Abstract
The Prescription Drug Use Questionnaire (PDUQ) is one of several published tools developed to help clinicians better identify the presence of opioid abuse or dependence in patients with chronic pain. This paper introduces a patient version of the PDUQ (PDUQp), a 31-item questionnaire derived from the items of the original tool designed for self-administration, and describes evidence for its validity and reliability in a sample of patients with chronic nonmalignant pain and on opioid therapy. Further, this study examines instances of discontinuation from opioid medication treatment related to violation of the medication agreement (MAVRD) in this population, and the relationship of these with problematic opioid misuse behaviors, PDUQ and PDUQp scores. A sample of 135 consecutive patients with chronic nonmalignant pain was recruited from a multidisciplinary Veterans Affairs chronic pain clinic, and prospectively followed over one year of opioid therapy. Utilizing the PDUQ as a criterion measure, moderate to good concurrent and predictive validity data for the PDUQp are presented, as well as item-by-item comparison of the two formats. Reliability data indicate moderate test stability over time. Of those patients whose opioid treatment was discontinued due to MAVRD (n = 38 or 28% of sample), 40% of these (n = 11) were due to specific problematic opioid misuse behaviors. Based upon specificity and sensitivity analyses, a suggested cut-off PDUQp score for predicting MAVRD is provided. This study supports the PDUQp as a useful tool for assessing and predicting problematic opioid medication use in a chronic pain patient sample.
Keywords: Chronic nonmalignant pain, opioid medications, substance use disorder, problematic opioid use and/or misuse, medication agreements
Introduction
The past 25 years have witnessed a sea change in the use of opioid analgesics for the management of chronic nonmalignant pain (CNMP). Challenging previous concerns that tolerance, side effects or non-responsiveness would ultimately result in treatment failure, Portenoy and Foley (1) provided credible and provocative evidence that opioids could be effective for the treatment of CNMP. Since that time, increasingly rigorous research has supported this conclusion, with opioid therapy demonstrating meaningful improvements in pain severity, affective distress, and quality of life for many patients with CNMP of inflammatory and/or neuropathic origin (2–5). Coupled with recent concerns about the daily use of nonsteroidal anti-inflammatory analgesics (6), clinicians are increasingly prescribing long-acting opioids (i.e., oxycodone, hydrocodone) for the treatment of CNMP (7).
Although influential, there are important limitations to these data. As noted in recent meta-analyses (8, 9), the long-term safety of opioids with respect to addiction outcomes remains poorly described. A barrier to doing so has been the inconsistency with how the term or concept of addiction has been defined in these clinical studies, thus making estimates of incidence or prevalence imprecise. It is well recognized that there are unique difficulties associated with applying standard Diagnostic and Statistical Manual of Mental Disorders (4th edition, text revision) (DSM-IV-TR®) psychiatric criteria for the substance use disorders (substance abuse and substance dependence) (10) in patients for whom opioids are prescribed (see 11–13). For example, several commonly-accepted markers for addiction in this population (e.g., drug-seeking behaviors, history of drug use) have been shown to have only modest specificity for substance use disorders in this population (14, 15). In fact, the presence of aberrant drug using behaviors in pain patients can reflect such phenomena as pseudoaddiction (drug-seeking behaviors based on inadequate pain relief [16]), or medication misuse (noncompliance, recreational use, diversion), and not a substance use disorder (SUD) per se (17). In this paper, we will follow the terminology suggested by Ballantyne and LaForge (12) and refer to an opioid SUD as opioid addiction, and the presence of aberrant behaviors related to opioid treatment, in the absence of clearly identified addiction, as opioid misuse or problematic opioid use.
Several assessment tools have been recently published designed to either predict which pain patients will develop opioid addiction (18, 19), and/or identify those with opioid SUD, at the time of the exam (14, 20–22). One of these, the Prescription Drug Use Questionnaire (PDUQ) (14), was developed to help clinicians detect addiction in pain patients, and was specifically validated against expert clinician diagnosis of SUD. The aim of the instrument was to identify CNMP patients with addiction, and it included items that assessed both current medication use behaviors as well as historical risk factors that together would support the diagnosis of a SUD. The PDUQ subsequently has been used as a comparison measure in validating other assessment tools (18, 20, 21).
The 42-item (39 scored items) PDUQ was developed to be administered in an interview format, and takes approximately 20 minutes to complete by a trained clinician. Since many of the PDUQ questions are amenable to being answered by the patient him- or herself, we hypothesized that this item set may be useful as the foundation for a patient self-report tool to predict or identify opioid addiction in chronic pain patients on opioid therapy. Development of a self-administered assessment tool is potentially advantageous in terms of ease of data collection, decreased clinician burden, and possibly increased candidness of responses due to responding to written questions versus an interviewer.
The use of medication agreements have been recommended in recent opioid prescription guidelines to help specify appropriate opioid use behaviors and monitor for (via contract violations) the emergence of behaviors indicative of addiction, as well as promote safe and effective use of opioid medications (23–28). These agreements typically include behavioral guidelines such as proscription of alcohol or other substance use and adherence to clinic protocols such as submission to urine toxicology screens, maintenance of agreed upon medication schedules, use of a single provider for opioid prescriptions, and keeping scheduled appointments. In many settings, violation of these medication agreements results in discontinuation of prescribed opioid medications. Although imperfect, medication agreement violation-related discontinuations (MAVRD) may therefore be viewed as a rough proxy for problematic opioid medication use, and which in a certain percentage of cases, represent true opioid SUD. In their follow-up of patients using opioid contracts with chronic pain management, Hariharan and colleagues (26) found that 17% of patients had their opioid contracts cancelled by the physician. Of these, 50% were discontinued due to positive urine toxicology screens (marijuana or cocaine), 26% for prescription opioid abuse, and 7% for contract rule violations. We expect that MAVRD is a reasonable indicator of problematic substance use, but not a specific indicator of opioid addiction.
The aims of the present study are twofold. First, we evaluated the preliminary psychometric properties of a self-administered version of the PDUQ (herein referred to as the PDUQp). Included are estimates of reliability, validity, and sensitivity and specificity with respect to two criterion measurements: 1) MAVRD and 2) behaviors specific to opioid misuse. Secondly, in an effort to evaluate the predictive utility of the PDUQ for problematic opioid use, we examined the contribution of baseline PDUQp scores and patient characteristics (demographics, pain, affect, disability) in predicting subsequent MAVRD.
