Abstract
This study used latent class analysis to examine distinctive subtypes of Ecstasy users based on 24 abuse and dependence symptoms underlying standard DSM-IV criteria. Data came from a three-site, population-based, epidemiological study to examine diagnostic nosology for Ecstasy use. Subject inclusion criteria included lifetime Ecstasy use exceeding five times and once in the past year, with participants ranging in age between 16 to 47 years of age from St. Louis, Miami, U.S. and Sydney, Australia. A satisfactory model typified four latent classes representing clearly differentiated diagnostic clusters including: (1) A group of sub-threshold users endorsing few abuse and dependence symptom (negatives), (2) A group of ‘diagnostic orphans’ who had characteristic features of dependence for a select group of symptoms (mild dependent), (3) a ‘transitional group’ mimicking the orphans with regard to their profile of dependence also but reporting some abuse symptoms (moderate dependent), and (4) a ‘severe dependent’ group with a distinct profile of abuse and dependence symptoms. A multinomial logistic regression model indicated that certain latent classes showed unique associations with external non-diagnostic markers. Controlling for demographic characteristics and lifetime quantity of Ecstasy pill use, criminal behavior and motivational cues for Ecstasy use were the most efficient predictors of cluster membership. This study reinforces the heuristic utility of DSM-IV criteria applied to Ecstasy but with a different collage of symptoms that produced four distinct classes of Ecstasy users.
Keywords: Ecstasy, substance use disorders, abuse, dependence, latent class analysis
1. Introduction
Ecstasy (also called MDMA or 3,4-methylenedioxymethamphetamine) is one of several ‘party drugs’ (others being Rohypnol, GHB [γ-hydroxybutyrate], and Ketamine) receiving increasing recognition as a drug of abuse (Gold and McKewen, 1995; Winstock, et al., 2001; Yacoubian, 2002; Yacoubian et al., 2004). Ecstasy’s attraction is its ability to provide heightened sensory awareness and euphoric sensations of well-being, intense pleasure, and enhanced interpersonal closeness (Cohen, 1998; Davison and Parrot, 1997; Parrott and Lasky, 1998; Vollenweider et al., 1998). Media reports glamorize Ecstasy as the new age psychedelic for the ‘X’ generation (Cohen, 1998; Walsh, 2004) with some treatment experts suggesting it has therapeutic uses (Greer, 1985; Greer and Tolbert, 1990; Strassman, 1995). Ecstasy first surfaced as part of the drug subculture in the early 1980s with various epidemiological indicators showing its use spread quickly throughout Western Europe, Scandanavia, the United Kingdom (Kokkevi et al., 2002; Pederson and Skrondal, 1999; von Sydow et al., 2002; Winstock et al., 2001), North America (Adlaf and Smart, 1997), even reaching as far as Australia (Topp et al, 1999). The introduction of this mind-altering drug from the British Acid House scene spawned a resurgence of the psychedelic drug culture replete with rhythmic beating electronic music, laser light displays, and marathon all night dance parties held at secretive venues called “raves” (Lenton et al., 1997; Lyttle and Montagne, 1992; Schwartz and Miller, 1997; Weir, 2000).
Eventually, use of Ecstasy migrated to the U.S. where street ethnographic information shows the drug appeared sometime in the late 1980s, The first real signal of a growing problem came when an epidemic of Ecstasy use peaked in 2001 marked by 1.8 million new users (SAMHSA, 2007). According to the most recent prevalence data obtained from the National Household Survey of Drug Use and Health (NSDUH), the effect of the epidemic has not been unequivocal across different age groups. For example, among youth ages 12–17, lifetime rates of Ecstasy use (not including MDMA and other club drugs) declined from 3.4% in 2002 to 1.9% in 2006. Peak rates of lifetime Ecstasy use also appeared in 2002 with 15% of young adults 18–25 years of age reporting some use and this rate steadily declined to 13.4% in 2006. Among those ages 26 to 34 however, the rate of Ecstasy use has actually increased in this same time span going from 6% in 2001 (the supposed “peak” of the epidemic) to 11.8% most recently in 2006.
Trends among experienced drug users and those who report having used hallucinogens or other club drugs also reinforces that consumption of Ecstasy may not have abated (SAMHSA, 2007). Data for the youngest age group (12–17) show that 50% of experienced drug users reported using Ecstasy in 2001, and by 2006 this had dropped 42.2%. However, the apparent decline in use did not affect individuals who were between 18–25 years of age, where consumption actually increased, going from 59.2% in 2001 to 66.4% in 2006. Again, given the age of onset for Ecstasy use nationally is 20.6, it would appear that the drug is “gaining” attraction among young adults at greatest risk for onset and continued use. The remaining age groups monitored in the NSDUH reinforce this trend (ages 26 to 34 and 35 and older); a greater preponderance of experienced drug users reported having tried Ecstasy in 2006 compared to 2001, which was the height of the Ecstasy epidemicξ.
The gain in Ecstasy’s popularity is corroborated by reports that youth are more willing to use Ecstasy than cocaine, heroin, or LSD, and perceive less harm associated with using Ecstasy compared to other illicit drugs (Gamma et al., 2005; Kalant, 2001). Despite its popularity, evidence is accumulating that both frequent (Parrott, 2004; Parrott et al., 2002; Parrott and Lasky, 1998) and recreational use of Ecstasy (Bhattachary and Powell, 2001; Davison and Parrott, 1997; Gouzoulis-Mayfrank et al., 2000) can induce a range of negative consequences. Studies show that frequent and heavy Ecstasy use are responsible for neurodegenerative symptoms including Parkinson-like tremors, neurological deficits, and impaired cognitive functioning (Cole and Sumnall, 2003; Gerra et al., 2000; Krystal and Price, 1992; Morgan et al., 2002; Parrott et al., 1998; Rodgers, 2000; Roiser and Sahakian, 2004).
Additional evidence points toward elevated levels of depression among former users (MacInnes et al., 2001) and a litany of psychological and physical problems including sleep disorders, hyperthermia, weight loss, anxiety, and mood fluctuations (Curran and Travill, 1997; Parrott et al., 2002). Several studies indicate that neuropsychological deficits do not abate with prolonged abstinence (Bolla et al., 1998; Morgan et al., 2002) even among recreational users (Gouzoulis-Mayfrank et al., 2000; Morgan, 1999). Both laboratory and clinical investigations increasingly point to selective serotonin (5-HT2) neurotoxicity with corollary deficits in neurotransmission Battaglia et al., 1988; Gerra et al., 2000; Gerra et al., 1998; Kish, 2002; McCann et al., 1994; Parrott, 2002) suggesting that chronic use leads to irreversible brain damage (Beck, 1990; Merrill, 1996).
The search for a reliable and effective diagnostic classification system, which has considerable implications for communicating consequences and designing treatments are fueled collectively by both clinical evidence and epidemiological studies suggesting that more than one type of Ecstasy user exists (Carlson et al., 2005; McGuire et al., 1994; Parrott et al., 2002). In fact, evidence suggests that infrequent or “recreational” users are categorically different from heavy users in terms of drug-related consequences and impairment. The apparent differences and variability in patterns of drug consumption coupled with differences in reporting of symptoms and negative consequences from Ecstasy use necessitate further analysis of whether clinical features of consumption fit the typologies of abuse and dependence. Prior to elaborating a quantified model of Ecstasy user subtypes, we briefly explore a few of the cardinal issues tied to diagnostic nosology, many of which have been addressed previously by studies of alcohol and other substance abuse.
1.1. Conceptual Framework for Testing Validity of Diagnostic Criteria
Studies of the logical coherence of diagnostic criteria have been conducted for a wide range of substances including alcohol (Chick, 1980; Davidson et al., 1989; Edwards and Gross, 1976), cocaine (Bryant et al., 1991), and other drugs (Kosten et al., 1987). These studies share in common the identification of a set of criteria that help distinguish individuals on the basis of their behavioral, physiological, and cognitive responses to drug use. With the publication of Diagnostic and Statistical Manual of Mental Disorders, third edition (American Psychological Association, 1980), the machinery was set into motion to separate the universe of symptoms underlying alcoholism into those characterizing abuse from those indicating dependence (Cottler et al., 1995). Consistently, dual categorization schemes utilize exploratory factor analysis in an effort to boil down a large set of symptoms into more manageable and clinically meaningful criteria (Basu et al., 2004; Harford and Muthén, 2001; Muthén et al., 1993). Because there has not been a conclusive body of evidence supporting a clear and unequivocal representation of abuse and dependence criteria across a wide range of substances, researchers have begun to question whether abuse/dependence have distinct clinical profiles (Rounsaville et al., 1986).
Diagnostic classification of Ecstasy users is relatively new with only a handful of recent studies (Cottler et al., 2001; Jansen, 1998; Topp et al., 1999; von Sydow et al., 2002; Winstock et al., 2001; Yacoubian et al., 2004). While this body of work has helped to advance our understanding of the prevalence and patterns of Ecstasy use, abuse and dependency, a number of unresolved methodological and conceptual issues remain. Methodologically speaking, and with few exceptions (Cottler et al., 2001; Topp et al., 2004; Winstock et al., 2001), most of the studies cited are seriously underpowered, relying on either small ethnographic samples, using selected samples obtained through irregular data collection following attendance at raves, through snowballing techniques, or survey information obtained from music stations and dance magazines (Lenton et al., 1997; Petrides and Sherlock, 1996; Yacoubian et al., 2004; Winstock et al., 2001). Conceptually, previous studies still leave unresolved the question of fit between diagnostic classification and the full range of symptoms resulting from Ecstasy use. For instance, based on their sporadic or infrequent use of Ecstasy (used primarily on weekends), users may only intermittently report adverse social or physiological consequences including but not limited to dry mouth (sicca), bruxism (jaw clenching), hyperthermia, and agitation (Parrott et al., 2002; Topp et al., 1999; Yacoubian et al., 2004). As a result of their inconsistent patterns of use, it may be hard to obtain homogeneous groups of users that comport with discrete clusters of symptoms such as abuse and dependence.
Related to this, most studies have relied on abbreviated versions of DSM-IV criteria eliminating any potential to learn more about the full breadth of symptom classification and diagnostic utility of abuse and dependence. In DSM-IV, Ecstasy is lumped together with hallucinogenic compounds. As a result, most studies do not specifically assess for consequences of this drug separate from other drugs. Finally, none of the studies reported has examined the subtypes of Ecstasy users based on DSM-IV symptoms or criteria. In this respect, the field could benefit from a nosological study of culturally diverse samples of casual and heavy Ecstasy users with attention to a large number of symptoms, and implementation of appropriate statistical analysis to determine whether the abuse/dependence dichotomy fits the sample data. This is especially significant during the prelude phase of the DSM-V effort.
1.2. Goals of the Present Study
A primary aim of this study was to obtain a more refined picture of the different subtypes of Ecstasy users based on three geographically diverse general population samples using identical classification methods. Latent class analysis (LCA) was used to model clusters or discrete groups of users based on their observed response profiles to symptoms that are clinical features representing the core criterion for abuse and dependence. As we describe in more detail later, LCA is unique statistical approach that allows us to derive distinct and meaningful subgroups based on unobserved heterogeneity in a population and the similarity in their response profiles. A wide range of studies have now used this approach to explore subtypes based on consumption patterns (Collins et al., 1994; Pedersen and Skrondal, 1999; Uebersax, 1994), symptom data (Crum et al., 2005; Grant et al., 2005; Reboussin and Anthony, 2006), and underlying mental health problems including antisocial personality (Bucholz et al., 2000).
