Abstract
Acute demyelinating optic neuritis in children can occur in isolation or be associated with acute disseminated encephalomyelitis, multiple sclerosis or neuromyelitis optica. Clinical features, neuroimaging, cerebrospinal fluid findings and long term prognosis were reviewed in 26 children diagnosed with optic neuritis at the first presentation of demyelinating disease. The risk factors for the subsequent diagnosis of multiple sclerosis were analyzed. The mean duration of follow-up was 6.2 years. To date, six children have been diagnosed with multiple sclerosis (23 %). An abnormal brain magnetic resonance imaging (MRI), older age, oligoclonal bands in cerebrospinal fluid and elevated immunoglobulin G index were associated with multiple sclerosis outcome. Children with monosymptomatic optic neuritis and an abnormal brain MRI had a higher risk for multiple sclerosis. These children should be monitored closely for the subsequent diagnosis of multiple sclerosis and can be considered for early preventive therapy.
Keywords: Optic neuritis, pediatric multiple sclerosis, acute disseminated encephalomyelitis, demyelinating disorders
INTRODUCTION
Optic neuritis is an inflammatory disorder of the optic nerve often presenting with periorbital or supraorbital pain, decreased visual acuity and decreased color vision. Differential diagnoses include various infectious and autoimmune disorders. Demyelinating optic neuritis can present as isolated optic neuritis with no lesions elsewhere in the central nervous system or can be associated with acute disseminated encephalomyelitis, multiple sclerosis or neuromyelitis optica. In adults, isolated optic neuritis is frequently the heralding syndrome of multiple sclerosis1. The subsequent diagnosis of multiple sclerosis is reported in 19–42 % of children with optic neuritis2–5.
METHODS
Clinical features, magnetic resonance imaging (MRI), cerebrospinal fluid findings and long term prognosis were reviewed in children who were diagnosed optic neuritis at the first presentation of demyelinating disease at Children's Hospital of Pittsburgh between the years of 1990 and 2007. Follow-up information was obtained from medical records and phone contact with patients or parents. Clinical presentation is defined as monosymptomatic if optic neuritis was the only presenting feature and as polysymptomatic if there is at least one more symptom of central nervous system in addition to optic neuritis. Bilateral optic neuritis is defined as involvement of both eyes immediately or within a maximum period of two weeks2. Final diagnoses were assigned based on the clinical outcome after follow-up. Abnormal MRI is defined by the presence of one or more T2-hyperintense lesions on brain MRIs. Fisher exact test, Chi square test and Mann-Whitney U test were performed to evaluate the association of specific parameters to multiple sclerosis outcome. The study was approved by University of Pittsburgh Institutional Review Board.
RESULTS
Presentation
Thirty children with optic neuritis were identified. All presented with vision loss and 77% also had supraorbital pain or unilateral eye pain. Clinical features at presentation are summarized on Table 1. All children were treated with high dose intravenous methyl prednisolone for three days followed by a tapering dose of oral prednisone.
Table 1.
Clinical features of the optic neuritis cohort at presentation (n=30)
| Features | Results |
| Age at onset (years)–median (range) | 10.2 (3.4–16.9) |
| Gender (female: male ratio) | 1.1 (16/14) |
| Race | 80 % Caucasian |
| Family history of multiple sclerosis | 7 % (2/30) |
| Preceding infection | 50 % (15/30) |
| Monosymptomatic (optic neuritis only) | 70 % (21/30) |
| Unilateral optic neuritis | 67 % (20/30) |
| Bilateral optic neuritis | 33 % (10/30) |
| Papillitis | 40 % (12/30) |
| Positive oligoclonal bands in cerebrospinal fluid | 11 % (3/27) |
| Elevated immunoglobulin G index (3 0.7) | 23 % (6/26) |
| Cerebrospinal fluid, pleocytosis | 70 % (21/30) |
| Cerebrospinal fluid, elevated protein | 10 % (3/30) |
| Abnormal Brain MRI | 40 % (12/30) |
Clinical Outcome; multiple sclerosis
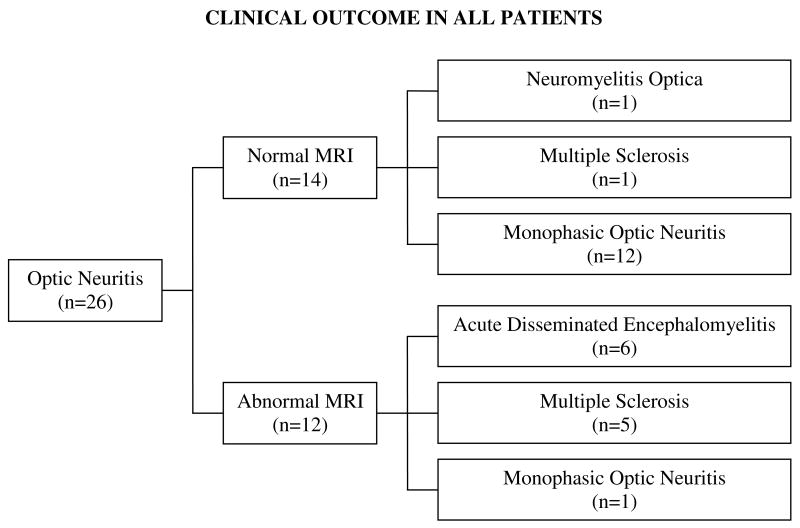
Follow-up information was available in 26 children. Four children were lost to follow-up and were not included in outcome analysis. Mean follow-up duration was 6.2 ± 3.6 years (0.7 to14.6 years). To date, six children (23%) have been diagnosed with multiple sclerosis6. None of the children with multiple sclerosis had encephalopathy in any demyelinating attack and therefore met the criteria for pediatric multiple sclerosis proposed by the Pediatric Multiple Sclerosis Study Group7. All of the children with multiple sclerosis presented initially with clinically isolated optic neuritis (monosymptomatic). Median interval from the first episode to the second disease defining episode was 6 months (3–15 months).