Methods
Participants
A sample of 135 consecutive patients with chronic nonmalignant pain was prospectively followed over one year of opioid therapy. Participants were veterans recruited from a chronic pain clinic at the Greater Los Angeles Veterans Affairs Healthcare System. Based upon the Structured Clinical Interview for DSM-IV-TR (29), patients diagnosed with current SUD were excluded from study participation in accordance with hospital policies restricting the prescription of opioids to individuals with this diagnosis. This study was approved by the local institutional review board, and participants were asked to give signed consent prior to enrollment.
Participants visited the chronic pain clinic on a monthly basis in order to refill their opioid prescriptions. At baseline and every month, participants completed various assessments reviewing pain, pain relief, mood, and medication use over the course of the month prior, as well as an assessment of disability every 4 months. At baseline and every four months, the PDUQp was administered to all subjects; to enable psychometric analyses, the original PDUQ was administered at months 4, 8, and 12.
Measures
Prescription Drug Use Questionnaire (PDUQ)
As previously noted, the PDUQ is one of several published tools designed to help the clinician identify addiction in pain patients on chronic opioid therapy. Unique in that scores have been validated against clinical expert diagnosis of SUD, the questionnaire (1) consists of 39 scored items evaluating five different domains of problematic opioid analgesic use in chronic pain patients, including the characteristics of the pain condition, opioid use patterns, social/family factors, familial/personal history of substance abuse/dependence, and psychiatric history. Limitations of the tool relate to its feasibility of use in the busy clinical setting, and its reliance on patient veracity. PDUQ responses and scores were utilized as comparators for PDUQp responses and scores in evaluation of the validity of the latter.
Prescription Drug Use Questionnaire-Patient Version (PDUQp)
The PDUQp was developed to replicate items from the original PDUQ, but in a self-administered format. Questions were re-worded to address patients directly (i.e., “Have you ever …” as opposed to “Has the patient ever…”). Six items not demonstrated to be good predictors of SUD in the original validity analysis (14) were not duplicated in the PDUQp. Specifically deleted were five items evaluating psychiatric history, and one item on prescription forgery, which was never endorsed by a single participant in the original tool. Two additional items were lost as the number of family-related questions was streamlined from 8 to 6 items. The resulting PDUQp includes 31 self-administered items effectively equivalent to PDUQ content (see Appendix). Scoring procedures replicated the PDUQ, with an affirmative response receiving a score of 1 (except for item 6, which was reverse scored), and summing for the total score. As in the PDUQ, item 1 (“do you have more than one painful condition?”) was not included in the total score. The total score for the PDUQp therefore ranges between 0 and 30.
Criterion Variables
To evaluate the specificity and sensitivity of the questionnaire, PDUQp responses and scores will be compared to two criterion variables: (1) discontinuation of treatment for any medication agreement violation (MAVRD), and (2) discontinuation for problematic opioid use behaviors in particular.
Medication Agreement Violation-Related Discontinuation (MAVRD)
For the purposes of these analyses, MAVRD was defined as any clinician-initiated opioid medication discontinuation secondary to evidence of medication use behaviors in violation of those stipulated in the Medication Agreement signed by both the patient and clinician at the initiation of treatment. Discontinuation decisions were made as a group by a multidisciplinary pain treatment team based on results of urine toxicology screens, evidence of medication agreement violations, and other factors such as observed alcohol intoxication or inappropriate behaviors in clinic. Primary members of the multidisciplinary team were all chronic pain specialists (psychologists and physicians), and the same team followed patients over an extended period of time. The team was cognizant of the difficulty in determining if a specific behavior was due to inadequate pain relief (i.e. pseudoaddiction), and was careful to only discontinue patients if the non-compliance behaviors did not cease with increased opioid provision (i.e. repeated violations). MAVRD status was evaluated every four months via chart review for the one-year duration of the study.
Opioid-Specific Misuse Behaviors
In that a MAVRD can reflect violations unrelated to the misuse of opioids, specific reasons for MAVRD were further inspected to identify those patients who were discontinued from treatment related to problematic opioid use in particular. Based on review of specific reasons for MAVRD, patients were categorized into one of three groups: 1) MAVRD specific to opioid use; 2) MAVRD related to use of other, non-opioid illicit substances; and 3) MAVRD related to other medication agreement noncompliance. This more detailed examination of MAVRD provided a more stringent criterion for the evaluation of opioid misuse or addiction. The category of “other medication agreement noncompliance” included patients with noncompliant behaviors that could not be clearly linked with problematic opioid use. For example, this might include presenting with urine toxicology screens with negative findings for the prescribed opioid medications or repeatedly running out of medications early or refusing to bring in remaining pills. Although more specific, problematic opioid use behaviors are not indicative of addiction, as these can also reflect of problematic opioid use, pseudoaddiction, or drug diversion.
Patient Characteristic Variables
Certain patient variables were inspected at baseline and every four months to evaluate their utility as predictors for MAVRD. Baseline demographics considered in these analyses were age, marital status, and employment status. Subjective perceptions of the pain condition were captured using four 10cm visual analogue scales (VAS) ranging from 0 to 10 rating the usual intensity of pain over the past month (0 - no pain, 10 - most intense pain imaginable), mood over the past month (0- extremely good mood, 10 – extremely bad mood), and the degree to which pain interfered with activity (0 – no interference, 10 – complete interference). Evidence for affective mood was evaluated using scores on the Hospital Anxiety and Depression Scales (30, 31). As a measure of patient functionality, the 10-item OSWESTRY pain disability questionnaire index (32, 33) was calculated at each study time point.
Analysis
Following descriptive analyses of the sample and study variables, the concurrent and predictive validity of the PDUQp was evaluated (using the original PDUQ as criterion variable), and the test-retest reliability from baseline to 4, 8, and 12 months calculated. To determine the specificity and sensitivity of the questionnaire, PDUQp scores were compared to the two criterion variables: 1) discontinuation for a medication agreement violation (MAVRD) in general, and 2) discontinuation for problematic opioid use behaviors in particular. Addressing the second aim of the study, baseline PDUQp score and patient characteristics (demographics, pain, affect, disability) were entered into a logistic regression analyses to identify predictors of subsequent MAVRD.
