Abstract
Background
While many factors can influence the way that cancer care is delivered, including the way that evidence is packaged and disseminated, little research has evaluated how health care professionals who manage cancer patients seek and use this information to identify whether and how this could be supported. Through interviews we identified that general surgeons experience challenges in coordinating care for complex cancer patients whose management is not easily addressed by guidelines, and conducted a population-based survey of general surgeon information needs and information seeking practices to extend these findings.
Methods
General surgeons with privileges at acute care hospitals in Ontario, Canada were mailed a questionnaire to solicit information needs (task, importance), information seeking (source, frequency of and reasons for use), key challenges and suggested solutions. Non-responders received up to three reminder packages. Significant differences among sub-groups (age, setting) were examined statistically (Kruskal Wallis, Mann Whitney, Chi Square). Standard qualitative methods were used to thematically analyze open-ended responses.
Results
The response rate was 44.2% (170/385) representing all 14 health regions. System resource constraints (60.4%), comorbidities (56.4%) and physiologic factors (51.8%) were top-ranked issues creating information needs. Local surgical colleagues (84.6%), other local colleagues (82.2%) and the Internet (81.1%) were top-ranked sources of information, primarily due to familiarity and speed of access. No resources were considered to be highly applicable to patient care. Challenges were related to limitations in diagnostics and staging, operative resources, and systems to support multidisciplinary care, together accounting for 76.0% of all reported issues. Findings did not differ significantly by surgeon age or setting of care.
Conclusion
General surgeons appear to use a wide range of information resources but they may not address the complex needs of many cancer patients. Decision-making is challenged by informational and logistical issues related to the coordination of multidisciplinary care. This suggests that limitations in system capacity may, in part, contribute to variable guideline compliance. Further research is required to evaluate the appropriateness of information seeking, and both concurrent and consecutive mechanisms by which to achieve multidisciplinary care.
Background
Cancer is a leading cause of premature death in many countries, but medical knowledge is thought to be sufficiently advanced such that one third of cancers could be prevented, a further one-third cured given early diagnosis, and the remainder effectively treated if management consistently complied with existing evidence-based standards [1]. Population-based studies from Canada, Australia and the United States have demonstrated that practice often differs from guidelines for cancer [2-8]. While many organizational and system-level factors can influence the way that cancer care is delivered, including the way that evidence is packaged and disseminated, little research has evaluated how health care professionals who manage cancer patients seek and use this information to identify whether and how this could be supported [9-16].
Research on information seeking among general practitioners found that family physicians seeing 25 patients in a typical day of outpatient care may have 15 clinical questions, but many are either not pursued or answers are not found [17-22]. Barriers to successful information seeking include limited insight on gaps in knowledge or skill, time constraints, access to information resources, searching ability, perceived attributes of the information sources, critical appraisal skills, and evidence that is incomplete, contradictory, or not applicable to individual patients [23-28]. It is not known whether search strategies that increase the sensitivity and specificity of retrieving clinically relevant research articles from literature databases, or journals that provide evidence synopses are used by health care providers [29,30]. A systematic review of 19 studies reported that the information sources used most often by general practitioners were textbooks such as physician desk references due to ease of access, and asking colleagues who can provide tacit, experiential knowledge to overcome organizational demands and constraints [31,32].
General surgeons care for a considerable proportion of patients with cancer, providing diagnosis, surgical treatment, and follow-up monitoring, and function as a critical link between patients and other cancer experts such as radiation and medical oncologists, and surgical sub-specialists. Thus it is important to investigate and optimize resources and processes associated with evidence seeking and utilization among general surgeons. As generalists who provide services for a wide range of conditions in both community and academic settings, their information seeking and utilization patterns may be similar to those of family physicians, but different from specialist surgeons who practice primarily in academic settings with greater access to human, information and technologic resources. A single identified study on information seeking by surgeons reported that they most often consult colleagues over other sources [31]. Through a series of interviews with community-based general surgeons we learned that they deal with very complex patient management issues which are not easily addressed by research evidence, and have few formal or informal opportunities for collegial interaction either within or outside of their organizations to discuss patient management issues [33]. In particular, lack of human and technical resources, and of organizational mechanisms to support multidisciplinary interaction needed for decision-making impeded information seeking and application, and the impact of quality improvement efforts [34,35].
To confirm and elaborate on these exploratory findings we surveyed general surgeons in the population from which interview participants were selected. Specifically, we collected data on the information resources that general surgeons use to address cancer-related questions, the factors that influence and challenge information seeking and use associated with cancer patient care, and the resources or strategies that they believe would address these challenges.
Methods
Approach
A survey strategy based on standard descriptive research methods was used to explore factors influencing information seeking and utilization among general surgeons in Ontario, Canada, and suggested improvements [36]. This involved quantitative and qualitative analysis of responses to closed and open questions in a mailed, cross-sectional questionnaire. Despite the fact that physicians are known to under-report information needs and over-report information utilization [37], this approach was considered appropriate as a preliminary step to explore the relative contribution, and interaction of system infrastructure with individual behaviour, and identify potential solutions that could be evaluated in future research. Ethical approval for this study was granted by Sunnybrook Health Sciences Centre.
Sampling
Contact information for general surgeons was obtained from the Canadian Medical Directory (n = 728). Eligible surgeons included practicing surgeons with privileges at community and academic acute care hospitals in Ontario, Canada and a primary specialty of general surgery not affiliated with our research group (-52). Surgeons were excluded if they possessed a sub-specialty suggestive of limited cancer management such as cardiac, head and neck, thoracic, trauma, urologic, or vascular surgery or endoscopy practice (-232), or responded that they did not treat cancer patients (-59). A total of 385 general surgeons were considered eligible.
