Abstract
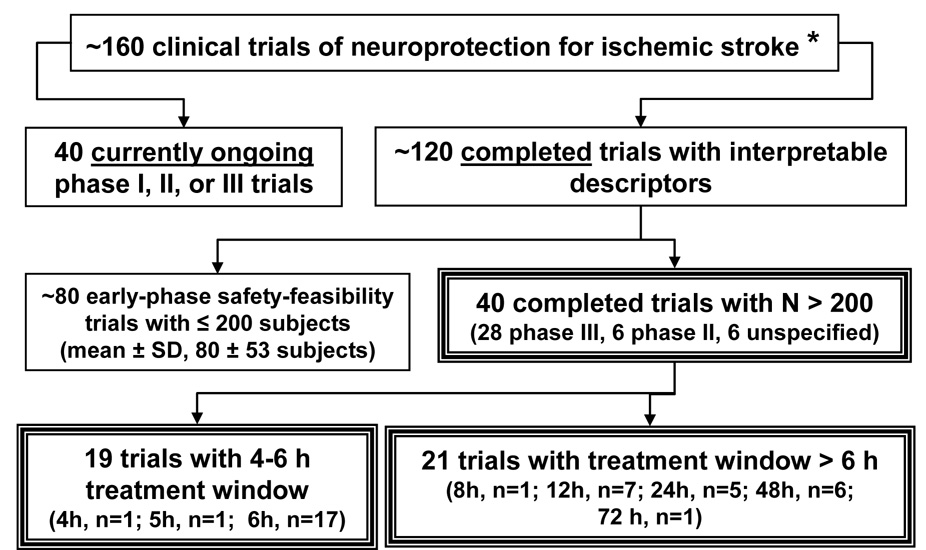
Neuroprotection for ischemic stroke refers to strategies, applied singly or in combination, that antagonize the injurious biochemical and molecular events that eventuate in irreversible ischemic injury. There has been a recent explosion of interest in this field, with over 1000 experimental papers and over 400 clinical articles appearing within the past 6 years. These studies, in turn, are the outgrowth of three decades of investigative work to define the multiple mechanisms and mediators of ischemic brain injury, which constitute potential targets of neuroprotection. Rigorously conducted experimental studies in animal models of brain ischemia provide incontrovertible proof-of-principle that high-grade protection of the ischemic brain is an achievable goal. Nonetheless, many agents have been brought to clinical trial without a sufficiently compelling evidence-based pre-clinical foundation. At this writing, around 160 clinical trials of neuroprotection for ischemic stroke have been initiated. Of the approximately 120 completed trials, two-thirds were smaller early-phase safety-feasibility studies. The remaining one-third were typically larger (>200 subjects) phase II or III trials, but, disappointingly, only fewer than one-half of these administered neuroprotective therapy within the 4–6 hour therapeutic window within which efficacious neuroprotection is considered to be achievable. This fact alone helps to account for the abundance of “failed” trials.
This review presents a close survey of the most extensively evaluated neuroprotective agents and classes and considers both the strengths and weakness of the pre-clinical evidence as well as the results and shortcomings of the clinical trials themselves. Among the agent-classes considered are calcium channel blockers; glutamate antagonists; GABA agonists; antioxidants/radical scavengers; phospholipid precursor; nitric oxide signal-transduction down-regulator; leukocyte inhibitors; hemodilution; and a miscellany of other agents. Among promising ongoing efforts, therapeutic hypothermia, high-dose human albumin therapy, and hyperacute magnesium therapy are considered in detail. The potential of combination therapies is highlighted. Issues of clinical-trial funding, the need for improved translational strategies and clinical-trial design, and “thinking outside the box” are emphasized.
Part I: Neuroprotection - from Past to the Present
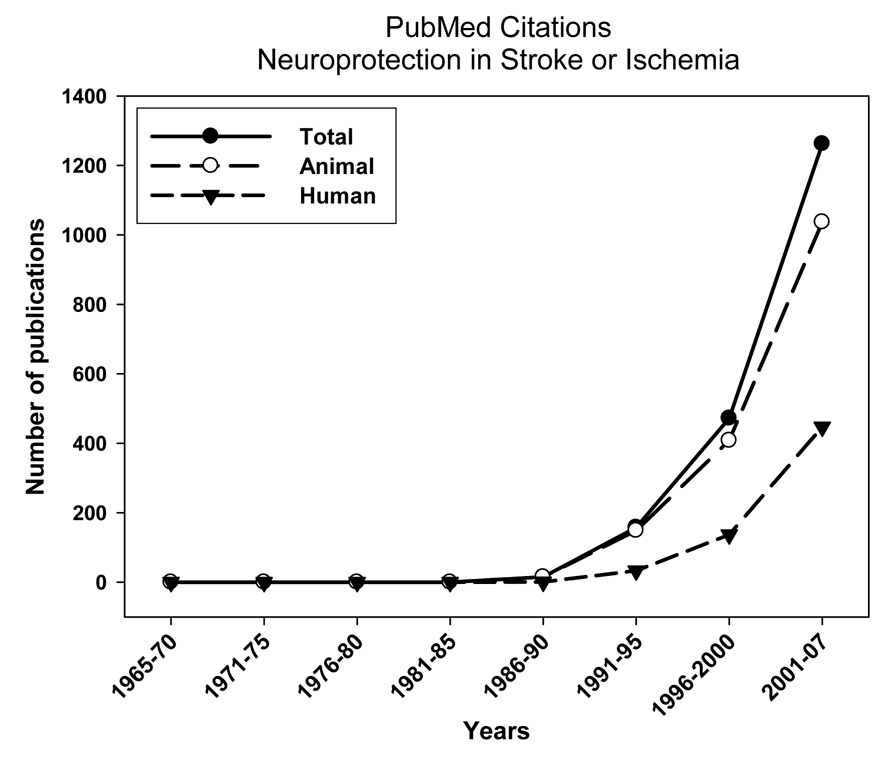
Neuroprotection for ischemic brain injury has emerged only recently as a topic of serious biomedical inquiry. A MEDLINE survey (PubMed, 2007) reveals virtually no publications on this topic until the early 1990’s but a remarkable surge in publications over the past 10 years (Figure 1). In the last 6 years alone, over a thousand experimental papers and over 400 clinical articles have appeared on this subject.
Figure 1.
Numbers of MEDLINE-indexed publications in neuroprotection in stroke / ischemia from 1965 to the present (PubMed, 2007).
The ability of neuroprotection to flourish as a productive field of research depended upon the emergence of a corpus of experimental investigations, beginning in the 1970’s, that defined and characterized the pathophysiology -- i.e., the mechanisms and mediators -- of ischemic brain injury and, by implication, pointed the way to potential interventional strategies for thwarting these injurious factors. Reproducible, physiologically controlled animal models of ischemic injury as well as in vitro systems were developed and validated. The cytopathology of ischemic injury was characterized. Biochemical and molecular events were elucidated, intracellular mediators identified, and numerous important modulatory influences explored. Table 1 summarizes these key topic-areas and provides useful references. Taken together, these advances in our understanding provided the fertile milieu in which ischemic neuroprotection could be rationally approached.
Table 1.
Overview of ischemia-pathophysiology: topics and targets of neuroprotection
Definition
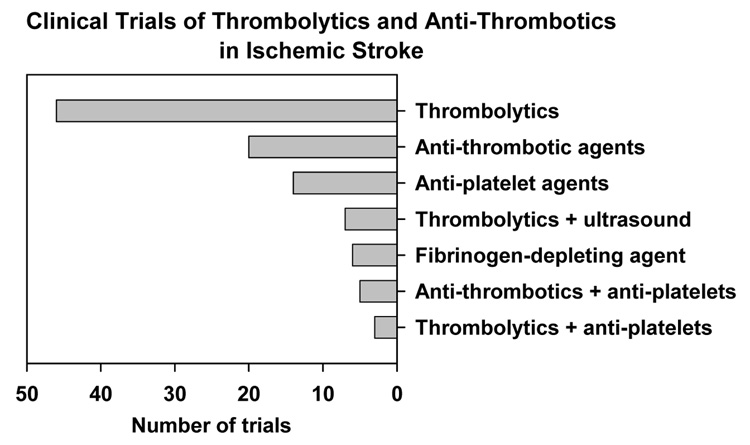
We define neuroprotection as any strategy, or combination of strategies, that antagonizes, interrupts, or slows the sequence of injurious biochemical and molecular events that, if left unchecked, would eventuate in irreversible ischemic injury. This operational definition excludes those therapeutic strategies that are directed primarily at the cerebral vasculature and have as their goal the maintenance of circulatory patency or the reversal of vascular occlusion. This latter category comprises thrombolytic agents (e.g., tissue plasminogen activator, urokinase, mechanical devices), anti-thrombotic agents (e.g., heparin, low molecular weight heparin), anti-platelet drugs (e.g., aspirin, dipyridamole, abciximab), and fibrinogen-depleting agents (e.g., Ancrod). Admittedly, these agents protect the brain but do so primarily via hemodynamic rather than metabolic mechanisms. Among clinical trials for ischemic stroke, those involving thrombolytic, anti-thrombotic, and anti-platelet agents are by far more numerous than clinical trials of neuroprotectants (Figure 2) (Internet Stroke Center, 2007), but they will not be further considered here.
Figure 2.
Clinical trials of thrombolytic agents, anti-thrombotics, and anti-platelet agents in ischemic stroke. (Internet Stroke Center, 2007).
Categories of neuroprotectants
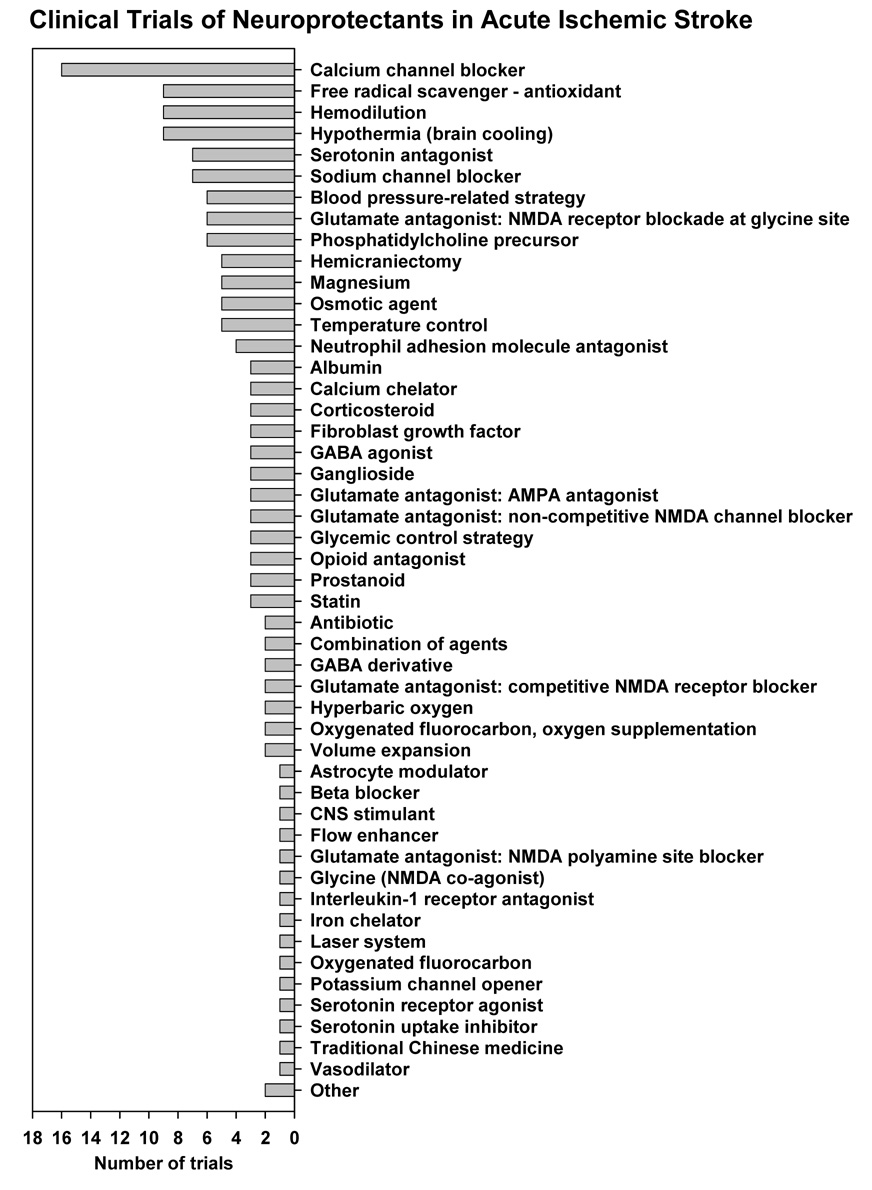
Figure 3 provides an overview of categories of neuroprotective strategies that have progressed to some stage of clinical trial (Internet Stroke Center, 2007). The heuristic value of this graphic is in directing the reader’s attention to the enormous variety of agents and strategies that have received clinical scrutiny – each grounded to some extent in a pathophysiological rationale. In all, approximately 165 ongoing or completed clinical trials are represented (Internet Stroke Center, 2007). By contrast, the MEDLINE database contains over 1,300 reports of ischemic neuroprotection in experimental preparations (Internet Stroke Center, 2007). The task of extracting a coherent viewpoint from this plethora is daunting.