Results
Demographics
Based on initial general categorization, 104 participants had a primary musculoskeletal pain problem, 26 participants had a primary neuropathic pain problem, and the remaining five participants had multi-category pain problems or it was unclear into what category the primary pain problems fit. The majority of patients (75%) reported that their pain was always present, 16% reported it was often present, and remainder reporting rare or variable pain. Mean age of the sample was 53, and ranged from 25 to 65 years old. The study sample included eight female and 127 male participants, with the high male-to-female ratio typical of Veterans Affairs populations, and precluded gender-specific analyses. Regarding marital status, 53 participants (39%) were married or living with their partner, 18 participants (13%) were never married, 54 participants (40%) were divorced or separated, and eight participants (6%) were widowed. Seventeen participants (13%) were working full-time, eight (6%) were working part-time, and the remainder (81%) were not working. Of the 105 participants who were not working, approximately 45% (47 participants) indicated that they were unemployed or unable to work due to pain.
PDUQp Descriptive Analysis
PDUQp responses showed that most patients (83%) reported having more than one painful condition, being disabled by pain (88%), and receiving disability payments (77%). Many in this sample also self-reported having tried non-medication approaches (81%), feeling that their pain had been well-managed over the past 6 months (53%), and that their family understood (90%) and participated in their pain care (51%). With respect to medication use, 47% reported having had to increase their use of pain medications over the past six months, and 58% felt that certain opioid medications were more effective than others. Baseline pain characteristics (severity, mood, functionality) and PDUQp scores for the sample are provided in Table 1.
Table 1.
Baseline Pain and PDUQp Values
| Non-MAVRD | MAVRD | Total | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| VAS Usual (cm) | 6.65 | 2.07 | 7.03 | 1.32 | 6.75 | 1.89 |
| VAS Mood (cm) | 5.31 | 2.60 | 5.95 | 2.46 | 5.49 | 2.57 |
| OSWESTRY | 48.35 | 13.55 | 47.86 | 13.17 | 48.21 | 13.39 |
| PDUQp | 8.95 | 2.85 | 10.32 | 3.65 | 9.34 | 3.15 |
PDUQp Validity
PDUQp Concurrent Validity - PDUQ Criterion
There was a significant concurrent correlation between PDUQp and PDUQ at the 4-month timepoint (r=0.64, P<0.001). This correlation reveals a moderately strong concurrent validity between the PDUQp and PDUQ, but is lower than would be expected based on the corresponding nature of the items between the PDUQp and PDUQ (i.e., alternate form reliability). To investigate possible sources of disagreement, analysis was done, removing those items on the PDUQ that were not included in the PDUQp, and correlating the new total scores. The results did not change, in that the correlation coefficient between the PDUQp and revised PDUQ total score at 4 months was r=0.61 (P<0.001). Total scores from the PDUQp and the equivalent item sets from the PDUQ were then compared, revealing that total scores for the PDUQ equivalent item sets were consistently lower than PDUQp total scores. Scores were as follows: 4months (PDUQp mean score = 8.08, PDUQ equivalent items total mean score = 6.56), 8months (PDUQp mean score = 8.18, PDUQ equivalent items total mean score = 5.99), and 12 months (PDUQp mean score = 7.82, PDUQ equivalent items total mean score = 5.20).
PDUQp Predictive Validity - PDUQ Criterion
Within this sample, the PDUQ showed good stability over time with significant correlations between the PDUQ total score at 4 months and 8 months (r=0.72, P<0.001), and from 4 months to 12 months (r=0.62, P<0.001). Regarding the relationship between the PDUQp and later PDUQ scores, there were weaker, but significant correlations between the PDUQp at baseline and the PDUQ total score at 4 months (r=0.48, P<0.001), 8 months (r=0.43, P<0.001), and 12 months (r=0.31, P<0.05).
Item-by-Item Response Patterns
An item-by-item analysis of response discrepancies was used to further examine possible sources of variance between scores on the PDUQ and PDUQp. Cross-tabulations were examined between equivalent items from the PDUQp and PDUQ. Using the item responses from the PDUQ as the criterion variable, this analysis allows for an examination of true positives and true negatives, along with response disagreements per item. Figure 1 displays a graphical representation of the percent disagreement on equivalent items of the PDUQp and PDUQ, with % subject disagreement PDUQ+ representing the degree to which subjects responded positively on the PDUQ but negatively on the PDUQp, and % subject disagreement PDUQp+ representing the opposite discrepancy trend.
Figure 1.
Percent disagreement on items at four-month timepoint.
As can be noted, item numbers 11, 16, 22, and 23 show the greatest degree of discrepancy with large numbers of patients responding positively on the PDUQp but negatively on the PDUQ. These items are as follows: (PDUQp 11) need to increase amount of pain medications in past 6 months, (PDUQp 16) thinking that certain medications work better or preferring certain medications over others, (PDUQp 22) family understanding and agreeing with patient’s use of medications, and (PDUQp 23) family helping to take care of patient due to pain problem. Upon removing these discrepant items from both the PDUQp and PDUQ, the correlation at four months between the PDUQp and PDUQ equivalent items set (r=0.65, P<0.001) was not different from previous calculations.
PDUQp Reliability
PDUQp Stability Over Time
There were significant correlations between the PDUQp from baseline to four months (r=0.67, P<0.001), eight months (r=0.61, P<0.001), and 12 months (r=0.40, P=0.001), providing evidence of good test-retest reliability.
PDUQp Sensitivity and Specificity - MAVRD and Opioid-Specific Use Behaviors
The utility of the PDUQp was examined by calculating the sensitivity and specificity of the tool using two different criteria: 1) the more general MARVD or 2) discontinuation due to Opioid-specific use behaviors. From the original sample, 38 subjects (28%) had their opioid medications discontinued due to Medication Agreement Violations (see Table 2). Using the more specific opioid use criteria, 15 subjects (11%) were discontinued due to specific opioid misuse behaviors, 13 subjects (9.6%) were discontinued due to use of other illicit substances, and 10 subjects (7.4%) were discontinued due to other medication agreement noncompliance. Thus, 40% of all MAVRD were attributed to opioid misuse behaviors.
Table 2.