In the development of our instrumentation, we augmented considerably the clinical indicators of abuse and dependence by adding experiences that would capture specific consequences from Ecstasy consumption. In our search for mutually exclusive subtypes of Ecstasy users, we hypothesized a priori four latent classes; one comprised of novice or sub-threshold Ecstasy users for whom patterns of use have not resulted in extensive symptom reporting; a second group, called diagnostic orphans, who report some dependency symptoms; a third, transition group mimicking the orphans but reporting some abuse symptoms as well; and a fourth, severe-dependent group with a distinct profile of symptom reporting fitting well with a DSM characterization of dependency.
A second aim involved testing the association between different non-diagnostic risk measures and the different Ecstasy subtypes using multinomial logistic regression. These models estimated a slope for the individual latent classes and determined whether the slopes differed significantly based on an optimal set of explanatory marker variables. The regression models also controlled for involvement in other drugs. This statistical control is essential because Ecstasy users are known to frequently engage in multiple drug use, thus making it imperative that we rule out that symptom reporting was attributed solely to their other drug involvement (Hammersley et al., 1999; Parrott et al., 2000; Schifano et al., 1998; Strote et al., 2002; Topp et al., 1999).
2. Methods
2.1. Study Protocols
Data were obtained from a National Institute on Drug Abuse-funded multi-site epidemiological study designed to ascertain the utility of DSM-IV diagnostic criteria for club drugs (i.e., Ecstasy, Ketamine, GHB, and Rohypnol) as well as the reliability and validity of the assessment. The study was conducted in Miami, Florida and St. Louis, Missouri between 2002 and 2004 with additional data collection taking place in Sydney, Australia from 2003 to 2005. A total of 46% (N=297) of the participants were from the St. Louis site, 29% from Miami (N=186), and 24% from Sydney (N=156). All three sites received the same instruction protocol, utilized the same assessment strategies, and relied on identical subject recruitment procedures, which included internet postings, advertisements in college and local newspapers, flyers posted in areas frequented by young people, and distribution at pubs, bars and dance clubs; a heterogeneous sample of Ecstasy users was targeted.
Eligibility requirements included self-reported lifetime Ecstasy use exceeding five times and at least once in the past 12 months. This selection threshold has been part of many large-scale epidemiological studies (Anthony and Helzer, 1991; Cottler et al., 1995) and recognized as a gold standard for designating cumulative lifetime consumption (von Sydow et al., 2002). Following telephone screens to determine study eligibility, participants 16 to 47 years of age were invited to be interviewed (Sydney participants were older than 18). The Washington University Risk Behavior Assessment for Club Drugs (RBA-CD) and the Center for Epidemiological Studies – Depression Scale (CES-D) were used. Revisions to the well standardized Composite International Diagnostic Interview Substance Abuse Module (CIDI-SAM: Cottler and Keating, 1990) and RBA (National Institute on Drug Abuse, 1993) resulted from focus groups conducted at the three sites probing club drug use and consumption patterns, specific withdrawal symptoms, physical and psychological problems. These changes resulted in the Substance Abuse Module for Club Drugs (SAM-CD) and were formatively used in developing the RBA-CD. The assessment procedure took approximately two hours and subjects received monetary compensation for their participation. All consent and human subject procedures received Institutional Review Board (IRB) approval at the respective institutions. For the present analyses only the test (or time 1) data were used yielding a final sample size of N=639.
2.2. Analysis strategy
Latent class analysis is a type of mixture modeling that uses categorical data to find homogeneous subgroups or “classes” based on observed response profiles. In the case of categorical symptom data provided by DSM type assessments, a respondent can answer either “yes” or “no” but not both to record presence or absence of a symptom. The proportional response profiles generated by a cross-classified table of different responses are then used to generate class-specific response probabilities, given membership in a designated ‘unobserved’ latent class (Sullivan et al., 1998). The general framework of LCA is likened to a multidimensional contingency table modeling probabilities of cell frequencies corresponding to qualitatively different classes or subgroups (Clogg, 1995; Goodman, 1974; McCutcheon, 1987). Just like optimal regression coefficients or factor loadings, estimated probabilities associated with membership in a particular latent class indicate the ‘strength of the relationship’ between the manifest indicator (i.e., symptom) and the latent class. In other words, membership in a particular latent status determines statistically the probability of endorsing a particular item or set of items (the items or dependent variables are called latent class indicators).
2.3. Symptom Measures
In the present study, a total of 24 lifetime symptom questions representing the hallmark DSM criteria, including eight abuse criteria: (1) resulting in failure to fulfill major role obligations (e.g., “Did your use of Ecstasy interfere with your responsibilities at home, at work, or at school?”), (2) use in situations when it is physically hazardous (e.g., “Have there been times when you were under the influence of Ecstasy when you could have gotten yourself or others hurt, or put yourself or others at risk”), (3) use resulting in substance-related legal problems, and (4) use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effect of Ecstasy. Social and interpersonal problems were further broken down into individual symptoms tapping problems with family, friends, people at work or school, and physical fights when using Ecstasy. A general item assessed continued use despite recognizing that Ecstasy was causing one or more of the social or interpersonal problems†.
Individual symptoms that comprised the seven dependence criteria included: (1) tolerance (“Did you ever find that the same amount of Ecstasy had much less effect on you than it once did; or did you find you ever had to use more Ecstasy to get the same effect?”), (2a) withdrawal (“During the first few hours or days of not using Ecstasy did you ever …”) consisting of 19 withdrawal symptoms that were bundled into six items tapping behavioral symptoms (e.g., “feel tired, sleepy, or weak”), nine items tapping somatic symptoms (e.g., “have runny eyes or nose”), and four items tapping neurological symptoms (e.g., “have vivid, unpleasant dreams”: a positive [yes] for any one of the symptoms in the scale registered a “1” for the entire scale), (2b) withdrawal avoidance (e.g., “did you ever use Ecstasy to avoid or get rid of any of those so-called withdrawal symptoms?”), (3) increased use of larger amounts of Ecstasy over a longer period of time than intended (e.g., “Have you often used more Ecstasy than you intended or kept using Ecstasy for a longer period of time than you intended?”), (4) persistent desire or unsuccessful efforts to cut down or control Ecstasy use (e.g., “Has there ever been a period of time when you wanted to quit or cut down on Ecstasy or tried to quit or cut down but were unable to for at least a month?”), (5) great deal of time spent in activities to obtain substance, use substance, or recover from its effects (i.e., “Has there ever been a period when you spent a lot of time using Ecstasy, planning how you would get Ecstasy, or recovering from its effects?”), (6) giving up or reducing important social, occupational or recreational activities because of substance use (i.e., “Did you ever give up or reduce any important activities to get or use Ecstasy, like getting together with friends or relatives, going to work or school, participating in sports or anything else?”), (7) use caused physical health problems (“Did using Ecstasy cause you any physical health problems like …”), and continued use despite knowledge of persistent or recurrent physical health problems caused or exacerbated by the substance (e.g., “Did you continue to use Ecstasy after you realized it was causing any of these physical health problems?”). The physical health problems for this paper were coded as three symptom indices with 13 items tapping somatic events, seven items assessing neurological events, and three items tapping problems of a non-specific nature. Respondents who acknowledge any one of these features received a “1” for the symptom scale. Another symptom cluster assessed emotional or psychological problems from Ecstasy use (“Did using Ecstasy cause you to have any emotional or psychological problems like …”), with the 13 symptoms clustered into seven items tapping neurological and mood-related events and six items assessing behavioral events. A follow-up yes/no question assessed whether respondents continued their use despite emotional or psychological problems (“Did you continue to use Ecstasy after you realized it was causing any of these emotional or psychological problems?”).
2.4. Construction of External Marker Variables
Four non-diagnostic domains of psychosocial risk including patterns of Ecstasy use, other substance use, criminal behavior, and psychological functioning were included to obtain a more refined picture of factors influencing class membership. A composite index of criminal behavior included five items assessing number of times having been arrested and then charged with an offense ( “0” for no arrests, “1” for only one arrest, “2” for two to five arrests, and “3” over five arrests), age at first arrest (coded “0” for never, “1” greater than 20 years of age, and “2” for less than 20 years of age), age at the last time of arrest (“0” for no arrests, “1” for more than 1 year ago and “2” for within the past year), nights spent in jail (coded “0” for no nights spent in jail, “1” for one to five nights, and “2” for six or more nights) and ever having a drug-related arrest (coded “0” for never arrested, “1” for arrested but not for drugs, and “2” for drug-related arrest). The criminal behavior index was then summed over the individual items (α=.95).
Measures of depression, contextual motivations for drug use, stressful life events, and social support were used as proxies for psychological functioning. The 20-item CES-D (Radloff, 1977) is a useful screening measure for current depressive symptoms including items assessing sleep disturbance (e.g., “my sleep was restless”), affective mood (e.g., “I had crying spells”), feelings of worthlessness (e.g., “I thought my life had been a failure”), loss of appetite (“I did not feel like eating; my appetite was poor”), and psychomotor retardation (“I could not get going”). Response categories were scaled from ‘rarely or none of the time’ (0) through ‘most or all of the time’ (3). The resulting highly skewed distributions for the individual questions necessitated reordering so that scores of “2” and “3” were set to “1” and all other scores coded “0.” A depression risk index was then formed (α=.86). An additive index of contextual factors and motivation for Ecstasy use (α=.74) assessed the different people to get Ecstasy from including “spouse, family member, roommate, stranger, and dealer;” different places to use Ecstasy with dichotomously coded responses including “raves, clubs, bars, and fraternities,” to name a few; people to use or share Ecstasy with including “spouse, friends, roommates, dealer, and others;” and various motives for using Ecstasy including “stress relief, bonding, pressure, spiritual experience, and curiosity.”
A measure of stressful life events included eight items assessing standard adverse (e.g., “mugged, beaten up, or stabbed”) and positive (e.g., “gotten married or entered into a new relationship”) events along with ratings of severity (e.g., “Was that stressful for you?”) that led to creation of a unit-weighted life events severity scale (α=.46). A six-item measure (α=.54) assessed social and instrumental support (e.g., “there is a person you can count on for understanding and advice”) with response formats coded ‘Disagree’ (0) and ‘Agree’ (1).
2.5. Quantity, Frequency Measures of Ecstasy
Patterns of Ecstasy use were elicited through number of pills used lifetime (“If you were to add up all of the Ecstasy pills you have used since you first started using Ecstasy, about how many pills would that be?”). Using a scheme proposed by Scholey et al. (2004), we then recoded the response categories into experimental (0–9 pills), moderate (10–99), and heavy use (100+pills). Past 30-day use included extent of involvement (“how many days did you use Ecstasy in the past 30 days?”), and frequency of use over the same period (“During these days [when you used], how many times a day did you usually use Ecstasy or MDMA?”). Number of times per day was recoded so that individuals reporting more than three pills per day were coded “4” and the interval categories below this remained intact.
2.6. Sociodemographic Measures and Other Illicit Drug Use
Covariates modeled in the latent class analyses included gender (referent category male), race (referent category White), age (referent category young [under 21]) and education (referent category less than high school). A continuous measure of multiple drug involvement (consisting of alcohol, marijuana, cocaine, heroin, stimulants, sedatives, inhalants, other club drugs [Ketamine, GHB, Rohypnol], hallucinogens, anabolic steroids) was assessed by summing across all other drugs used in the past 12 month period with the same inclusion criteria as used for Ecstasy users (5 or more times lifetime).