Figure 3.
Clinical trials of neuroprotectants in acute ischemic stroke. (Internet Stroke Center, 2007).
Proof-of-principle
As recently pointed out, a common view of neuroprotection research is that “everything works in animals but nothing works in people.” (O'Collins et al., 2006). Following the announcement of unsuccessful outcomes of clinical trials in neuroprotection, it is common for nihilistic generalizations to appear in print that assert or imply that ischemic neuroprotection may not be an attainable clinical goal. It is useful, therefore, to call attention to numerous studies in experimental animals that provide convincing proof-of-principle that high-grade protection of the ischemic brain is indeed achievable. Table 2 offers a few salient examples, some from the author’s laboratory, assembled to make this point that, in fact, certain therapeutic approaches have proven highly neuroprotective in well-constructed animal studies. Some caveats, however, must be added: It is certainly not the case that “everything works in animals.” It is apparent from the comprehensive review of O’Collins et al (O'Collins et al., 2006) that the pre-clinical evaluation of many agents that were subsequently brought to clinical trial showed only modest or inconsistent tissue protection. Among 66 agents (other than thrombolytics and anti-thrombotics) that they considered, the mean (± SD) overall extent of tissue protection for the group was a modest 31 ± 19% (O'Collins et al., 2006). In addition, there was great variability in the quality or scope of these pre-clinical studies as reflected in their adherence to the Stroke Therapy Academic and Industry Roundtable (STAIR) guidelines (STAIR, 1999). Thus, many agents were brought to clinical trial without a sufficiently solid or relevant evidence-based pre-clinical foundation. Others have analyzed the shortcomings identified in pre-clinical evaluations of putative neuroprotectants (Gorelick, 2000; Cheng et al., 2004). A great number of variables come into play in the design and execution of experimental cerebral-ischemia investigations and may influence the quality, consistency, and outcome of these pre-clinical studies; these are summarzied in Table 3.
Table 2.
Proof-of-Principle: Selected examples of high-grade neuroprotection in experimental cerebral ischemia
| Agent / Class | Animal model | End-point | Time of admin. post-onset | Degree of protection | Reference |
|---|---|---|---|---|---|
| Moderate hypothermia | MCA occlusion (2 h), rat | Behavior, histological infarct volume, 3 d | Onset 2 h; brain temp. 32°C × 3 h | 89% cortical infarct volume reduction | (Huh et al., 2000) |
| Moderate hypothermia | Global forebrain ischemia (10 min), rat | CA1 hippocampal neuronal survival at 28 days | Onset 6 h; brain temp. 32°C × 24h + 34°C × 24 h | 86% neuronal survival (hypothermia) vs. 1% (normothermia) | (Colbourne et al., 1999) |
| High-dose human albumin | MCA occlusion (2 h), rat | Behavior, histological infarct volume, 3 d | 2 h to 4 h | Infarct volume reduction, 84% (cortex) and 61–66% (total) | (Belayev et al., 1998; Belayev et al., 2001) |
| Stilbazulenyl nitrone – radical spin-trap | MCA occlusion (2 h), rat | Behavior, histological infarct volume, 3 d | First dose at 2 h | In 3 series, 64–97% cortical infarct volume reduction | (Ginsberg et al., 2003) |
| Minocycline – antibiotic | Global forebrain ischemia, gerbil | CA1 hippocampal neuronal survival at 6 days | 30 min | 71% neuronal survival (mino) vs. 10.5% (control) | (Yrjanheikki et al., 1998) |
Table 3.
Factors influencing experimental neuroprotection studies
| Animal-related factors |
| Species and strain: rat, mouse, cat, dog, non-human primate |
| Age |
| Sex |
| Co-morbidities |
| Anesthetic agent and co-administered drugs Extent and consistency of physiological control of: |
| Body and brain temperature |
| Arterial blood pressure |
| Arterial blood gases |
| Plasma glucose |
| Model-related factors |
| Focal vs. global ischemia |
| Method of vascular occlusion (e.g., suture, clip, thromboembolus, photothrombosis) |
| In focal ischemia, transient vs. permanent occlusion |
| Duration and intensity of ischemia |
| Duration and extent of reperfusion |
| Duration of survival |
| Consistency of model as reflected in behavioral and pathological sequelae |
| Outcome assessment |
| Method(s) of behavioral testing |
| Rigorous histopathopathology of perfusion-fixed brain material, vs. triphenyl tetrazolium staining |
| Method(s) for quantifying infarction, neuronal survival / death, apoptosis, etc. |
| Acute vs. chronic survival times |
| Quality of study design |
| Randomization among study groups |
| Blinded vs. unblinded outcome assessment |
| Biological variability of the model chosen |
| Statistical analysis: appropriateness of tests chosen; correction for multiple comparisons, etc. |
| Neuroprotective agent |
| Stability; solubility |
| Dose; dose-response characteristics |
| Route of administration |
| Time(s) of administration with respect to ischemic insult |
| Pharmacokinetics and –dynamics; plasma levels |
| Metabolic fate (? neuroprotective metabolites) |
Clinical trials of neuroprotection for ischemic stroke have been surveyed in recent reviews (Cheng et al., 2004; Labiche et al., 2004). The Internet Stroke Center website provides a comprehensive clinical stroke-trial database (Internet Stroke Center, 2007). Figure 3 and Figure 4 summarize the current universe of neuroprotection trials in acute ischemic stroke (Internet Stroke Center, 2007). Of the ~160 such trials, one-quarter are currently ongoing and three-quarters have been completed (or prematurely terminated). It is instructive to consider the completed trials in greater detail. Eighty completed studies are, in fact, merely early-phase safety or feasibility trials with 200 or fewer subjects (Figure 4). Only 40 completed trials have enrolled over 200 subjects, and of these fewer than one-half have instituted neuroprotective treatment within the 4–6 hour therapeutic window within which effacicious neuroprotection is considered possible. This fact alone is sufficient to explain the abundance of non-successful (“failed”) clinical trials.
Figure 4.
Overview of clinical trials of neuroprotection for ischemic stroke. *, Internet Stroke Center, surveyed October, 2007 (Internet Stroke Center, 2007).
Space does not permit a close analysis of all 40 larger completed trials. Rather, greater attention will be focused on the most extensively evaluated agents and classes. For these latter, we shall consider both the pre-clinical evidence (or lack thereof) supporting potential neuroprotective efficacy and the results and shortcomings of the clinical trials themselves. Table 4 summarizes these trials.
Table 4.
Larger completed and published randomized clinical trials of neuroprotection in acute ischemic stroke
| Agent | Trial name | No. subjects | Max. time to treatment | Publications |
|---|---|---|---|---|
| Nimodipine | American Nimodipine Study | 1064 | 48 h | (American Nimodipine Study Group, 1992) |
| Nimodipine | Intravenous Nimodipine West European Stroke Trial [INWEST] | 295 | 24 h | (Wahlgren et al., 1994) |
| Nimodipine | Randomized, double-blind placebo-controlled trial of nimodipine in acute ischemic hemispheric stroke | 350 | 48 h | (Kaste et al., 1994) |
| Nimodipine | Randomised, double-blind placebo-controlled trial of nimodipine in acute stroke [TRUST] | 1215 | 48 h | (TRUST Study Group, 1990) |
| Nimodipine | Very Early Nimodipine Use in Stroke [VENUS] | 454 | 6 h | (Horn et al., 2001a) |
| Aptiganel | Aptiganel Acute Stroke Trial | 628 | 6 h | JAMA 2001;286:2673-82 |
| Selfotel | Acute Stroke Studies Involving Selfotel Treatment [ASSIST] | 567 | 6 h | (Davis et al., 1997; Davis et al., 2000) |
| Gavestinel | Glycine antagonist in neuroprotection for patients with ischemic stroke [GAIN Americas] | 1646 | 6 h | (Sacco et al., 2001) |
| Gavestinel | Glycine antagonist (gavestinel) in neuroprotection [GAIN International] | 1804 | 6 h | (Lees et al., 2000) |
| Clomethiazole | Clomethiazole acute stroke study [CLASS] | 1360 | 12 h | (Wahlgren et al., 1999) |
| Clomethiazole | Clomethiazole Acute Stroke Study in ischemic stroke [CLASS-I] | 1198 | 12 h | (Lyden et al., 2002) |
| Diazepam | Early GABA-ergic activation study in stroke trial [EGASIS] | 880 | 12 h | (Lodder et al., 2006) |
| Magnesium | Intravenous Magnesium Efficacy in Stroke trial [IMAGES] | 2589 | 12 h | (Muir et al., 2004) |
| NXY-059 | Stroke-Acute Ischemic NXY Treatment trial [SAINT I] | 1722 | 6 h | (Lees et al., 2006) |
| NXY-059 | Stroke-Acute Ischemic NXY Treatment trial [SAINT II] | 3195 | 6 h | (Shuaib et al., 2007) |
| Tirilazad | Randomized Trial of High Dose Tirilazad in Acute Stroke [RANTTAS] | 556 | 6 h | (The RANTTAS Investigators, 1996) |
| Ebselen | Ebselen in Acute Ischemic Stroke | 302 | 48 h | (Yamaguchi et al., 1998) |
| Edaravone | Edaravone Acute Infarction Study [EAIS] | 252 | 72 h | (Edaravone Acute Infarction Study, 2003) |
| Citicoline | Treatment of acute cerebral infarction with a choline precursor | 272 | 14 days | (Tazaki et al., 1988) |
| Citicoline | Citicoline Stroke Study [Citicoline 001] | 259 | 24 h | (Clark et al., 1997) |
| Citicoline | Randomized efficacy trial of citicoline in patients with acute ischemic stroke [Citicoline 007] | 394 | 24 h | (Clark et al., 1999b) |
| Citicoline | Phase III trial of citicoline 2000 mg vs placebo [Citicoline ECCO 2000] | 899 | 24 h | (Clark et al., 2001) |
| Citicoline | Effect of citicoline on lesion volume in acute stroke [Citicoline 010] | 100 | 24 h | (Warach et al., 2000) |
| Lubeluzole | US and Canadian Lubeluzole Ischemic Stroke Study (Lub) | 721 | 6 h | (Grotta, 1997) |
| Lubeluzole | European and Australian Lubeluzole Ischaemic Stroke Study | 725 | 6 h | (Diener, 1998) |
| Lubeluzole | Lubeluzole in ischemic stroke (LUB-INT-13) | 1786 | 8 h | (Diener et al., 2000) |
| Enlimomab | Enlimomab Acute Stroke Trial [EAST] | 625 | 6 h | (EAST Trial, 2001) |
| UK-279,276 | Acute Stroke Therapy by Inhibition Neutrophils [ASTIN] | 966 | 6 h | (Krams et al., 2003) |
| Hemodilution | Scandinavian Stroke Study | 373 | 48 h | (Scandinavian Stroke Study Group, 1987; Scandinavian Stroke Study Group, 1988) |
| Hemodilution | Italian Acute Stroke Study | 1267 | 12 h | (Italian Acute Stroke Study Group, 1988) |
| Hemodilution | Amsterdam Stroke Study | 300 | 48 h | (Goslinga et al., 1992) |
| Hemodilution | Multicenter Austrian Hemodilution Trial | 200 | 6 h | (Aichner et al., 1998) |
| Hemodilution + GM-1 | Italian Acute Stroke Study – Hemodilution [IASS-H] | 502 | 12 h | (Argentino et al., 1989) |
Calcium Channel Blocker: Nimodipine
Calcium plays a central role in the pathophysiology of ischemic brain injury as well as cardiac disorders (Siesjo et al., 1989; Choi, 1995; Tymianski et al., 1996; Erecinska et al., 1996). Thus, calcium channel antagonists have found applications in the therapy of angina pectoris, hypertension, and certain arrhythmias (Scriabine et al., 1989). In the brain, blockade of slowly activating (L-type) calcium channels reduces calcium entry into neurons – a potentially salutary action in ischemia and other disorders. Nimodipine is a 1,4-dihydropyridine calcium channel antagonist that exerts neuronal effects and, in addition, is a preferential vasodilator of cerebral vessels, with less pronounced peripheral vasodilation (Kazda et al., 1982; Scriabine et al., 1989). In patients with subarachnoid hemorrhage, nimodipine reduces severe neurological deficits due to cerebral vasospasm (Allen et al., 1983).