Data collection
Based on research describing health professional information seeking and utilization [38], a questionnaire was developed to elicit information on information need (type of cancer, task/issue, question importance), information seeking (source, frequency of use), and reasons for use (familiarity, prior success, speed of access, applicability to patients); individual attributes (sex, age, academic or community setting) and organizational or system features (resource availability, important/common challenges to delivering care), and suggested strategies for supporting cancer care delivery (See Additional file 1). Most questions were closed with nominal (two or more categories) or ordinal response options (five-point scale). All closed questions allowed respondents to add, and rate additional relevant items not already listed. Questions about most common problems faced when caring for cancer patients and the resources or strategies to address each were open-ended.
The questionnaire was not tested for psychometric properties because the purpose of this survey was exploratory and descriptive, and not analytic. However, the questionnaire was pilot-tested for face validity with four general surgeons who were subsequently not surveyed. They were asked to complete the questionnaire and provide feedback on format, clarity and meaning of questions, instructions and response options. Their suggestions were all incorporated in the questionnaire, which was then reviewed for the same issues by all co-investigators, who suggested further minor modifications to wording and response options.
Based on research evidence for increasing survey response rates, the questionnaire was mailed with an addressed, stamped return envelope, and a personalized cover letter identifying academic affiliation of the researchers, and endorsement by both the Ontario agency overseeing cancer services, and the Ontario professional association for general surgeons; a second package was mailed after two weeks to non-responders; and a third package was mailed to non-responders after another two-week period [39,40]. The names of those returning a completed survey were entered into a draw for a $1000 gift certificate. Initial distribution took place on March 26, 2007 and the third reminder package was distributed on May 1, 2007.
Data analysis
Survey responses were entered by one individual into an Access database with validation rules to minimize data entry errors. Double data entry was performed by a second individual by entering a random sample of 10% of the surveys into a replicated Access database. The two databases were compared and no consistent errors were noted. Statistically significant differences in characteristics (sex, age, setting) between responders and non-responders were calculated with the chi square test. Questionnaire responses were analyzed for the entire group using summary statistics (frequency, proportion). Statistical significance of differences among sub-groups (age, setting) was established with the Kruskal Wallis test or Mann Whitney U test for information need and resources used, and with the chi square test for information seeking and reasons that particular resources were used. Chi square was reported with a continuity correction for categories where counts were fewer than five. Age was categorical for the Kruskal Wallis test (30–39, 40–49, 50–59, 60+) and nominal for the chi square test (<50, ≥ 50) to optimize cell counts. All statistical analyses were performed in SPSS 16.0.
Open-ended responses were examined thematically using standard qualitative analysis methods and a grounded approach, meaning ideas were inductively extracted from the responses [41,42]. This involved repeated reading to identify key themes, developing of codes to reflect themes, applying thematic codes to all relevant responses, and grouping of responses by theme. Several strategies were employed for sampling (population-based, identification of limitations), analysis (data examined independently by three individuals) and interpretation (reporting of findings with anonymous identifier codes to illustrate both congruent and divergent themes, comparison of findings with other research) to enhance the reliability and validity of these findings.
Results
Respondents
The overall response rate was 44.2% (170/385). Responses were received from all 14 health regions ranging from 16.1% (5/31) to 77.8% (7/9). Responders included a higher proportion of surgeons in academic settings compared with non-responders (p = 0.024). There were no significant differences between responders and non-responders by sex or year from graduation (Table 1). Respondents are involved in breast and colorectal cancer surgery primarily. They reported the following proportion of practice devoted to breast cancer: less than 10% (50.0%), 10–25% (27.6%), 26–50% (14.1%), and more than 51% (8.2%) and colorectal cancer: less than 10% (31.8%), 10–25% (41.8%), 26–50% (14.7%), and more than 51% (11.8%). While there was no significant difference in the range of proportion of practice devoted to colorectal cancer surgery by setting (p = 0.912), significantly more surgeons in community settings manage lower volumes of breast cancer (up to 25% of practice) (p < 0.001). The majority of surgeons reported that less than 10% of their practice was devoted to gastric (92.9%), melanoma (92.4%) or hepatopancreatobiliary cancer (89.4%).
Table 1.
