doctor of pharmacy degree programs have been started at academic institutions. Efforts to address the serious pharmacist work-force shortage by increasing enrollments in doctor of pharmacy degree programs and thus producing more graduates prepared to enter practice have placed stress on the education system. Increased enrollment results in a need for increased experiential education placements, which in turn stresses patient care delivery systems, including hospital pharmacy departments.
STUDY INTRODUCTION
Serious concern has been raised among hospital and health-system practitioners about the capacity of their sites to accommodate increases in student experiential education placements, considering that degree requirements mandate that both introductory and advanced experiences be conducted in hospitals and health systems. Further, some of the ambulatory care experiences (which are distinct from community pharmacy experiences in the ACPE requirements) are also conducted in hospitals and health systems.
There are four required advanced experiences per ACPE's standards. These must include (1) community pharmacy, (2) hospital or health-system pharmacy, (3) ambulatory care, and (4) inpatient and acute care general medicine.12 All of the advanced experiences in hospital and health-system pharmacy and in inpatient and acute care general medicine occur in hospitals. Some ambulatory care experiences occur in hospitals and health systems, as well as some electives in various clinical services (e.g., drug information, anticoagulation clinic) or specialty areas of care (e.g., transplantation, emergency care).
The colleges and schools have faced challenges in identifying, developing, and sustaining quality practice sites that meet the expected educational objectives for experiential education. Consistent with the profession's vision16 and faithful to its mission5 to educate pharmacy graduates recognized as the health care professionals responsible for providing patient care that ensures optimal medication therapy outcomes, the academic community has been attentive to the challenges associated with delivering high-quality experiential education comprising 30% or more of the curriculum.
Numerous research and association reports with recommendations for actions to achieve experiential education needs have been generated. Challenges have been noted with respect to identifying qualified practice sites, finding sites in rural locations, developing and training qualified preceptors, and financing experiential education.17-19 Colleges and schools have consistently reported that hospital and health-system practice–partner sites for conducting experiential education in internal medicine and ambulatory care are the most difficult to secure.17,20-23 Contributing to this challenge, now, is the increased July 2007 requirement to conduct introductory experiences in both community and hospital settings.8
ASHP and the American Pharmacists Association conducted a survey in the fall of 2005 and found that 81% of college and school experiential education administrators who responded found it extremely or somewhat difficult to find and place students in quality hospital and health-system sites.24 In contrast, about 50% of respondents found it extremely or somewhat difficult to place students in community pharmacies and managed care settings that met the ACPE standards.
While most doctor of pharmacy degree programs exceed the 1440-hour (36-week) minimal requirement for advanced experiences as stipulated in the ACPE standards, it is reasonable to assume for projection purposes that approximately 1600 hours (40 weeks) of experiential education may be representative of a majority of doctor of pharmacy degree programs in the United States. Assuming a 5-week duration for each advanced experience, eight placements would be necessary to accommodate the 40 weeks of experiential education. Further, it is reasonable to assume for projection purposes that four advanced experiences (20 weeks) in hospitals occur per graduate from the overall total of eight placements (40 weeks). Most advanced experiences begin three years after enrollment in a four-year doctor of pharmacy program. However, the need for introductory experiences can be almost immediate, depending on the specific curriculum of the college or school. The estimate of four advanced experiences per graduate in hospitals does not include additional advanced experiences conducted as electives.
In 2006, there were 9,040 doctor of pharmacy graduates from 87 U.S. colleges and schools, 48,592 students enrolled in various professional years at 98 colleges and schools, and an anticipated 2007 graduating class size of 9,865.25 The 11 new doctor of pharmacy degree programs did not produce graduates in 2006.
With growing enrollment numbers, branch and satellite campus expansions, and the emergence of new colleges and schools, caution must be used when projecting the future numbers of graduates and subsequent requirements for experiential education; therefore, projections beyond five years are not included in this report.
On behalf of their members and in the interest of advancing quality experiential education, AACP and ASHP recognized the critical need to assess the current status and future capacity of hospitals and health systems to engage in partnerships for experiential education. To that end, AACP and ASHP collaborated on a survey of ASHP members to investigate the current and projected capacity for experiential education for doctor of pharmacy students in hospitals and health systems, the current status of student learning experiences, factors influencing participation, the type of investment and support from the academic partners, perceived benefits to hospitals and health systems, and site demographics. The information presented in this report should help AACP and ASHP and their members understand the benefits and challenges in successful partnerships between colleges and schools and hospitals and health systems and identify strategies to facilitate participation and enhance the quality of the experience.
This report provides a snapshot of a select sample of ASHP members and the current and potential capacity of their hospitals to partner with colleges and schools of pharmacy to conduct experiential education for doctor of pharmacy students at their respective sites.
METHODS
An online survey of ASHP members identified as U.S. pharmacy directors was conducted to assess their current and future involvement in partnering with colleges and schools to meet the experiential education requirements for doctor of pharmacy students.
Staff from ASHP and AACP served on a steering committee, and an advisory panel of eight (four members drawn from each organization) was appointed to assist in questionnaire development and report critique. ASHP administered the project.
Survey design.
The survey was constructed with the assistance of the advisory panel. The advisory panel and steering committee met by conference call, with additional e-mail communication occurring among participants.
The questionnaire was pilot tested for face and content validity by 12 individuals. In-depth interviews were conducted using a cognitive-feedback technique26 with 4 pharmacy directors from small hospitals and 4 ASHP staff members who formerly held positions as hospital pharmacy directors. In addition, 4 pharmacy directors from hospitals of various sizes and types completed the draft questionnaire and provided written feedback. The results of the pilot testing were used to evaluate the questionnaire for item clarity, ease of completion, format, and online system use. Several modifications were made based on the feedback received. The questionnaire is available from ASHP and AACP.
Five-point Likert scales were used to assess perceptions and beliefs (e.g., 1 = low influence and 5 = high influence; 1 = not dependent and 5 = highly dependent; 1 = strongly discourage and 5 = strongly encourage) and allowed collapsing of the data where appropriate. Opportunities for free-text comments were made available for respondents; however, a complete analysis of the comments made is beyond the scope of this report.
Study design.
The survey was distributed to a convenience sample that included all individuals identified in ASHP's membership database as directors of pharmacy with an e-mail address on record. Two days before the survey was launched, a notice was e-mailed to the selected directors to inform them of the upcoming survey. A link to the online questionnaire was e-mailed to the 2840 pharmacy directors on September 13, 2007. Reminder e-mails were sent to all nonrespondents on September 19 and September 25; the survey was closed on September 29, 2007. Qualtrics (Provo, UT) survey software was used to build, administer, and host the online questionnaire.
The questionnaire asked recipients to identify their practice setting. Pharmacy directors in hospitals and long-term-care settings comprised the population meeting criteria for inclusion in data analysis. Respondents identifying themselves in other settings were routed to a different, very brief questionnaire inviting their free-text comments about conducting experiential education.
Survey recipients were asked to identify key site demographics, including average daily census, geographic location, and population setting (urban or rural). They were also asked whether experiential education was explicitly stated in their organization's mission, whether experiential education for other health disciplines was conducted at their hospitals, and whether their hospitals conducted ASHP-accredited residency programs. Questions to determine current and anticipated future participation in pharmacy experiential education were included. Respondents were asked whether their hospitals had conducted advanced experiences in the past 12 months with the expectation that some would continue in the next year. Those who had conducted advanced experiences for the 2007 graduates were provided the entire questionnaire to complete. Respondents who had not conducted an advanced experience for a 2007 graduate were directed to an abbreviated questionnaire.