Reasons for Early Termination
| Reason for discontinuation | No. |
|---|---|
| Medication agreement violation | 38 |
| Patient voluntary withdrawal | 17 |
| Surgical/medical reasons | 10 |
| Psychiatric/mental health reasons | 2 |
| Other | 2 |
| Total patient drop-out | 69 |
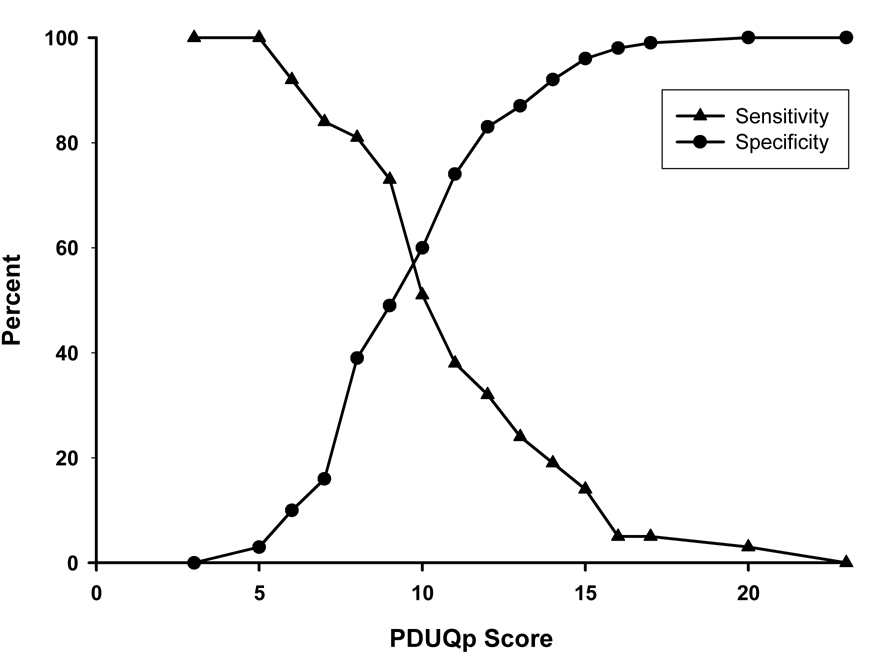
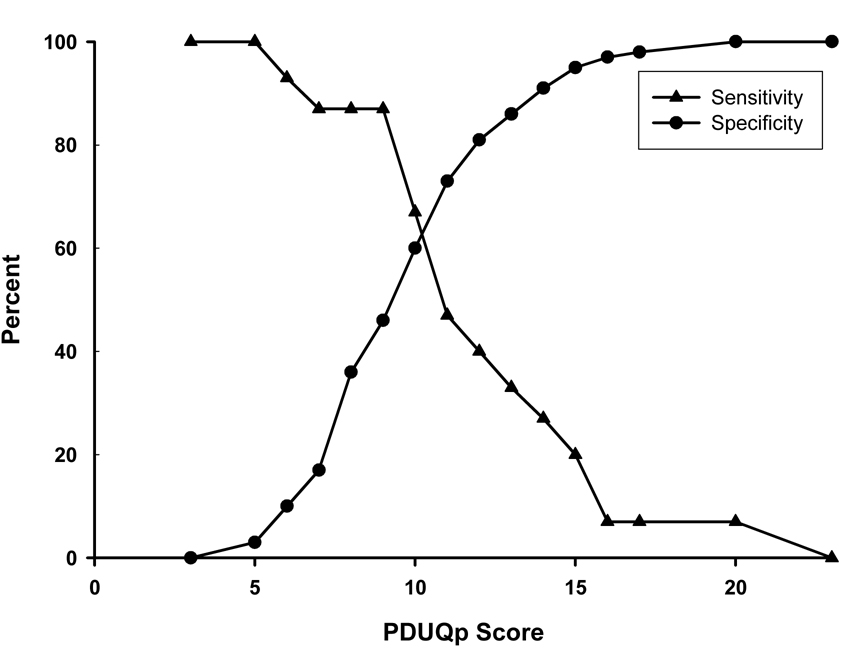
Sensitivity / Specificity Analyses
Figure 2 and Figure 3 display graphs of sensitivity and specificity statistics for the PDUQp total score based on comparison with the general MAVRD discontinuation criterion and the opioid-specific use criterion respectively. As can be seen from these graphs, a cut-off score of 10 or greater appears to provide optimal sensitivity and specificity for both criteria. As expected, the PDUQp shows slightly higher levels of sensitivity at this optimal cut-off point using the more stringent opioid-specific use criterion (sensitivity = 66.7% / specificity = 59.7%) as compared with the more general MAVRD criterion (sensitivity = 51.4% / specificity = 59.8%). The differences in specificity are however small and may not be of significant difference in the clinical setting.
Figure 2.
PDUQp sensitivity / specificity with MAVRD Criterion.
Figure 3.
PDUQp sensitivity / specificity with Opioid Misuse Criterion.
Item Correlations with Discontinuation Criteria
Table 3 displays correlation coefficients along between PDUQp items and the MAVRD and opioid-specific use criteria respectively. Significant correlations were found between the MAVRD criterion and items 1 (having more than one painful condition), 8 (receiving pain medications from more than one clinic), 17 (ever lost pain medications), 29 (having an alcohol or drug SUD diagnosis previously), and 30 (having a drug or alcohol abuse treatment history). There was a negative correlation between the MAVRD criterion and item 23 (family caring for patient due to pain problem). Significant correlations were found between the opioid-specific use criterion and following items: 5 (has tried non-medication treatments), 8 (receiving pain medications from more than one clinic), 9 (thinking they might be addicted to pain medications), 17 (ever lost pain medications), 18 (needing to go to emergency room for pain medications), and 30 (history of alcohol or drug abuse treatment).
Table 3.
PDUQp Item Correlations with MAVRD versus Opioid Misuse Criteria
| MAVRD Criterion | Opioid Misuse Criterion | |
|---|---|---|
| PDUQp Item Number | Phi Correlation Coefficient | Phi Correlation Coefficient |
| 1 | 0.23a | 0.16 |
| 2 | 0.06 | 0.05 |
| 3 | 0.00 | −0.10 |
| 4 | −0.07 | −0.02 |
| 5 | 0.13 | 0.17a |
| 6 (reverse-score) | −0.11 | −0.05 |
| 7 | −0.11 | 0.00 |
| 8 | 0.20b | 0.31a |
| 9 | 0.07 | 0.19b |
| 10 | −0.10 | −0.04 |
| 11 | 0.11 | 0.05 |
| 12 | 0.03 | 0.07 |
| 13 | 0.04 | 0.13 |
| 14 | 0.09 | 0.02 |
| 15 | 0.05 | 0.06 |
| 16 | 0.06 | 0.03 |
| 17 | 0.20b | 0.21b |
| 18 | 0.08 | 0.19b |
| 19 | −0.02 | −0.07 |
| 20 | −0.01 | 0.07 |
| 21 | 0.00 | 0.14 |
| 22 | 0.00 | 0.09 |
| 23 | −0.18b | −0.17 |
| 24 | 0.02 | 0.11 |
| 25 | −0.10 | −0.05 |
| 26 | 0.14 | 0.17 |
| 27 | 0.09 | 0.09 |
| 28 | 0.09 | −0.10 |
| 29 | 0.30a | 0.14 |
| 30 | 0.34a | 0.19b |
| 31 | 0.00 | 0.17 |
P < 0.01.