Comparison of responders to non-responders
| Subgroup | Eligible | Responders | % | Nonresponders | % | p-value |
| Sex | ||||||
| male | 332 | 141 | 42.47 | 191 | 57.53 | 0.129 |
| female | 53 | 29 | 54.72 | 24 | 45.28 | |
| Graduation | ||||||
| ≤ 1979 | 134 | 54 | 40.30 | 80 | 59.70 | 0.114 |
| 1980–1989 | 114 | 60 | 52.63 | 54 | 47.37 | |
| ≥ 1990 | 137 | 56 | 40.88 | 81 | 59.12 | |
| Setting | ||||||
| academic | 112 | 59 | 52.68 | 53 | 47.32 | 0.024 |
| community | 273 | 111 | 40.66 | 162 | 59.34 | |
| Health region | ||||||
| 1 | 19 | 7 | 36.84 | 12 | 63.16 | 0.022 |
| 2 | 37 | 18 | 48.65 | 19 | 51.35 | |
| 3 | 14 | 10 | 71.43 | 4 | 28.57 | |
| 4 | 50 | 21 | 42.00 | 29 | 58.00 | |
| 5 | 9 | 7 | 77.78 | 2 | 22.22 | |
| 6 | 29 | 11 | 37.93 | 18 | 62.07 | |
| 7 | 61 | 33 | 54.10 | 28 | 45.90 | |
| 8 | 26 | 12 | 46.15 | 14 | 53.85 | |
| 9 | 39 | 21 | 53.85 | 18 | 46.15 | |
| 10 | 17 | 8 | 47.06 | 9 | 52.94 | |
| 11 | 31 | 5 | 16.13 | 26 | 83.87 | |
| 12 | 15 | 5 | 33.33 | 10 | 66.67 | |
| 13 | 27 | 9 | 33.33 | 18 | 66.67 | |
| 14 | 11 | 3 | 27.27 | 8 | 72.73 | |
| Total | 385 | 170 | 215 | |||
Information needs
The three top-ranked tasks or issues giving rise to at least some uncertainty (Table 2) when managing cancer patients were human and technologic resource constraints (60.4%), comorbid conditions (56.4%) and other patient factors such as age and physiology (51.8%). In contrast, the top-ranked clinical tasks giving rise to uncertainty that would reportedly trigger information seeking were chemotherapy or radiotherapy treatment (92.4%), pathology (92.9%), and surgical approach or technique (87.4%), followed closely by lack of or conflicting evidence (86.5%) and tumour stage (84.4%). These views did not differ significantly by age or setting of care.
Table 2.
Factors contributing to information needs and information seeking
| Factor | Degree of uncertainty | Uncertainty triggers information seeking | ||
| N | % | N | % | |
| Resource availability (human/technologic) | 99 | 60.4 | 111 | 73.0 |
| Comorbid conditions | 93 | 56.4 | 122 | 77.7 |
| Patient factors such as age or physiology | 86 | 51.8 | 107 | 68.6 |
| Evidence, unaware, lacking or conflicting | 74 | 45.7 | 134 | 86.5 |
| Tumour stage | 64 | 38.6 | 130 | 84.4 |
| Patient safety | 60 | 36.8 | 113 | 73.9 |
| Chemotherapy or radiotherapy | 59 | 35.8 | 146 | 92.4 |
| Patient preferences | 56 | 33.7 | 88 | 58.3 |
| Ethical issues | 42 | 25.8 | 105 | 68.6 |
| Pathology | 40 | 23.8 | 145 | 92.9 |
| Legal issues | 35 | 21.2 | 104 | 68.9 |
| Surgery | 21 | 12.7 | 132 | 87.4 |
Information seeking
The three sources of information used by surgeons most frequently when faced with clinical uncertainty (Table 3) were local surgical colleagues (84.6%), other local colleagues (82.2%), and the Internet (81.1%), followed closely by office journals (77.6%). This did not differ significantly by age or setting of care. Surgeons in community settings were more likely to phone (p = 0.007), or refer to external specialists (p = 0.018). A larger proportion of community surgeons reported never taking part in intra- or inter-departmental meetings, or cancer conferences. Those that did were more likely to attend on a monthly basis compared with surgeons in academic settings who reported higher rates of weekly participation (p < 0.001).
Table 3.
Sources used during information seeking
| Source | Frequency of use | |
| N | % | |
| Local colleague, surgeon | 143 | 84.6 |
| Local colleague, clinician | 139 | 82.2 |
| Internet (journals, guidelines) | 137 | 81.1 |
| Journal in office | 128 | 77.6 |
| Intradepartment meeting | 119* | 70.4 |
| Textbook in office | 100 | 59.9 |
| Interdepartment meeting | 99* | 59.3 |
| Cancer conferences (local, regional) | 86* | 50.9 |
| Refer to external specialist | 70* | 41.9 |
| Phone external specialist | 68* | 40.5 |
| Hospital library | 63 | 37.7 |
| Computer decision aid | 37 | 22.7 |
| Librarian | 19 | 11.6 |
* p < 0.05 by Mann Whitney U test two-tail significance for setting of care
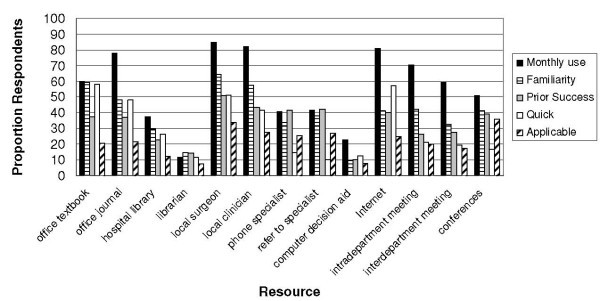
When asked to select the reasons for using various sources of information (Table 4), local surgical (64.7%) and other colleagues (57.6%) and office textbooks (59.4%) and journals (48.2%) were ranked most familiar; local surgical (50.6%) and other colleagues (43.5%) and either phone calls (41.8%) or referrals to external specialists (42.4%) were highest ranked for prior success; the Internet, defined as any resource providing access to evidence such as journals or guidelines (57.1%), local surgical colleagues (51.2%), and office textbooks (58.2%) or journals (48.2%) offered speediest access to cancer-related information; and cancer conferences (35.9%) and local surgical colleagues (34.1%) provided information considered to be the most applicable to patient care. Older surgeons more often used the hospital library (p = 0.042) or interdepartmental meetings (p = 0.011) due to familiarity, and fewer considered office journals to be applicable (p = 0.046) compared with younger surgeons. Community-based surgeons more often chose to refer to external specialists (p = 0.003) or consult computer decision aids (p = 0.009) based on prior success. Academic surgeons most often used interdepartmental meetings for this reason (p = 0.017). Speedy access prompted more academic surgeons to consult office journals (p = 0.009) while community surgeons more often reported applicability as the reason for using office textbooks (p = 0.044).