Questionnaire items examined the factors on which expanded involvement in experiential education would depend, the nature of support provided by colleges and schools, the types of experiences available for students, respondents' perceptions of factors influencing the quality of experiential education, the value of experiential education to the sites, respondents' challenges and concerns about experiential education, and respondents' current capacity and projections for introductory and advanced experiences in the next five years (i.e., through 2012).
To provide insight into the possibility of nonresponse bias, a comparison was made between early and late responders. No statistically significant differences were found (p > 0.05). Data were analyzed using Microsoft Excel (Redmond, WA) and SPSS, version 16.0 (SPSS Inc., Chicago, IL). Descriptive statistics were used extensively. Chi-square analysis examined how responses differed as a function of hospital characteristics. Student's t test was used to determine the relationship among survey variables. The a priori level of significance was set at 0.05.
RESULTS
The questionnaire was sent to 2840 individual e-mail addresses. After accounting for undeliverable e-mails, the overall response rate was 26% (n = 726). Of these respondents, 609 were located in practice settings meeting the criteria for inclusion in the analyses. The 603 responses from hospitals represented 8.7% of the 6921 hospitals in the United States and 21.2% of the questionnaire recipients. Ninety-one percent of respondents (n = 503) were directors of pharmacy, with all states represented but one.
Respondent demographics.
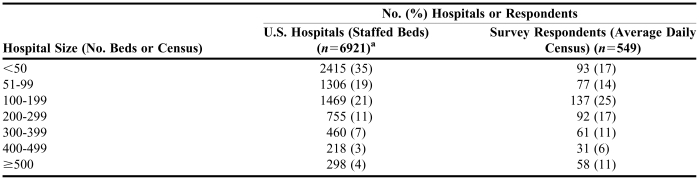
The pattern of the 549 responses tabulated by hospital census was skewed toward larger hospitals compared with the national distribution (Table 1). Eleven percent of respondents worked in hospitals with more than 500 beds, compared with 4% nationally. Although 75% of all hospitals in the United States have 199 or fewer beds, in this study these hospitals accounted for 56% of respondents. The number of responses from nonhospital sites was too small to be analyzed; thus, no data are reported here for them. The number of pharmacists per site varied by hospital census. Hospitals that engaged in experiential education had greater numbers of pharmacists (t test, t = 6.881, df = 542, p = 0.001).
Table 1.
Hospital Size Distribution of U.S. Hospitals and Survey Respondents
Tabulated by ASHP from Verisoan Hospital Market Profile database: 2007 Feb.
Current status of participation for inpatient advanced experiences.
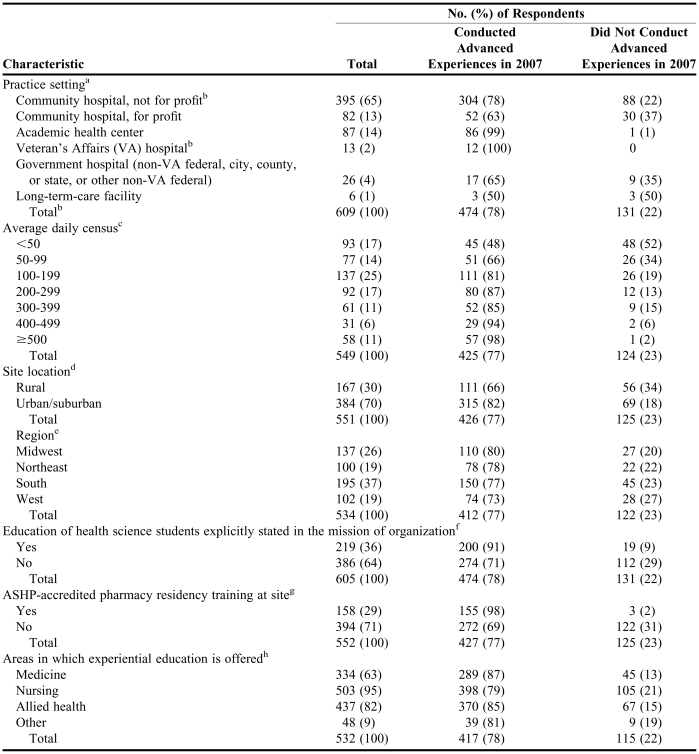
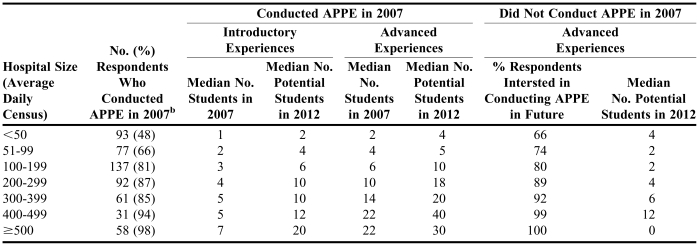
Table 2 compares the characteristics of sites that conducted advanced experiences in 2007 with those of sites that did not. The majority (78%, n = 474) of respondents indicated that they had conducted advanced experiences for their 2007 graduates and anticipated that they would continue to do so. A total of 131 respondents indicated that they had not conducted advanced experiences for pharmacy students in 2007, but 80% of those said they would be interested in conducting advanced experiences.
Table 2.
Characteristics of Sites That Did and Did Not Conduct Advanced Experiences in 2007
χ2 =41.217, df=5, p=0.001
Total n is larger than row n detail because not all community hospitals (not for profit) and VA hospitals responded to this questions
χ2 =77.322, df =6, p=0.001
χ2 =16.074, df =1, p=0.001
χ2 =2.204, df=3, p=0.564
χ2 =34.074, df=1, p=0.001
χ2 =54.39, df=1, p=0.001
χ2 =95,423, df=4, p=0.001
The majority of respondents reported having multiple partnerships with colleges or schools for conducting experiential education. Thirty percent of respondents reported partnering with one college or school, 30% with two, 24% with three, and 15% with four or more. Each hospital partnered with a mean of 2.56 colleges and schools. Some respondents commented that the number of partnerships would be increasing in the future because of the opening of new colleges and schools in their geographic areas.
Placement of pharmacy students in inpatient advanced experiences classified as “general or specialized clinical” (e.g., internal medicine, electives such as oncology or critical care) was reported by 94% of respondents. Likewise, similar placements for inpatient advanced experiences in the “inpatient pharmacy department” (i.e., focused on medication systems) were reported by 74% of respondents. General or specialized clinical advanced experiences in the ambulatory care setting were reported by 33% of respondents. Fifteen percent conducted ambulatory care advanced experiences focused on medication systems.
Factors influencing site participation in experiential education.
As reported in Table 2, respondents who worked in for-profit community hospitals were less engaged in conducting advanced experiences than other hospitals (p = 0.001). All but one academic health center conducted advanced experiences in 2007, compared with 77% of not-for-profit community hospitals. Thirty percent of respondents worked in rural hospitals, and the remaining worked in urban and suburban hospitals, which tended to have a larger census. Twenty-nine percent of respondents reported that their sites conducted ASHP-accredited residency programs. Of the hospitals that did so, 98% conducted advanced experiences for pharmacy students. Respondents in two thirds of these hospitals said residents served as preceptors for introductory or advanced experiences. Thirty-six percent assigned first-year residents as preceptors, 10% assigned second-year residents, and 21% assigned both.