3. Results
3.1. Sample Description
Overall, the mean age of the sample was 23 years (SD = 5.21); 42% were female, 62% white, and 45% under 21 years of age; nearly all reported never being married (93%); 88% were high school graduates. Proportional tests indicated a few site differences in demographics including more Hispanic and fewer White participants in Miami, χ2(4) = 252.41, p ≤ .0001, and more single participants in Sydney, χ2(2) = 9.76, p ≤ .01. Table 1 shows the symptom prevalence rates for male and female participants and for the three sites (for clarity the same proportional tests for race, education, and marital status are not shown but can be obtained from the first author). Among the noted gender differences, males were more likely than females to report withdrawal-related behavioral symptoms, χ2(1) = 5.71, p ≤ .05, to use Ecstasy in larger amounts or over a longer period than was intended, χ2(1) = 5.30, p ≤ .05, report a persistent desire or unsuccessful effort to cut down, χ2(1) = 4.32, p ≤ .05, give up social, occupational, or recreational activities, χ2(1) = 4.32, p ≤ .05, and continue using Ecstasy even in the face of continued emotional or psychological problems, χ2(1) = 6.15, p ≤ .05.
Table 1.
Lifetime Symptoms by Gender and Site
| Total | |||||||
|---|---|---|---|---|---|---|---|
| Symptom | F (N=268) |
M (N=371) |
P-value | St. Louis (N=297) |
Miami (N=186) |
Sydney (N=156) |
P-value |
| Major role obligations | 31.0 | 22.0 | .010 | 20.9 | 23.7 | 37.8 | <.001 |
| Physically hazardous | 51.7 | 50.5 | NS | 49.8 | 51.1 | 53.2 | NS |
| Legal problems | 3.0 | 5.7 | NS | 3.4 | 7.0 | 3.9 | NS |
| Problems with family | 24.4 | 20.1 | NS | 16.5 | 24.2 | 29.5 | .004 |
| Problems with friends | 19.9 | 15.5 | NS | 15.8 | 19.4 | 18.0 | NS |
| Problems at school/work | 12.6 | 10.9 | NS | 8.8 | 11.3 | 17.3 | .026 |
| Fights from ecstasy use | 3.0 | 2.2 | NS | 3.0 | 1.6 | 2.6 | NS |
| Continued use despite probs. | 31.4 | 27.2 | NS | 25.9 | 30.7 | 32.7 | NS |
| Tolerance | 51.3 | 48.6 | NS | 43.1 | 56.5 | 54.5 | .007 |
| Withdrawal – Behavioral | 85.2 | 77.7a | .017 | 77.4 | 80.7 | 87.8 | .028 |
| Withdrawal – Somatic | 52.0 | 53.8 | NS | 48.5 | 55.4 | 59.0 | NS |
| Withdrawal – Neurological | 57.2 | 49.7 | NS | 51.2 | 56.5 | 51.9 | NS |
| Withdrawal – Avoidance | 16.6 | 12.5 | NS | 12.5 | 16.7 | 14.8 | NS |
| Use more XTC than intended | 48.0 | 38.9 | .021 | 37.4 | 47.9 | 46.8 | .038 |
| Persistent desire quit cut down | 20.7 | 14.4 | .038 | 14.1 | 18.3 | 21.2 | NS |
| Time spent acquiring, using, recovering from XTC use | 56.1 | 55.2 | NS | 48.2 | 62.4 | 61.5 | .002 |
| Give up social, recreational occupational activities | 29.5 | 22.3 | .038 | 20.1 | 24.7 | 34.6 | .006 |
| Physical health problems – somatic | 87.5 | 85.1 | .387 | 84.2 | 89.3 | 85.9 | NS |
| Physical health problems –neurological | 62.0 | 59.8 | .572 | 58.6 | 57.5 | 68.6 | NS |
| Physical health problems –non specific | 30.6 | 26.4 | NS | 20.9 | 28.5 | 41.7 | <.001 |
| Continued use w physical health problems | 80.1 | 78.3 | NS | 76.8 | 81.2 | 80.8 | NS |
| Emotional psych problems –Mood change | 78.6 | 75.8 | NS | 74.4 | 79.0 | 79.5 | NS |
| Emotional psych problems –thought disturbance | 75.7 | 74.7 | NS | 72.4 | 82.8 | 71.2 | .015 |
| Continued use even with emotional psych problems | 83.4 | 75.3 | .013 | 76.1 | 83.9 | 77.6 | NS |
Note. All of the comparison tests based on χ2 proportional test statistic.
Users at the Sydney site were more likely to report recurrent use resulting in the failure to fulfill major role obligations, χ2(2) = 15.97, p ≤ .001, problems with family, χ2(2) = 10.88, p ≤ .01, people at work or school, χ2(2) = 7.33, p ≤ .05, withdrawal-related behavioral symptoms, χ2(2) = 7.14, p ≤ .05, giving up social, occupational, or recreational activities because of their Ecstasy use, χ2(2) = 10.25, p ≤ .01, and more non-specific physical health problems associated with their Ecstasy use, χ2(2) = 21.86, p ≤ .0001. Users from Miami were more likely to report tolerance, χ2(2) = 9.99, p ≤ .01 a great deal of time acquiring, using or recovering from the effects of Ecstasy, χ2(2) = 12.35, p ≤ .01, and emotional or psychological problems related to thought disturbance, χ2(2) = 8.36, p ≤ .05. St. Louis users reported a lower rate of using more Ecstasy than intended, χ2(2) = 6.53, p ≤ .05. Overall, there were no consistent differences in symptom reporting evident from site to site resulting in a fairly homogeneous sample. The few observed statistical differences by way of proportional analyses did not highlight any systematic bias in the sample recruitment procedures.
Table 2 shows the results of analysis of variance for the continuous measures of psychological functioning, criminal behavior, Ecstasy, and other drug use controlling for site, and gender (we also tested interaction terms). As shown, there was some marked site differences in the measures of psychosocial functioning including criminal behavior, depression, and motivation for drug use. There was also site differences in consumption patterns for Ecstasy (lifetime, days used, and number of times per day), as well as other drug use (other club drugs, other drugs without club drugs, and other drugs without Ecstasy). Only one of the interactions was significant (p ≤ .010) involving stressful life events. Post-hoc follow-up analyses indicated that females from St. Louis and males from Miami reported significantly higher stressful life events.
Table 2.
Mean Comparisons for External Marker Variables
| Composite Scales |
Total Sample |
Female (N=271) |
Male (N=368) |
P-Value Gender |
Miami (N=186) |
St. Louis (N=297) |
Sydney (N=156) |
P-Value Site |
|---|---|---|---|---|---|---|---|---|
| Criminal Index | 2.99 | 1.39 | 3.80 | <.001 | 2.88a | 3.51a | 1.39 | <.001 |
| CES-D | 6.22 | 6.27d | 6.05d | NS | 6.53a | 6.47a | 5.47 | <.001 |
| Motivation | 15.99 | 15.91d | 16.36d | NS | 16.72a | 15.14 | 16.55a | <.001 |
| Stressful Life Events | 1.57 | 1.58d | 1.52d | NS | 1.61 | 1.65 | 1.38 | NS |
| Support | 4.01 | 4.10 | 3.93 | .014 | 4.08 | 4.03 | 3.95 | NS |
| Lifetime XTC Use | 2.30 | 2.30d | 2.36d | NS | 2.36a | 2.18 | 2.44a | <.001 |
| # Days Used Past 30 Days | 0.48 | 0.55d | 0.51d | NS | 0.32a | 0.34a | 0.94 | <.001 |
| # Times/Days Past 30 Days | 0.70 | 0.80d | 0.79d | NS | 0.51a | 0.43a | 1.44 | <.001 |
| # Other Club Drugs Used¥ Past 12 mos. | 0.27 | 0.29 | 0.44 | .006 | 0.44a | 0.24 | 0.42a | <.001 |
| # of Other Drugs Used (no club drugs) Past 12 mos. | 3.93 | 3.68 | 4.00 | .017 | 3.95a | 4.07a | 3.52 | .003 |
| # of Other Drugs Used (no XTC) | 4.28 | 3.98 | 4.44 | .004 | 4.39a | 4.30a | 3.94 | NS |
Note. XTC = Ecstasy. Least square (adjusted) means are reported for subgroup comparisons.
Mean comparisons by site.
Mean comparisons by gender. P-Values for Site comparisons are based on Ftest statistics. P-Values for Gender comparisons are based on Student’s t-test. Means in the same row that do not share superscripts differ significantly in Scheffe post hoc analysis. In some cases, overall F-test may not be significant and post hoc comparisons are presented for purposes of clarity. NS = not significant.
3.2. Patterns of Ecstasy and Other Drug Use
Mean lifetime Ecstasy use was 227 pills (SD = 544.3), ranging from 5 to over 5000 pills and the modal number of pills taken was 30. As a group, mean age for first time using Ecstasy was 19 and mean age of most recent use was 23 years of age. Among those reporting Ecstasy use in the past 30 days, the modal number of times they took a pill was once per day (24%). Modal number of years using Ecstasy was between three and four and the modal number of pills used was between 10 and 99 (52%). Twenty-seven percent reported using other club drugs in the past 12-months (Ketamine, GHB, or Rohypnol), while almost all (97%) reported a history of using other drugs. Specifically, 99% reported lifetime alcohol use (there were no significant site or gender differences).
Sites varied slightly in consumption patterns and a few other non-diagnostic measures. Participants from Sydney were more likely to have used in the past 30 days, χ2(2) = 114.37, p ≤ .0001 (46% vs. 21% and 30% from Miami and St. Louis, respectively), but did not differ significantly in the number of days used in this same time frame. Sydney participants also reported significantly more numbers of times they used per day in the past 30 days compared to St. Louis, but not more than Miami, F(2, 268) = 4.82, p ≤ .01 (1.83 pills versus 1.72 and 1.43, for Miami and St. Louis, respectively).
Sites differed somewhat with regard to non-diagnostic measures including cultural factors that may account for consumption patterns. Participants from St. Louis (49%) were more likely to live apart from their biological father before age 15 compared to Miami (34%) and Sydney (17%), χ2(2) = 18.86, p ≤ .0001. There were no significant site differences in parent-child communication patterns, parental monitoring, or frequency of discussing sex when participants were adolescents. Participants from St. Louis were more likely to report their parents searched them for drugs, χ2(2) = 10.40, p ≤ .01, (47% vs. 34%, and 18%, for Miami and Sydney, respectively) and tested them for drugs, χ2(2) = 22.94, p ≤ .0001 (50% vs. 44% and 6%, respectively). The St. Louis participants also reported their parents were more likely to disapprove of drug use, χ2(2) = 33.32, p ≤ .0001 (47% vs. 30%, and 22%, respectively). Sites did not differ significantly in the number of raves attended (sample average was 36 lifetime) or the mean age when participants attended a rave (means for all three sites hovered around age 21).
We also examined family composition, religious attendance, and other measures that give some insight into possible cultural differences across the sites. More St. Louis participants reported never being married, χ2(4) = 10.34, p ≤ .05 (45.6% vs. 28.5%, and 25.8% for Miami and Sydney, respectively) but the same participants were more likely to have children, χ2(2) = 15.46, p ≤ .001 (68% vs. 22% and 9.4%, respectively). St. Louis participants also were more likely to have been arrested, χ2(2) = 24.07, p ≤ .0001 (54% vs. 31% and 14.5%, respectively) and to have been in alcohol or drug treatment, χ2(2) = 18.65, p ≤ .0001 (58% vs. 33% and 9%, respectively). Participants from St. Louis were more likely to value religious participation, χ2(4) = 28.11, p ≤ .0001 (57% vs. 25%, and 13%, respectively).