Clinical Outcome; non-multiple sclerosis
Twenty children remained monophasic without further demyelinating events. The mean duration of follow-up in these patients was 6.5 ± 3.7 years (0.7 to 14.6 years). Six of these 20 patients had both polysymptomatic presentation and an abnormal brain MRI. Their follow up MRIs showed complete or almost complete resolution of abnormalities with at most only mild residual gliosis. Five of the six did not have encephalopathy at presentation and they were initially designated as clinically isolated syndrome according to current definitions proposed by the Pediatric Multiple Sclerosis Study Group7. Follow-up data suggested that these six children with abnormal brain MRI had the acute disseminated encephalomyelitis phenotype as they remain relapse free to date. One patient had a polysymptomatic presentation and a normal brain MRI. This patient had concurrent transverse myelitis and was diagnosed with neuromyelitis optica. Thirteen patients had a monosymptomatic presentation. One of these patients had an abnormal brain MRI and is designated as having monophasic optic neuritis. She has been relapse free for 2.3 years. In all probability she represents an example of mild acute disseminated encephalomyelitis. Twelve of the 20 patients with monophasic illness had isolated optic neuritis and a normal brain MRI. None of these patients was found to have multiple sclerosis.
Clinical parameters and multiple sclerosis outcome
The age at presentation correlated with multiple sclerosis outcome. Patients with multiple sclerosis were older at presentation in comparison to the patients who remained monophasic (13.3 ± 5.0 years vs. 9.4 y ±3.0 years, p= 0.039). Elevated immunoglobulin G index (p=0.003) and cerebrospinal fluid oligoclonal bands (p=0.005) were significantly associated with multiple sclerosis outcome. Gender, unilateral or bilateral vision loss, monosymptomatic presentation, and preceding infection were not associated with multiple sclerosis outcome.
MRI results and multiple sclerosis outcome
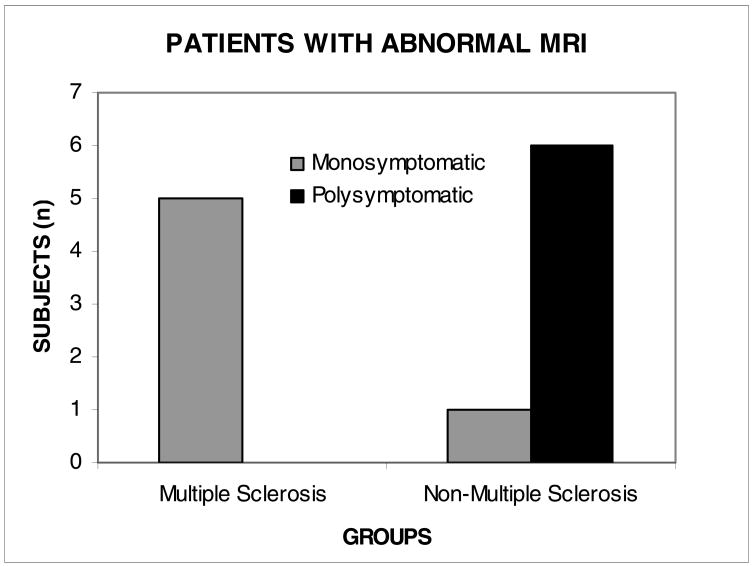
Five of 12 patients with an abnormal brain MRI had multiple sclerosis compared with one of 14 patients with a normal brain MRI (Figure 1). This difference approaches statistical significance (p=0.065). In patients with abnormal MRI, monosymptomatic presentation correlated strongly with multiple sclerosis outcome (p=0.015) (Figure 2). The one child with a normal MRI who was diagnosed with multiple sclerosis had recurrent optic neuritis and developed brain MRI lesions later during the course. Neuromyelitis optica-immunoglobulin G antibody was negative in this child. The presence of periventricular perpendicular ovoid lesions itself strongly suggested multiple sclerosis (p=0.001). The details of the patients presenting with abnormal MRI are shown in Table 2.