In 36% of sites, education was explicitly stated in the site's mission (Table 2). Forty-two percent of respondents currently participating in advanced experiences stated that the education of health science students is consistent with their hospitals' educational mission. There was a significant association between hospitals with such a mission and their participation in advanced experiences (p = 0.001). Experiential education for nursing was the most commonly reported type of experiential training provided by hospitals that did and did not conduct advanced experiences in 2007 (Table 2). Hospitals that conducted advanced experiences were more likely to have conducted experiential education in medicine and allied health than were hospitals that did not conduct advanced experiences (p = 0.001).
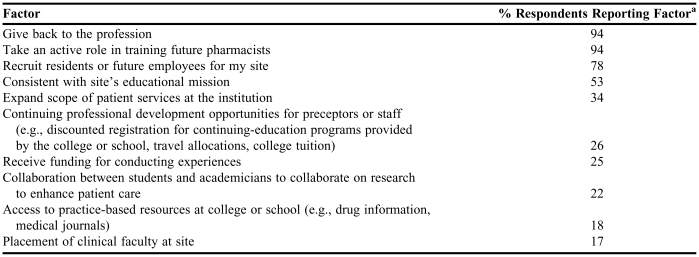
The top three factors that contributed to a site's decision to conduct advanced experiences were (1) giving back to the profession (94%), (2) taking an active role in training future pharmacists (94%), and (3) the ability to recruit residents or future employees (78%) (Table 3). Additional factors listed by some respondents included benefits to their staff in terms of skills and knowledge, the opportunity to share with students their perspectives about the professional progress made in hospital pharmacy, and the ability to convey to students their own opportunities to be influencers of change in the profession during their careers.
Table 3.
Factors Contributing to Sites' Decision to Conduct Advanced Experiences in 2007 (n=431)
Mean number of factors reported by respondents was 4.6
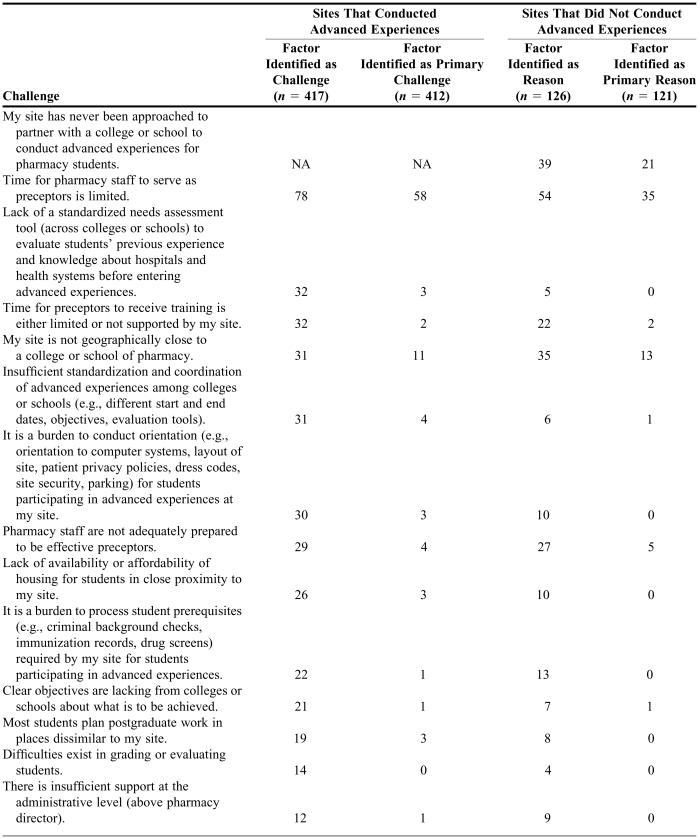
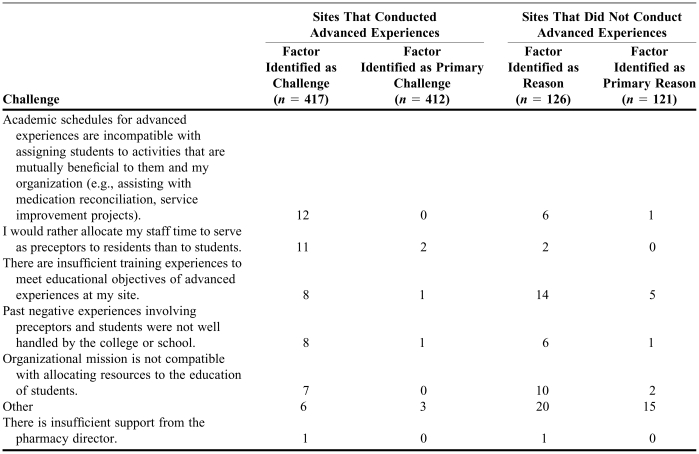
Respondents were asked to identify perceived challenges related to conducting advanced experiences and rank one as a primary challenge. Among the top challenges identified were concerns about time to serve and become trained as preceptors and a lack of standardization and coordination among colleges and schools (Table 4). The most frequently cited challenge—“time for pharmacy staff to serve as preceptors is limited”—was identified as the primary concern both for respondents that had taken students in 2007 and those that had not. Of the respondents who had conducted advanced experiences, 29% indicated that their pharmacy staff was not adequately prepared to be effective preceptors, compared with 27% of respondents who had not conducted advanced experiences.
Table 4.
% Sites Acknowledging Factors Influencing Ability to Conduct Advanced Experiences within Past 12 Monthsa
Factors were identified as challenges to increasing the quality or quantity of advanced experiences or as reasons for not partnering with a college of school of pharmacy in conducting an advanced experience in the past 12 months. One factor was designated as the primary challenge or primary reason. NA = not applicable
Thirty-nine percent of respondents who had not conducted advanced experiences said their hospitals had never been approached to partner with a college or school to conduct advanced experiences; 21% said this was the primary reason they did not participate (Table 4). Geographic proximity was identified as a challenge both by respondents who had and those who had not conducted advanced experiences.
Respondents were invited to comment on state regulation of pharmacy practice related to their sites' engagement in experiential education and changes that needed to be addressed to assist in the provision of experiential education. Comments were received from 51 respondents. Student licensing, differentiating students from technicians in the scope of practice, and variance in technician use were mentioned as issues that needed to be addressed by stakeholders to facilitate engagement in experiential education. Some noted that state regulations with respect to ratios of pharmacists to students and pharmacy technicians negatively affected the number of students that could be accommodated for experiential education.