3.3. Results of LCA
Derivation of the different classes proceeded sequentially from the most parsimonious one-class model (Ecstasy users are all the same with regard to their patterns of reporting specific experiences resulting from their Ecstasy use) to a more differentiated seven-class model. Fit statistics for each model are contained in Table 3 with models adjusted for the demographic control variables. The likelihood ratio (chi-square) statistic (L2) indicates the amount of association among the variables unexplained following estimation of the model (i.e., deviation between the maximum likelihood estimates for expected and observed cell frequencies) and thus provides an indication of lack of fit. For this statistic, lower values indicate better fit and follow a χ2 distribution with large samples. The L2 can be divided by its respective degrees of freedom (df) to yield an approximate F statistic (Haberman, 1979). Both of the information criteria statistics (Bayesian [Schwarz, 1978] and Akaike (1981) are useful for sparse data and weight both model fit and parsimony (adjusting the log likelihood by the number of parameters in the model resulting in a maximum penalized likelihood statistic). Again lower values of both these statistics indicate better fit. The percent reduction in L2 is less statistically precise than the information criteria statistics, but provides an overall sense of variation in the model accounted for by the k>1 cluster models versus a fully saturated model. Based on the model fit statistics contained in Table 3 there is a slight improvement with increasing number of classes, peaking at around four classes. The BIC does not change appreciably from the four-cluster solution (5976) to the five-cluster model (5978) and there is a 1% gain in Classification Error between these two models. Recent simulation studies reinforce the BIC works well to discriminate the number of classes (Nylund, Asparouhov and Muthén, 2007). Using the principle of parsimony (Kotz and Johnson, 1985) the statistical fit indices points toward the four-class model as an acceptable summarization of the data. Increasing the number of classes beyond this ‘saturation point’ would result in weak identifiability resulting from too many classes, too few class indicators, and too few people allocated to the various classes (i.e., sparse data), affecting estimation of item probabilities (Garrett and Zeger, 2000).
Table 3.
Fit Statistics from the Latent Class Analyses
| Model Description |
Log-likelihood (L2) |
BICL2 | AICL2 | Npar/DF | P-value | CEa | %ERb | L2/df |
|---|---|---|---|---|---|---|---|---|
| 1-class | 12445.92 | 8473.08 | 11215.92 | 24/615 | 4.6 e-2171 | .0000 | 0.0 | 20.24 |
| 2-class | 10201.52 | 6428.94 | 9033.52 | 55/584 | 3.0 e-1729 | .0385 | 81.97 | 17.46 |
| 3-class | 9628.81 | 6056.48 | 8522.81 | 86/553 | 3.0 e-1631 | .0632 | 77.37 | 17.41 |
| 4-class | 9348.56 | 5976.49 | 8304.56 | 117/522 | 3.6 e-1593 | .0724 | 75.12 | 17.91 |
| 5-class | 9150.80 | 5978.98 | 8168.80 | 148/491 | 3.8 e-1572 | .0820 | 73.53 | 18.64 |
| 6-class | 9036.55 | 6064.99 | 8116.55 | 179/460 | 1.7 e-1568 | .0812 | 72.61 | 19.64 |
| 7-class | 8845.52 | 6074.23 | 7987.52 | 210/429 | 2.7 e-1549 | .0726 | 71.08 | 20.62 |
Note. CE = Classification Error is the proportion of cases expected to be misclassified values closer to zero are better).
%ER = percent error reduction in L2 when model is pitted against the null model of complete independence. Model is conditioned for gender (male), age group (< 21 years of age), race (white), marital status (married), education (high school graduate), and site.
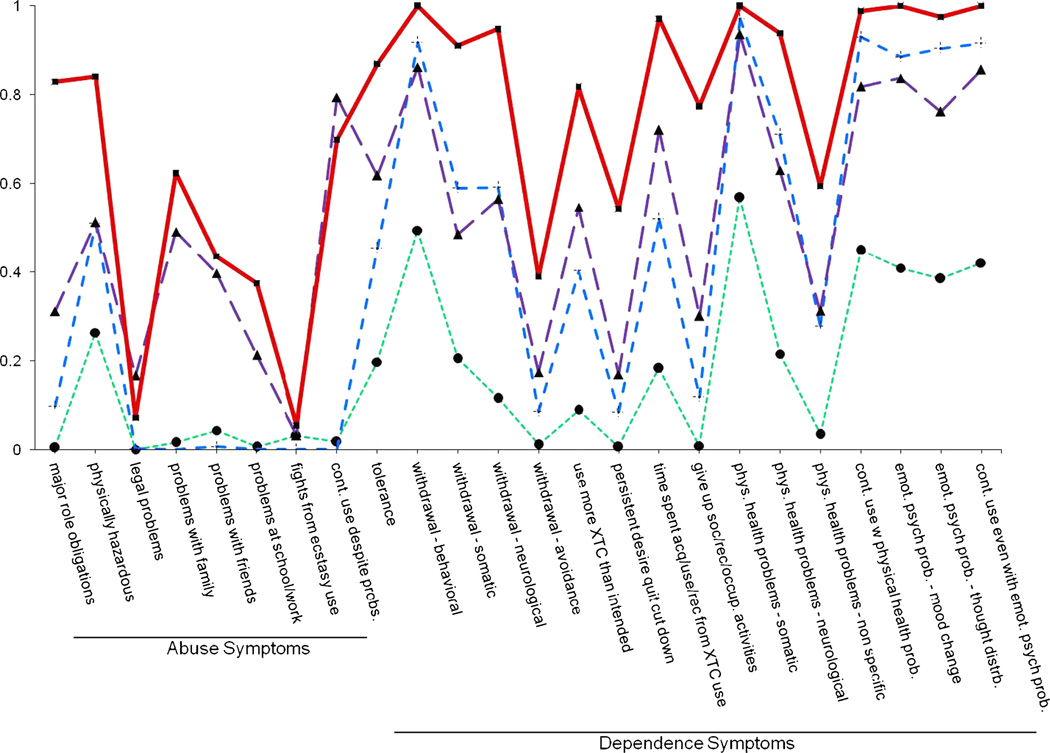
Figure 1 contains a plot of the conditional item endorsement probabilities for all 24 symptoms based on the four-cluster model. Members of Cluster 1 (27.1% estimated prevalence of the total sample) do not tend to meet criteria for abuse symptoms (none reported an endorsement probability above .50) or dependence symptoms with the exception of physical health problems-somatic (.57). Cluster 1 is thus aptly named the ‘negative’ group since persons in this group are relatively symptom free and do not meet abuse or dependence criteria. Cluster 2 (34.6%) contains individuals who do not meet criteria for abuse and have a slightly more than 50% endorsement probability for continued use in situations in which it is physically hazardous (.51). Of the 16 dependence symptoms, 10 are above the .50 endorsement cut-point, including those symptoms belonging to the withdrawal group, a few of the physical health problems as well as all of the emotional/psychological problem symptoms. What distinguishes this cluster group is the relatively high endorsement of the withdrawal-behavioral symptom (.92), physical health problems-somatic (.97), continued use despite physical health problems (.93), and the consistently high level of symptom reporting for the emotional/psychological problems (.88, .90, and .91, respectively). We called individuals in this second cluster ‘mild dependent.’ Members of Cluster 3 typified itself by selecting almost every symptom at a moderate level and are delineated by only two abuse symptoms that exceed the .50 endorsement probability threshold (e.g., continued use in situations which are physically hazardous [.51] and continued use despite social or interpersonal problems [.79]). Notably, one symptom, problems with family, is slightly under the designated threshold (.49). The endorsement patterns for the dependence symptoms reinforce further that these individuals are different from the mild group. For example, six dependence symptoms exceed .70; thus we call this group the ‘moderate-dependent’ cluster.
Figure 1. Final four-cluster LCA model depicting conditional probabilities.
● = Cluster 1 (Negatives); + = Cluster 2 (Mild); ▲ = Cluster 3 (Moderate); ■ = Cluster 4 (Severe Dependent).
The final dependent group, Cluster 4 shows a clearly delineated pattern that falls in line with dependence (20.1% estimated prevalence). There is evidence of a consistent pattern of symptom endorsement for abuse symptoms and 12 of the dependence symptoms and thus given the morbid characteristics of this cluster it is labeled the ‘severe-dependent’ group, characterized by more pronounced reporting of dependence symptoms.
In summary, a four-cluster model fit the data the best, mimicking the mild, moderate and severe depiction of an earlier DSM nosology§. Abuse did not figure prominently as a diagnostic characterization of Ecstasy users. Additionally, abuse symptoms do not occur independently of dependence symptoms. Further, only two of the 24 symptoms overall (2 out of 8 abuse symptoms) did not significantly distinguish cluster membership including legal problems from Ecstasy use (p ≤ .17) and fighting (p ≤ .05) and thus could be considered for elimination.
3.5. Multinomial Logistic Regression Analyses
With the obtained four-class solution in hand, a final step involved validating the derived clusters against the external markers using multinomial (polytomous) logistic regression. Individuals were assigned to classes using their estimated conditional posterior probabilities of class membership based on their symptom reporting. Class membership is then treated as a dependent measure and regressed on the external marker variables. This type of analysis is not without statistical pitfalls given that the posterior probability of latent class membership is ‘estimated’ and not known. Thus there is an element of ‘uncertainty’ in the prediction of class membership, which leads to biases in both the estimate and the test statistic (Roeder et al., 1999). Some statistical solutions include using model-averaging, use of the BIC statistic over the likelihood ratio test to choose models, and where appropriate using substantive arguments based on model dominance to choose the correct model (Kass and Raftery, 1995).
A total of four external marker domains were modeled in the multinomial logistic regression including: (1) an ordinal measure of lifetime Ecstasy use (low, medium, and high), frequency of use in the past 30 days, number of days using Ecstasy (past 30 days), (2) two measures of other drug use within the past year including number of other club drugs and other drugs excluding club drugs, (3) an index of criminal behavior, and (4) measures of depressive symptoms, social support, stressful life events, and motivation for Ecstasy use. We tested the discriminative value of each domain incrementally, which provided a means to evaluate the significance of each respective measure with regard to class membership within the different domains and to systematically detect possible sources of suppression. Non-significant variables were eliminated through use of backward elimination procedures with the overall incremental change to the model examined by the Wald χ2 statistic (Hosmer and Lemeshow, 2000).
The reference group or baseline category was the clean ‘negatives’ (Cluster 1) from the four-cluster model. Prior to testing the incremental value of each of the four behavioral and psychosocial domains, we examined the relative importance of the demographic control factors. Only age significantly predicted class membership (Cluster 2: b = −.529, SE = .213, z = 2.49, p ≤ .05; Cluster 3: b = −.661, SE = .258, z = 2.56, p ≤ .05; and Cluster 4: b = −.792, SE = .250, z = 3.17, p ≤ .01), Likelihood Ratio (LR) χ2(18) = 49.90, p ≤ .0001), Psuedo R2 = .029. Both site (b = .588, SE = .147, z = 3.99, p ≤ .001) and gender (b = −.626, SE = .246, z = 2.54, p ≤ .05) were significant predictors for Cluster 4. Of the three consumption measures, only lifetime quantity predicted cluster membership (Cluster 2: b = .743, SE = .184, z = 4.03, p ≤ .001; Cluster 3: b = 1.49, SE = .243, z = 6.14, p ≤ .001; Cluster 4: b = 2.31, SE = .268, z = 8.65, p ≤ .001) with a Pseudo R2 = .096, LR χ2(18) = 166.06, p ≤ .001. The Wald test for removing parameters (constrained to zero) indicated that trimming the model of both number of times used within past 30 days and frequency of Ecstasy use per day would not cause an appreciable decrement in model fit.