P < 0.05.
Comparison of PDUQ and PDUQp Total Scores by Discontinuation Status
T-tests revealed significant differences (P<0.05) between PDUQp total scores at baseline between patients whose medications were discontinued due to MAVRD criterion (x = 10.32) and non-MAVRD patients (x = 8.95). After more specific categorization of patients by reason for discontinuation, there was a significant difference (P<0.01) between PDUQp total scores at baseline between non-MAVRD patients (x=8.95) and patients whose medications were discontinued due to opioid-specific use behaviors (x=11.33), but no significant difference between non-MAVRD patients and patients whose medication agreement violations were non-opioid related violations (i.e., abuse of other substances, clinic non-compliance (x=9.64)).
T-tests also indicated a significant difference (P<0.05) on PDUQ total scores at the four-month time point between MAVRD patients (x=10.08) and non-MAVRD patients (x=8.20). There was a significant difference (P<0.05) between PDUQ total score at 4 months between non-MAVRD patients (x=8.20) and patients whose medications were discontinued due to opioid-specific use behaviors (x=10.67), but no significant difference between non-MAVRD patients and patients whose medication agreement violations were non-opioid related violations (x = 9.73). These data on PDUQ and PDUQp scores by discontinuation status suggest a strong positive relationship between PDUQp scores and opioid-related reasons for discontinuation.
Predictors of MAVRD
As noted, patient attrition from treatment was notable; starting with a sample size of 135, 66 (49%) remained in treatment by study end, with MAVRD accounting for the largest number of discontinuations (38 or 28% of the sample). The rate of attrition from the study was relatively constant over time points (approximately 20 patients dropped per four-month interval); slopes of drop-out were similar between patients with MAVRD and those who either completed the study or otherwise discontinued for non-medication-related reasons (non-MAVRD).
Broadening the use of the PDUQ beyond identification of addiction in CNMP, binary logistic regression analysis was performed to learn the relative contribution of predictor variables to MAVRD. Predictor variables (age, marital status, employment status, usual pain VAS, mood VAS, OWESTRY index, and baseline PDUQp score) were entered in a forward likelihood-ratio method of entry, with criteria for entry set at P = 0.05 and removal at P =0.10. The resultant model contained only one variable, PDUQp score (B = 0.142, P = 0.03), and was demonstrated to provide good prediction of MAVRD (model chi-square = 5.06, P = 0.024), and to fit the data well (Hosmer and Lemeshow Goodness-of-Fit Chi square = 9.19, n.s.). Overall, an increase in the baseline PDUQp score increased the odds of MAVRD occurring by a factor of 1.15.
Discussion
Assessing abuse of or dependence on prescription opioids in chronic pain patients is a challenging task for the clinician (34, 35), complicated by the lack of diagnostic clarity in defining SUD in this group (12–14, 36). It has been noted that traditional diagnostic criteria used by mental health specialists for SUD may not adequately distinguish between chronic pain patients on opioid treatment with and without these disorders due to their diagnoses’ reliance on physical dependence, tolerance, and desire to cut down or stop use, all of which are expected responses to the chronic use of prescribed opioids (13, 17). In response to this diagnostic uncertainty, The American Academy of Pain Medicine, American Pain Society, and the American Society of Addiction Medicine (37) developed a consensus document defining dependence, tolerance, and addiction, describing behaviors characteristic of addiction in the context of the use of opioids in the treatment of pain. Though this work has been beneficial with respect to clarifying terminology, translation of these to specific pain patient characteristics and drug using behaviors in the clinical setting remains incomplete.
The overall goal of this study was to contribute to the emerging literature on predicting and identifying opiate misuse and addiction among chronic pain patients on opioid maintenance therapy in two ways. Firstly, a patient version of the PDUQ (the PDUQp) was developed and introduced, with preliminary evidence for validity and reliability provided. Further, the phenomenon of MAVRD was described with emphasis on how it relates to self-reported prescription drug use behaviors as well as other demographic and pain-related variables. Data collected have clear implications for both the identification and prediction of problematic opioid use in the clinic setting.
The PDUQp
Regarding its validity, the patient-administered PDUQp showed statistically significant concurrent and predictive validity with the original PDUQ, and moderate stability over time. Based on t-test results, PDUQp total score was able to distinguish between patients whose opioids were eventually discontinued due to problematic opioid use (MAVRD or opioid-specific use) as compared with patients who either completed the one-year study period or discontinued from the study for other reasons. Additionally, within a logistic regression analysis, the PDUQp score was a significant predictor of MAVRD as compared with other baseline variables including demographic variables, average pain, and mood, and disability. Although the PDUQp was related to the opioid misuse in this study, the diagnosis of SUD was not specifically evaluated, so we cannot determine directly its correspondence with this psychiatric diagnosis.
Although the PDUQ and the PDUQp had almost identical item content, the criterion validity analysis indicate that the tools should be viewed as measures of a similar construct, as opposed to alternative forms of the same instrument. The exploratory item-based analyses suggest the differences between the instruments are not the result of any small subset of items but more likely represent more general variability between a patient’s and clinician’s views of the wide range of behaviors included in the tests. Differences in clinician and patient rated questionnaires have been similarly reported across a diversity of disorders such as major depression (38) and Parkinson’s disease symptoms (39).
When discrepancies were examined between the PDUQp and PDUQ, four items showed greater than 20% across subjects. Two of these items, regarding whether or not the patient’s family understands the patient’s use of pain medications (item 22) and helps to care for the patient due to their pain problem (item 23), may not have been interpreted by patients in the same manner as intended in the original PDUQ. Whereas the PDUQ items were phrased so that the interviewer could assess the degree to which family interactions sustained/facilitated the patient’s opioid use, the focus of the corresponding PDUQp items were related to more general family support. Alternatively, low concordance rates for the other two highly discrepant items, “Have you had to increase the amount of pain medications you take over the past 6 months?” (item 11) and “Do you think certain pain medications work better for you…” (item 16), may reflect increased willingness on the part of the patient to reveal these suggestive behaviors on a self report instrument as opposed to during clinician interview. Although it was not possible to test if changes to these items would improve the criterion validity of the PDUQp we have included in the appendix the PDUQp with suggested revisions to these items based on this analysis.