Table 4.
Reasons for use of information resources
| Source | Reasons for use | |||||||
| Familiar | Prior success | Quick access | Most applicable | |||||
| N | % | N | % | N | % | N | % | |
| Textbook in office | 101 | 59.4 | 64 | 37.6 | 99* | 58.2 | 35 | 20.6 |
| Journal in office | 82 | 48.2 | 63 | 37.1 | 82** | 48.2 | 37 | 21.8 |
| Hospital library | 50* | 29.4 | 39 | 22.9 | 45 | 26.5 | 21 | 12.4 |
| Librarian | 25 | 14.7 | 24 | 14.1 | 20 | 11.8 | 13 | 7.6 |
| Local colleague, surgeon | 110 | 64.7 | 86 | 50.6 | 87 | 51.2 | 58 | 34.1 |
| Local colleague, clinician | 98 | 57.6 | 74 | 43.5 | 71 | 41.8 | 47 | 27.6 |
| Phone external specialist | 58 | 34.1 | 71 | 41.8 | 25 | 14.7 | 43 | 25.3 |
| Refer to external specialist | 65 | 38.2 | 72** | 42.4 | 17 | 10.0 | 46 | 27.1 |
| Computer decision aid | 16 | 9.4 | 17** | 10.0 | 22 | 12.9 | 14 | 8.2 |
| Internet (journals, guidelines) | 70 | 41.2 | 68 | 40.0 | 97 | 57.1 | 42 | 24.7 |
| Intradepartment meeting | 72 | 42.4 | 45 | 26.5 | 36* | 21.2 | 34 | 20.0 |
| Interdepartment meeting | 56* | 32.9 | 47** | 27.6 | 33 | 19.4 | 30 | 17.6 |
| Conferences (local, regional) | 70 | 41.2 | 67 | 39.4 | 29 | 17.1 | 61 | 35.9 |
* p < 0.05 by Chi square test two-tail significance for age.
** p < 0.05 by Chi square test two-tail significance for setting of care
Sources of information used at least monthly were considered according to reasons for use (Figure 1). The single resource used most frequently by the majority of respondents, local surgical colleagues, was ranked highly for each of familiarity, prior success, speedy access and applicability to patients. Familiarity and prior success contribute to use of the second most frequently used resource, other local colleagues. The third most used resource, the Internet, was viewed as readily accessible. Notably, most resources were not considered by the majority of surgeons to provide information that was applicable to cancer patient care, including local surgical colleagues, thought by 34.1% of respondents to provide relevant information, despite being the most frequently consulted resource.
Figure 1.
Reported use and reasons for use of information resources.
Cancer management challenges
In response to an open-ended question, 74% (126/170) of respondents listed up to three important concerns faced when caring for cancer patients, and suggested solutions (Table 5). These were organized into eight thematic categories. The majority of comments were related to barriers to diagnosing and staging cancer, lack of operative resources, and barriers to coordinating multidisciplinary care. Together these accounted for 76.0% (204/268) of all reported issues. Increased funding for resources was the most frequently mentioned solution for these concerns (82/167, 49.1%). The availability of evidence to support cancer care decision making was named by 19 individuals (19/268, 7.1%). Greater production of guidelines was recommended as a possible solution by four individuals. Thus information seeking and utilization was not viewed as an important challenge compared with limitations in system infrastructure and communication with colleagues to coordinate care delivery.
Table 5.
Cancer care concerns and suggested solutions
| Concerns (n, % respondents) |
Issues (n respondents) |
Suggested solutions (n respondents) |
| Barriers to diagnosing and staging cancer (82, 30.6) | CT/MRI/ERUS (22) Endoscopy (21) Core biopsy/breast imaging (19) Access to/timely radiology (17) Referral by family physicians (3) |
Funding for more resources (33) Establish and monitor benchmarks (6) Prioritize cancer cases (5) Centralized workup facility (4) Improved coordination (3) Patient education (1) Privatize (1) Colorectal cancer screening program (1) |
| Lack of operative resources (67, 25.0) | OR time (53) Lack of surgical beds (5) Nuclear medicine/equipment for SLNB (4) Anesthesia shortage (2) Lack of nurses (1) Old laparoscopic equipment (1) Surgery assistants (1) |
Funding for more resources (24) Prioritize cancer cases (11) Lobby/increase public awareness (2) Weekend operating time (1) Privatize (1) Create non-hospital surgical centres (1) Clinical model (refer to group) (1) |
| Barriers to coordinating multidisciplinary care (55, 20.0) | Coordination of care (23) Referral to specialists (16) Proximity to cancer specialists (6) Challenge of participating in tumor boards (6) Patient retention at large centres (2) Challenges of organizing clinical trials (2) |
Regional integration/coordination services (7) Funding for more specialists (5) Oncology electronic medical record (5) Communication to referring offices (5) Radiation oncologist visits satellite clinic (3) Open new radiation facilities (3) Organized implementation tumor boards (3) List of available specialists (2) Patient-centred care pathway (1) |
| Lack of data to guide care delivery (20, 7.5) | Lack of/applicability of evidence (19) Timely performance measurement (1) |
Patient-specific guidelines (4) Funding for more resources (3) Tumor boards (2) Develop cancer-specific programs (2) |
| Access to pathology (15, 5.6) | Delayed pathology (15) | Funding for more resources (8) Establish and monitor benchmarks (1) |
| Need for patient support resources (12, 4.5) | Navigation (5) Information (5) Shared decision making tools (2) |
Funding for the development of information resources (5) |
| Heavy workload (10, 3.7) | Overwhelmed (9) Patients with no family physician (1) |
Nurse practitioners/GP oncologists (5) Funding for more surgeons (4) Prioritize cancer patient access to family physicians (1) |
| Need for opportunities to develop skills (7, 2.6) | Training for practicing surgeons (7) | Increase mentorship opportunities (3) |
CT computed tomography scan; MRI magnetic resonance imaging; ERUS endorectal ultrasound; SLNB sentinel lymph node biopsy
Discussion