Next in the sequence were the measures of other drug use. None were significant and thus were trimmed from the model (there was no increase in Pseudo R2 with their inclusion). Criminal behavior was significant for all three cluster groups (Cluster 2: b =−.078, SE = .029, z = 2.61, p ≤ .01; Cluster 3: b = −.087, SE = .037, z = 2.35, p ≤ .05; Cluster 4: b = −.103, SE = .038, z = 2.66, p ≤ .01) with a Pseudo R2 = .097, LR χ2(15) = 167.42, p ≤ .001. Negative loadings for each of the coefficients indicated less criminal activity compared to the negatives. Motivation (tapping reasons for Ecstasy use and contextual factors surrounding use) was significant for all three cluster groups (Cluster 2: b = .109, SE = .030, z = 3.62, p ≤ .001; Cluster 3: b = .164, SE = .038, z = 4.36, p ≤ .001; Cluster 4: b = .312, SE = .042, z = 7.34, p ≤ .001) with a Pseudo R2 = .155, LR χ2(27) = 267.29, p ≤ .001. While the severe dependent cluster was more likely to be depressed (b = .131, SE = .039, z = 3.29, p ≤ .001) the mild dependent cluster was marginally significant for depression (b = .072, SE = .038, z = 1.86, p ≤ .07). Neither stressful life events nor social support related significantly to cluster membership.
Table 5 shows the results for the final trimmed model containing all of the significant external markers for each of the clusters, LR χ2(21) = 258.70, p ≤ .001, Pseudo R2 = .15. The far right column includes the relative risk ratios (rrr), which, similar to an odds ratio obtained from a standard logistic model, indicates the odds of being in one cluster compared to negatives in the referent Cluster 1. Compared to negatives, Ecstasy users in the mild dependent cluster (Cluster 2) were younger, reported more of lifetime pill use, were less likely to be criminally involved, and reported more problems resulting from contextual and motivational cues for Ecstasy use. Whereas compared to negatives, members of the moderate dependent cluster (Cluster 3) were younger, consumed more Ecstasy pills in their lifetime, they reported less criminal involvement, more motivational problems, and more depressive symptoms. Additionally, members in the severe dependent group (Cluster 4) had characteristics identical to the moderate dependent class except that they were less likely to be female. Comparatively speaking, the relative risk ratios in Table 5 reinforce the severity of criteria and clinical features that accompanies membership in this cluster. The risk ratio for lifetime pill quantity was almost twice the moderate group (4.47 versus 2.72) and substantially higher than the mild group (4.47 versus 1.61).
Table 5.
Results of Multinomial Regression Analyses
| Mild “+” | β | SE | P >|z| | RRR1 | 95% CI |
|---|---|---|---|---|---|
| Site | −.192 | .141 | .173 | .826 | .627 – 1.088 |
| Gender (male) | .014 | .234 | .950 | 1.015 | .642 – 1.605 |
| Age (older) | −.705 | .226 | .002 | .494 | .317 – .769 |
| Lifetime Ecstasy Pill Use | .476 | .206 | .021 | 1.610 | 1.073 – 2.413 |
| Criminal Behavior Index | −.099 | .031 | .002 | .906 | .852 – .963 |
| Motivation (contextual cues) | .112 | .029 | <.001 | 1.119 | 1.056 – 1.186 |
| CES-D (depressive symptoms) | .048 | .032 | .129 | 1.049 | .986 – 1.116 |
| Intercept | −1.470 | .484 | .002 | N/A | N/A |
| Moderate “▲” |
|||||
| Site | −.062 | .171 | .720 | .940 | .672 – 1.316 |
| Gender (male) | .026 | .291 | .927 | 1.027 | .581 – 1.815 |
| Age (older) | −1.04 | .284 | <.001 | .354 | .203 – .618 |
| Lifetime Ecstasy Pill Use | 1.00 | .272 | <.001 | 2.727 | 1.599 – 4.649 |
| Criminal Behavior Index | −.126 | .039 | .001 | .881 | .816 – .952 |
| Motivation (contextual cues) | .172 | .037 | <.001 | 1.187 | 1.104 – 1.277 |
| CES-D (depressive symptoms) | .082 | .037 | .026 | 1.086 | 1.010 – 1.167 |
| Intercept | −4.535 | .672 | <.001 | N/A | N/A |
| Severe Dependent “■” |
|||||
| Site | .246 | .180 | .172 | 1.27 | .898 – 1.821 |
| Gender (male) | −.602 | .305 | .048 | .548 | .301 – .996 |
| Age (older) | −1.46 | .304 | <.001 | .232 | .128 – .420 |
| Lifetime Ecstasy Pill Use | 1.50 | .304 | <.001 | 4.47 | 2.461 – 8.119 |
| Criminal Behavior Index | −.179 | .043 | <.001 | .836 | .768 – .910 |
| Motivation (contextual cues) | .304 | .041 | <.001 | 1.36 | 1.251 – 1.469 |
| CES-D (depressive symptoms) | .124 | .038 | .001 | 1.13 | 1.051 – 1.219 |
| Intercept | −8.179 | .837 | <.001 | N/A | N/A |
Note. RRR = Relative Risk Ratio of being in the designated cluster versus the clean negatives (Cluster-1).
4. Discussion
We applied the first LCA of Ecstasy users obtained from three population-based samples to derive meaningful diagnostic typologies. These efforts follow on the tails of previous research with other major drugs of abuse that accentuate the need for two diagnostic classes possessing different clinical profiles and realizing that Ecstasy is not yet a separate drug category in the DSM and ICD nomenclature. The analyses used symptom rather than criteria information to obtain a more fine-grained picture of problems associated with Ecstasy use. Several important findings emerge from this study. First, statistical information helped us to enumerate a four-class model based on the patterns of symptoms related to Ecstasy consumption. This more variegated taxonomy might have otherwise been missed with the imposition of the traditional abuse/dependence diagnostic typology. In particular, the four-cluster solution yielded a group of Ecstasy users relatively asymptomatic for abuse symptoms (with the exception of situations in which use is physically hazardous). In many respects, this mild cluster mimicked the ‘diagnostic orphans’ that have been observed in the alcohol literature with both adolescent and adult populations (Hasin and Paykin, 1998; Pollock and Martin; 1999; Sarr et al., 2000). The patterning of symptom reporting associated with the mild cluster would not necessarily meet the traditional dependence criteria according to DSM-IV for a substance use disorder. Further, members of this cluster mimic negatives with respect to most of the clinical features that accompany abuse symptoms.
Individuals that would be characterized as diagnostic orphans and be part of the mild cluster did not quite show the same patterning of dependence symptoms as with individuals in the moderate or even the more severe-dependent clusters. Because of their sub-clinical or sub-diagnostic nature, users in this cluster are likely to fall through the cracks of classification despite reporting being affected by a full gamut of withdrawal, physical health and psychological/emotional problems. Participants who were sorted into the moderate dependent cluster (Cluster 3) were less likely to show clinical features of dependence compared to the severely dependent cluster but were more likely to select abuse symptoms as clinical features of their Ecstasy use than the mild group. In this regard, individuals in the moderate cluster appear to be ‘transitioning’ between a non-diagnostic status and a more florid state of dependence. Moreover, the lack of consistent and high rates of endorsement for the abuse symptoms may represent a clear cut and premorbid diagnostic feature of Ecstasy dependence. The final cluster showed clear clinical features of the dependence syndrome replete with symptom patterns reinforcing a wide gamut of behavioral, physiological, neurological, and psychological problems stemming from Ecstasy use.
Additional analyses sought to validate the obtained four classes with non-diagnostic measures of psychosocial and behavioral risk associated with addiction in general and more specifically with Ecstasy use. Among the key demographic measures included in the model younger age was instrumental in differentiating the mild (orphan), moderate, and severe cluster groups from the negatives but did not effectively discriminate these three groups from each other (based on the relative risk ratios). Among the measures of Ecstasy consumption, only lifetime quantity of pill use significantly differentiated cluster membership. This was somewhat surprising since the other two consumption measures captured recent and intense patterns of use, which we expected would be related to certain physical health problems and could provide a clear-cut empirical basis to distinguish Ecstasy users. It is possible that more recent use does not discern cluster groups well because despite inclusion criteria stipulating Ecstasy use in the past year, many users curtailed their use in the months preceding the study, diminishing the overall importance of recent consumption patterns. There also is the possibility that consumption is age dependent and older participants had more exposure allowing them time to inure to the drug and the drug’s consequences. The addition of consumption measures controlling for age weakens this argument considerably. Moreover, zero-order associations show that age is not a powerful factor in consumption practices (r = .11, p ≤ .01) but is moderately related to years of use (r = .54, p ≤ .0001). Across the board, age is weakly related to the individual symptoms, but once these symptoms are aggregated to define homogeneous groups of individuals, age becomes an efficient predictor of class membershipf. In a series of logistic regression analyses, not reported here, we regressed the individual lifetime symptoms on age, age of onset, years of use, lifetime quantity, and site. None of these models indicated that age was a significant predictor. Likewise, consumption measures were fairly independent, thus elimination from the model of a measure of recent use and intensity of use (frequency per day) more likely reflects the potency of sustained long-term use, captured by lifetime number of pills.
Consistent with reports of multiple drug use by Ecstasy users, we also modeled involvement with other drug use as part of the multinomial regression models. These measures were not informative with respect to cluster membership and were dropped from further tests. Their lack of differentiability was also somewhat striking given evidence of lifetime polydrug use by Ecstasy users. Subsequent follow-up analyses not reported showed other drug use (not including club drugs) was a significant factor differentiating the clusters but once controls for demographics and lifetime Ecstasy pill quantity were included, this effect considerably diminished. In effect, the prevalent nature of polydrug use among all types of Ecstasy users does not efficiently distinguish them based on symptom reporting and the underlying clinical features of dependence.
Despite reporting less Ecstasy use, the negative or symptom free cluster reported more criminal involvement than the remaining clusters and there was no evidence of suppression in this effect. Quite possibly, the older age associated with negatives coupled with a history of multiple drug use may portend greater criminal activity. Interestingly, relative risk ratios for the mild, moderate, and severe clusters were comparable for the criminal behavior index (.91, .88, and .84 for mild, moderate, and severe clusters, respectively), showing little differentiation of criminal activity between these clusters.
Among the remaining external markers, higher depression scores distinguished all individuals in the moderate and severe clusters from negatives. The less than optimal performance by depressive symptoms as an external marker is somewhat surprising because the literature documents persistent forms of depression and other mental health problems among both light and heavy Ecstasy users (Curran and Travill, 1997; Davison and Parrott, 1997; Krystal and Proce, 1992; MacInnes et al., 2001). One essential factor that may lesson or attenuate the importance of this marker is the recent time frame covered by the questions tapping depressive symptoms (one week). Moreover, inclusion criteria for this study necessitated a minimum threshold of Ecstasy use in the one year preceding the study; however, this usage could have abated allowing enough time for any persistent symptoms of depression to cease.
A multi-faceted measure of motivation optimally distinguished between the base and remaining clusters but did not appreciably separate the mild, moderate, and severe clusters from each other. The components of the motivational measure included means to obtain Ecstasy (e.g., free, trading sex, dealing), people and places to obtain Ecstasy (e.g., spouse, friend, dealer and using it at raves, parties, work or school), people with whom to use Ecstasy with (e.g., spouse, partner, dealer, alone), and impetus to use Ecstasy (i.e., relieve stress, bond with friends, get more in touch with yourself). Ecstasy users are apparently sensitive to contextual factors and motivational cues that may play a role in maintaining their use (i.e., support from friends) including attendance at raves which increases exposure to Ecstasy.
4.1. Limitations
The results of this study need to be interpreted in light of several important limitations. First, the strategy we chose to facilitate mapping diagnostic groupings was based on symptom level and not a more restrictive criteria approach. We felt this approach would help give us an initial upper hand in determining the diagnostic value of each symptom and perhaps lead to a better understanding of Ecstasy-related substance use disorders at this formative stage in Ecstasy nosology. Had we relied first on criterion-level information, which consolidates and then abbreviates symptom data, we would have glossed over important distinctions as to which symptoms are most useful in rendering abuse and dependence diagnoses. Related to this the time frames used for the symptom data is lifetime and thus may gloss over important discriminating events that could usefully discern user typology. Events may have transpired during the framework of a single year to abate or exacerbate symptoms and we don’t have a barometer to gauge the effects of these experiences and their relations to drug use.