Pre-clinical ischemia studies
Over 250 animal studies of nimodipine in cerebral ischemia have been published. A careful survey of this literature, however, was able to identify only 20 controlled animal studies of focal cerebral ischemia in which nimodipine was administered after the induction of ischemia and its consequences assessed (Horn et al., 2001b). Ten of these studies reported a positive outcome, but 10 did not; in the 7 studies in which exact infarct-size data were presented, the pooled effect size (standardized mean difference) favoring nimodipine was −1.2 (Horn et al., 2001b). In several of the positive studies, nimodipine treatment was initiated within the first 15 minutes after onset of ischemia. Subgroup analysis of studies in which treatment was initiated at 1 hour or longer after induction of ischemia revealed overall non-significance (Horn et al., 2001b). The general quality of the studies analyzed was judged to be methodologically weak.
Clinical stroke trials
The Internet Stroke Center registry (Internet Stroke Center, 2007) lists 13 completed clinical trials of nimodipine in acute ischemic stroke, but 8 of these are early-phase, non-definitive studies of fewer than 200 patients. The largest of these was a double-blind randomized trial of 186 patients treated within 24 hours of stroke onset; during the 4-week treatment period, all-cause mortality was reduced with nimodipine, but the effect was restricted to men (Gelmers et al., 1988).
Five larger randomized, double-blind efficacy trials of nimodipine in acute ischemic were subsequently published (Table 4). In the first, 1,215 patients were randomized to oral nimodipine or placebo started within 48 hours (TRUST Study Group, 1990). The trial was negative for the primary end-point – independence at 6 months on the Barthel index (OR 1.22 (95% CI 0.95–1.57)) -- but there was a suggestion of delayed recovery in the nimodipine group at 3 weeks. In the second trial, 1,064 patients were randomized to oral therapy begun within 48 hours and continued for 21 days (American Nimodipine Study Group, 1992). The primary outcome was defined using the Toronto Scale and a motor strength scale. No primary-outcome difference in mortality or neurological outcome was found with any of the rating scales for the overall cohort, but a post-hoc subgroup analysis suggested benefit in the 120-mg nimodipine group when treatment was begun within 18 hours. In the third trial, 350 patients were also randomized to oral treatment within 48 hours (Kaste et al., 1994). The primary endpoints were the Rankin scale, neurological score, and mobility at 12 months. No difference between treatment groups was found for the primary-outcome measures, and post-hoc analyses failed to identify any subgroups that benefited. Case-fatality rates were high in nimodipine-treated patients at 1 and 3 months but not at 1 year; this was possibly attributed to the drug’s blood pressure-lowering effect. A fourth trial randomized 295 patients at 34 centers to treatment within 24 h of stroke onset with intravenous nimodipine or placebo for 5 days. Patients treated with nimodipine, 2 mg/h, fared worse than the placebo group on the primary outcome measures -- neurological status on the Orgogozo scale and functional status on the Barthel index at 21 days; a similar trend was noted in the lower-dose nimodipine group (Wahlgren et al., 1994). A meta-analysis published in 1994, using data from these and other, smaller ischemic-stroke trials found no overall benefit of nimodipine; however, in a subgroup of 616 patients treated within 12 hours after stroke onset, a beneficial effect on neurological and functional was reported (Mohr et al., 1994). Another meta-analysis of calcium antagonists in 825 patients with acute ischemic stroke was unable to confirm this positive result (Horn et al., 2000). In that analysis, intravenous administration of calcium antagonists was, in fact, associated with an increase in poor outcomes; and oral nimodipine started within 12 hours conferred no benefit.
This VENUS Trial, which followed upon these meta-analyses, was intended to test the efficacy of early nimodipine therapy; 454 patients were randomized to oral nimodipine or placebo in a primary-care setting, with treatment begun within 6 hours and continued for 10 days (Horn et al., 2001a). The steering committee terminated the trial prematurely owing to sample-size concerns. The primary end point, defined as poor outcome -- death or dependency after 3 months – did not differ between treatment groups. (Horn et al., 2001a).
Comment
Nearly 3,400 patients were studied in the 5 larger trials summarized here, and over 7,500 in the Cochrane Database meta-analysis (Horn et al., 2000). These trials, carried out in an era of less sophisticated clinical-trial methodology, evince serious design-flaws. Chief among these is the initiation of treatment in 4 of the 5 major trials at 24 or 48 h after stroke onset, well beyond the likely window of therapeutic efficacy. In several studies, the sample size was unrealistically below the number needed statistically to reveal a modest treatment effect and to avoid a type II error. The inclusion criteria and outcome measures used are also open to criticism. Furthermore, these trials were conducted without adequate attention to emerging pre-clinical data that revealed only limited and inconsistent neuroprotection with nimodipine. The uniformly negative primary outcomes of the clinical trials are thus not surprising.
Glutamate Antagonism
It is well established that glutamate, the major excitatory CNS neurotransmitter, is also capable of inducing excitotoxic neural injury in the setting of cerebral ischemia and other disorders (Rothman et al., 1986; Choi et al., 1990; Benveniste, 1991; Hossmann, 1994a; Hansen, 1995; Ginsberg, 1995; Pellegrini-Giampietro et al., 1997; Billups et al., 1998; Bruno et al., 2001; Aarts et al., 2003; Schurr, 2004; Arundine et al., 2004). Glutamate and related excitatory amino acids interact with several receptor-classes, which are relevant to neuroprotection. These include the N-methyl-D-aspartate (NMDA) and the 3-hydroxy-5-methyl-4-isoxazole proprionic acid (AMPA) receptors.
Non-competitive NMDA antagonism
The NMDA receptor complex, which mediates both calcium and sodium ion fluxes, contains an agonist-binding site, a glycine modulatory site, and binding sites within the ion channel, where magnesium exerts a voltage-dependent block (Ginsberg, 1995).
Pre-clinical ischemia studies
The most extensively studied NMDA antagonist is the non-competitive agent MK-801 (dizocilpine), which binds to NMDA receptors with high affinity and produces a long-lasting blockade. MK-801 was extensively evaluated in animal models of focal ischemia (reviewed in (Ginsberg, 1995)) and was capable of reducing infarct volume substantially in several models; typically, it was most effective with treatment initiated prior to ischmia or within the first 1–2 hours thereafter. Dextromethorphan, a centrally acting dextrorotatory analog of codeine, and its metabolite dextrorphan are also high-affinity non-competitive NMDA-channel blockers that are neuroprotective in experimental focal ischemia (Ginsberg, 1995).
Aptiganel (CNS-1102, Cerestat) is the only non-competitive NMDA antagonist to have progressed to later-phase clinical trials. In pre-clinical reports, CNS-1102 treatment begun 15 min after MCA occlusion in rats yielded significant reductions in infarct volume by diffusion-weighted MR imaging and post mortem analysis (Minematsu et al., 1993) and benefitted both gray and white matter (Schabitz et al., 2000). The effective pre-clinical doses of ~2000 micrograms/kg were vastly higher than those tested in subsequent clinical trials (see below).
Clinical stroke trials
In the case of dextrorphan and MK-801, clinical development was halted in the pilot phase. In an ascending-dose trial of dextrorphan begun within 48 hours in patients with mild-to-moderate hemispheric stroke, a variety of dose-related reversible adverse events commonly occurred, including nausea and vomiting, somnolence, hallucinations, agitation, and rapid-onset symtomatic hypotension. The highest infusion rates induced deep stupor or apnea (Albers et al., 1995). The development of MK-801 was also abandoned after early-phase clinical trial experience; although these results were never published, it is commonly assumed that MK-801 also induced dose-limiting neuropsychological adverse events (Olney, 1994).
When aptiganel was tested in normal volunteers, the maximal tolerated dose was ~30 micrograms/kg i.v. over 15 min. (This dose-range, it should be noted, is several orders of magnitude below the effective neuroprotective doses shown in animals.) At higher doses, hypertension and unacceptable degrees of sedation and CNS excitation developed. Euphoria, disinhibition, hallucinations, psychomotor retardation, paranoia, and catatonia were described (Muir et al., 1994; Muir et al., 1995). These results notwithstanding, a phase II/III randomized controlled trial was begun: The Aptiganel Acute Stroke Trial was a double-blind trial of 628 patients at 156 centers randomized to treatment within 6 hours with high- or low-dose aptiganel or placebo (Albers et al., 2001). The primary outcome was the modified Rankin score at 3 months. No improvement in the primary outcome was seen with either dose of aptiganel, and the 4-month mortality rate was higher in the high-dose aptiganel group (26%) than in the placebo group (19%). The trial was aborted by the sponsor and by the independent data and safety monitoring board because of both a lack of efficacy and the imbalance in mortality.
Competitive NMDA antagonism
A single agent of this type – CGS 19755 (selfotel) -- was both evaluated pre-clinically (albeit in a rather limited fashion) and progressed to a larger clinical trial. In permanent MCA occlusion in rats, CGS 19755 administered within 5 min of the insult reduced infarct size and reduced postischemic glucose hypermetabolism, which was putatively excitation-induced (Simon et al., 1990). In cats with 90-min MCA occlusion plus only 4 h of reperfusion, CGS 19755 in a dose of 40 mg/kg at 75 min led to ~50% infarct size reduction (Miyabe et al., 1997). When this agent was brought to clinical trial, a small safety and tolerability study showed that adverse events, comprising agitation, hallucinations, confusion, paranoia, and delirium occurred in all patients treated at 2 mg/kg and in a substantial fraction treated at lower doses (Grotta et al., 1995). (One notes that this dose is far below the protective dose-range demonstrated pre-clinically.) Two pivotal phase 3 prospective studies were then carried out, in which 567 subjects were randomized to a single 1.5 mg/kg dose of selfotel within 6 hours of stroke onset (Davis et al., 2000). The trials were suspended because of a trend toward higher mortality in the selfotel-treated group (Davis et al., 1997; Davis et al., 2000).