The overall objective of this research was to understand how general surgeons could be better supported to undertake decision making for patients with cancer. In previous exploratory work we learned that general surgeons care for patients with complex cancer problems [33]. This population-based survey confirms that general surgeons experience clinical uncertainty at an informational level due to the complexity of care required for cancer patients who have comorbid conditions and other physiologic factors that confound management. Since these uncertainties may not be directly addressed by searching for available research evidence, respondents most often turn to local surgical colleagues, as was found to be the case among family physicians [31,32]. Perhaps because research on information seeking and utilization by family physicians was conducted in the 1980s and 1990s when the Internet was not widely available, in contrast to family physicians, general surgeons appear to frequently use the Internet [17-22,37]. These findings were similar for surgeons of younger and older age, and practicing in both community and academic settings. Surgeons also experience clinical dilemmas at a logistical level related to human and technologic constraints in the health care sector that challenge the appropriate and coordinated care of complex cancer cases. Community-based surgeons reported no, or limited interaction with colleagues for the discussion of patient care issues, and frequently refer patients to other centres for diagnostic, surgical and oncologic services. This was also identified in our previous study [33].
While surgeons consulted the Internet and colleagues, neither was considered highly applicable to the expressed informational and logistical decision-making needs associated with complex management issues. Among a population-based sample of 15,626 American patients with cancer, 68.7% had comorbidity, and 32.6% had two or more comorbid conditions [43]. These rates were higher in the elderly, smokers and those with lower socioeconomic status. Hence, the complexity of decision-making for a considerable number of cancer patients might not be entirely solved by either developing more guidelines, or providing surgeons with informatics training or tools since available evidence may not be applicable to individual patients with complex indications. Instead, qualitative information collected by this survey suggests that better access to, and coordination of multidisciplinary decision-making could address many of the identified informational and logistical problems.
Recommendations of an informational nature included development of a cancer care medical record to provide electronic access to consolidated patient information. Electronic health records may not be prevalent in many settings, nor shared across the different settings that are involved in delivering care to individual patients [44]. Surveys of Canadian and American hospitals found that few have implemented such systems [45,46]. Research investigating the use of patient held records for patients with cancer found that there was a low level of use, perhaps due to lack of agreement between patients and health professionals regarding their function [47-50]. Many respondents highlighted the need for more efficient communication of tests and treatment results to referring surgeons from cancer clinics. Lack of referral reply, delay in receiving the consultant's reply letter, and insufficient detail in reply letters are common concerns expressed by surgeons elsewhere [51]. Content analysis of both referral and reply letters has shown that their quality and comprehensiveness could be improved [51-53]. Communication could be enhanced with the use of structured letter templates that facilitate more consistent inclusion of key patient and educational information to referring doctors [53,54].
Recommendations to address logistical issues such as surgeon interaction with other health care professionals involved in diagnosing, staging or treating cancer patients included development of centralized cancer diagnostic facilities or satellite cancer clinics on a regional basis. We conducted a systematic review of diagnostic assessment units for cancer [55]. While evidence was limited, they appear to reduce time to diagnosis. Another systematic review based on nine studies found that specialist outreach clinics improved access, health outcomes, more efficient and guideline-consistent care, and less use of inpatient services [56]. Several respondents recommended greater use of multidisciplinary cancer conferences (MCCs), or tumour boards [57]. We found that videoconferencing could be used to successfully involve community-based surgeons in MCCs [58], and subsequently evaluated an MCC that regularly engages surgeons affiliated with six community hospitals in one health region, and oncologists from the closest cancer centre [33]. Physicians thought that collegial interaction improved awareness of current evidence, patient satisfaction with treatment plans, appropriate care delivery, and continuity of care. Given that most of our survey respondents were frequent Internet users, further development of this platform to support multidisciplinary consultation and care delivery is warranted since it was used successfully to support MCCs in Germany [59].
The results of this survey are limited by self-report bias inherent in survey methods, and the 44.2% response rate which is lower than the mean response rate of 54% for published surveys of physicians [40,41]. Non-response to surveys is a problem if the respondents differ in a meaningful way from non-respondents. We found no difference between responders and non-responders by sex or graduation date (proxy for age). Although some regions were less well represented than others, for reasons we cannot identify based on this data, we did achieve responses from all 14 health regions, thusly accounting for geographic factors that might impact information seeking. While general surgeons in academic settings were over-represented among respondents, we received information from 59 academic and 111 community surgeons, providing sufficient power to find no statistically significant differences in our key results according to this factor. Hence, we believe that our findings are generalizable to the general surgeon population from which our sample was drawn. They may be less relevant to general surgeons in other jurisdictions where resource constraints and the organization of cancer care services may be different from those in Ontario. Furthermore, we examined perceived informational needs, and not specific patient care decisions made, and their correspondence with evidence of appropriate care. Since physicians are known to under-estimate their need for knowledge [23,37], it may be that current information seeking behaviour among this population inadequately makes use of existing information resources, but this would need to be addressed in further studies. Ongoing research should evaluate the implementation and benefit of various multidisciplinary care models, including concurrent (outreach clinics, centralized diagnostic centres, MCCs, telemedicine, Internet networking) and consecutive (improved referral communication, electronic health records, patient-held medical records) mechanisms to assess their cost-effectiveness.