Figure 1.
Clinical outcome in optic neuritis cohort according to normal and abnormal magnetic resonance imaging (MRI) of brain (p= 0.065).
Figure 2.
Clinical outcome in patients only with abnormal magnetic resonance imaging (MRI) of brain according to monosyptomatic or polysymptomatic presentation (p=0.015)
Table 2.
Details of the patients who presented with optic neuritis and abnormal MRI at onset (n=12)
| Age at onset (years) | Gender | Clinical presentation | Vision loss | MRI features at onset | Duration of follow-up (years) | Clinical outcome |
|---|---|---|---|---|---|---|
| 16.0 | Female | monosymptomatic | Unilateral | Multiple lesions; PVPOL, CWM | 5.0 | Multiple sclerosis |
| 13.7 | Female | monosymptomatic | Unilateral | Multiple lesions; PVPOL, CBL | 10.2 | Multiple sclerosis |
| 12.1 | Male | monosymptomatic | Unilateral | Two lesions; CWM and internal capsule | 8.4 | Multiple sclerosis |
| 16.3 | Male | monosymptomatic | Unilateral | Multiple lesions; PVPOL, SCWM, CC | 0.7 | Multiple sclerosis |
| 16.9 | Female | monosymptomatic | Bilateral | Multiple lesions; PVPOL, BS, CC, CBL, CWM | 2.1 | Multiple sclerosis |
| 12.9 | Female | monosymptomatic | Bilateral | Two lesions; Bilateral thalami (DGM) | 2.3 | Monophasic optic neuritis |
| 9.1 | Female | polysymptomatic | Bilateral | Multiple lesions of SCWM, CWM, DGM and BS | 6.5 | ADEM* |
| 5.8 | Male | polysymptomatic | Unilateral | Multiple lesions of SCWM, CWM, DGM | 11.2 | ADEM* |
| 7.1 | Male | polysymptomatic | Unilateral | Multiple lesions of CWM, CBL, CC | 6.0 | ADEM* |
| 8.7 | Female | polysymptomatic | Unilateral | Multiple lesions of CWM, SCWM, CBL | 3.9 | ADEM* |
| 5.9 | Male | Polysymptomatic Only child with encephalopathy | Unilateral | Bilateral diffuse lesion of posterior white matter | 0.7 | ADEM |
| 12.0 | Female | polysymptomatic | Unilateral | Single enhancing lesion of CBL | 3.3 | ADEM* |
ADEM: acute disseminated encephalomyelitis, MRI: magnetic resonance imaging, CBL: cerebellum, CC: corpus callosum, CWM, central white matter, SCWM: subcortical white matter, BS: brainstem, DGM: deep gray matter, PVPOL: periventricular perpendicular ovoid lesion.
Because of the absence of encephalopathy, these patients are considered clinically isolated syndrome when pediatric consensus definitions are applied 7.
DISCUSSION
Children with optic neuritis were found to have a 23% risk for developing multiple sclerosis within six years in our study. This study has the third largest cohort with one of the longest duration of follow-up published2–5. Relapses defining multiple sclerosis usually occur within one year following optic neuritis, as noted in this study and others3, 4. Our follow-up was sufficient to detect multiple sclerosis because all children except one were followed for longer than two years in the monophasic group.
The long term prognosis of inflammatory demyelinating optic neuritis in children is mainly determined by the results of brain MRI at presentation. In this study multiple sclerosis was diagnosed in 42% of children with an abnormal MRI whereas 93% of children with normal MRI remained relapse free. These results are in concordance with outcomes reported by Wilejto et al3. Patients that present with optic neuritis only, with no lesions on MRI have a typically monophasic course and a favorable prognosis. One exception consists of children with a first attack of neuromyelitis optica (Devic’s disease) who present with optic neuritis but do not have concurrent transverse myelitis8. These children can be identified by the presence of serum neuromyelitis optica-immunoglobulin G antibody9.