Comment
Several obvious factors emerge from the results presented above: a) Virtually all pre-clinical studies suggested that NMDA antagonists protected in focal ischemia only with very early administration, yet the design of clinical trials incorporated much longer times to treatment. b) It was impossible to approximate the pre-clinically protective doses in clinical trials because of dose-limiting neurobehavioral toxicity in humans. In this context, a pre-clinical study is of interest, in which the therapeutic ratio (the ratio of the minimum effective dose for impaired rotarod performance and the minimum effective dose for significant neuroprotection) was measured in a mouse permanent-MCA occlusion model (Dawson et al., 2001). For both aptiganel (Cerestat) and selfotel, this ratio proved to be very low (1 or less), predicting the implausibility of clinical application. Finally, c) the possibility exists that NMDA antagonism, while potentially protective in focal ischemia, is also deleterious in terms of adversely affecting endogenous NMDA-receptor-mediated neuronal-survival mechanisms (Hoyte et al., 2004).
NMDA receptor glycine-site antagonism: gavestinel
Glycine is a co-agonist at the NMDA receptor complex and is required for NMDA receptor function. GV150526 (gavestinel; (E)-3[(phenylcarbamoyl)ethenyl]-4,6-dichloroindole-2-carboxylic acid sodium salt) is a highly potent, highly selective antagonist of the glycine site.
Pre-clinical ischemia studies
In rats with MCA occlusion, GV150526, 3 mg/kg i.v., administered up to 6 h after occlusion yielded significant reduction of infarct volume measured at 24 h and protected somatosensory evoked potential (SEP) responses, although SEP responses recorded from a cortical field closest to the ischemic core were significantly protected only when treatment was begun at 1 h (Bordi et al., 1997). In an MRI study in rats with MCA occlusion, although maximal protection was seen with pre-ischemic administration, when GV 150526 was first administered at 6 h, ischemic volume was still reduced by ~45% (Reggiani et al., 2001). In contrast to NMDA receptor antagonists such as dizocilpine, GV 150526 failed to produce neuronal vacuolization or impaired learning, suggesting that it had a much greater margin of safety than other NMDA antagonists (Bordi et al., 1999).
Clinical stroke trials
Several smaller clinical trials of gavestinel revealed a benign safety profile (Dyker et al., 1999; North American GAIN Investigators, 2000). Two pivotal randomized, double-blind multicenter phase III trials were then conducted: the GAIN Americas Trial (1,646 subjects) (Sacco et al., 2001), and the GAIN International Trial (1,804 subjects) (Lees et al., 2000). These two trials were similarly designed: Patients were stratified by age and stroke severity and were randomly assigned to treatment within 6 hours with either intravenous gavestinel (loading dose 800 mg, plus 5 doses of 200 mg each at 12-h intervals) or placebo. The primary outcome measure was the trichotomized Barthel index at 3 months. Although patients with acute intracranial hemorrhage were enrolled, they were excluded from the target population for the primary efficacy analysis. It is of interest that while tPA was administered in 24.4% of the primary efficacy population in the GAIN Americas Trial, none of the GAIN International subjects received it. Each of these trials was entirely neutral – i.e., showed no difference between treatment groups for either the primary outcome or for mortality or any secondary outcome measures (Lees et al., 2000; Sacco et al., 2001). A small MRI substudy drawn from these two trials, designed to test whether gavestinel would attenuate lesion growth relative to placebo, was also negative (Warach et al., 2006). The patients from the GAIN International and GAIN Americas trials with intracerebral hemorrhage (N=571) were pooled for separate analysis, which revealed that gavestinel neither harmed nor benefited this subgroup (Haley, Jr. et al., 2005).
Comment
In the case of gavestinel, we have an agent whose clinical evaluation was thorough and exemplary in many respects: two large, independently conducted, well-designed, adequately powered phase III trials employing a clinically relevant primary outcome and drug-dosing that yielded plasma concentrations exceeding target levels for pre-clinically predicted protective efficacy (Lees et al., 2000). Rather, it is the pre-clinical evaluation that is found wanting. The demonstration of pre-clinical efficacy consisted of only a few published studies, mostly from Glaxo-Wellcome itself, whose methodological quality was sub-optimal (van der Worp et al., 2005) and whose results were not independently replicated (Gorelick, 2000).
AMPA receptor antagonism
It is of interest that, while AMPA antagonists showed neuroprotective efficacy in certain pre-clinical settings of both focal and global cerebral ischemia (Li et al., 1993; Gill, 1994; Xue et al., 1994; Lees, 2000; Takahashi et al., 2002), the successful completion of larger clinical trials has not been reported. In a phase II double-blind multicenter trial (Elting et al., 2002), the AMPA antagonist ZK200755, when administered in a higher dose, produced a marked transient worsening of the NIHSS score attributable to a depression of consciousness (stupor or coma). In addition, this agent elevated serum concentrations of S-100B (a glial marker). The trial was suspended after 61 patients for safety reasons, and further development ceased.
The ARTIST MRI Trial (AMPA Receptor Antagonist Treatment in Ischemic Stroke) was a randomized double-blind study of the AMPA antagonist YM872 in ischemic stroke, with a 6-hour treatment window, requiring a baseline MRI showing diffusion-perfusion mismatch. The primary outcome was MRI-lesion volume at day 28. This trial began in 2001 and as of July, 2002, had enrolled 108 patients (Internet Stroke Center, 2007). A related ongoing trial, ARTIST+ , reported enrollment of 312 patients randomized within 3 hours to YM872 or placebo; all patients received i.v. tPA within 3 hours; efficacy measures were neurological function and disability scales (Internet Stroke Center, 2007). No full-length reports have emerged from either trial.
GABA Agonism: Clomethiazole, Diazepam
Clomethiazole is a GABA(A)-agonist; its mechanism of action involves potentiation of the activity of GABA, the brain’s major inhibitory neurotransmitter (Wilby et al., 2004). It has been widely used as a sedative.
Pre-clinical ischemia studies
Clomethiazole was perhaps more extensively evaluated in animal models of transient global forebrain ischemia than in focal ischemia. In global ischemia, its protective effect tended to disappear long-term and may have been mediated by hypothermia (Chaulk et al., 2003). Focal ischemia studies included a study of 1-h MCA suture occlusion in rats, followed by 24-h reperfusion, in which clomethiazole was given either 60 min prior to occlusion or at 10 min after the start of reperfusion (i.e., at 70 min after onset of ischemia) (Sydserff et al., 1995b). Histological protection was observed. When studied in a rat model of permanent MCA occlusion, clomethiazole reduced the volume of ischemic damage by 58% when administered at 1 h after occlusion but was ineffective when given at 3 h (Sydserff et al., 1995a). Clomethiazole was also studied in marmosets (small primates) with permanent MCA occlusion; treatment at 5 min reduced overall damage by 32% and improved use of the disabled arm (Marshall et al., 1999). However, when treatment was initiated at 1 h after occlusion in this model, the agent improved spatial neglect but not the affected limb’s severe motor impairment (Marshall et al., 2000).
Clinical stroke trials
In a safety and efficacy trial (the CLASS Trial) involving 1,360 patients with acute hemispheric stroke randomized to clomethiazole or placebo within 12 hours, no difference was found in the proportions of patients achieving functional independence at 90 days (Wahlgren et al., 1999). However, in a subgroup with “total anterior circulation syndrome”, i.e., large hemispheric strokes, the clomethiazole-treated group had an ~11% higher proportion with functional independence than the placebo group. Sedation was the most common adverse event. A small pilot trial (CLASS-T) was then conducted to explore the effect of clomethiazole vs. placebo treatment within 12 hours, when added to conventional tPA therapy (Lyden et al., 2001). The results again showed that patients with large hemispheric strokes treated with clomethiazole showed greater improvement than the placebo-treated group on the Barthel index at 90 days.
A subsequent large trial, CLASS-I, was designed to test the hypothesis, suggested by the earlier findings, that clomethiazole would be protective in larger ischemic strokes (Lyden et al., 2002). That trial studied 1,198 patients with major acute ischemic stroke producing limb weakness, higher cortical dysfunction and visual field deficits. Subjects were randomized to clomethiazole or placebo beginning at 12 hours. The proportion of patients attaining a Barthel index score of 60 or above at 90 days did not differ between groups. Subgroup analysis of patients treated early (< 6h) versus 6–12 hours also failed to show a treatment effect.
Clomethiazole was also studied in a randomized trial of neuropsychological function after coronary artery bypass surgery (245 pts), with treatment administered during surgery. No improvement was shown (Kong et al., 2002).
Comment
Pre-clinical studies showed that the protective effect of clomethiazole depended upon its very early administration, yet the clinical trials for acute stroke allowed a time-to-treatment of 12 hours. Their negative outcomes are not surprising.
Diazepam, a GABA-ergic drug, was studied in a trial of 880 stroke patients randomized within 12 hours of onset. The primary outcome - independence on the Rankin scale at 3 months - was not significantly different between groups (Lodder et al., 2006).
Magnesium
Magnesium may be viewed as an endogenous calcium antagonist that may protect via multiple mechanisms, including NMDA receptor blockade, inhibition of excitatory neurotransmitter release, blockade of calcium channels, as well as vascular smooth muscle relaxation (Ovbiagele et al., 2003). Magnesium sulfate has long been used clinically with great success to treat pre-eclampsia, where it reduces the risk of frank (convulsive) eclampsia by more than one-half (Witlin et al., 1998; Duley et al., 2003).
Pre-clinical ischemia studies
Studies of magnesium as a neuroprotectant in focal ischemia have been rather limited in scope. In one study, intraperitoneal MgCl2 administered just after MCA occlusion in rats reduced infarct volume in rats (Izumi et al., 1991). In another study in rats with autologous MCA thromboemboli treated with 5% MgSO4 (90 mg/kg), improved neurological outcome was described with administration out to 6 h (Yang et al., 2000). A third study, designed primarily to assess serum levels, treated rats with 90-min MCA occlusion beginning with a pre-ischemic MgSO4 bolus; magnesium serum levels below 3 mmol/L were well tolerated but doses above that level produced cardiodepressive effects. Mean infarct-volume reductions of up to 42% were observed (Westermaier et al., 2005). A fourth study employed pre-ischemic intracarotid infusion of MgSO4 prior to MCA occlusion in rats; with higher Mg doses and shorter ischemia durations, infarct-volume reductions up to ~60% could be achieved (Marinov et al., 1996). The overall impression in a recent review of these trials was of mixed results, and concern that a possibly confounding (i.e., protective) influence of hypothermia could not be excluded in the positive studies (Meloni et al., 2006).
Clinical stroke trials
A large multicenter efficacy trial was conducted (Intravenous Magnesium Efficacy in Stroke Trial; IMAGES) in 2,589 patients with acute stroke, in which subjects were randomized to intravenous MgSO4 or placebo with a 12-hour window to treatment (Muir et al., 2004). The primary outcome was a global endpoint incorporating death or disability at day 90; this outcome failed to be improved by magnesium, and mortality was slightly higher in the magnesium- than in the placebo-group. Secondary outcomes were also negative, but planned a subgroup analysis showed a benefit of magnesium in non-cortical strokes.
Comment
Magnesium is a potentially appealing neuroprotectant because it is safe and inexpensive. Nonetheless, the pre-clinical studies reviewed above reveal that it is, in fact, a rather weak neuroprotectant. As is typical of trials with other agents, the multicenter IMAGES trial incorporated a window-to-treatment (12 h) vastly longer than was justified by the findings of pre-clinical focal-ischemia studies. In IMAGES, the median time-to-treatment was 7 hours, and only 3% were treated within 3 h (Muir et al., 2004)
Antioxidant Spin-Trap: NXY-059
NXY-059 (disodium 4-[tert-butylimino)methyl] benzene-1,3-disulfonate N-oxide), a proprietary nitrone spin-trap agent, is a bis-sulfonated derivative of PBN [α-phenyl-N-tert-butyl nitrone], a generic nitrone spin-trap agent that has been shown to protect in models of brain ischemia and trauma.