Conclusion
This study found that, regardless of age or setting of care, general surgeons consult a variety of informational resources, most frequently colleagues, although none are considered to adequately solve clinical uncertainty associated with the complexity of many cancer patients. Decision-making is challenged by both informational and logistical issues related to the coordination of multidisciplinary care. This suggests that limitations in the organization of multidisciplinary care leading to suboptimal exchange of information among involved health care professionals may, in part, contribute to variable compliance with what is considered to be appropriate care according to current guidelines. There are many different mechanisms by which multidisciplinary care can be achieved but none have been comprehensively evaluated. Ongoing research will develop and evaluate mechanisms by which to support peer interaction for routine decision making and continuing professional development.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ARG conceptualized and designed the study, obtained funding, coordinated all aspects, collected and analyzed data, interpreted findings, and prepared the manuscript. FCW, DD, RSM and DRU assisted with design of the study, interpretation of data, and review of the manuscript. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Survey instrument. Questionnaire used to collect data from general surgeons on health professional information seeking and utilization patterns.
Acknowledgments
Acknowledgements
This study was conducted and published with funding from the University of Toronto, Faculty of Medicine Dean's Fund New Staff Grant and an unrestricted research grant from Cancer Care Ontario. Neither source had any influence on the collection, analysis, and interpretation of data; on the writing of the manuscript; and in the decision to submit the manuscript for publication.
Contributor Information
Anna R Gagliardi, Email: anna.gagliardi@sunnybrook.ca.
Frances C Wright, Email: frances.wright@sunnybrook.ca.
Dave Davis, Email: ddavis@aamc.org.
Robin S McLeod, Email: rmcleod@mtsinai.on.ca.
David R Urbach, Email: david.urbach@uhn.on.ca.
References
- World Health Organization Cancer Fact Sheets 297. http://www.who.int/mediacentre/factsheets/fs297/en/index.html accessed March 15, 2007.
- Latosinsky S, Fradette K, Lix L, Hildebrand K, Turner D. Canadian breast cancer guidelines: have they made a difference. Can Med Assoc J. 2007;176:771–776. doi: 10.1503/cmaj.060854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor SE, Hilsden RJ, Li FX, Bryant HE, Murray A. Low uptake of colorectal cancer screening 3 yr after release of national recommendations for screening. Am J Gastroenterol. 2007;102:1727–1735. doi: 10.1111/j.1572-0241.2007.01217.x. [DOI] [PubMed] [Google Scholar]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Malin JL, Schneider EC, Epstein AM, Adams J, Emanuel EJ, Kahn KL. Results of the National Initiative for Cancer Care Quality: how can we improve the quality of cancer care in the United States? J Clin Oncol. 2006;24:626–634. doi: 10.1200/JCO.2005.03.3365. [DOI] [PubMed] [Google Scholar]
- Koshy A, Buckingham JM, Zhang Y, Craft P, Dahlstrom JE, Tait N, Members of the ACT and SE NSW Breast Cancer Treatment Group Surgical management of invasive breast cancer: a 5-year prospective study of treatment in the Australian Capital Territory and South-Eastern New South Wales. ANZ J Surg. 2005;75:757–761. doi: 10.1111/j.1445-2197.2005.03514.x. [DOI] [PubMed] [Google Scholar]
- Barton MB, Gabriel GS, Miles S. Colorectal cancer patterns of care in the Western Sydney and Wentworth Area Health Services. ANZ J Surg. 2004;74:406–412. doi: 10.1111/j.1445-1433.2004.03017.x. [DOI] [PubMed] [Google Scholar]
- Young JM, Leong DC, Armstrong K, O'Connell D, Armstrong BK, Spigelman AD, Ackland S, Chapuis P, Kneebone AB, Solomon MJ. Concordance with national guidelines for colorectal cancer care in New South Wales: a population-based patterns of care study. Med J Aust. 2007;186:292–295. doi: 10.5694/j.1326-5377.2007.tb00903.x. [DOI] [PubMed] [Google Scholar]
- Ellis P, Robinson P, Ciliska D, Armour T, Brouwers M, O'Brien MA, Sussman J, Raina P. A systematic review of studies evaluating diffusion and dissemination of selected cancer control interventions. Health Psychol. 2005;24:488–500. doi: 10.1037/0278-6133.24.5.488. [DOI] [PubMed] [Google Scholar]
- Armstrong R, Waters E, Crockett B, Keleher H. The nature of evidence resources and knowledge translation for health promotion practitioners. Health Promot Int. 2007;22:254–260. doi: 10.1093/heapro/dam017. [DOI] [PubMed] [Google Scholar]
- Cooney A, Gattellari M, Donnelly N, Ward J. Impact of national guidelines about the management of colorectal cancer on Australian surgeons' awareness of evidence. Colorectal Dis. 2004;6:418–427. doi: 10.1111/j.1463-1318.2004.00710.x. [DOI] [PubMed] [Google Scholar]