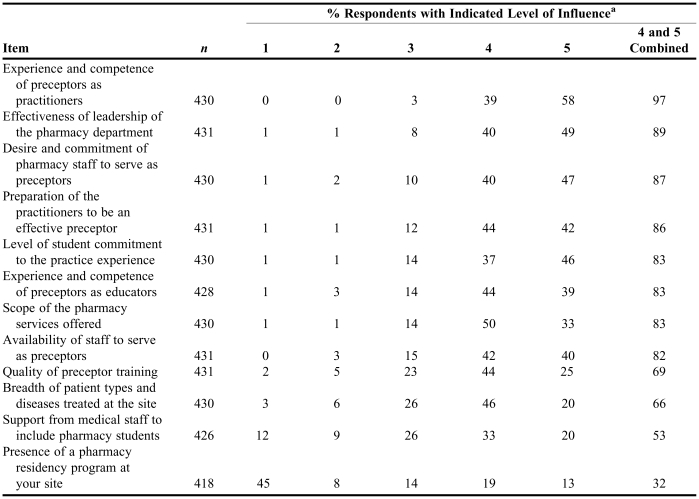
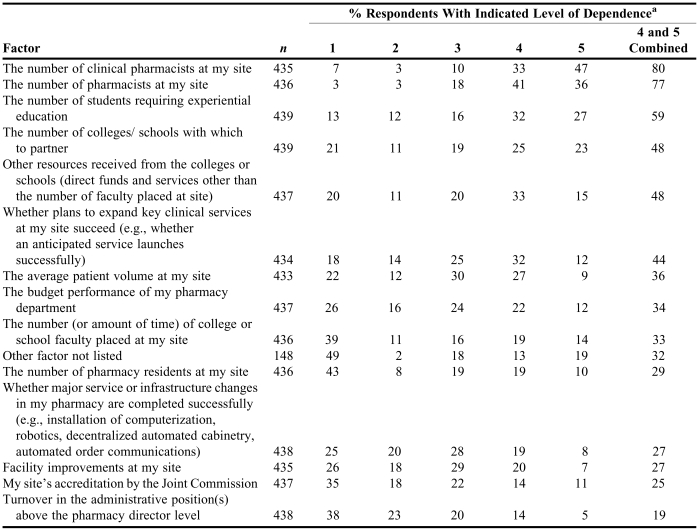
Factors influencing quality experiential education.
Factors that respondents believed had the most influence on the quality of experiential education at their hospitals are listed in Table 5. Most notable among these was the experience and competence of preceptors as practitioners. The effectiveness of leadership of the pharmacy department, the desire and commitment of pharmacy staff to serve as preceptors, and the preparation of practitioners to be effective preceptors were also highly rated. Some respondents also listed hospital administrative support and a perception of value for experiential education as influential factors.
Table 5.
Items That Influence the Quality of Experiential Education Conducted at Respondents' Sites
A rating of 1 indicates low influence and a rating of 5 indicates high influence
Of respondents conducting advanced experiences, 94% believed that students were receiving high-quality experiences. Eighty-five percent said that pharmacists at their hospitals were professionally committed to educating students. Sixty-seven percent said their hospitals had adequate resources to ensure high-quality education.
About two thirds of the respondents conducting advanced experiences indicated that the preferred duration of an advanced experience in a hospital was four or six weeks (31% and 32%, respectively). Fifteen percent preferred a five-week experience, and 8% said that multiple experiences at the same site were more important to them than the experience duration. Fifty-six percent agreed or strongly agreed that it would be desirable for a given student to have multiple placements at the same site.
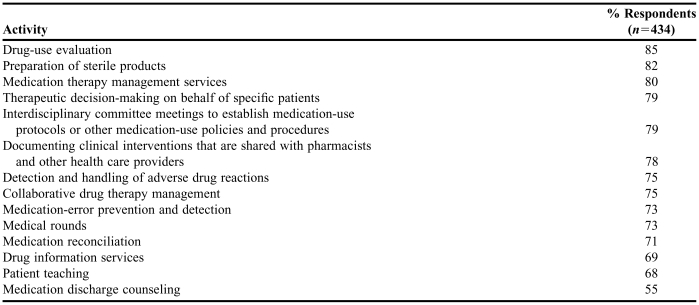
Table 6 displays the activities available to students during experiential education. The most common activities identified were drug-use evaluation (85%), preparation of sterile products (82%), and medication therapy management services (80%). The activity cited least often was medication discharge counseling (55%). In free text, some respondents identified other activities, including opportunities for pharmacy administration, management of compliance with external standards, pharmacy informatics, assessment of system safety, investigational drug handling, telepharmacy, and educational presentations to other professionals.
Table 6.
Activities Available to Students During Experiential Education at Respondents' Sitesa
No differentiation was made between introductory and advanced experiences in question wording
Perceived benefits and tangible support realized by the practice site partner.
Benefits and support received by hospitals for partnering with colleges and schools to conduct experiential education are most often described in terms of transfer of resources (fiscal, personnel, or in-kind services). Examples include shared faculty positions; funding arrangements under affiliation agreements; and access to resources, programs, or services at the colleges and schools. Other benefits to the hospital are realized through the integration of students into the site's practice model. The questionnaire explored both types of support.
Perceived benefits to the hospital or health-system partner.
Respondents were asked to identify benefits from participating in experiential education. Ninety percent of respondents agreed or strongly agreed that being placed in preceptor roles stimulated their staff to maintain their own knowledge and stay up-to-date. Eighty-two percent found value in assigning students to activities that were mutually beneficial to students and the sites (e.g., medication reconciliation,27-31 service improvement projects, assisting with literature searches). Sixty-nine percent said students shared insights and perspectives that were helpful in improving services at their sites. Fifty-seven percent said students shared insights and perspectives about general developments in health care and pharmacy. In free text, some respondents noted that students made it possible to extend medication therapy management to more patients and that students made educational presentations to professional staff.
Fifty-nine percent of respondents reported hiring former advanced experience students as pharmacists after graduation. Similarly, 30% said they had selected advanced experience students as residents after graduation. Partnering with colleges and schools for experiential education assisted them in recruitment.
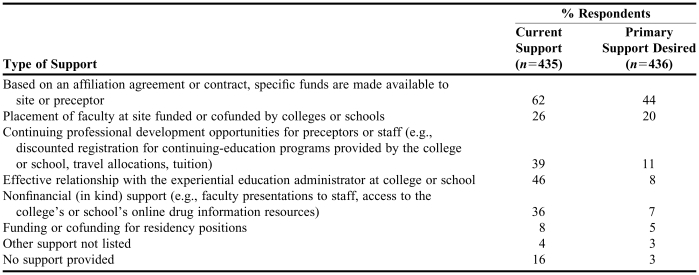
Direct support provided by the academic partner.
The ways in which the respondents' sites were supported by colleges and schools for partnering in experiential education are listed in Table 7. Data are also reported for the support most desired by respondents. The most common means of support reported was specific funding made available to the site or preceptor based on an affiliation agreement or contract (62%). Twenty-three percent of respondents reported that there were pharmacists present who were employed by a college or school and served as preceptors; 14% reported the presence of preceptors cofunded by the sites and colleges and schools.
Table 7.
Type of Support Currently Provided by and Primary Support Desired from College and Schools for Conducting Advanced Experiencesa
Calculated by examining each support type desired and cross-tabulating with the number of sites not receiving that type of support
While funding was identified as the most desired form of support from the colleges and schools (Table 7), funds did not rank high as a decisive factor for hospitals' participation in advanced experiences (Table 3). Similarly, the second most desired form of support was the placement of faculty at experiential education sites. However, the placement of faculty ranked low as a decisive factor to conduct advanced experiences.
Support derived from the relationship with colleges and schools in conducting educational experiences was reported. Twenty-nine percent of respondents agreed or strongly agreed that when they encountered students whose knowledge or performance was not sufficient, the colleges and schools provided appropriate assistance in dealing with the matter. Thirty-six percent indicated appropriate assistance from colleges and schools when they encountered students whose behavior was unsatisfactory.
Capacity for experiential education experiences in hospitals.
Estimated current capacity (2007).