Pre-clinical ischemia studies
In a transient (2-h) MCA occlusion model in rats, NXY-059 treatment begun at 1 hour after recirculation had a marked dose-dependent effect on infarct volume, with the highest dose reducing infarct volume by 77% (Kuroda et al., 1999). Even when started at 3 h of recirculation (i.e., 5 h after the onset of ischemia), neurologic deficits were still improved and infarct volume was still reduced by approximately two-thirds. Other workers confirmed these effects in similar models (Sydserff et al., 2002) Neuroprotective effects were also described in rat models of permanent MCA occlusion: In one such study, higher-dose NXY-059 treatment begun at 5 min after onset of permanent MCA occlusion in spontaneously hypertensive (SHR) rats led to a 36% reduction in cortical infarct volume (Zhao et al., 2001). In another permanent-occlusion model in rats, 44% infarct reduction was observed even when treatment was initiated at 4 h after stroke onset (Sydserff et al., 2002).
In marmosets pre-trained on behavioral tasks and subsequently given permanent MCA occlusion, NXY-059 treatment begun at 5 min and continued for 48 hours led to improved function of the hemiparetic arm and a lessening of spatial perceptual neglect at 3 and 10 weeks, and to 51% reduction in overall brain damage (Marshall et al., 2001). When treatment was begun at 4 hours after stroke onset, behavioral improvement and a 28% reduction in the overall infarct still resulted (Marshall et al., 2003). Beneficial effects of NXY-059 were also reported in a small-clot embolus model in rabbits (Lapchak et al., 2002b). In similar studies employing large-clot embolism, NXY-059 used alone increased the brain-hemorrhage rate but, when used together with tPA, appeared to reduce tPA-induced hemorrhage (Lapchak et al., 2002a).
Comment
The pre-clinical development of NXY-059 was more extensive than for most other candidate-drugs: The agent was tested in both transient and permanent models of focal ischemia and in both rodents and non-human primates; physiological monitoring was generally appropriate. Both behavioral and histological end-points were used. Beneficial results were replicated in several laboratories. Nonetheless, various deficiencies of these studies have been identified (Savitz, 2007). However, when taken together these pre-clinical results were certainly promising enough to warrant consideration of clinical trials. The high safety-profile of NXY-059 allowed plasma levels to be achieved in humans that equaled or exceeded levels shown to be effective in animal models (Green et al., 2003).
Nonetheless, certain shortcomings are evident in the properties of the compound itself: NXY-059 is a polar, highly water-soluble molecule with very low blood-brain barrier (BBB) permeability (Kuroda et al., 1999) and negligible cellular penetration (Dehouck et al., 2002), suggesting that its major action might be confined to the blood-endothelial cell interface. In addition, NMR-based studies have shown that both PBN and NXY-059 are two orders of magnitude less potent in inhibiting free radical-mediated peroxidative reactions than physiological compounds such as vitamin E (Becker et al., 2002); and cyclic voltametry reveals that PBN (and by inference, NXY-059) have oxidation potentials far higher than those of important biological chain-breaking antioxidants such as vitamin E, glutathione, and beta-carotene (Buettner, 1993; Becker et al., 1998; Ginsberg, 2007). Finally, NXY-059 has extremely low potency, so that very large quantities must be administered.
Clinical stroke trials
NXY-059 was studied in two large randomized, double-blind trials, which to some extent proceeded concurrently. The first trial, SAINT I, involved 1,722 patients (Lees et al., 2006); SAINT II enrolled 3,306 subjects (Shuaib et al., 2007). In both trials, subjects were randomly assigned to receive a 72-hour infusion of intravenous NXY-059 or placebo beginning within 6 hours of stroke onset; each study site was required to maintain an average time-to-treatment of 4 hours or less. In SAINT I, NXY-059 significantly improved the overall distribution of scores on the modified Rankin scale (mRS) as compared to placebo (p=0.038), with a common odds ratio of 1.20 (95% CI, 1.01–1.42) (Lees et al., 2006). However, NXY-059 did not improve outcome on the NIHSS scale or the Barthel index. By contrast, the results of SAINT II were entirely negative: the distribution of mRS scores was virtually identical in the NXY-059 and placebo groups, and there was no evidence of efficacy for the secondary end-points (Shuaib et al., 2007). As regards safety, an excess of hypokalemia was noted in NXY-059-treated patients (Serebruany, 2006).
Comment
Why did the results of SAINT I and II differ? Closer inspection of the SAINT I results reveals that, despite a statistically significant treatment effect on the overall mRS distribution, the magnitude of clincal effect was in fact quite modest and, it might be argued, unimportant. For example, if one were to use a mRS score of 0–1 as a more stringent definition of favorable outcome, the NXY-059 and placebo groups of SAINT I would have attained this result in 33.4% and 31.0% of subjects, respectively – i.e., an absolute percentage difference of only 2.4% and a predicted needed-to-treat number of 41.7 to achieve one positive outcome (Ginsberg, 2007). In this author’s view, the “positive” results of SAINT I are likely to have occurred by chance. Other authors have critically analyzed the design- and statistical weaknesses of SAINT I (Koziol et al., 2006; Saver, 2007). One curious design feature was the inclusion of both tPA-treated and non-tPA-treated subjects (tPA fraction, 29% in SAINT I, 44% in SAINT II) without adequately powering these subgroups for analysis of the primary outcome (Lees et al., 2006; Shuaib et al., 2007). It is conceivable that NXY-059 with vs. without tPA might have conferred differential benefit.
Others have been quick to draw pessimistic generalizations from the failure of SAINT II (.e.g., “ The failure of SAINT II… raises a number of questions about the future of neuroprotection trials and casts doubt on the neuroprotection hypothesis”) (Savitz et al., 2007). The latter inference appears strongly counter-intuitive given the abundant experimental evidence that neuroprotection can, in fact, be achieved. Rather, attention should be directed primarily to the characteristics of the compound itself. Factors likely to have contributed to the lack of clinical success with NXY-059 are: a) its sub-optimal biochemical and physicochemical profile (poor CNS penetration, poor redox characteristics) and b) the fact that SAINT I and II utilized longer windows to treatment (6 hours) than had been shown to confer efficacy when NXY-059 was studied experimentally.
Other Antioxidants: Tirilazad, ebselen, edaravone
Three other antioxidant/radical scavenging agents also deserve mention because each has undergone clinical trials of over 200 subjects.
Tirilazad mesylate (U-74006F) is a non-glucocorticoid 21-aminosteroid inhibitor of iron-dependent lipid peroxidiation that was extensively evaluated pre-clinically beginning in the mid-1980’s in models of traumatic brain injury, hemorrhagic shock, spinal cord injury, experimental subarachnoid hemorrhage, cardiopulmonary arrest, excitotoxicity, as well as in global and focal cerebral ischemia. An extensive systematic pre-clinical review and meta-analysis has been published, surveying animal models of focal ischemia involving tirilazad in which outcome was measured as infarct volume and/or neurological score (Sena et al., 2007). Overall, tirilazad reduced infarct volume by 29% (95% CI, 21–37%) and improved neurobehavioral score by 48%. Efficacy was higher in temporary occlusion than in either permanent or thrombotic models (Sena et al., 2007). Maximum efficacy was seen when treatment was given before the onset of ischemia, with a trend for efficacy to decline thereafter. It is noteworthy that the median time to administration in the studies surveyed was only 10 min after onset of the insult! The authors’ analysis reveals that, with times to treatment greater than 60 min, the efficacy data showed very broad confidence intervals (Sena et al., 2007). Furthermore, tirilazad was effective over a very narrow dose range of 3–10 mg/kg.
A prospective, randomized clinical trial of tirilazad mesylate was conducted in 660 patients with acute stroke treated within 6 hours of onset (median 4.3 h); the primary outcome was disability on the Glasgow Outcome Scale and Barthel index at 3 months (The RANTTAS Investigators, 1996). The trial was prematurely terminated based on an independent interim analysis. In the 556 fully analyzed subjects, there was no effect of tirilazad on outcome. A radiological analysis of these subjects revealed that tirilazad had no effect on infarct volume (van der Worp et al., 2002). A subsequent clinical trial, RANTTAS II, was planned to test the hypothesis that the lack of efficacy in RANTTAS might have been secondary to inadequate dosing. The trial was stopped when questions regarding safety emerged from a parallel trial in Europe (Internet Stroke Center, 2007). A Cochrane-Collaboration meta-analysis was published of six double-blind placebo-controlled tirilazad trials (4 published, 2 unpublished) in 1,757 patients with acute ischemic stroke (Tirilazad International Steering Committee, 2000). This analysis revealed that, while tirilazad did not alter early or end-of-trial case fatality rates, it did increase the odds of being dead or disabled by about one-fifth (borderline-significant).
In comparing the pre-clinical and clinical tirilazad studies, it is apparent that the clinical trials a) used a much broader (by implication, too low) dose range and b) employed a much longer time to treatment (median ~5 h) than the animal trials (median, 10 min).
Ebselen (2-phenyl-1,2-benzisoselenazol-3(2H)-one) is a selenium compound with glutathione peroxidase-like activity; it also reacts with peroxynitrite and inhibits a variety of enzymes (Parnham et al., 2000). In rodent models of MCA-distribution ischemia, ebselen reduced ischemic damage when administered prior to ischemia (Namura et al., 2001) and was modestly protective if begun 30 min after induction of ischemia (Takasago et al., 1997). When treatment was begun at the onset of recirculation after 2-h MCA occlusion in rats, ebselen reduced early brain injury and improved neurological deficits at 24 hours (Imai et al., 2001), but this protection was not sustained at 7 days (Salom et al., 2004). In a clinical trial of 302 acute ischemic-stroke patients randomized to oral ebselen or placebo treatment begun within 48 hours and continued for 2 weeks, the intent-to-treat primary-outcome analysis was significant for ebselen at 1 month but not 3 months (Yamaguchi et al., 1998). A secondary analysis suggested benefit in the ebselen-subgroup treated within 24 h. A Phase III study of 394 patients incorporating a 24-hour window was slated to begin in 2001 (Internet Stroke Center, 2007), but no report has appeared.
Edaravone (MCI-186; 3-methyl-1-phenyl-2-pyrazolin-5-one) is an oxygen radical scavenger and blocker of lipid peroxidation. Early pre-clinical reports described salutary effects in both global and focal cerebral ischemia (Watanabe et al., 1994). In a rat modelf of transient (1-h) MCA occlusion, edaravone reduced infarct volume when administered prior to the insult but failed to protect when started at 1–2 hours after onset of ischemia (Nakajima et al., 2005). Another study reported ~30% reduction of total infarct volume in rats with 2-h MCA occlusion treated at the onset of reperfusion (Amemiya et al., 2005). In mice with 60-min MCA occlusion, edaravone appeared to reduce infarct volume and improve neurological score at 24 h even when administered at 6 h after onset of ischemia (Zhang et al., 2005a). Only a single randomized clinical trial of edaravone has been fully published: a phase II study of 252 ischemic-stroke patients with a 72-hour window to treatment; this trial was said to show improved outcome on the modified Rankin scale at 3 months (Edaravone Acute Infarction Study, 2003).