- Sheldon TA, Cullum N, Dawson D, Lankshear A, Lowson K, Watt I, West P, Wright D, Wright J. What's the evidence that NICE guidance has been implemented? Results from a national evaluation using time series analysis, audit of patients' notes, and interviews. Br Med J. 2004;329:999. doi: 10.1136/bmj.329.7473.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavis JN, Robertson D, Woodside JM, McLeod CB, Abelson J. How can research organizations more effectively transfer research knowledge to decision makers. Milbank Q. 2003;81:221–248. doi: 10.1111/1468-0009.t01-1-00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunfeld E. Canadian breast cancer guidelines are as effective as possible under the circumstances. Can Med Assoc J. 2007;176:785–786. doi: 10.1503/cmaj.070164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, Sam J, Haynes RB. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes. J Am Med Assoc. 2005;293:1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- Dy SM, Garg PP, Nyberg D, Dawson PB, Pronovost PJ, Morlock L, Rubin HR, Diener-West M, Wu AW. Are critical pathways effective for reducing postoperative length of stay. Med Care. 2003;41:637–648. doi: 10.1097/00005650-200305000-00011. [DOI] [PubMed] [Google Scholar]
- Gorman P. Information needs in primary care. Stud Health Technol Inform. 2001;84:338–342. [PubMed] [Google Scholar]
- Curley SP, Connelly DP, Rich EC. Physicians' use of medical knowledge resources: preliminary theoretical framework and findings. Med Decis Making. 1990;10:231–241. doi: 10.1177/0272989X9001000401. [DOI] [PubMed] [Google Scholar]
- McKnight M, Peet M. Health care providers' information seeking: recent research. Med Ref Serv Q. 2000;19:27–50. doi: 10.1300/J115v19n02_03. [DOI] [PubMed] [Google Scholar]
- Verhoeven AA, Boerma EJ, Meyboom-de Jong B. Use of information sources by family physicians: a literature survey. Bull Med Libr Assoc. 1995;83:85–90. [PMC free article] [PubMed] [Google Scholar]
- Haug JD. Physicians' preferences for information sources: a meta-analytic study. Bull Med Libr Assoc. 1997;85:223–232. [PMC free article] [PubMed] [Google Scholar]
- Ely JW, Osheroff JA, Chambliss ML, Ebell MH, Rosenbaum ME. Answering physicians' clinical questions: obstacles and potential solutions. J Am Med Inform Assoc. 2005;12:217–224. doi: 10.1197/jamia.M1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. J Am Med Assoc. 2006;296:1094–1102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]
- Maier RV. What the surgeon of tomorrow needs to know about evidence-based surgery. Arch Surg. 2006;141:317–323. doi: 10.1001/archsurg.141.3.317. [DOI] [PubMed] [Google Scholar]
- Krahn J, Sauerland S, Rixen D, Gregor S, Bouillon B, Neugebauer EA. Applying evidence-based surgery in daily clinical routine: a feasibility study. Arch Orthop Trauma Surg. 2006;126:88–92. doi: 10.1007/s00402-005-0095-0. [DOI] [PubMed] [Google Scholar]
- Scott I, Heyworth R, Fairweather P. The use of evidence-based medicine in the practice of consultant physicians. Results of a questionnaire survey. Aust N Z J Med. 2000;30:319–326. doi: 10.1111/j.1445-5994.2000.tb00832.x. [DOI] [PubMed] [Google Scholar]
- Naylor CD. Grey zones of clinical practice: some limits to evidence-based medicine. Lancet. 1995;345:840–842. doi: 10.1016/S0140-6736(95)92969-X. [DOI] [PubMed] [Google Scholar]
- Petrova M, Dale J, Fulford BK. Values-based practice in primary care: easing the tensions between individual values, ethical principles and best evidence. Br J Gen Pract. 2006;56:703–709. [PMC free article] [PubMed] [Google Scholar]
- Wong SSL, Wilczynski NL, Haynes RB. Comparison of top-performing search strategies for detecting clinically sound treatment studies and systematic reviews in MEDLINE and EMBASE. J Med Libr Assoc. 2006;94:451–455. [PMC free article] [PubMed] [Google Scholar]
- Haynes RB. Of studies, syntheses, synopses, summaries and systems: the "5S" evolution of information services for evidence-based healthcare decisions. Evid Based Med. 2006;11:162–164. doi: 10.1136/ebm.11.6.162-a. [DOI] [PubMed] [Google Scholar]
- Dawes M, Sampson U. Knowledge management in clinical practice: a systematic review of information seeking behaviour. Int J Med Inform. 2003;71:9–15. doi: 10.1016/S1386-5056(03)00023-6. [DOI] [PubMed] [Google Scholar]
- Gabbay J, le May A. Evidence based guidelines or collectively constructed "mindlines"? Ethnographic study of knowledge management in primary care. Br Med J. 2004;329:1013. doi: 10.1136/bmj.329.7473.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagliardi AR, Wright FC, Anderson MA, Davis D. The role of collegial interaction in continuing professional development. J Contin Educ Health Prof. 2007;27:214–219. doi: 10.1002/chp.140. [DOI] [PubMed] [Google Scholar]
- Gagliardi AR, Wright FC, Khalifa MA, Smith AJ. Multiple factors influence compliance with colorectal cancer staging recommendations: an exploratory study. BMC Health Serv Res. 2008;8:34. doi: 10.1186/1472-6963-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govindarajan A, Fraser N, Cranford V, Wirtzfeld D, Gallinger S, Law CH, Smith AJ, Gagliardi AR. Predictors of multivisceral resection in patients with locally advanced colorectal cancer. Ann Surg Oncol. 2008;15:1923–1930. doi: 10.1245/s10434-008-9930-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15:261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- Covell DG, Uman GC, Manning PR. Information needs in office practice: are they being met? Ann Intern Med. 1985;103:596–599. doi: 10.7326/0003-4819-103-4-596. [DOI] [PubMed] [Google Scholar]