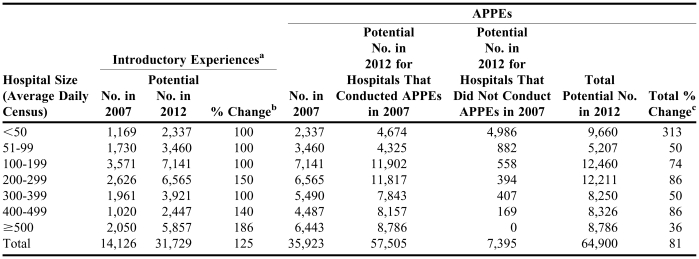
Based on the survey findings and projecting them to all hospitals in the United States, approximately 35,923 advanced experiences and 14,126 introductory experiences were conducted in hospitals for the 2007 graduates (Table 8). Based on AACP student enrollment data, 39,460 advanced experiences would have been conducted (9,865 students multiplied by four placements per student) in hospitals for the same graduation class of 2007. Thus for 2007, based on the findings and enrollment data, between 35,923 and 39,460 advanced experiences were conducted in hospitals for all graduates of doctor of pharmacy programs in 2007.
Table 8.
Estimated 2007 and Projected Potential 2012 Introductory and Advanced Pharmacy Practice Experiences (APPEs) in U.S. Hospitals
If conducted in 2007
Calculated as follows: (potential 2012 experiences/2007 experiences) - 1 × 100%
Calculated as follows: (total potential 2012 APPEs/APPEs conducted in 2007) - 1 × 100%
Projected capacity through 2012.
Graduation projections (based on fall 2006 enrollment data) for the graduating classes of 2007, 2008, and 2009 were 9,865, 10,828, and 11,421, respectively.25 These graduation projections represent growth rates of 9.1%, 9.8%, and 5.5%, respectively, from the preceding year. If growth rates continued at 9% through 2012, the projected number of graduates would be approximately 14,790; for a growth rate of 5%, the number of graduates would be approximately 13,220.
Another source projected the number of graduates in 2012 to be 10,655, based on an expectation (in 2006) that each year there would be an average of one new college or school graduating 100 students.32 Given that the recent actual growth rate of new colleges and schools has been higher than that, this projected number of graduates (and corresponding need for experiential education placements) through 2012 may be an underestimate.
Employing the premise of four advanced experiences in hospitals per graduate, the number of advanced experience placements necessary in hospitals would be 39,460 for 2007 graduates and between 42,620 and 59,160 (using the highest projected graduate numbers described above) for 2012 graduates. When asked to project capacity to 2012, existing advanced experience hospitals indicated capacity for an additional 21,582 student placements, for a projected total of 57,505 placements (an increase of 60% over the 2007 level). Hospitals that did not conduct advanced experiences for the 2007 graduates projected a capacity for 7,395 student placements (11% of the total advanced experience estimate for 2012). Total student placement capacity for advanced experiences in hospitals in 2012 was projected by respondents to be 64,900 (81% more than the 2007 level). Table 8 (last column) shows the percent growth necessary to achieve the estimates by size of hospital. The challenge for achieving the estimates for 2012 will be substantial for hospitals of all sizes; it will be the greatest in hospitals with a census of less than 50. The greatest capacity for expansion of advanced experiences is in sites that already participate.
According to the projected capacity estimates and based on survey responses (Tables 8 and 9), there could be adequate capacity in hospitals to conduct advanced experiences for the projected number of graduates through at least 2012. That projection, however, must be interpreted in light of the dependent factors in Table 10. On a 5-point Likert scale of “not dependent” to “highly dependent,” the top three ranked factors (combining ranks 4 and 5) on which the growth would depend were the number of clinical pharmacists at the practice sites, the number of pharmacists at the practice sites, and the number of students requiring experiences.
Table 9.
APPE = advanced pharmacy practice experience
χ2 = 77.322, df = 6, p = 0.001
Table 10.
Respondents' Ratings of Factors on Which Their Projected Advanced Experiences Depend
Responses were given using a 5-point Likert scale, where 1 = not dependent on factor and 5 = highly dependent on factor
Based on their past history with student placements in introductory experiences, respondents projected that they could increase the number of introductory experiences in hospitals 125%, from 14,126 to 31,729 for 2012 graduates (Table 8). In constructing Tables 8 and 9, the median numbers of respondents' answers were used to construct the national estimates in 2012.
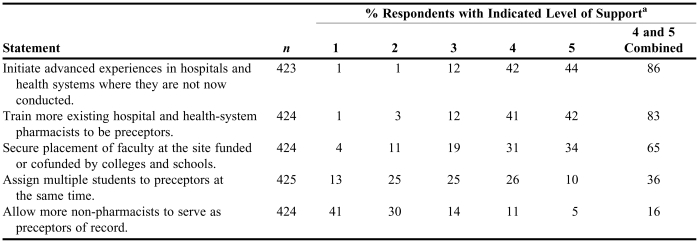
Strategies to increase the quantity of pharmacy experiential education in hospitals.
Respondents were asked to rank their agreement with the statements in Table 11. Highly favored approaches were to initiate advanced experiences in hospitals that did not already conduct them (86%) and to train more existing hospital and health-system pharmacists to be preceptors (83%). The respondents did not favor allowing more nonpharmacists to be preceptors.
Table 11.
Respondents' Level of Support of Suggested Methods for Increasing the Quantity of Experiential Education Placements
Responses were given using a 5-point Likert scale, where 1 = strongly discourage and 5 = strongly recommend
Respondents provided free-text comments about approaches they used to make introductory and advanced experiences more effective or easier to conduct. Among these were training preceptors, standardizing experiential education designs and grading across colleges and schools in their state, standardizing contracts across the colleges and schools with which they partnered, ensuring that students visit a different type of hospital (urban or rural, teaching or nonteaching) to gain perspective about the spectrum of hospital pharmacy services, ensuring that every student provides some direct patient care every day, and engaging the students in medication reconciliation and other clinical care.
Discussion and Implications
Experiential education constitutes at least 30% of the professional curriculum in doctor of pharmacy degree programs. Working assumptions in this report are that (1) experiential education is mostly carried out by volunteer practitioners regardless of setting (although some financial and nonfinancial support may be provided to practice sites), (2) approximately half of all experiential education for pharmacy students occurs in hospitals, and (3) the number of pharmacy graduates is expanding, and thus the experiential education capacity needs are expanding as well.
Capacity.
A primary purpose of this study was to determine whether there is sufficient capacity in hospitals and health systems to accommodate the increased number of students requiring introductory and advanced experiences. Based on findings projected to all U.S. hospitals and projected enrollment data of pharmacy students, at least through 2012 there may be adequate capacity in hospitals to conduct advanced experiences. Calculations supporting this take into account that the number of advanced experience placements in hospitals in 2012 for 10,655–14,790 graduates would be 42,620–59,160. According to the projected estimates of the numbers of graduates and based on survey responses, student placement capacity for advanced experiences in hospitals in 2012 is projected to accommodate 64,900 placements, indicating capacity in excess of the projected need. To achieve the growth projected for 2012 would require an 81% increase from 2007 levels in advanced experiences, with the greatest capacity for expansion occurring in hospitals that already participate.
Although respondents in this survey provided estimates of their future capacity for introductory experiences, they answered from the perspective of how those experiences were conducted before July 2007. Much is still unknown about the capacity to participate in introductory experiences consistent with the July 2007 ACPE standards. The need for introductory experiences likely will be greater in hospitals near colleges and schools, which are already the hospitals most engaged in experiential education.