Second, the study captured cross-sectional relations between drug use and symptoms. Thus, we are unable to make any inferences regarding stability of symptom reporting across time and relate this prospectively to patterns of Ecstasy use. To date, only one study has included longitudinal data, with a fairly representative sample, and included adequate psychometric assessment (von Sydow et al., 2002). More research with high quality assessment and that follows subjects over time is required to make inferences regarding the stability of diagnosis and determine which factors have utility for making accurate diagnosis.
With regard to the multinomial regression models, we included a select number of external marker variables that have been linked as etiological risk factors or consequences of Ecstasy use (i.e., depression). The moderately small magnitude of model variance accounted for by this set of markers (< 16%) clearly indicates the need to widen the net in an effort to learn more about the different types and patterns of Ecstasy users. Other factors that may precipitate a deeper understanding of Ecstasy use could certainly draw upon psychological and motivational measures linked with drug use in general and specifically with insight oriented drugs like Ecstasy. In addition to the low overall proportion of variance accounted for in the multinomial model, several of the external marker variables were not informative with regard to cluster assignment. This opens up the door for future studies to investigate additional non-diagnostic marker variables that may be informative. Other factors that might be considered include measures of family functioning, interpersonal relations, self-esteem, mental health, impulsivity, and sensation seeking all of which can precipitate drug use.
Other concerns that stem from the study design include the potential lack of purity with street purchased Ecstasy. Although we were able to obtain a clear picture of consumption patterns in defined periods of time, we know very little about street purity. The Drug Enforcement Agency conducts laboratory analyses of seized drugs to determine purity: however it is still possible that many purchases of street drugs involve adulterants. Customarily, Ecstasy tablets are stepped on with methamphetamine, caffeine, cough suppressant (dextromethorphan), the diet drug ephedrine, and even impure cocaine. Unfortunately, we did not obtain any information on street purity from the informants at the time of the interviews. Communication with the DEA offices in the two U.S. cities indicated that Ecstasy pills contained mostly MDMA by forensic analysis£. We also did not perform any biological assays of fluids (saliva, urine, or blood) to determine physiological markers of purity relying instead of self-report for all data collection. Self-report is an appropriate methodology for a convenience sample that requires extraordinary recruitment measures to obtain valid interviews. Ecstasy is a psychotropic drug with mind-altering properties and is used in very special circumstances like raves. As such, users are reminiscent of the sixties counterculture replete with hippies endorsing peace, love, unity, and respect. The snowball interview methods netted a group of motivated users who wanted to share their experiences with the field workers. Interviewers were instructed to ask about any use of drugs on the day of the interview and also to query subjects whether they were high at the time of the interview.
4.2. Implications for DSM-V
To date, this study contains the largest number of Ecstasy users studied for diagnostic purposes. As such, the study findings suggest Ecstasy users can and do share reports of their symptoms from drug use and this information can responsibly inform DSM-V in several ways. First, the multi-site findings from this four-cluster model argue that Ecstasy users may not fall cleanly and decisively into a two-tiered system of diagnostic classification. While many other drugs may follow this traditional cookie cutter diagnostic system, based on their patterns of symptom reporting, Ecstasy users in the present sample fit into a more variegated classification system. Second, and somewhat related to this first point, the nature of the symptoms that underlie abuse and dependence may have to be reformulated especially in light of the absence of any clear cut pattern of abuse for all four clusters. Of the eight abuse symptoms we used, only one group endorsed any of them at a rate that would signify detection for diagnosis (severe-dependent cluster). It may be that several of the abuse symptoms are not applicable for drugs possessing similar behavioral properties like Ecstasy (fighting and legal problems). This was also apparent for some of the dependence symptoms, which were not heavily selected as clinical features by Ecstasy users in this sample. Consistent with the argument we made for the behavioral properties of a drug like Ecstasy, the pharmacological properties of Ecstasy may not lend themselves to specific symptoms (e.g., continued use despite withdrawal) in the same manner as other drugs like cocaine or heroin.
Third, there also may be implications for treatment providers who rely on diagnostic criteria to inform treatment progress and selection of treatment modalities. Ecstasy users may claim their drug use is not problematic and fail to acknowledge remediation through treatment but their symptoms indicate otherwise. It is especially important for treatment providers to recognize that there may be selective recall and importance for some symptoms and a diminution of others when Ecstasy users are reporting their problems. The pronounced nature of certain adverse effects and the lack of importance to other areas (i.e., desire or efforts to cut down) may encourage treatment experts to attend more to certain problems specific to this drug while diminishing the importance of others (i.e., interpersonal problems) that curry favor in the treatment community. It is quite possible that Ecstasy users may not seek treatment for their Ecstasy use per se but for another drug that instigates problems. The fine line between those problems that arise from Ecstasy and those from other drugs is made clearer in part by studies of this nature. As a result, treatment experts may be able to acquire deeper insight into the problems associated with chronic use/abuse of Ecstasy and become more acutely aware how these problems manifest themselves.
We are currently engaged in a replication study in Taipei, the Republic of China. Additional studies like this can only help to increase our understanding of Ecstasy diagnostics and allow for closer inspection of cultural differences in symptom reporting especially in the face of criminal sanctions related to even admitting use in some parts of the world. Finally, despite the emergence of two distinct clusters capturing the mild and moderate users, the overall impression from these findings supports the heuristic value of an abuse/dependence dichotomy for Ecstasy. Future studies that rely on similar analytic strategies that can map closely to the pattern of symptoms used in the present study should be able to confirm the validity of diagnostic classification. In this respect, this study represents the first essential step towards validating the clinical consequences of Ecstasy use, which deserves further empirical attention.
Table 4.
Conditional Probabilities (Loadings) From Four Cluster Latent Class Model (N=639)
| Symptom Measure | Cluster-1 Negatives (27.1%) |
Cluster-2 Mild (34.6%) |
Cluster-3 Moderate (18.1%) |
Cluster-4 Severe (20.1%) |
|---|---|---|---|---|
| Failure to fulfill major role obligations | .0041 | .0977 | .3109 | .8266 |
| Situations in which it is physically hazardous | .2633 | .5105 | .5124 | .8398 |
| Substance-related legal problems | .0001 | .0023 | .1662 | .0716 |
| Problems with family | .0160 | .0003 | .4915 | .6230 |
| Problems with friends | .0430 | .0071 | .3968 | .4350 |
| Problems with people at school/work | .0064 | .0002 | .2131 | .3740 |
| Problems w fighting | .0306 | .0000 | .0316 | .0546 |
| Continued use despite social or interpersonal problems | .0176 | .0003 | .7934 | .6984 |
| Tolerance symptoms | .1972 | .4544 | .6175 | .8685 |
| Withdrawal behavioral | .4945 | .9171 | .8615 | .9996 |
| Withdrawal somatic | .2045 | .5892 | .4852 | .9094 |
| Withdrawal neurological | .1150 | .5911 | .5648 | .9471 |
| Continued use despite withdrawal symptoms | .0108 | .0854 | .1737 | .3894 |
| Taken in large amounts | .0887 | .4024 | .5472 | .8174 |
| Desire or efforts to cut down | .0060 | .0842 | .1685 | .5425 |
| Time spent to obtain drug or recover from effects | .1832 | .5199 | .7198 | .9701 |
| Important activities given up or reduced | .0089 | .1181 | .3003 | .7735 |
| Physical health problems – somatic | .5678 | .9703 | .9350 | .9997 |
| Physical health problems – neurological | .2151 | .7102 | .6297 | .9376 |
| Physical health problems – non specific | .0344 | .2781 | .3118 | .5936 |
| Continued use despite physical health problems | .4487 | .9288 | .8174 | .9877 |
| Emotional/psychological problems – mood | .4087 | .8842 | .8369 | .9995 |
| Emotional/psychological problems – thought disorder | .3844 | .9032 | .7618 | .9740 |
| Continued use despite emotional & psychological problems | .4205 | .9150 | .8554 | .9995 |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The inconsistency in reporting also varies depending on whether we look at prevalence rates for lifetime, past year, or past month and contingent on whether the respondent is male or female. Overall, the NSDUH statistics show that rates of consumption for past year and past month are going down in the period between 2001 and 2006. In some cases, however, especially if we examine older age groups (26 and older), lifetime, and past year rates are going up. In addition, consumption patterns appear to be declining for males and females in the youngest age group (12–17), however, this same pattern is not observed among those reporting some illicit drug use including hallucinogens (where club drugs were bundled in the NSDUH computer survey). In addition, past year initiation rates (new users) is down from .5% to .3% in the same time frame for survey respondents 12 and older. However, rates of initiation are up for the period 2005 to 2006 particularly if we examine data for respondents who tried the substance for the first time among all those who report some drug use over the past year (past year initiates). For instance, isolating respondents between 18 and 25 years of age who report they already use illicit drugs, rates of initiation to Ecstasy are 32.2% in 2005 increasing to 40.1% in 2006. In addition, it would appear that trends in Ecstasy consumption are declining (lifetime, past year, past month) for very young survey respondents (ages 12 and 13), but as we examine the data for older youth (ages 14–18), there is an apparent increase in prevalence rates for lifetime, past year, and past month Ecstasy use.
Using only the accepted four and seven criteria for abuse and dependence, respectively, would argue strongly for the criteria typologies without truly testing their appropriateness at the symptom level. Thus, we included the full set of five abuse and nine dependence categories at the symptom level.
We are grateful to the reviewer who pointed out the problems resonating around inclusion of age as a predictor given that consumption may be age dependent. This would be true if age was related linearly and monotonically to consumption, but that is not the case in these data. In fact, age is only weakly related to some consumption measures. If consumption was age dependent and consumption was a driving force in symptomatology, then age may factor into reporting of various abuse and dependence symptoms. However, this is also not the case. In fact, age was not a significant predictor of an index reflecting total abuse symptoms and very weakly associated with an index of dependence symptoms (t = 3.29, p ≤ .01; b = − 1.37, SE = .42). Age was also not a significant predictor of the individual criterion, controlling for site, age of onset, years of use, and lifetime quantity. It would appear that age surfaces as an efficient predictor of class status only when the underlying currents of response profiles are bundled according to severity.
One assumption of LCA is that the response to an observed indicator (used to classify individuals) is not informative with respect to answers to any other indicator once the latent class variable is controlled. That is, a persons’ latent class membership tells you everything about the association among the items used to derive the class membership score. This assumption of conditional independence can be relaxed, allowing dependence between items that is posited as residual covariances (Hagenaars, 1988). One problem is that such model refinements are not theory-based and capitalize on chance associations as much as they reflect true underlying variation. At the suggestion of one reviewer, we tested whether relaxing local independence would create interpretable models that augment the four-class model we report. Unfortunately, any of the models obtained with the local dependence criteria imposed were not informative from a theoretical point of view. The results of these models with the relaxed assumptions can be obtained from the first author.
Information on purity obtained from seized drug program based on analysis for trapped solvents, Drug Enforcement Agency, Office of Forensic Sciences, Special Testing Research Laboratory, Drug and Chemical Evaluation Section, Alexandria, Virginia.