Phospholipid Precursor: Citicoline
Citicoline refers to the exogenously supplied form of cytidine 5-diphosphocholine (CDP-choline), a product of the rate-limiting step in the synthesis of phosphatidylcholine from choline. Orally administered citicoline is hydrolyzed in the gut to cytidine and choline, which are rapidly absorbed (Weiss, 1995), cross the blood-brain barrier, and can be incorporated into the phospholipid fraction of neuronal membranes (Secades et al., 1995). CDP-choline increases phospholipid synthesis, inhibits phospholipid degradation and free fatty acid release, increases CNS levels of norepinephrine and dopamine, and restores mitochondrial and membrane ATPase activities (Secades et al., 1995; Weiss, 1995). While CDP-choline and its components do not directly affect phospholipase A2 (PLA2) activity in vitro, when studied in vivo citicoline attenuates ischemia-induced PLA2 stimulation and thereby diminishes the injurious consequences of phospholipid hydrolysis – namely, the generation of arachidonic acid, whose metabolism leads to formation of reactive oxygen species, lipid peroxides and toxic aldehydes (Adibhatla et al., 2003). In the setting of transient focal ischemia, citicoline restores phosphatidylcholine levels by differentially affecting PLA2 and CTP-phosphocholine cytidlyltransferase (Adibhatla et al., 2006). Citicoline also inhibits glutamate-induced apoptosis in cultured cerebellar granule neurons (Mir et al., 2003) and increases glutamate uptake and expression of the membrane glutamate transporter EAAT2 in cultured astrocytes (Hurtado et al., 2005).
Pre-clinical ischemia studies
Several studies in rodent models of focal ischemia have been reported. In a rat model of transient MCA occlusion, high-dose citicoline treatment begun at the time of reperfusion (2 h) reduced infarct volume by one-half, but the study was flawed by failure to control brain temperature and substantial premature mortality (Schabitz et al., 1996). In another MCA occlusion study, treatment was begun at 15 min after onset of ischemia; citicoline improved behavioral and morphological indices chiefly in rats with submaximal insults (ischemia of 30–75 min) (Aronowski et al., 1996a). When ischemia was produced by clot embolus, one study showed that citicoline begun at 45 min failed to affect infarct size unless tPA was co-administered (Andersen et al., 1999); and another showed that citicoline administered prior to tPA failed to confer additional benefit but, if administered 10 min after tPA, led to less ischemic injury than with tPA alone (Alonso de Lecinana M. et al., 2006). An interesting recent report (Hurtado et al., 2007) provides evidence that citicoline treatment begun 24 hours after MCA occlusion and maintained for 28 days improves functional outcome and enhances dendritic complexity and spine density in layer V pyramidal cells of the undamaged motor cortex, suggesting that chronic treatment may increase neuronal plasticity within noninjured, functionally connected brain regions.
Comment
The biochemical actions of exogenous CDP-choline (citicoline) have been well characterized. However, the published reports of citicoline in pre-clinical ischemia models were limited in scope and failed to provide key translational data needed to assess the potential for clinical neuroprotection (particularly, defining the therapeutic window of efficacy). Positive results were linked to early administration. The interesting possibility that chronic citicoline treatment enhances neuronal plasticity deserves further study.
Clinical stroke trials
Citicoline in doses of 1 g per day for 14 days proved entirely safe (Tazaki et al., 1988). Indeed, the clinical safety of citicoline has been repeatedly confirmed. Four important trials and a pooled meta-analysis have been reported. In the first, 259 acute ischemic stroke patients were randomized to 6-week treatment with citicoline (3 different doses) or placebo commencing within 24 hours (mean, 14.5 h). With covariate adjustment for baseline NIHSS scale, 2 citicoline dose-groups were found to be significantly improved at 90 days on the Barthel index (Clark et al., 1997). There ensued a 33-center randomized double-blind efficacy trial in 394 subjects, with oral treatment begun within 24 hours and continued for 6 weeks (Clark et al., 1999b). There was a significantly higher percentage of patients with mild stroke (baseline NIHSS < 8) in the placebo group compared to the citicoline group. The primary efficacy analysis (Barthel index at 12 weeks) was not completed due to the failure of a key statistical assumption, and the planned secondary analyses were not positive. Only a post-hoc analysis of the subgroup with baseline NIHSS = > 8 suggested that citicoline subjects were more likely to have full recovery (33%) than placebo (21%). A third trial in 899 ischemic-stroke subjects treated beginning at 24 hours (mean, 13 h) again showed no between-group difference in the primary analysis (Clark et al., 2001). A fourth study was an MRI-based trial of 100 acute ischemic stroke subjects treated for 6 weeks, beginning within 24 h, and followed for MRI lesion-size changes at 12 weeks (Warach et al., 2000). The primary MRI analysis (baseline-to-12-week change) showed no significant difference between groups, but secondary analysis of lesion volume from week 1 to week 12 showed a greater decrease in the citicoline group.
A pooled analysis of individual patient data from the 4 randomized trials of oral citicoline described above (N=1,372 with baseline NIHSS = >8), re-analyzed using a global 3-month outcome measure incorporating NIHSS, mRS and Rankin scales, revealed a statistically significant effect of citicoline on global recovery (25.2% vs. 20.2%, OR 1.33 (95% CI, 1.10–1.62, p=0.0034) (Davalos et al., 2002). The highest effect was seen in the 2000 mg dose-group.
Comment
Citicoline is consistently safe in patients. A key flaw of all these trials is their unrealistically long time to treatment – 24 hours – a duration adopted despite a complete absence of pre-clinical evidence supporting efficacy with a 24-h delay to treatment. Individual clinical trials suffered from other design flaws. The significant result of the pooled meta-analysis is, however, a “positive” result and is consistent with either a mild neuroprotective effect or else an effect of citicoline on longer-term neuronal plasticity and recovery processes. A major strength is that all these studies were published in full. Currently ongoing is the ICTUS International Citicoline Trial on Acute Stroke; planned recruitment is N=2,600; combined neurological and MRI end-points will be considered. It is unfortunate that the window to treatment remains at 24 hours (Internet Stroke Center, 2007).
Nitric Oxide Signal Transduction Down-Regulator: Lubeluzole
Lubeluzole, the S-isomer of a novel 3,4-difluoro benzothiazole, is thought to act by down-regulating the glutamate-activated nitric oxide synthase pathway (Lesage et al., 1996). In vitro, lubeluzole improved the ability of hippocampal slices to recover their membrane potential after repeated DC depolarizations (Ashton et al., 1997) and protected hippocampal neurons against nitric oxide toxicity (Maiese et al., 1997).
Pre-clinical ischemia studies
Lubeluzole was studied most extensively in a photochemical model of parietal sensorimotor cortical stroke in rats; in this model, lubeluzole rescued tactile/proprioceptive hindlimb placing reactions when administered 5 min after stroke onset and protected 60% of rats when administered at 6 h (De Ryck et al., 1996). The optimal regimen begun at 5 min reduced infarction by 28% at 7 days (De Ryck et al., 1996) and attenuated infarct growth as assessed by MRI (De Ryck et al., 2000). Lubeluzole also blocked peri-infarct glutamate increases in this model (Scheller et al., 1997). In rats with reversible MCA and carotid artery occlusions for 120 min or more, lubeluzole treatment started 15 or 30 min after onset of ischemia reduced infarct size by 50% and 34%, respectively (Aronowski et al., 1996b). Other workers described infarct-volume reductions of 33% in rat MCA occlusion with treatment begun at 3 h (Culmsee et al., 1998). In rats with global cerebral ischemia, lubeluzole treatment begun at 5 min protected hippocampal CA1 neurons (Haseldonckx et al., 1997).
Comment
These pre-clinical results support mechanistically based neuroprotective efficacy with very early administration but do not adequately substantiate whether robust neuroprotection is possible with longer, clinically relevant, treatment delays.
Clinical stroke trials
A safety study in 193 patients with carotid artery-territory ischemic stroke was terminated prematurely because of an imbalance in mortality between treatment groups, highest in the 20 mg/day lubeluzole group; the lower, 10 mg/day dose was considered safe (Diener et al., 1996). A multicenter US and Canadian double-blind trial was then conducted in 721 patients randomized to lubeluzole (7.5 mg + 10 mg/day × 5 days) or placebo initiated within 6 hours of symptom onset. The primary end-point, mortality at 12 weeks, did not differ between groups, but recovery on the NIHSS scale and Barthel index was improved by lubeluzole (Grotta, 1997). A European and Australian study randomized 725 patients to treatment in a manner similar to the US and Canadian study, with a 6-hour treatment window. Overall mortality at 3 months was again similar for lubeluzole and placebo, but a post-hoc analysis suggested that mortality in patients with mild or moderate strokes was reduced by lubeluzole (Diener, 1998). Finally, a third large trial was then carried out in 1,786 patients, with the efficacy analysis conducted in patients 75 years old or younger treated at 0–6 hours after stroke. The treatment groups showed no difference in either the primary outcome measure -- the trichotomized Barthel index at 12 weeks -- or secondary outcome measures (Diener et al., 2000). A Cochrane Database meta-analysis, reviewing five trials and 3,510 patients, also found no effect on mortality or dependency but noted a significant increase of heart-conduction disorders (Q-T prolongation) in lubeluzole-treated subjects (Gandolfo et al., 2002).
Comment
These studies mostly used a 6-h window to treatment – a duration not strongly supported by the pre-clinical data. It might be argued that the extent of preclinical efficacy was insufficient to warrant such a large investment in clinical trials. The use of mortality as a primary outcome measure is considered to be a weak design feature; in current trials, neurological outcome and functional recovery are preferred as primary end-points.
Leukocyte Inhibition: Enlimomab and UK 279,276
Enlimomab is a murine intercellular adhesion molecule-1 (ICAM-1) antibody that reduces leukocyte adhesion. In rats with 2-h transient MCA occlusion treated at 1 h of reperfusion, a reduction in size of the ischemic lesion was seen; there was no effect, however, in permanent occlusion (Zhang et al., 1995). In the EAST multicenter clinical trial, 625 patients with acute ischemic stroke were randomized to enlimomab or placebo within 6 hours of onset. The primary efficacy endpoint was the modified Rankin Scale at 90 days. This trial showed a highly significant worsening of outcome in enlimomab-treated patients compared to placebo (p=0.004), and a higher death rate (EAST Trial, 2001). To elucidate the reasons for this negative clinical outcome, an experimental study was performed in which a murine anti-rat ICAM-1 antibody was administered to rats with focal ischemia (Furuya et al., 2001). This treatment failed to reduce infarct size but elicited host antibody production and activated circulating neutrophils and complement; these mechanisms were offered as a possible explanation for the treatment-related deterioration in the clinical trial.
In a related approach, neutrophil activation was blocked by a recombinant protein inhibitor of the CD11b/CD18 receptor, UK 279,276. In the ASTIN Trial (Acute Stroke Therapy by Inhibiton of Neutrophils), 966 acute stroke patients were treated within 6 hours of onset with the agent or placebo, and neurological recovery was assessed at 90 days. The trial, which incorporated a Bayesian sequential design, was terminated early for futility (Krams et al., 2003). A possible reason to explain lack of efficacy was a body of pre-clinical evidence that UK 279,276 conferred benefit in reperfused focal ischemia models but failed in the absence of reperfusion (Sughrue et al., 2004).
Hemodilution
Hemodilution is thought to decrease blood viscosity and may increase cerebral perfusion or oxygen delivery, but in fact various hemodiluting agents have differing effects. For example, in a comparison study (Haass et al., 1986), both dextran 40 and hydroxyethyl starch (HES) lowered hematocrit and whole-blood viscosity, but dextran 40 increased plasma viscosity and red-cell aggregration while HES did the opposite. Thus, HES was thought to be more appropriate for use in plasma volume-expansion.