The capacity of hospitals to accommodate increased student placements will depend on initiating experiential education in many hospitals that have never conducted such experiences before and on receiving the appropriate resources from colleges and schools. It will depend strongly on adequate staff (including clinical staff) and leadership in hospital pharmacy departments. With up to half of the required advanced experiences and an uncertain number of introductory experiences occurring in hospitals, it is in the interest of both partners (i.e., colleges and schools and hospital pharmacies) to collaborate and introduce students to hospital pharmacy practice early in the curriculum. Without an adequate pharmacy work force in hospitals, the delivery of quality experiential education in this setting will be difficult to accomplish.
Accomplishing growth in the number of experiential education experiences in hospitals will require direct interaction among college and school leaders, hospital pharmacy directors, and hospital administrators. Those administrators establish the performance constraints that pharmacy directors must meet with respect to staffing and service productivity. The case will have to be made clearly that there are benefits to hospitals33,34 and that hospitals have societal obligations related to their participation. Hospitals are eligible for financial incentives if they provide community service (e.g., indigent care, wellness promotion). Possibly an advocacy case can be made that experiential education for pharmacy students provides a service to the community by helping to sustain and build the nation's pharmacist work force.35
Factors influencing participation.
The findings indicate that current participation by hospitals and health systems in the sample is influenced by intrinsic motivation (e.g., professional responsibility, mission congruence, participation in other educational or training programs) and extrinsic factors (e.g., support from the colleges and schools, recruitment of residents and employees, expanding scope of services). Just over half (53%) of the respondents' hospitals participated in experiential education of pharmacy students because their hospitals included education explicitly in their missions (Table 3). Importantly, however, many hospitals that did not explicitly express education in their missions engaged in experiential education of various disciplines, including pharmacy experiential education (Table 2). Hence, it seems realistic to anticipate that hospitals would be likely to participate in pharmacy experiential education if they are engaged in experiential education of other professionals.
There are important insights in the findings with respect to experiential education and ASHP-accredited residency sites. Twenty-nine percent of respondents' hospitals conducted ASHP-accredited residencies; in 98% of these sites, the advanced experiences were also conducted (Table 2). Of the respondents who identified factors that contributed to their site's decision to conduct advanced experiences, 78% identified the potential for recruitment of residents or staff as a factor (Table 3).
Most ASHP-accredited residency positions are funded by the hospitals that conduct the residencies. However, some colleges and schools fund or cofund residency positions; 8% of respondents said that college and school funding of residencies was a current form of support from their college and school partners. Only 5%, however, said such funding was the most preferred form of support (Table 7). Increasing partnerships between hospitals and colleges and schools with respect to ASHP- accredited residencies and expanding the number of hospitals conducting such residencies could be avenues for increasing experiential education in hospitals.
Benefits.
The findings identified tangible benefits to hospitals, including advances in pharmacy services. This information may be useful to colleges and schools in communicating with hospital pharmacy directors and their administrators to formalize sustained partnerships for experiential education. Ninety percent of respondents agreed or strongly agreed that having their staff placed in preceptor roles stimulated them to maintain their knowledge and stay up-to-date. While 82% indicated that students could be assigned to activities that were mutually beneficial and while the expansion of such activities to include medication reconciliation and medication discharge counseling needs to be encouraged, these activities must be balanced with scheduling coordinated between hospitals and the colleges and schools.
Historically, early acculturation to professional practice was largely a function of employment, because students were not placed in practice settings as part of their educational program requirements until their final year. Introductory experiences can assist in the professionalization of students and provide opportunities to interest students in hospital and health-system practice early in their degree programs.36,37 The 59% of respondents who indicated they had hired students as pharmacists after graduation and the 30% that attracted residents after student exposure to advanced experiences at their hospitals received a positive return on their involvement in experiential education.
Challenges.
This study identified existing challenges for hospitals to conduct experiential education with colleges and schools. The most significant challenge to hospitals is the lack of availability of staff time to serve as preceptors. Many respondents cited a lack of readiness or competency of practitioners to be preceptors. In order for practitioners to be successful and effective preceptors, they need time to receive appropriate training and preparation, which is a staffing resource issue as well. Similarly, when forecasting their future capacity to accommodate students, respondents indicated that their projections were highly dependent on the number of pharmacists at their hospitals. Many respondents noted that their capacity projections were tied to their ability to expand clinical services at their hospitals. Since hospital pharmacist staffing levels have not increased appreciably in recent years,38 the ability of hospitals to ensure adequate staff time to serve as preceptors or to develop new services as a means of increasing student experience capacity is an issue that must be addressed. This comes at a time when hospital patient volumes and related pharmacy service demands are continuing to grow.39
A lack of standardization across administrative and academic processes, schedules, assessment tools, and requirements for students and preceptors presents challenges to hospitals, especially when partnering with multiple colleges and schools. Standardization can benefit students and colleges and schools as well. For instance, a standardized approach to the assessment of students' prior experiences in pharmacy settings (e.g., hospitals, health systems, community) may prove useful in matching students' learning objectives to learning experiences that can be provided by specific hospitals. Standardized assessment tools would ease the burden on preceptors and provide consistency in the students' experiences. Some respondents reported success in regional collaborative efforts with schools on some of these issues, suggesting that these challenges might be overcome. In addition, hospitals incur an administrative responsibility for orienting and processing students for their activities at their respective sites. Administrative requirements (e.g., criminal background checks, drug screens, immunizations) must be met before students can enter a facility, and standardization of such requirements among all academic programs and hospitals would be useful.
A lack of geographic proximity of hospitals to colleges and schools of pharmacy was cited as a universal challenge for hospitals precepting both introductory and advanced experience students as well as those not currently engaged in experiential education. While the location of a practice site cannot be changed, potential solutions include ready access to temporary housing and multiple placements in proximity to participating hospitals. Proximity is particularly a challenge for students seeking introductory experiences, since they may be partial-day experiences interwoven with class time. Introductory experience students often need more direct time from their preceptors, yet students' time at the hospital may be limited.
Resources.
Responsible and informed decisions are needed to align the needs and desires of hospitals engaged in experiential education with the type and extent of resources and other support available from the colleges and schools. There would be participation and resource implications for the colleges and schools if hospitals weighted the most desired support higher in their decisions to participate. Given the multiple sites required for experiential education, it is unrealistic to imagine that the colleges and schools will be able to place faculty members in all the hospitals participating in experiential education. Further, at any given site, managing the simultaneous presence of faculty members from multiple colleges and schools and their interfaces with staff would be challenging.
The survey contained no questions about the physical space and technological requirements for experiential education in hospitals; however, some respondents noted these areas as concerns. Hospitals may have many types of learners present at the same time (e.g., allied health, medicine, nursing), increasing the simultaneous demand for resources. Space can be limited, and physical access to equipment such as computers and medication-related devices (e.g., medication storage and vending cabinets) can be hindered when too many people are present. Capacity expansion, therefore, will in some cases depend on the physical space and other resources available at hospitals.
The survey contained no questions about pharmacy technicians, but respondents commented that greater freedom to expand the roles of qualified pharmacy technicians would enable pharmacists to devote more time to experiential education. Over time, this could become a contributing factor in the ability to expand capacity for experiential education.
Future collaborations.