References
- Adlaf EM, Smart RG. Party subculture or dens of doom? An epidemiological study of rave attendance and drug use patterns among adolescent students. J. Psychoactive Drugs. 1997;29:193–198. doi: 10.1080/02791072.1997.10400187. [DOI] [PubMed] [Google Scholar]
- Akaike H. Likelihood of a model and information criteria. J. Econ. 1981;16:3–14. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- Anthony JC, Helzer J. Syndromes of drug abuse and dependence. In: Robins LN, Regier DA, editors. Psychiatric Disorders in America: The ECA study. New York: The Free Press; 1991. pp. 116–154. [Google Scholar]
- Basu D, Ball SA, Feinn R, Gelernter J, Kranzler HR. Typologies of drug dependence: Comparative validity of a multivariate and four univariate models. Drug Alcohol Depend. 2004;73:289–300. doi: 10.1016/j.drugalcdep.2003.11.004. [DOI] [PubMed] [Google Scholar]
- Battaglia G, Yeh SY, De Souza EB. MDMA-induced neurotoxicity: Parameters of degeneration and recovery of brain serotonin neurons. Pharmacol Biochem, Behav. 1988;29:269–274. doi: 10.1016/0091-3057(88)90155-4. [DOI] [PubMed] [Google Scholar]
- Beck J. The public health implications of MDMA use. In: Peroutka SJ, editor. Ecstasy: The Clinical, Pharmacological and Neurotoxicological Effects of the Drug MDMA. Boston: Kluwer; 1990. pp. 77–103. [Google Scholar]
- Bhattachary S, Powell J. Recreational use of 3,4-methylenedioxymethamphetamine (MDMA) or ‘ecstasy’: Evidence for cognitive impairment. Psychol Med. 2001;31:647–658. doi: 10.1017/s0033291701003828. [DOI] [PubMed] [Google Scholar]
- Bolla KI, McCann UD, Ricaurte GA. Memory impairment in abstinent MDMA (“Ecstasy”) users. Neurology. 1998;51:1532–1537. doi: 10.1212/wnl.51.6.1532. [DOI] [PubMed] [Google Scholar]
- Bryant KJ, Rounsaville BJ, Babor TF. Coherence of the dependence syndrome in cocaine users. Brit J Addict. 1991;86:1299–1310. doi: 10.1111/j.1360-0443.1991.tb01705.x. [DOI] [PubMed] [Google Scholar]
- Bucholz K, Hesselbrock V, Heath A, Kramer J, Schuckit M. A latent class analysis of antisocial personality disorder symptom data from a multi-centre family study of alcoholism. Addiction. 2000;95:553–567. doi: 10.1046/j.1360-0443.2000.9545537.x. [DOI] [PubMed] [Google Scholar]
- Callow N. Use of the “snowballing” technique to investigate subjective mood and personality traits associated with “ecstasy.”. Proceedings of the British Psychological Society. 1996;4:65. [Google Scholar]
- Carlson RG, Wang J, Falck RS, Siegal HA. Drug use practices among MDMA/ecstasy users in Ohio: A latent class analysis. Drug Alcohol Depend. 2005;79:167–179. doi: 10.1016/j.drugalcdep.2005.01.011. [DOI] [PubMed] [Google Scholar]
- Chen L, Eaton WW, Gallo JJ, Nestadt G. Understanding the heterogeneity of depression through the triad of symptoms, course and risk factors: A longitudinal, population-based study. J Affect Disord. 2000;59:1–11. doi: 10.1016/s0165-0327(99)00132-9. [DOI] [PubMed] [Google Scholar]
- Chick J. Is there a unidimensional alcohol dependence syndrome? Br. J. Addict. 1980;75:265–280. doi: 10.1111/j.1360-0443.1980.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Clogg CC. Latent class models. In: Arminger G, Clogg CC, Sobel ME, editors. Handbook of Statistical Modeling for the Social and Behavioral Sciences. New York: Plenum Press; 1995. pp. 311–359. [Google Scholar]
- Cohen RS. The Love Drug – Marching to the Beat of Ecstasy. New York: Haworth Medical Press; 1998. [Google Scholar]
- Cole JC, Sumnall HR. Altered states: The clinical effects of Ecstasy. Pharmacol Ther. 2003;98:35–58. doi: 10.1016/s0163-7258(03)00003-2. [DOI] [PubMed] [Google Scholar]
- Collins LM, Graham JW, Long JD, Hansen WB. Cross-validation of latent class models of early substance use onset. Mult Behav Res. 1994;29:165–183. doi: 10.1207/s15327906mbr2902_3. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Keating SK. Operationalization of alcohol and drug dependence criteria by means of a structured interview. Recent Dev Alcohol. 1990;8:69–83. [PubMed] [Google Scholar]
- Cottler LB, Schuckit MA, Helzer JE, Crowley T, Woody G, Nathan P, Hughes J. The DSM-IV field trial for substance use disorders: Major results. Drug Alcohol Depend. 1995;38:59–69. doi: 10.1016/0376-8716(94)01091-x. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Womack SB, Compton WM, Ben-Abdallah A. Ecstasy abuse and dependence among adolescents and young adults: Applicability and reliability of DSM-IV criteria. Hum Psychopharmacol. 2001;16:599–606. doi: 10.1002/hup.343. [DOI] [PubMed] [Google Scholar]
- Crum RM, Storr CL, Chan Y-F. Depression syndromes with risk of alcohol dependence in adulthood: A latent class analysis. Drug Alcohol Depend. 2005;79:71–81. doi: 10.1016/j.drugalcdep.2005.01.001. [DOI] [PubMed] [Google Scholar]
- Curran HV, Travill RA. Mood and cognitive effects of (+/−)3,4-methylenedioxymethamphetamine (MDMA, “ecstasy”): Weekend “high” followed by mid-week low. Addiction. 1997;92:821–831. [PubMed] [Google Scholar]
- Davidson R, Bunting B, Raistrick D. The homogeneity of the alcohol dependence syndrome: A factorial analysis of the SADD questionnaire. Brit J Addict. 1989;84:907–915. doi: 10.1111/j.1360-0443.1989.tb00763.x. [DOI] [PubMed] [Google Scholar]
- Davison D, Parrott AC. Ecstasy in recreational users: Self-reported psychological and physiological effects. Hum Psychopharmacol. 1997;12:91–97. [Google Scholar]
- de Wijngaart V, Braam R, de Bruin D, Fris M, Maalste N, Verbraeck H. Ecstasy use at large-scale dance events in the Netherlands. J Drug Issues. 1999;29:679–702. [Google Scholar]
- Eaton WW, McCutcheon A, Dryman A, Sorenson A. Latent class analysis of anxiety and depression. Soc. Meth. Res. 1989;18:104–125. [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: Provisional description of a clinical syndrome. Br Med J. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwwod LJ, Lynskey MT. The comorbidities of adolescent problem behaviors: A latent class model. J Abnorm Child Psychol. 1994;22:339–354. doi: 10.1007/BF02168078. [DOI] [PubMed] [Google Scholar]
- Gamma A, Jerome L, Liechti ME, Sumnall HR. Is ecstasy perceived to be safe? A critical survey. Drug Alcohol Depend. 2005;77:185–193. doi: 10.1016/j.drugalcdep.2004.08.014. [DOI] [PubMed] [Google Scholar]
- Garrett ES, Zeger SL. Latent class model diagnosis. Biometrics. 2000;56:1055–1067. doi: 10.1111/j.0006-341x.2000.01055.x. [DOI] [PubMed] [Google Scholar]
- Gerra G, Zaimovic A, Ferri M, Zambelli U, Timpano M, Neri E, Marzocchi GF, Delsignore R, Brambilla F. Long-lasting effects of 3,3-methylenedioxymethamphetamine (Ecstasy) on serotonin system function in humans. Biol Psychiatry. 2000;47:127–136. doi: 10.1016/s0006-3223(99)00180-8. [DOI] [PubMed] [Google Scholar]
- Gerra G, Zaimovic A, Giucastro G, Maestri D, Monica C, Sartori R, Caccavari R, Delsignore R. Serotonergic function after (+/−)3,4-methylene-dioxymethamphetamine (‘Ecstasy’) in humans. Int Clin Psychopharmacol. 1998;13:1–9. doi: 10.1097/00004850-199801000-00001. [DOI] [PubMed] [Google Scholar]
- Gold MS, McKewen M. Trends in hallucinogenic drug use: LSD, “ecstasy, ” and the rave phenomenon. Directions in Psychiatry. 1995;15:1–7. [Google Scholar]
- Goodman LA. Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika. 1974;61:215–231. [Google Scholar]
- Gouzoulis-Mayfrank E, Daumann J, Tuchtenhagen F, Pelz S, Becker S, Kunert H-K, Fimm B, Sass H. Impaired cognitive performance in drug free users of recreational ecstasy (MDMA) J Neurol, Neurosurg Psychiatry. 2000;68:719–725. doi: 10.1136/jnnp.68.6.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JD, Scherrer JF, Lyons MJ. Subjective reactions to cocaine and marijuana are associated with abuse and dependence. Addict Behav. 2005;30:1574–1586. doi: 10.1016/j.addbeh.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Greer G. Using MDMA in psychotherapy. Advances. 1985;2:57–62. [Google Scholar]
- Greer G, Tolbert R. The therapeutic use of MDMA. In: Peroutka SJ, editor. Ecstasy: the Clinical, Pharmacological, and Neurotoxicological Effects of the Drug MDMA. Boston: Kluwer Academic Publishers; 1990. pp. 21–36. [Google Scholar]
- Haberman SJ. Vol 2: New developments. New York: Academic Press; 1979. Analysis of quantitative data. [Google Scholar]
- Hagenaars JA. Latent structure models with direct effects between indicators: Local dependence models. Soc. Meth Res. 1988;16:379–405. [Google Scholar]
- Hammersley R, Ditton J, Smith I, Short E. Patterns of ecstasy use by drug users. Brit J Crim. 1999;39:625–647. [Google Scholar]
- Harford TC, Muthén BO. The dimensionality of alcohol abuse and dependence: A multivariate analysis of DSM-IV symptom items in the National Longitudinal Survey of Youth. J. Stud. Alcohol. 2001;62:150–157. doi: 10.15288/jsa.2001.62.150. [DOI] [PubMed] [Google Scholar]
- Hasin D, Paykin A. Dependence symptoms but no diagnosis: Diagnostic ‘orphans’ in a community sample. Drug Alcohol Depend. 1998;50:19–26. doi: 10.1016/s0376-8716(98)00007-6. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. 2nd edition. New York: John Wiley & Sons; 2000. [Google Scholar]
- Jansen KL. Ecstasy (MDMA) dependence. Drug Alcohol Depend. 1998;53:121–124. doi: 10.1016/s0376-8716(98)00111-2. [DOI] [PubMed] [Google Scholar]
- Kalant H. The pharmacology and toxicology of ‘ecstasy’ (MDMA) and related drugs. Canadian Medical Association Journal. 2001;165:917–928. [PMC free article] [PubMed] [Google Scholar]
- Kass R, Raftery AE. Bayes factors. J Amer Stat Assoc. 1995;90:773–795. [Google Scholar]
- Kish SJ. How strong is the evidence that brain serotonin neurons are damaged in human users of ecstasy? Pharmacol Biochem Behav. 2002;71:845–855. doi: 10.1016/s0091-3057(01)00708-0. [DOI] [PubMed] [Google Scholar]
- Kokkevi A, Loukadakis M, Plagianakou S, Politikou K, Stefanis C. Sharp increase in illict drug use in Greece: trends from a general population survey on licit and illicit drug use. Eur. Addict. Res. 2000;8:42–49. doi: 10.1159/000019008. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Rounsaville BJ, Babor TF, Spitzer RL, Williams JB. Substance-use disorders in DSM-III-R: Evidence for the dependence syndrome across different psychoactive substances. Brit J Psych. 1987;151:834–843. doi: 10.1192/bjp.151.6.834. [DOI] [PubMed] [Google Scholar]