Medication Agreement Violation-Related Discontinuation of Treatment (MAVRD)
A recent consensus statement from the Initiative on Methods, Measurement and Pain Assessment in Clinical Trials (IMMPACT.org) recommended that a core outcome for clinical trials on the treatment of chronic pain be participant disposition, or the status of the subject at the conclusion of the trial, including “premature withdrawal from the study” (p.338, ref 40). Interestingly, a category of disposition that has received limited empirical attention is discontinuation due to clinician concerns about problematic medication use or addiction, a gap which has in part, been attributed to the relatively short duration of observation (≤ 8 weeks), and the tendency to exclude from participation subjects with a history of SUD (3, 4, 6, 9, 40–42).
This study is among the first to provide detailed analysis on discontinuation from opioid treatment related to violation of the medication agreement in general, as well as opioid-specific misuse behaviors specifically. As noted, approximately half of patients were still in treatment 12 months following enrollment, and MAVRD accounted for the largest number of discontinuations (38 or 28% of the sample). Further inspection of patient MAVRD records showed that 11% of the total sample had their opioids discontinued for opioid-specific misuse behaviors (i.e., independent increase of dosages, using opioids other than those prescribed). These data provide evidence that MAVRD reflects a wide range of medication use patterns, only one of which is may be opioid addiction. In other words up to 25% of MAVRD may be indicators of pseudoaddiction, diversion or problematic medication use.
Certain items on the baseline PDUQp were found to correspond more strongly with MAVRD and the opioid-specific use criterion than others. Several of these items, 8 (receiving pain medications from more than one clinic), 9 (thinking they might be addicted to pain medications, and 29 (having an alcohol or drug SUD diagnosis previously), were noted on the original PDUQ as having significant relationships with SUD status. This finding confirms consistency between the PDUQp and PDUQ regarding the detection of behaviors associated with treatment discontinuation, and emphasizes the relative importance of these in predicting treatment failures.
Analysis of the sensitivity and specificity results of the PDUQp indicate that a cut-off score of 10 provides optimal sensitivity and specificity results with regard to predicting MAVRD and opioid-specific misuse. Confirmation of this cut-off score was found within comparison of the mean PDUQp scores between problematic versus non-problematic opioid use, in which patients whose opioids were eventually discontinued (either due to general medication agreement violations or opioid-specific use) had scores of one to two points higher than those discontinued for other reasons. Improved sensitivity/specificity for the PDUQp was appreciated with the opioid-specific misuse criterion than for the more general MAVRD criterion, providing evidence that PDUQp score targets opioid-specific use behaviors specifically as opposed to more general medication agreement violations.
There were various limitations to this study. Importantly, data were collected at a single clinical site, and despite efforts to toward objectivity and consistency in arriving at MAVRD decisions, certain aspects of the decision-making process or culture are likely to be specific to the setting. In an effort to maximize the reliability and validity of the MAVRD measure, both study physicians and staff received specific instructions on how to code patient discontinuations, and as noted, all MAVRD decisions were made as a group by a multidisciplinary pain treatment team. Also, as with many studies evaluating opioid therapy for chronic non-malignant pain, patients diagnosed with current substance abuse or dependence (including opioid abuse/dependence) were excluded from study participation. Thus, little can be said about rates of opioid-specific use behaviors and PDUQp responses in pain patients who concurrently suffer SUD. Importantly, in that MAVRD reflects more than opioid addiction, the validity of the PDUQp to predict the latter has yet to be established.
The total sample size is small, and the subsample of interest (MAVRD patients), even smaller. Further, the sample was comprised of (primarily male) VA patients, who are more likely than the general patient population to suffer from SUD (43). Additional reliability, validity and psychometric data for both the PDUQ and PDUQp in larger and more diverse pain populations is needed to fully evaluate the utility of the questionnaire in predicting and identifying SUD in chronic pain patients on opioid therapy. Finally, the clinical utility of the PDUQp is likely to remain limited due to its length (31 items); future refinement of the tool to define a more efficient, as well as shorter, item set is needed to advance the field.
In conclusion, this study introduces a new patient-version of the Prescription Drug Use Questionnaire (PDUQp), which is moderately correlated to the original tool (PDUQ), and has good predictive validity for MAVRD within 12 months. The tool appears to have even greater sensitivity and specificity for predicting problematic opioid-specific use behaviors in particular, as opposed to other discontinuation criteria, although it does not support the diagnosis of SUD. Further, the data replicate the findings of the original PDUQ testing, showing that questionnaire items related to having multiple sources of medication supply, a personal history of drug or alcohol SUD, and thinking they might be addicted to pain medications, were highly predictive of discontinuation related to violation of the medication agreement (14).
The study also provides new data on relative frequency of behaviors leading to discontinuation of opioid treatment, and confirms that, at least for the sample studied, many of the discontinuations due to violations of the medication agreement are related to opioid-specific use. However, it is important to note that a proportion of patients with MAVRD did not show clear signs of substance abuse or dependence, but rather displayed behaviors that might better be labeled as treatment noncompliance and in a very few cases, possible drug diversion. These data reinforce the importance of careful delineation of the multiple treatment and follow-up categories when examining opioid discontinuation and the need for further development of valid and agreed upon measurement instruments for assessment of opioid abuse and dependence in patients with chronic pain as well as operational definitions of safe and effective opioid treatment.
Acknowledgments
This work was supported by VA Health Services Research and Development.