The literature contains many examples of small clinical trials of hemodilution for stroke (Asplund, 2002); these will not be reviewed here. The larger hemodilution trials in acute ischemic stroke form a highly heterogeneous group, employing a variety of agents, procedures, and settings. The Scandinavian Stroke Study was a randomized phase III trial of 373 subjects with a 48-hour treatment window; venesection and dextran 40 were both employed. There was no improvement in outcome or survival at 3 months (Scandinavian Stroke Study Group, 1987), and a subgroup analysis was also negative (Scandinavian Stroke Study Group, 1988). In a large Italian trial, 1,267 patients with hemispheric stroke (comprising both ischemia and intracerebral hemorrhage) of 12 hours or less, and with hematocrit of 35% or more, were randomized to hemodilution by venesection and dextran 40 volume replacement, or to control management (Italian Acute Stroke Study Group, 1988). Mortality at 6 months was similar in the two groups, and there was no improvement with treatment even in the subgroups with ischemic stroke < 6 h and highest hematocrit. In another trial, the Amsterdam Stroke Study (Goslinga et al., 1992), 300 patients were studied. Normovolemic hemodilution was induced with 20% albumin plus crystalloids, targeting a pulmonary capillary wedge pressure of 12 mmHg and hematocrit of 32%. Analysis at 3 months suggested a complex pattern of responses related both to treatment and to initial hematocrit. In the IASS-H trial, 502 patients were randomized with respect to both GM1 ganglioside treatment and hemodilution, with a 12-hour window; the results were negative (Argentino et al., 1989). Finally, the Multicenter Austrian Hemodilution Trial was a randomized double-blind study of hypervolemic hemodilution instituted within 6 hours of MCA-territory ischemic stroke; groups were randomized to either 10% hydroxyethyl starch or to pure rehydration with Ringer’s lactate (Aichner et al., 1998). The primary outcome was clinical improvement within 7 days on the Glasgow Outcome Scale. The trial was halted after an interim analysis of 200 patients failed to show a beneficial effect.
A Miscellany of Other Agents Studied Without Success in Larger Clinical Trials
These agents are listed in descending order of numbers of subjects studied.
BMS-204352, a fluoro-oxindole, is an activator of neuronal potassium channels. In rats with permanent occlusion, BMS showed ischemic protection with treatment at 2 hours (Gribkoff et al., 2001). This compound was studied in two parallel clinical trials involving 1,978 subjects randomized to treatment within 6 hours of stroke onset. The primary outcome was change from baseline to 12 weeks on the NIHSS scale. The agent failed to exhibit efficacy, and a full publication did not appear (Internet Stroke Center, 2007).
GM1 ganglioside, a monosialoganglioside, was studied in a trial of 287 acute stroke patients randomized to treatment within 48 hours with GM1 by intramuscular injection, or placebo, for 28 days. The trial was negative (SASS Trial, 1994). In another trial (also mentioned above), 502 acute stroke patients were randomized to treatment initiated within 12 hours with GM1 or placebo, with or without hemodilution. Again, there was no effect of treatment (Argentino et al., 1989). In a third randomized trial of GM1, 792 subjects were treated within 5 hours. The primary outcome was mortality and change in Canadian Neurological Scale score at 4 months. There was a non-significant trend toward greater improvement with GM1 (Lenzi et al., 1994). A Cochrane meta-analysis found that there was insufficient evidence to conclude benefit of GM1 in stroke, and caution was warranted because of sporadic cases of Guillain-Barre syndrome after ganglioside therapy (Candelise et al., 2001).
Piracetam is an agent thought to act as a modifier of membrane fluidity (Muller et al., 1999), cognition- and microcirculation-enhancer, neuroprotectant, and anticonvulsant (Winblad, 2005). A phase III trial of piracetam was conducted in 927 acute stroke patients randomized to treatment within 12 hours of onset. The primary outcome, neurological function at 4 weeks, was similar in the two groups, but post-hoc analyses suggested superiority of piracetam in the subgroup presenting within 7 h of onset (De Deyn et al., 1997).
Nalmefene (Cervene), an opioid antagonist with relative selectivity for kappa opiate receptors, received very little experimental testing in animal models of focal ischemia but was nonetheless brought to clinical trial. A phase II trial of 312 patients randomized to treatment within 6 hours revealed safety but no significant difference in functional outcome at 3 months (Clark et al., 1999a). Similarly, a phase III trial of 368 subjects treated within 6 hours showed no difference in the primary outcome – Barthel index and Glasgow Outcome Scale at 12 weeks (Clark et al., 2000).
Basic fibroblast growth factor is thought to stabilize intracellular calcium ion homeostasis, induce antioxidant enzymes, and diminish glutamate-mediated excitotoxicity (Mattson, 1997b). A randomized multicenter trial, planned for 900 subjects with a 6-hour treatment window, was halted after 286 subjects were enrolled. There was no significant difference in outcome between groups (Bogousslavsky et al., 2002). Another similar trial was aborted after 302 subjects, and the results were not published.
Fosphenytoin, a sodium channel blocker and anticonvulsant, was studied in a phase III trial of 462 ischemic strokes randomized to treatment within 4 hours. The primary outcome was modified Rankin scale at 3 months. The trial was stopped after an interim analysis that found no differences between treatment groups. The results were not published (Internet Stroke Center, 2007).
Flunarizine
This calcium channel blocker was studied in a multicenter randomized trial of 331 subjects treated within 24 hours. There was no effect of treatment (Franke et al., 1996).
Pentoxifylline, a vasodilator with possible rheologic effects, was studied in a phase II study of 297 subjects with acute stroke randomized to treatment within 12 hours. Followup was 28 days. The groups did not differ in mortality or functional deficit (Hsu et al., 1988).
Repinotan (BAY x3072), a serotonin 5HT1A receptor agonist, was studied in a phase II trial of 240 subjects with hemispheric ischemia treated within 6 hours (Bayer Randomized Acute Ischemia Neuroprotectant Study – BRAINS). The results, which are assumed to have been negative, were not published (Internet Stroke Center, 2007).
Shortcomings of Completed Clinical Trials of Neuroprotection
From the review of individual agents and trials presented above (Table 4), many shortcomings, both pre-clinical and clinical, crop up repeatedly from agent to agent. Taken singly, each factor is potentially capable of sabotaging success; when present in combinations, failure is virtually assured. Some of these factors are more important than others. The discussion below highlights key considerations.
Time-window to treatment a) There is practically no evidence that neuroprotection for acute ischemic stroke is possible with any agent beyond ~6 hours. b) Even within the 4–6 hour upper limit of putative efficacy, the extent of protection with any agent is likely to decline with increasing delay to administration. c) Whenever a clinical trial establishes a treatment-window of X hours, the majority of subjects are enrolled within the last possible hour. Taken together, these points force one to the conclusion that clinical trials of neuroprotection must be designed with a very early window to treatment. In over one-half of the completed trials reviewed here, the window was beyond 6 hours; and even a 6-hour window may have been too late. Furthermore, it is often the case that clinical trials were designed with a long window-to-treatment despite strong pre-clinical evidence that the window was, in fact, much shorter. Any hope for clinical success in these cases must be judged as purely fanciful.
Solid pre-clinical evidence of neuroprotective efficacy: The minimal pre-clinical preconditions to be satisfied before bringing an agent to clinical trial should be: a) demonstration of robust, clinically relevant protective efficacy (e.g., 50% or greater infarct-size reduction plus neurobehavioral improvement with a window-to-treatment of at least 3–4 hours after onset of ischemia); b) proper experimental design of these studies (including full monitoring and control of physiological variables, so as to avoid (for example), the confounding influence of brain hypothermia; randomized allocation to treatment groups; blinded outcome assessment; demonstration of enduring protective effect with survival times of at least several days to one week; proper statistics with correction for multiple comparisons; etc.); and c) confirmation (replication) of positive findings by other laboratories. Many if not most of the large completed clinical trials reviewed above were launched without fully satisfying these pre-clinical milestones. Recent reviews critically addresses the factors that contribute to the quality of experimental stroke research (van der Worp et al., 2005; Dirnagl, 2006).
Ability to achieve pre-clinically efficacious drug-doses or plasma levels in human subjects: There are several examples of clinical trials designed using drug-dosing vastly lower than the levels shown to protect the brain of animals. For some agents (e.g., NMDA antagonists), dose-limiting adverse events not fully anticipated in pre-clinical studies emerged during human trials. In general, agents that cannot be administered to humans in doses equivalent to those required for neuroprotection in animals should not be brought to phase II/III clinical trial, and agents with an unfavorable therapeutic ratio of efficacy relative to toxicity should probably be avoided.
Incorporation of crucial design-features into pivotal clinical trials: These include: a) a short window to treatment compatible with the pre-clinical findings; b) drug-dosing compatible with pre-clinically demonstrated efficacious doses; c) adequate follow-up period (3 months is commonly used in ischemic stroke trials); d) choice of clinically meaningful primary-outcome measures and avoidance of statistically forgiving but clinically unimportant end-points; e) sample size powered to demonstrate efficacy with statistical certitude and avoid type II errors; f) choice of stratification variables relevant to the agent in question (e.g., thrombolysed vs. non-thrombolysed subjects -- a factor of importance with agents that require reperfusion in order to neuroprotect). Again, many of the completed trials discussed above were deficient in these respects (Cheng et al., 2004).
Part II: Neuroprotection -- Moving from the Present into the Future
Some Promising Ongoing Efforts
1. Therapeutic hypothermia
Moderate therapeutic hypothermia represents one of the most solidly evidence-based neuroprotective strategies currently available (Hemmen et al., 2007). A large corpus of experimental studies over the past 20 years has provided incontrovertible evidence that moderate hypothermia is capable of conferring high-grade neuroprotection in focal and global cerebral ischemia by impeding a host of deleterious metabolic and biochemical injury-mechanisms, with a therapeutic window appropriate for clinical application in ischemic stroke (Ginsberg et al., 1992; Colbourne et al., 1997; Barone et al., 1997a; Corbett et al., 2000; Huh et al., 2000; Gunn et al., 2005; Ginsberg et al., 2005). By contrast, even modest degrees of fever (hyperthermia) have been shown, both experimentally and clinically, to worsen outcome in stroke and other types of brain injury (Reith et al., 1996; Castillo et al., 1998; Ginsberg et al., 1998a; Wang et al., 2000). As fever is common in critically ill neurological and neurosurgical patients, the latter considerations have led to heightened efforts to prevent and treat fever in the ICU setting (Kilpatrick et al., 2000; Mayer et al., 2004; Diringer, 2004).
Two landmark clinical trials published in 2002 demonstrated that mild therapeutic hypothermia (32–34°C × 12 or 24 h) instituted after cardiac arrest significantly reduces mortality and improved neurological function (Bernard et al., 2002; Hypothermia After Cardiac Arrest Study Group, 2002). Similarly, in neonates with hypoxic-ischemic encephalopathy, whole-body cooling or selective head cooling resulted in a decrease in basal ganglia and thalamic lesions by MRI (Rutherford et al., 2005); and in a large multicenter trial, infants with neonatal encephalopathy and less severe EEG changes benefitted from head cooling for 72 h, begun within 6 h of birth (rectal temperature 34–35°C), as assessed by death or severe disability at 18 months (Gluckman et al., 2005).
These clinical successes notwithstanding, the application of moderate therapeutic hypothermia to treat patients with acute ischemic stroke has proceeded slowly. In part, this is attributable to a) the increased difficulty and complexity of patient management (e.g., need for intensive care unit setting, sedation, shivering control, possible intubation, cooling-device management); and b) concerns regarding possible adverse events, including pneumonia and (at lower temperatures) cardiac arrhythmias and coagulation disturbances. Recent improvements in shivering management and advances in cooling technology, however, have contributed to making therapeutic hypothermia in stroke patients more feasible at the present time.
Shivering represents a serious “dose-limiting” factor in the clinical application of moderate hypothermia in conscious patients. Oral buspirone (30 mg) and intravenous meperidine (0.4 µg/mL) have been shown to act synergistically to lower the shivering threshold from 35.7°C to 33.4°C while producing only minimal sedation (Mokhtarani et al., 2001; Doufas et al., 2004). When skin-surface warming is used in conjunction with meperidine, the shivering threshold is additively reduced (Kimberger et al., 2007). Buspirone and meperidine plus skin warming were used successfully to reduce the shivering threshold in patients with acute myocardial infarction who received percutaneous coronary intervention and were randomized to endovascular cooling. Target temperatures of 33.2°C were well tolerated (Dixon et al., 2002).