Advances and improvements may be possible through appropriate joint work and advocacy by AACP and ASHP, as well as other stakeholders. In the recent past, AACP has focused on quality, capacity, and efficiency in experiential education as high priorities and will continue to do so. AACP leadership and resources are dedicated to providing programs, products, and services to assist colleges and schools and their practice partners in achieving quality experiential education.
The colleges and schools of pharmacy do not have the faculty resources to conduct experiential education on their own without partnering with practitioner preceptors.17,22 Training for preceptors is critical, especially if experiential education is to be expanded to practitioners who are not now engaged in it. ASHP-accredited residency programs have been invested in education and training for preceptors, which may partially account for why hospitals with ASHP-accredited residencies tend to be more engaged in experiential education of pharmacy students.
The survey findings identified benefits to hospitals, including advances in pharmacy services, which may be used by colleges and schools in fashioning communications to pharmacy directors and their administrators to formalize sustained partnerships for experiential education. These findings inform opportunities for AACP and ASHP to document and communicate the value of partnering between hospitals and colleges and schools for experiential education and to help their respective members in education and practice address the challenges to participation.
The findings point toward directions for future research inquiries, such as investigating the extent to which professional society membership is related to participation in the education of the profession's future work force. Case studies, reports, and investigations that demonstrate the value of sustained partnerships between academic pharmacy and hospital and health-system pharmacy practice should be pursued. Future investigations would be useful to better characterize and quantify introductory experiences and their effect on student career choice.
Limitations.
The overall response rate in this survey was 26%, and the response rate from hospitals was 21.2%. A higher response rate would provide a higher degree of confidence about the generalizability of the findings and projections. Pharmacy directors who are members of ASHP were surveyed, which may not be representative of all hospital pharmacy directors nationwide, though many of the issues identified with respect to experiential education may be similar among hospitals. Professional society members as a whole and the respondents in this study may be more likely to be advocates for the profession and more interested in providing educational experiences for future practitioners. Their professional affiliation with ASHP may have functioned as an optimistic bias for their future estimates to accommodate students requiring experiential education. However, many of the challenges that all sites face in conducting experiential education are probably similar. Lastly, the projections are based on estimated numbers of graduates through 2012. Those estimates could be incorrect. The findings are exploratory and informative and should be useful in action planning among hospitals and colleges and schools of pharmacy as well as AACP and ASHP.
Inferences of the study.
According to the projected estimates of the number of graduates and based on responses in this study, there could be adequate capacity in hospitals to conduct advanced experiences through at least 2012. Similarly, there appears to be capacity for expanding introductory experiences in hospitals. The projections, however, must be interpreted in light of the numerous factors described in this report. The expansion capacity for introductory experiences is less certain, given that the complete characteristics of introductory experiences that are compliant with ACPE's July 2007 requirements have yet to evolve. The greatest capacity for expansion of introductory and advanced experiences is in hospitals that already participate.
Preparation of the future pharmacist work force requires all stakeholders in pharmacy education and practice to engage in collaborative relationships that provide meaningful outcomes for all. The prospect of more than 10,000 pharmacy students annually contributing directly and indirectly to the patient care provided in U.S. hospitals and health systems, under the direction and mentoring of effective pharmacy preceptors, presents an opportunity for contributing to the public health on a scale not yet realized.
Action priorities.
The findings suggest several action priorities for AACP, ASHP, and other stakeholders and provide guidance to colleges and schools of pharmacy and hospital and health-system practice partners for enhancing the capacity, quality, efficiency, and success of partnerships for experiential education. These priorities include the following:
AACP and ASHP should collaborate to document and communicate the sustained value of partnerships between colleges and schools of pharmacy and hospitals and health systems with respect to experiential education as a means to encourage enhanced participation.
Academic pharmacy and hospital and health-system pharmacy should collaborate on an ongoing basis to stimulate reassessment of the current state laws and regulations that pertain to pharmacy students to promote student professionalization and maximize the student learning experience.
Leaders at the administrative level of colleges and schools of pharmacy, hospital and health-system pharmacy departments, and hospitals and health systems should engage in dialogue to initiate and sustain successful experiential education partnerships that provide mutual value for the colleges and schools and the hospitals and health systems.
Because future capacity is projected through 2012 in hospitals that currently participate as well as in those that have not participated, colleges and schools should target both in order to initiate new experiential education partnerships and expand learning experiences.
Academic pharmacy and health-system pharmacy should collaborate to ensure the availability and standardization of educational preparation for preceptors.
Because smaller hospitals are currently underrepresented in experiential education and have indicated a willingness to participate, ASHP should assist these institutions in practice model development and expansion of patient care to meet expectations for experiential education.
Colleges and schools should collaborate with hospitals and health systems to develop curricular models for introductory experiences in hospitals and health systems so that students progress from introductory to increasingly complex levels of pharmacy services as they advance in their doctor of pharmacy degree programs.
Given that hospitals and health systems currently partner with multiple colleges and schools and that increasing the number of experiential education placements of students is likely to increase the number of partnerships, standardization of processes and evaluations (administrative and academic) and a reduction in variance in scheduling (e.g., duration of experience, calendar) should be encouraged at multiple levels (national, regional, and local) to facilitate efficiency and quality.
CONCLUSION
A survey of pharmacy directors suggested an adequate capacity in U.S. hospitals to conduct advanced experiential education opportunities for pharmacy students under projected growth scenarios through 2012. Expanded capacity for introductory experiences was also reported.
NOTES
aFor brevity, in most places in this report, the term “colleges and schools” is used.
bpt?>Before the adoption of ACPE's July 2007 standards, the 2000 standards were the first to include any requirement about introductory experiences. Note that no guidance was provided to the colleges and schools about the quantity of introductory experiences required. The following excerpts (italics indicate added emphasis) were the only portions addressing introductory experiences:
[In Standard No. 11. Areas and Content of Curricular Core]: The areas and content of the curriculum in pharmacy should provide the student with a core of knowledge, skills, abilities, attitudes, and values which, in composite, relate to the professional competencies and outcome expectations … . The areas and content of the curricular core are as follows:
… professional experience, including introductory and advanced practice experiences acquired throughout the curriculum as a continuum, progressing from the Introductory Pharmacy Practice Experiences through the Advanced Pharmacy Practice Experiences in a variety of practice settings.
[In Guideline 11.5]:
The Introductory Pharmacy Practice Experiences should be offered in various practice settings during the early sequencing of the curriculum for purposes of providing transitional experiential activities and active learning. Such practice experiences should be organized as a curricular progression leading to advanced practice experiences so as to support growth in the student's capabilities to render pharmaceutical care. The scope and breadth of the introductory experiences should involve the initial development of practice skills, and should be consistent with these stated purposes. A quality control procedure should be established in accord with stated purposes and outcome expectations; the Introductory Pharmacy Practice Experiences may be designed in conjunction with didactic courses or as a discrete experiential offering.
REFERENCES
- 1.American Association of Colleges of Pharmacy. Academic practice partnership initiative. Summit to Advance Experiential Education in Pharmacy. Final report and proceedings. http://aacp.org/Docs/MainNavigation/Resources/7048_SummitFinalReport.pdf (accessed 2007 Nov 9).
- 2.American Association of Colleges of Pharmacy. Professional experience program (PEP) library of resources. www.peplibrary.vcu.edu/search.asp (accessed 2007 Nov 9).