Abnormal brain MRI has previously been reported in 54 % of the patients with optic neuritis3 and was found in 40 % in this study. The prognostic significance of an abnormal MRI with optic neuritis differs in children and adults. In adults an abnormal MRI often suggests multiple sclerosis but in children who have a high frequency of acute disseminated encephalomyelitis, clinical characteristics must be used to ascertain the significance of an abnormal MRI. Children with optic neuritis and an abnormal MRI could be divided into patients with polysymptomatic or patients with monosymptomatic presentation. In this study, six children had polysymptomatic presentation and none of them had relapses. One of these children who had encephalopathy met the consensus criteria for acute disseminated encephalomyelitis7. The other five children shared similar clinical and radiological characteristics at presentation and remained relapse free during the follow-up. We think that this group also had acute disseminated encephalomyelitis but current criteria define this group as clinically isolated syndrome. This observation is important because it illustrates that optic neuritis can be a symptom of acute disseminated encephalomyelitis with a monophasic course. Six children presented with optic neuritis alone, a monosymptomatic presentation, and five of them were diagnosed with multiple sclerosis on follow-up. It has been suggested that MRI evidence of multiple clinically silent (asymptomatic) lesions may be associated with an increased risk for multiple sclerosis7 and our results support this observation in an optic neuritis cohort. A monosymptomatic presentation with multiple silent MRI lesions is usually a characteristic of multiple sclerosis but not of acute disseminated encephalomyelitis.
Luchinetti et al. reported the largest childhood series of optic neuritis to date with the longest period of follow-up2. They found a greater risk of developing multiple sclerosis in those patients who had sequential or recurrent optic neuritis, compared with those patients who had a single episode of optic neuritis occurring in either one eye or both eyes simultaneously. Consistent with these findings, we had one child with recurrent optic neuritis and this child was subsequently diagnosed with multiple sclerosis.
The present study re-examined the outcome predictors of optic neuritis using a long observation period in a pediatric cohort. Correct identification of patients who are at high risk for developing multiple sclerosis is important because therapy is available for early stage disease. However, the MRI criteria for adult patients6 and periventricular perpendicular ovoid lesions may have low sensitivity in children, especially those less than 10 years of age. Based on the results of this study and current literature we suggest that children with optic neuritis meeting the following criteria can be considered for early preventive treatment for multiple sclerosis: monosymptomatic presentation, age greater than 12 years, multiple white matter lesions on brain MRI including periventricular perpendicular ovoid lesions, positive oligoclonal bands in the cerebrospinal fluid and negative serum neuromyelitis optica-immunoglobulin G antibody. Children with multiple sclerosis may reach high disability scores at a young age because of the early onset of their disease. Until well designed multicenter studies using consensus criteria and definitions7 are performed in children, management decisions will remain individual. Further studies are needed to investigate the long-term benefit of early-stage treatment of multiple sclerosis in children.
Acknowledgments
This work was done at Children’s Hospital of Pittsburgh, Pittsburgh, PA. The study was supported in part by the National Institutes of Health under Ruth L. Kirschstein National Research Service Award NS07495 and in part by the NIH NINDS under grant K 12 NS052163. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
The work was presented at the 36th Annual Child Neurology Society Meeting, October 10-13, 2007. Quebec City, Canada.
The authors have no conflict of interest.
References
- 1.Tselis AC, Lisak RP. Other demyelinating diseases. Adv Neurol. 2006;98:335–349. [PubMed] [Google Scholar]
- 2.Lucchinetti CF, Kiers L, O’Duffy A, et al. Risk factors for developing multiple sclerosis after childhood optic neuritis. Neurology. 1997;49:1413–1418. doi: 10.1212/wnl.49.5.1413. [DOI] [PubMed] [Google Scholar]
- 3.Wilejto M, Shroff M, Buncic JR, et al. The clinical features, MRI findings, and outcome of optic neuritis in children. Neurology. 2006;67:258–262. doi: 10.1212/01.wnl.0000224757.69746.fb. [DOI] [PubMed] [Google Scholar]
- 4.Riikonen R, Donner M, Erkkila H. Optic neuritis in children and its relationship to multiple sclerosis: a clinical study of 21 children. Dev Med Child Neurol. 1988;30:349–359. doi: 10.1111/j.1469-8749.1988.tb14560.x. [DOI] [PubMed] [Google Scholar]
- 5.Morales DS, Siatkowski RM, Howard CW, Warman R. Optic neuritis in children. J Pediatr Ophtalmol Strabismus. 2000;37:254–259. [PubMed] [Google Scholar]
- 6.McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50:121–127. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- 7.Krupp LB, Banwell B, Tenembaum S. International Pediatric MS Study Group. Consensus definitions proposed for pediatric multiple sclerosis and related disorders. Neurology. 2007;68(16 Suppl 2):S7–2. doi: 10.1212/01.wnl.0000259422.44235.a8. [DOI] [PubMed] [Google Scholar]
- 8.Wingerchuk DM, Hogancamp WF, O’Brien PC, Weinshenker BG. The clinical course of neuromyelitis optica (Devic’s syndrome) Neurology. 1999;53:1107–1114. doi: 10.1212/wnl.53.5.1107. [DOI] [PubMed] [Google Scholar]
- 9.Lennon VA, Wingerchuk DM, Kryzer TJ, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364:2106–112. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]