- Kotz S, Johnson NL, editors. Encyclopedia of Statistical Sciences. New York: John Wiley & Sons; [Google Scholar]
- Krystal J, Price L. Chronic 3,4-methylenedioxymethamphetamine (MDMA) use: Effects on mood and neuropsychological function? Am J Drug Alcohol Abuse. 1992;18:331–334. doi: 10.3109/00952999209026070. [DOI] [PubMed] [Google Scholar]
- Lenton S, Boys A, Norcross K. Raves, drugs and experience: drug use by a sample of people who attend raves in Western Australia. Addiction. 1997;92:1327–1337. [PubMed] [Google Scholar]
- Lyttle T, Montagne M. Drugs, music and ideology: a social pharmacological interpretation of the Acid House Movement. Int. J. Addict. 1992;27:1159–1177. doi: 10.3109/10826089209047341. [DOI] [PubMed] [Google Scholar]
- MacInnes N, Handley SL, Harding GF. Former chronic methylenedioxymethampetamine (MDMA or ecstasy) users report mild depressive symptoms. J Psychopharmacol. 2001;15:181–186. doi: 10.1177/026988110101500310. [DOI] [PubMed] [Google Scholar]
- McCann UD, Ridenour A, Shaham Y, Ricaurte GA. Serotonin neurotoxicity after (±)3,4-methylenedioxymethamphetamine (MDMA; ”Ecstasy”): A controlled study in humans. Neuropsychopharmacology. 1994;10:129–138. doi: 10.1038/npp.1994.15. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL. Latent Class Analysis. Beverly Hills, CA: Sage Publications; 1987. [Google Scholar]
- McGuire PK, Cope H, Fahy TA. Diversity of psychopathology associated with use of 3,4-methylenedioxymethamphetamine (‘Ecstasy’) Br. J. Psychiatry. 1994;165:391–395. doi: 10.1192/bjp.165.3.391. [DOI] [PubMed] [Google Scholar]
- Merrill J. Ecstasy and neurodegeneration. Br. Med. J. 1996;313:423. doi: 10.1136/bmj.313.7054.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan MJ. Ecstasy (MDMA): A review of its possible persistent psychological effects. Psychopharmacology. 2000;152:230–248. doi: 10.1007/s002130000545. [DOI] [PubMed] [Google Scholar]
- Morgan MJ. Memory deficits associated with recreational use of “ecstasy” (MDMA) Psychopharmacology. 1999;141:30–36. doi: 10.1007/s002130050803. [DOI] [PubMed] [Google Scholar]
- Morgan MJ, McFie L, Fleetwood LH, Robinson JA. Ecstasy (MDMA): Are the psychological problems associated with its use reversed by prolonged abstinence? Psychopharmacology. 2002;159:294–303. doi: 10.1007/s002130100907. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Grant B, Hasin D. The dimensionality of alcohol abuse and dependence: Factor analysis of the DSM-III-R and proposed DSM-IV criteria in the 1988 National Health Interview Survey. Addiction. 1993;88:1079–1090. doi: 10.1111/j.1360-0443.1993.tb02127.x. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Risk behavior assessment. 3rd edition. Rockville: Author; 1993. [Google Scholar]
- Nylund KL, Asparohhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture models: A Monte Carlo simulation study. Structural Equation Modeling. 2007;14:535–569. [Google Scholar]
- Parrott AC. MDMA (3,4-Methylenedioxymethamphetamine) or Ecstasy: The neuropsychobiological implications of taking it at dances and raves. Neuropsychobiology. 2004;50:329–335. doi: 10.1159/000080961. [DOI] [PubMed] [Google Scholar]
- Parrott AC. Recreational Ecstasy/MDMA, the serotonin syndrome, and serotonergic neurotoxicity. Pharmacology, Biochemistry, & Behavior. 2002;71:837–844. doi: 10.1016/s0091-3057(01)00711-0. [DOI] [PubMed] [Google Scholar]
- Parrott AC, Buchanan T, Scholey AB, Heffernan T, Ling J, Rodgers J. Ecstasy/MDMA attributed problems reported by novice, moderate and heavy recreational users. Hum Psychopharmacol. 2002;17:309–312. doi: 10.1002/hup.415. [DOI] [PubMed] [Google Scholar]
- Parrott AC, Lasky J. Ecstasy (MDMA) effects upon mood and cognition: Before, during, and after a Saturday night dance. Psychopharmacol. 1998;139:261–268. doi: 10.1007/s002130050714. [DOI] [PubMed] [Google Scholar]
- Parrott AC, Lees A, Garnham NJ, Jones M, Wesnes K. Cognitive performance in recreational users of MDMA of ‘Ecstasy’: Evidence for memory deficits. J Psychopharmacol. 1998;12:79–83. doi: 10.1177/026988119801200110. [DOI] [PubMed] [Google Scholar]
- Parrott AC, Sisk E, Turner JJ. Psychobiological problems in heavy “ecstasy” (MDMA) polydrug users. Drug Alcohol Depend. 2000;60:105–110. doi: 10.1016/s0376-8716(99)00146-5. [DOI] [PubMed] [Google Scholar]
- Pederson W, Skrondal A. Ecstasy and new patterns of drug use: a normal population study. Addiction. 1999;94:1695–1706. doi: 10.1046/j.1360-0443.1999.941116957.x. [DOI] [PubMed] [Google Scholar]
- Petrides A, Sherlock K. How much ecstasy do the British really take? Mixmag. 1996 July [Google Scholar]
- Pollack NK, Martin CS. Diagnostic orphans: Adolescents with alcohol symptoms who do not qualify for DSM-IV Abuse or dependence diagnoses. Am. J. Psych. 1999;156:897–901. doi: 10.1176/ajp.156.6.897. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reboussin BA, Anthony JC. Is there epidemiological evidence to support the idea that a cocaine dependence syndrome emerges soon after onset of cocaine use? Neuropsychopharmacol. 2006:1–10. doi: 10.1038/sj.npp.1301037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers J. Cognitive performance amongst recreational users of “ecstasy.”. Psychopharmacol. 2000;151:19–24. doi: 10.1007/s002130000467. [DOI] [PubMed] [Google Scholar]
- Roeder K, Lynch KG, Nagin DS. Modeling uncertainty in latent class membership: A case study in criminology. J Amer Stat Assoc. 1999;94:766–776. [Google Scholar]
- Roiser JP, Sahakian BJ. Relationship between ecstasy use and depression: A study controlling for poly-drug use. Psychopharmacol. 2004;173:411–417. doi: 10.1007/s00213-003-1705-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rounsaville BJ, Spitzer RL, Williams JBW. Proposed changes in DSM-III substance use disorders: Description and rationale. Am J Psychiatry. 1986;143:463–468. doi: 10.1176/ajp.143.4.463. [DOI] [PubMed] [Google Scholar]
- Sarr M, Bucholz KK, Phelps DL. Using cluster analysis of alcohol use disorders to investigate ‘diagnostic orphans’: Subjects with alcohol dependence symptoms but no diagnosis. Drug Alcohol Depend. 2000;60:295–302. doi: 10.1016/s0376-8716(00)00118-6. [DOI] [PubMed] [Google Scholar]
- Schifano F, Di Furia L, Forza G, Minicuci N, Bricolo R. MDMA (“ecstasy”) consumption in the context of polydrug abuse: A report on 150 patients. Drug Alcohol Depend. 1998;52:85–90. doi: 10.1016/s0376-8716(98)00051-9. [DOI] [PubMed] [Google Scholar]
- Scholey AB, Parrott AC, Buchanan T, Heffernan TM, Ling J, Rodgers J. Increased intensity of Ecstasy and polydrug usage in the more experienced recreational Ecstasy/MDMA users: A WWW study. Addict Behav. 2004;29:743–752. doi: 10.1016/j.addbeh.2004.02.022. [DOI] [PubMed] [Google Scholar]
- Schwartz RH, Miller NS. MDMA (Ecstasy) and the rave: a review. Pediatrics. 1997;100:705–708. doi: 10.1542/peds.100.4.705. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Spitzer RL, Williams JBW, Skodol AE. DSM-III: The major achievements and an overview. Am J Psychiatry. 1980;137:151–164. doi: 10.1176/ajp.137.2.151. [DOI] [PubMed] [Google Scholar]
- Strassman RJ. Hallucinogenic drugs in psychiatric research and treatment. J Nerv Ment Dis. 1995;183:127–138. doi: 10.1097/00005053-199503000-00002. [DOI] [PubMed] [Google Scholar]
- Strote J, Lee JE, Wechsler H. Increasing MDMA use among college students: Results of a national survey. J Adol Health. 2002;30:64–72. doi: 10.1016/s1054-139x(01)00315-9. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National Findings (Office of Applied Studies, NSDUH Series H-32, DHHS Publication No. SMA 07-4293) Rockville, Maryland: 2007. [Google Scholar]
- Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the National Comorbidity Survey. Am J Psychiatry. 1998;155:1398–1406. doi: 10.1176/ajp.155.10.1398. [DOI] [PubMed] [Google Scholar]
- Topp L, Barker B, Degehardt L. The external validity of results derived from ecstasy users recruited using purposive sampling strategies. Drug Alcohol Depend. 2004;73:33–40. doi: 10.1016/j.drugalcdep.2003.09.001. [DOI] [PubMed] [Google Scholar]
- Topp L, Hando J, Dillon P, Roche A, Solowij N. Ecstasy use in Australia: Patterns of use and associated harm. Drug Alcohol Depend. 1999;55:105–115. doi: 10.1016/s0376-8716(99)00002-2. [DOI] [PubMed] [Google Scholar]
- Uebersax JS. Latent class analysis of substance abuse patterns. In: Collins L, Seitz L, editors. Advances in Data Analysis for Prevention Intervention Research. NIDA Research Monograph 142. Rockville, MD: National Institute on Drug Abuse; 1994. pp. 64–80. [PubMed] [Google Scholar]
- Vollenweider FX, Gamma A, Liechti M, Huber T. Psychological and cardiovascular effects and short-term sequelae of MDMA (“Ecstasy”) in MDMA-naïve healthy volunteers. Neuropsychopharmacol. 1998;19:241–251. doi: 10.1016/S0893-133X(98)00013-X. [DOI] [PubMed] [Google Scholar]
- Von Sydow K, Lieb R, Pfister H, Höfler M, Wittchen H-U. Use, abuse and dependence of ecstasy and related drugs in adolescents and young adults—a transient phenomenon? Results from a longitudinal community study. Drug Alcohol Depend. 2002;66:147–159. doi: 10.1016/s0376-8716(01)00195-8. [DOI] [PubMed] [Google Scholar]
- Walsh H. My first love-Clubbing, house music, and ecstasy. Observer Music Magazine. 2004;6:22–27. [Google Scholar]
- Wier E. Raves: a review of the culture, the drugs and the prevention of harm. Canadian Medical Association Journal. 2000;162:1843–1848. [PMC free article] [PubMed] [Google Scholar]
- Winstock AR, Griffiths P, Stewart D. Drugs and the dance music scene: A survey of current drug use patterns among a sample of dance music enthusiasts in the UK. Drug Alcohol Depend. 2001;64:9–17. doi: 10.1016/s0376-8716(00)00215-5. [DOI] [PubMed] [Google Scholar]
- Yacoubian GS. Assessing the temporal relationship between race and ecstasy use among high school seniors. J Drug Educ. 2002;32:213–225. doi: 10.2190/EXJE-K8Y4-80DH-RYV6. [DOI] [PubMed] [Google Scholar]
- Yacoubian GS, Miller S, Pianim S, Kunz M, Orrick E, Link T, Palacios WR, Peters RJ. Toward an ecstasy and other club drug (EOCD) prevention intervention for rave attendees. J Drug Educ. 2004;34:41–59. doi: 10.2190/QQCT-61H5-CL3F-FVQ3. [DOI] [PubMed] [Google Scholar]