- 3.American Association of Colleges of Pharmacy. Development of a profile system to display exemplary pharmacy practice experiential sites. http://aacp.org/Docs/MainNavigation/Resources/8615_QualityCriteria.pdf (accessed 2007 Nov 9).
- 4.American Association of Colleges of Pharmacy. The 2007–2008 Crystal APPLE Award. http://aacp.org/site/page.asp?TRACKID=&VID=1&CID=1379&DID=7928 (accessed 2007 Nov 9).
- 5.Bradberry JC, Droege M, Evans RL, et al. Curricula then and now—an environmental scan and recommendations since the commission to implement change in pharmaceutical education: report of the 2006-2007 academic affairs committee. Am J Pharm Educ. 2007;71 article S10. [Google Scholar]
- 6.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree: standard no. 9. www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf (accessed 2008 Jul 28).
- 7.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree: standard no. 13. www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf (accessed 2008 Jul 28).
- 8.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree: standard no. 10. www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf (accessed 2008 Jul 28).
- 9.Peters SJ, MacKinnon GE., III Introductory practice and service learning experiences in US pharmacy curricula. Am J Pharm Educ. 2004;68 article 27. [Google Scholar]
- 10.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree: guideline 14.4. www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf (accessed 2008 Jul 28).
- 11.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree: appendix C. www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf (accessed 2008 Jul 28).
- 12.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree: guideline 14.5. www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf (accessed 2008 Jul 28).
- 13.U.S. Department of Health and Human Services. The pharmacist workforce: a study of the supply and demand for pharmacists. http://bhpr.hrsa.gov/healthworkforce/reports/pharmacist.htm (accessed 2007 Nov 9).
- 14.American Society of Health-System Pharmacists. 2006 ASHP pharmacy staffing survey results. www.ashp.org/s_ashp/docs/files/PPM_2006StaffSurvey.pdf (accessed 2007 Nov 9).
- 15.Knapp DA. Professionally determined need for pharmacy services in 2020. Am J Pharm Educ. 2002;66:421–9. [Google Scholar]
- 16.Joint Commission of Pharmacy Practitioners. JCPP future vision of pharmacy practice, final version.www.aacp.org/Docs/MainNavigation/Resources/8597_JCPPVisionStatement.pdf (accessed 2007 Nov 9).
- 17.Harralson AF. Financial, personnel, and curricular characteristics of advanced practice experience programs. Am J Pharm Educ. 2003;67 article 17. [Google Scholar]
- 18.Littlefield LC, Haines ST, Harralson AF, et al. Academic pharmacy's role in advancing practice and assuring quality in experiential education: report of the 2003-2004 professional affairs committee. Am J Pharm Educ. 2004;68 article S8. [Google Scholar]
- 19.Reynolds JR, Briceland LL, Carter JT, et al. Experiential education delivery: ensuring success through support and development of the faculty and administrative team: report of the 2004-2005 professional affairs committee. Am J Pharm Educ. 2005;69 article S9. [Google Scholar]
- 20.Draugalis JR, Carter JT, Slack MK. Curricular and financial implications of PharmD clerkship placements. Am J Pharm Educ. 1996;60:146–51. [Google Scholar]
- 21.Plaza CM, Draugalis JR. Implications of advanced pharmacy practice placements. Am J Pharm Educ. 2000;64:404–9. [Google Scholar]
- 22.O'Sullivan T, Hammer DP, Manolakis PG, et al. Pharmacy experiential education present and future: realizing the Janus vision. A background paper for the AACP APPI Summit to Advance Experiential Education in Pharmacy. [accessed 2007 Nov 9]; www.pubinfo.vcu.edu/pharmacy/peplibrary/resources/AACP_SummitBackgroundPaper.pdf . [Google Scholar]
- 23.Plaza CM, Draugalis JR. Implications of advanced pharmacy practice placements: a 5-year update. Am J Pharm Educ. 2005;69 article 45. [Google Scholar]
- 24.Data on file. American Society of Health-System Pharmacists, Bethesda, MD.
- 25.American Association of Colleges of Pharmacy. Profile of pharmacy students 2005–06. Applicant pool degrees conferred 2005–06. www.aacp.org/site/page.asp?TRACKID=&VID=1&CID=1420&DID=8230 (accessed 2008 Jan 2).
- 26.Willis GB. Cognitive interviewing. A “how to” guide. http://appliedresearch.cancer.gov/areas/cognitive/interview.pdf (accessed 2007 Nov 9).
- 27.Chase P. Rethinking experiential education (or does anyone want a pharmacy student?) Am J Pharm Educ. 2007;71 doi: 10.5688/aj710227. article 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lubowski TJ, Cronin LM, Pavelka RW, et al. Effectiveness of a medication reconciliation project conducted by PharmD students. Am J Pharm Educ. 2007;71 doi: 10.5688/aj710594. article 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walker PC, Flanders SA, Tucker-Jones J et al. Pharmacist facilitated discharge: a prospective study of medication reconciliation and telephone follow-up interventions. Paper presented at ASHP Summer Meeting. San Francisco, CA; 2007 Jun 25.
- 30.Padiyara RS, Rabi SM. Pharmacy students and reconciliation of medication upon hospital admission. Paper presented at ASHP Midyear Clinical Meeting. Anaheim, CA; 2006 Dec 5.
- 31.Ahmed KM, Bazrafshan P, Ahmed S. Medication reconciliation involving an intern pharmacist in an acute care facility. Paper presented at ASHP Summer Meeting. San Francisco, CA; 2007 Jun 25.
- 32.Knapp KK, Cultice JM. New pharmacist supply projections: lower separation rates and increased graduates boost supply estimates. J Am Pharm Assoc. 2007;47:463–70. doi: 10.1331/JAPhA.2007.07003. [DOI] [PubMed] [Google Scholar]
- 33.Skrabal MZ, Kahaleh AA, Nemire RE, et al. Preceptors' perspectives on benefits of precepting student pharmacists to students, preceptors, and the profession. Am J Pharm Educ. 2006;46:605–12. doi: 10.1331/1544-3191.46.5.605.skrabal. [DOI] [PubMed] [Google Scholar]
- 34.Lin AY, Altiere RJ, Harris WT, et al. Leadership: the nexus between challenge and opportunity: reports of the 2002-03 academic affairs, professional affairs, and research and graduate affairs committees. Am J Pharm Educ. 2003;67 article S05. [Google Scholar]
- 35.Sandrick K. Defining and measuring community benefit. www.hhnmag.com/hhnmag_app/jsp/articledisplay.jsp?dcrpath=HHNMAG/PubsNewsArticle/data/2006November/0611HHN_FEA_Boardroom&domain=HHNMAG. (accessed 2007 Nov 8).
- 36.MacKinnon GE, III, McAllister DK, Anderson SC. Introductory practice experience: an opportunity for early professionalization. Am J Pharm Educ. 2001;65:247–53. [Google Scholar]
- 37.Plake KS, Wolfgang AP. Impact of experiential education on pharmacy students' perceptions of health roles. Am J Pharm Educ. 1996;60:13–9. [Google Scholar]
- 38.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: patient monitoring and education—2006. Am J Health-Syst Pharm. 2007;64:350–65. doi: 10.2146/ajhp060669. [DOI] [PubMed] [Google Scholar]
- 39.American Hospital Association. Chartbook: trends affecting hospitals and health systems. Chapter 3: utilization and volume. www.aha.org/aha/research-and-trends/chartbook/ch3.html (accessed 2008 Feb 12).