Appendix
Prescription Drug Use Questionnaire – Patient Version
| If you are currently taking any type of narcotic pain medication (such as Vicodin, Codeine, Percocet, Morphine, Darvon, etc.), please answer all the following questions. Circle either “Y” for a response of “Yes” or “N” for a response of “No” to each question. | |||
| 1. | Do you have more than one painful condition? | Y | N |
| 2. | Are you disabled by pain (unable to work or participate fully in activities)? | Y | N |
| 3. | Are you receiving any disability payments (such as SSI, or VA disability)? | Y | N |
| 4. | Do you have any current lawsuits or claims related to your pain problem? | Y | N |
| 5. | Have you tried any non-medication treatments for your pain problem (such as physical therapy, TENS, biofeedback) | Y | N |
| 6. | Has your pain been adequately treated over the past 6 months? | Y | N |
| 7. | Do you feel at all angry or mistrustful toward your previous doctors? | Y | N |
| 8. | Have you been given pain medications from more than one clinic over the past 6 months? | Y | N |
| 9. | Have you ever been or do you think you might currently be addicted to pain medications? | Y | N |
| 10. | Has a doctor ever told you that you were addicted to pain medications? | Y | N |
| 11. | Have you had to increase the amount of pain medications you take over the past 6 months? | Y | N |
| 12. | Have you had to call in for more pain medications because your prescription ran out? | Y | N |
| 13. | Have you used the pain medications to help other symptoms such as problems sleeping, anxiety, or depression? | Y | N |
| 14. | Do you save up unused medications in case you might need them in the future? | Y | N |
| 15. | Do you ever use alcohol to help relieve some of the pain? | Y | N |
| 16. | Do you think certain pain medications (such as vicodin, codeine, or percocet) work better for you and you prefer to take them and not others? | Y | N |
| 17. | Have you ever lost your pain medications and needed them replaced? | Y | N |
| 18. | Have you had to visit the emergency room in the past 6 months because of your pain problem? | Y | N |
| 19. | Have you ever had to buy pain medications on the street? | Y | N |
| 20. | Have doctors ever refused to give you the pain medications you felt you needed because of fear that you might abuse them? | Y | N |
| 21. | Is anyone in your family or among your friends concerned that you might be addicted to pain medications? | Y | N |
| 22. | Do any of your family members disagree with your use of pain medications? a | Y | N |
| 23. | Does anyone in your family help to take care of you due to your pain problem? b | Y | N |
| 24. | Does your spouse or significant other have problems with drugs or alcohol? | Y | N |
| 25. | Have those in your family or among your friends ever obtained pain medications for you? | Y | N |
| 26. | Have you ever borrowed pain medications from a friend or family member? | Y | N |
| 27. | Has anyone in your immediate family (father, mother, siblings) ever had a problem with drugs or alcohol? | Y | N |
| 28. | Has anyone in your immediate family (father, mother, siblings) ever had a problem with chronic pain? | Y | N |
| 29. | Have you ever had an alcohol or drug addiction problem? | Y | N |
| 30. | Have you ever been treated for an alcohol or drug abuse problem? | Y | N |
| 31. | Have you ever been taken partially or completely off pain medications to decrease your tolerance? | Y | N |
Recommended wording revision based on results.
Recommend removal of item in future questionnaire revisions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Portenoy RK, Foley KM. Chronic use of opiate analgesics in non-malignant pain: report of 38 cases. Pain. 1986;25:171–186. doi: 10.1016/0304-3959(86)90091-6. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg E, McNicol ED, Carr DB. Efficacy and safety of opiate agonists in the treatment of neuropathic pain of nonmalignant origin: systematic review and meta-analysis of randomized controlled trials. JAMA. 2005;293:3043–3052. doi: 10.1001/jama.293.24.3043. [DOI] [PubMed] [Google Scholar]
- 3.Rowbotham MC, Twilling L, Davies PS, et al. Oral opiate therapy for chronic peripheral and central neuropathic pain. N Engl J Med. 2003;348:1223–1232. doi: 10.1056/NEJMoa021420. [DOI] [PubMed] [Google Scholar]
- 4.Devulder J, Richarz U, Nataraja SH. Impact of long-term use of opiates on quality of life in patients with chronic, non-malignant pain. Curr Med Res Opin. 2005;21:1555–1568. doi: 10.1185/030079905X65321. [DOI] [PubMed] [Google Scholar]
- 5.Kalso E, Edwards JE, Moore RA, McQuay HJ. Opiates in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112:372–380. doi: 10.1016/j.pain.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Hermann M, Ruschitzka F. Coxibs, non-steroidal anti-inflammatory drugs and cardiovascular risk. Intern Med J. 2006;36:308–319. doi: 10.1111/j.1445-5994.2006.01056.x. [DOI] [PubMed] [Google Scholar]
- 7.Dasgupta N, Kramer ED, Zalman MA, et al. Association between non-medical and prescriptive usage of opiates. Drug Alcohol Depend. 2006;82:135–142. doi: 10.1016/j.drugalcdep.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 8.Eisenberg E, McNicol E, Carr DB. Opiates for neuropathic pain. Cochrane Database Syst Rev. 2006;3 doi: 10.1002/14651858.CD006146. CD006146. [DOI] [PubMed] [Google Scholar]
- 9.Martell BA, O'Connor PG, Kerns RD, et al. Systematic review: opiate treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. Task Force on DSM-IV. [Google Scholar]
- 11.Ballantyne JC, Mao J. Opiate therapy for chronic pain. N Engl J Med. 2003;349:1943–1953. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- 12.Ballantyne JC, La Forge KS. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007;129:235–255. doi: 10.1016/j.pain.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 13.Kirsh KL, Whitcomb LA, Donaghy k, Passik SD. Abuse and addiction issues in medically ill patients with pain: attempts at clarification of terms and empirical study. Clin J Pain. 2002;18:S52–S60. doi: 10.1097/00002508-200207001-00006. [DOI] [PubMed] [Google Scholar]
- 14.Compton P, Darakjian J, Miotto K. Screening for addiction in patients with chronic pain and "problematic" substance use: evaluation of a pilot assessment tool. J Pain Symptom Manage. 1998;16:355–363. doi: 10.1016/s0885-3924(98)00110-9. [DOI] [PubMed] [Google Scholar]