- Leckie GJ, Pettigrew KE, Sylvain C. Modeling the information seeking of professionals: a general model derived from research on engineers, health care professionals, and lawyers. Libr Q. 1996;66:161–193. [Google Scholar]
- Asch DA, Jedrziewski K, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/S0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- Edward P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, Kwan I. Increasing response rates to postal questionnaire: systematic review. Br Med J. 2002;324:1183–1192. doi: 10.1136/bmj.324.7347.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach CF, Silverstein LB. Qualitative data: an introduction to coding and analysis. New York: New York University Press; 2003. [Google Scholar]
- Pope C, Ziebland S, Mays N. Analysing qualitative data. Br Med J. 2000;320:114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogle KS, Swanson GM, Woods N, Azzouz F. Cancer and comorbidity: redefining chronic diseases. Cancer. 2000;88:653–663. doi: 10.1002/(SICI)1097-0142(20000201)88:3<653::AID-CNCR24>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- Brazil K, Bainbridge D, Sussman J, Whelan T, O'Brien MA, Pyette N. Providing supportive care to cancer patients: a study on inter-organizational relationships. Int J Integr Care. 2008;8:e01. doi: 10.5334/ijic.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AK, Ferris TG, Donelan K, DesRoches C, Shields A, Rosenbaum S, Blumenthal D. How common are electronic health records in the United States? A summary of the evidence. Health Aff. 2006;25:496–507. doi: 10.1377/hlthaff.25.w496. [DOI] [PubMed] [Google Scholar]
- Nagle LM, Catford P. Toward a model of successful electronic health record adoption. Healthc Q. 2008;11:84–91. [PubMed] [Google Scholar]
- Williams JG, Cheung WY, Chetwynd N, Cohen DR, El-Sharkawi S, Finlay I, Lervy B, Longo M, Malinovszky K. Pragmatic randomized trial to evaluate the use of patient held records for the continuing care of patients with cancer. Qual Health Care. 2001;10:159–165. doi: 10.1136/qhc.0100159... [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecouturier J, Crack L, Mannix K, Hall RH, Bond S. Evaluation of a patient-held record for patients with cancer. Eur J Cancer. 2002;11:114–121. doi: 10.1046/j.1365-2354.2002.00301.x. [DOI] [PubMed] [Google Scholar]
- Gysels M, Richardson A, Higginson IJ. Does the patient-held record improve continuity and related outcomes in cancer care: a systematic review. Health Expect. 2007;10:75–91. doi: 10.1111/j.1369-7625.2006.00415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urowitz S, Wiljer D, Apatu E, Eysenbach G, Delenardo C, Harth T, Pai H, Leonard KJ. Is Canada ready for patient accessible electronic health records? A national scan. BMC Med Inform Decis Mak. 2008;8:33. doi: 10.1186/1472-6947-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell D, Butow PN, Tattersall MH. Improving the letters we write: an exploration of doctor-doctor communication in cancer care. Br J Cancer. 1999;80:427–437. doi: 10.1038/sj.bjc.6690374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grol R, Rooijackers-Lemmers N, van Kaathoven L, Wollersheim H, Mokkink H. Communication at the interface: do better referral letters produce better consultant replies. Br J Gen Pract. 2003;53:217–219. [PMC free article] [PubMed] [Google Scholar]
- Scott IA, Mitchell CA, Logan E. Audit of consultant physicians' reply letters for referrals to clinics in a tertiary teaching hospital. Intern Med J. 2004;34:31–37. doi: 10.1111/j.1444-0903.2004.00424.x. [DOI] [PubMed] [Google Scholar]
- Gagliardi A. Use of referral reply letters for continuing medical education: a review. J Contin Educ Health Prof. 2002;22:222–229. doi: 10.1002/chp.1340220406. [DOI] [PubMed] [Google Scholar]
- Gagliardi A, Grunfeld E, Evanx WK. Diagnostic assessment units. J Clin Oncol. 2004;22:1126–1135. doi: 10.1200/JCO.2004.06.057. [DOI] [PubMed] [Google Scholar]
- Gruen RL, Weeramanthri TS, Knight SE, Bailie RS. Specialist outreach clinics in primary care and rural hospital settings. Cochrane Database Syst Rev. 2004;1:CD003798. doi: 10.1002/14651858.CD003798.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright FC, DeVito C, Langer B, Hunter A, the Expert Panel on Multidisciplinary Cancer Conference Standards Multidisciplinary cancer conferences : a systematic review and development of practice standards. Eur J Cancer. 2007;43:1002–1010. doi: 10.1016/j.ejca.2007.01.025. [DOI] [PubMed] [Google Scholar]
- Gagliardi AR, Smith A, Goel V, DePetrillo D. Feasibility study of multidisciplinary oncology rounds by videoconference for surgeons in remote locales. BMC Med Inform Dec Mak. 2003;3:7. doi: 10.1186/1472-6947-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chekerov R, Denkert C, Boehmer D, Suesse A, Widing A, Ruhmland B, Giese A, Mustea A, Lichtenegger W, Sehouli J. Online tumor conference in the clinical management of gynecological cancer. Int J Gynecol Cancer. 2008;18:1–7. doi: 10.1111/j.1525-1438.2007.01096.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Survey instrument. Questionnaire used to collect data from general surgeons on health professional information seeking and utilization patterns.