- 15.Dunbar SA, Katz NP. Chronic opiate therapy for nonmalignant pain in patients with a history of substance abuse: report of 20 cases. J Pain Symptom Manage. 1996;11:163–171. doi: 10.1016/0885-3924(95)00165-4. [DOI] [PubMed] [Google Scholar]
- 16.Weissman DE, Haddox JD. Opioid pseudoaddiction--an iatrogenic syndrome. Pain. 1989;36:363–366. doi: 10.1016/0304-3959(89)90097-3. [DOI] [PubMed] [Google Scholar]
- 17.Sees KL, Clark HW. Opioid use in the treatment of chronic pain: assessment of addiction. J Pain Symptom Manage. 1993;8(5):257–264. doi: 10.1016/0885-3924(93)90154-n. [DOI] [PubMed] [Google Scholar]
- 18.Adams LL, Gatchel RJ, Robinson RC, et al. Development of a self-report screening instrument for assessing potential opiate medication misuse in chronic pain patients. J Pain Symptom Manage. 2004;27:440–459. doi: 10.1016/j.jpainsymman.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 19.Butler SF, Budman SH, Fernandez K, Jamison RN. Validation of a screener and opiate assessment measure for patients with chronic pain. Pain. 2004;112:65–75. doi: 10.1016/j.pain.2004.07.026. [DOI] [PubMed] [Google Scholar]
- 20.Manchikanti L, Pampati V, Damron KS, McManus CD. Evaluation of variables in illicit drug use: does a controlled substance abuse screening tool identify illicit drug use? Pain Physician. 2004;7:71–75. [PubMed] [Google Scholar]
- 21.Butler SF, Budman SH, Fernandez KC, et al. Development and validation of the Current Opiate Misuse Measure. Pain. 2007;130:144–156. doi: 10.1016/j.pain.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu SM, Compton P, Bolus R, et al. The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opiate use in chronic pain. J Pain Symptom Manage. 2006;32:342–351. doi: 10.1016/j.jpainsymman.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 23.Burchman SL, Pagel PS. Implementation of a formal treatment agreement for outpatient management of chronic nonmalignant pain with opiate analgesics. J Pain Symptom Manage. 1995;10:556–563. doi: 10.1016/0885-3924(95)00085-d. [DOI] [PubMed] [Google Scholar]
- 24.Doleys DM, Rickman L. Other benefits of an opiate "agreement. ". J Pain Symptom Manage. 2003;25:402–403. doi: 10.1016/s0885-3924(03)00102-7. author reply 403–404. [DOI] [PubMed] [Google Scholar]
- 25.Fishman SM, Bandman TB, Edwards A, Borsook D. The opiate contract in the management of chronic pain. J Pain Symptom Manage. 1999;18:27–37. doi: 10.1016/s0885-3924(99)00035-4. [DOI] [PubMed] [Google Scholar]
- 26.Hariharan J, Lamb GC, Neuner JM. Long-term opiate contract use for chronic pain management in primary care practice. A five year experience. J Gen Intern Med. 2007;22:485–490. doi: 10.1007/s11606-006-0084-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katz NP, Adams EH, Benneyan JC, et al. Foundations of opiate risk management. Clin J Pain. 2007;23:103–118. doi: 10.1097/01.ajp.0000210953.86255.8f. [DOI] [PubMed] [Google Scholar]
- 28.Passik SD, Kirsh KL. Opiate therapy in patients with a history of substance abuse. CNS Drugs. 2004;18:13–25. doi: 10.2165/00023210-200418010-00002. [DOI] [PubMed] [Google Scholar]
- 29.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV, Axis I disorders, clinician version (SCID-CV) Washington, DC: American Psychiatric Press, Inc; 1996. [Google Scholar]
- 30.Carroll BT, Kathol RG, Noyes R, Jr, Wald TG, Clamon GH. Screening for depression and anxiety in cancer patients using the Hospital Anxiety and Depression Scale. Gen Hosp Psychiatry. 1993;15:69–74. doi: 10.1016/0163-8343(93)90099-a. [DOI] [PubMed] [Google Scholar]
- 31.Clarke DM, Smith GC, Herrman HE. A comparative study of screening instruments for mental disorders in general hospital patients. Int J Psychiatry Med. 1993;23:323–337. doi: 10.2190/J5HD-QPTQ-E47G-VJ0X. [DOI] [PubMed] [Google Scholar]
- 32.Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002;82:8–24. doi: 10.1093/ptj/82.1.8. [DOI] [PubMed] [Google Scholar]
- 33.Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 34.Kahan M, Srivastava A, Wilson L, Gourlay D, Midmer D. Misuse of and dependence on opiates: study of chronic pain patients. Can Fam Physician. 2006;52:1081–1087. [PMC free article] [PubMed] [Google Scholar]
- 35.Lusher J, Elander J, Bevan D, Telfer P, Burton B. Analgesic addiction and pseudoaddiction in painful chronic illness. Clin J Pain. 2006;22:316–324. doi: 10.1097/01.ajp.0000176360.94644.41. [DOI] [PubMed] [Google Scholar]
- 36.Savage SR. Assessment for addiction in pain-treatment settings. Clin J Pain. 2002;18:S28–S38. doi: 10.1097/00002508-200207001-00004. [DOI] [PubMed] [Google Scholar]
- 37.Consensus statement: definitions related to the use of opiates in the treatment of pain. Glenview, IL: AAPM/APS, and Chevy Chase, MD: ASAM; 2001. American Academy of Pain Medicine, American Pain Society, American Society of Addiction Medicine. [Google Scholar]
- 38.Zimmerman M, Coryell W, Wilson S, Corenthal C. Evaluation of symptoms of major depressive disorder. Self-report vs. clinician ratings. J Nerv Ment Dis. 1986;174:150–153. doi: 10.1097/00005053-198603000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Stacy M, Bowron A, Guttman M, et al. Identification of motor and nonmotor wearing-off in Parkinson's disease: comparison of a patient questionnaire versus a clinician assessment. Mov Disord. 2005;20:726–733. doi: 10.1002/mds.20383. [DOI] [PubMed] [Google Scholar]
- 40.Turk DC, Dworkin RH, Allen RR, et al. Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain. 2003;106:337–345. doi: 10.1016/j.pain.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 41.Roth SH, Fleischmann RM, Burch FX, et al. Around-the-clock, controlled-release oxycodone therapy for osteoarthritis-related pain: placebo-controlled trial and long-term evaluation. Arch Intern Med. 2000;160:853–860. doi: 10.1001/archinte.160.6.853. [DOI] [PubMed] [Google Scholar]
- 42.Watson CP, Babul N. Efficacy of oxycodone in neuropathic pain: a randomized trial in postherpetic neuralgia. Neurology. 1998;50:1837–1841. doi: 10.1212/wnl.50.6.1837. [DOI] [PubMed] [Google Scholar]
- 43.Leslie DL, Rosenheck RA. Inpatient treatment of comorbid psychiatric and substance abuse disorders: comparison of public sector and privately uninsured populations. Adm Policy Ment Health. 1999;26:253–268. doi: 10.1023/a:1022269926310. [DOI] [PubMed] [Google Scholar]