Another major advance is the development, by several companies, of endovascular cooling-catheters that afford rapid induction and precise control of body temperature (Krieger, 2004; Yon et al., 2004; Polderman et al., 2006). In one study, an intravascular heat-exchange catheter placed into the inferior vena cava via the femoral vein achieved average core body-temperature cool-down rates of 4.8°C per hour, tight temperature control to within ±0.1°C, and well-controlled average rewarming rates of 1.9°C per hour (Yon et al., 2004). A related technical advance is the development of hydrogel-coated water-circulating energy-transfer pads that are applied directly to the body; this system can also be used to induce controlled hypothermia (Zweifler et al., 2004) and has been applied to reduce fever burden in the neurological intensive-care setting (Mayer et al., 2004).
The feasibility of applying these approaches to acute stoke patients has now been demonstrated. In one study, 17 awake patients with acute stroke were cooled within 12 h (mean, 3.25 h) to 35.5°C with a forced-air surface-cooling blanket; meperidine was used to control shivering (Kammersgaard et al., 2000). In a second feasibility trial (Cooling for Acute Ischemic Brain Damage – COOL AID), 40 ischemic stroke patients were randomized within 12 hours of symptom onset to hypothermia of 33°C for 24 h via an endovascular cooling device; the procedure was generally well-tolerated (De Georgia et al., 2004). A third group used an endovascular cooling device in the inferior vena cava, plus a combination of buspirone, meperidine and cutaneous warming with a heating blanket to suppress shivering (Guluma et al., 2006). They succeeded in reducing core temperature to a median of 33.4°C within 1.7 h and maintaining hypothermia for 24 h, followed by controlled rewarming, without the need for intubation or neuromuscular blockade.
Several important clinical trials of hypothermia for acute ischemic stroke are currently planned or ongoing (Internet Stroke Center, 2007). A major phase I trial is planning to randomize 130 acute ischemic stroke patients; those arriving within 3 h will receive tPA alone or with cooling; those arriving at 3–6 h will be randomized both to tPA/non-tPA and to cooling/no cooling (Internet Stroke Center, 2007). Follow-up out to 90 days is planned. The cooling methods established in a previous feasibility study will be applied here (Guluma et al., 2006). Another ongoing trial, the Nordic Cooling Stroke Study, plans to randomize 1,000 patients within 6 hours of stroke onset to 35°C cooling for 9 h followed by passive rewarming; outcomes will be assessed at 90 days (Internet Stroke Center, 2007).
2. High-dose human albumin therapy
The use of high-dose human albumin as a neuroprotective agent began with serendipitous observations in the author’s laboratory and was pursued in systematic investigations in rodent ischemia models. Moderate- to high-dose human albumin therapy proved to be highly neuroprotective in animal models of both temporary (Belayev et al., 1997a; Belayev et al., 1998; Belayev et al., 2001) and permanent (Liu et al., 2001) focal cerebral ischemia as well as in global cerebral ischemia (Belayev et al., 1999b) and traumatic brain injury (Belayev et al., 1999a). In focal ischemia, albumin (dose, 1.25 g/kg i.v.) diminished total infarct volume by two-thirds and reduced brain edema by three-quarters or more, with a therapeutic window of full efficacy extending to four hours (Belayev et al., 2001). In a comprehensive meta-analysis of focal ischemia data, albumin-treated rats exhibited ~80% reductions in mean cortical infarct volume (Ginsberg et al., 2004).
Albumin is thought to be neuroprotective by virtue of its multiple salutary actions. It is the plasma’s major antioxidant, antagonizing both endogenous and exogenous sources of oxidative stress (Wayner et al., 1985; Halliwell, 1988). At least three mechanisms are responsible for albumin’s potent antioxidant action: a) its reactive cysteine-34 thiol moiety; b) its ability to bind redox-active transition metals, in particular copper ions, thereby inhibiting copper ion-dependent lipid peroxidation and formation of the highly reactive hydroxyl radical species (Halliwell, 1988); and c) its binding of amphipathic species such as fatty acids and heme, which may participate in injurious redox reactions. Next, albumin maintains plasma colloid oncotic pressure and, in pharmacological doses, induces hemodilution. Albumin also exerts multiple salutary actions on vascular endothelium, helping to maintain normal microvascular permeability (He et al., 1993) and decreasing red blood cell sedimentation under low-flow conditions (Reinhart et al., 1995). Albumin reacts with nitric oxide to form a stable S-nitrosothiol that has endothelium-derived relaxing factor-like properties (Keaney et al., 1993). Albumin also plays a crucial role in binding and transport of fatty acids (Curry et al., 1998). We have shown that albumin reduces ischemic brain swelling (Belayev et al., 1997a; Belayev et al., 1998; Belayev et al., 2001); improves blood flow to critically perfused brain regions (Huh et al., 1998); reduces postischemic thrombosis and blood-element adhesion within the brain’s microvasculature (Belayev et al., 2002); improves microvascular flow velocity within the ischemic cortex (Nimmagadda et al., 2007); and supplies important free fatty acids to the postischemic brain (Rodriguez de Turco et al., 2002).
During 2001–2005, we conducted an NIH-funded pilot clinical trial – the ALIAS (Albumin in Acute Stroke) Pilot Clinical Trial -- in 82 patients at two clinical sites (Palesch et al., 2006; Ginsberg et al., 2006a). This dose-escalation, safety trial treated acute ischemic-stroke subjects within 16 hours of stroke onset with 25% human albumin (ALB) in doses ranging from 0.37 to 2.05 g/kg. One-half of the subjects also received standard-of-care i.v. tPA therapy. At 3 months, the NIHSS, modified Rankin Scale (mRS), and Barthel Index were measured. Albumin therapy was well tolerated; the sole ALB-related adverse event was mild or moderate pulmonary edema in 13.4% of subjects, which was readily managed with diuretics. The 3-month outcome data were analyzed for suggestions of efficacy by comparing the highest three (putatively therapeutic) ALB dose-tiers (1.37–2.05 g/kg) to the lowest three (presumed subtherapeutic) doses (0.34–1.03 g/kg), and to historical cohort data derived from the NINDS rt-PA Stroke Study (National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group, 1995). After adjusting for the tPA effect, the probability of good outcome (defined as modified Rankin Scale 0–1 or NIH Stroke Scale 0–1 at 3 months) at the highest three ALB doses was 81% greater than in the lower dose-tiers (relative benefit, 1.81; 95% CI, 1.11–2.94); and was 95% greater than in the comparable NINDS rt-PA Stroke Study cohort (relative benefit, 1.95; 95% CI, 1.47–2.57) (Palesch et al., 2006). The tPA-treated subjects who received higher-dose ALB were 3 times more likely to achieve a good outcome than subjects receiving lower-dose ALB, suggesting a positive synergistic effect between ALB and tPA (Figure 5).
Figure 5.
Efficacy analysis in ALIAS (Albumin in Acute Stroke) Pilot Trial, comparing modified Rankin scale (mRS) at 3 months in tPA subjects who received lower-dose versus higher-dose albumin treatment. [ Reproduced with permission from (Palesch et al., 2006)].
Based on these encouraging results, the National Institutes of Health has funded a large randomized multicenter placebo-controlled efficacy trial – the ALIAS Phase III Trial. This trial, currently in progress at ~70 clinical sites in North America, consists of two separate but concurrently implemented trials of 900 subjects each: (1) a cohort that receives standard-of-care thrombolytic treatment with intravenous and/or intra-arterial tPA; and (2) a cohort that does not receive tPA therapy. Within each cohort, subjects are randomized in a 1:1 ratio to either 25% human albumin (2.0 g/kg i.v.) or saline placebo; treatment is initiated within 5 hours of stroke onset. To date, 390 subjects have been enrolled. The primary efficacy end-point is either an NIH Stroke Scale (NIHSS) score of 0 or 1, or a modified Rankin Score (mRS) of 0 or 1, or both, at 3 months (Ginsberg et al., 2006b).
3. Hyperacute magnesium therapy
Completed pre-clinical studies and clinical trials of magnesium were reviewed above. Jeffrey Saver and colleagues are continuing to assess magnesium, however, as a prototype of hyperacute neuroprotectant therapy for stroke, initiated prior to hospitalization and without the need for prior CT-scanning. They established the feasibility of this approach in the Field Administration of Stroke Therapy - Magnesium (FAST-MAG Pilot Trial), an open-label trial in which intravenous magnesium sulfate therapy was rapidly initiated by paramedical personnel prior to hospitalization (Saver et al., 2004). Patients with likely stroke were identified by the Los Angeles Prehospital Stroke Screen; the goal was to initiate treatment within 12 hours of symptom onset with a 4g loading dose followed by 16g over 24 h. Twenty patients were enrolled, of whom 80% had ischemic and 20% hemorrhagic strokes. The median time-to-treatment initiation was an impressive 100 min! No serious adverse events were encountered. As part of the effort to accelerate field transport and treatment-initiation, a novel telephonic strategy was developed to obtain informed consent prior to hospitalization (Saver et al., 2006).
A definitive FAST-MAG phase III multicenter efficacy trial is now underway, planned for 1,298 subjects with a 2-hour treatment window. Probable stroke patients (both infarction and hemorrhage) will be randomized to hyperacute treatment with either intravenous MgSO4 or placebo; one-half of subjects will be treated within 1 hour of stroke; and the other half within 1–2 hours. The primary end-point is functional outcome on the modified Rankin scale at 90 days. At this writing, 198 subjects have been enrolled (Internet Stroke Center, 2007; FAST-MAG Trial website, 2007). This effort is laudable. If it fails, it will be due, in all likelihood, to the fact that magnesium (as reviewed above) is a rather weak neuroprotectant.
Parenthetically, an in vitro study from this group (Stewart et al., 2006) has established that MgSO4 concentrations higher than levels targeted in therapeutic stroke trials does not affect tPA-induced fibrinolytic activity; this finding supports the potential suitability of combined therapy with magnesium and tPA in acute stroke.
Some Future-Directed Heuristic Thoughts
Federal vs. corporate-pharmaceutical funding for multicenter neuroprotection trials
It is of interest that all three ongoing clinical-trial efforts discussed above (hypothermia + thrombolysis; albumin; magnesium) are being supported by the National Institutes of Health (ClinicalTrials.gov website, 2007). Indeed, without such support it would be impossible to fund large-scale trials of non-proprietary drugs or procedures. Continued federal support of future trials is therefore essential.
A survey indicated that in the mid-1990’s over one-half of controlled clinical trials for acute stroke were supported by the pharmaceutical industry (Dorman et al., 1999). The problem, succinctly stated by these authors, is “ … drug development strategies adopted by the pharmaceutical industry are likely to address primarily commercial, regulatory, and marketing requirements rather than issues of public health” (Dorman et al., 1999). Considerations of remaining patent-life for proprietary compounds and the pressing need to establish any degree of efficacy (no matter how small) sufficient to garner FDA approval have led to many large-phase clinical trials of products having little pre-clinical promise and tested clinically in a manner not consonant with the product’s pre-clinical characteristics (e.g., therapeutic window, effective dose). The very large per-subject fees offered by many industry-sponsored trials tend to “out-compete” federally sponsored trials, which are typically more modestly funded (Dorman et al., 1999). Publication bias is another major concern in industry-sponsored trials; this may take the form of selective reporting of favorable results, and/or a disinclination to publish or present the results of negative trials (Goldstein et al., 1999). The CONSORT (Consolidated Standards of Reporting Trials) statements address the need to improve the quality of reporting randomized controlled trials (Moher et al., 2001a; Moher et al., 2001b; Piaggio et al., 2006).
Improved translational-medicine strategies and clinical-trial design
Clinical trialists have learned incrementally from the failed trials of the past, and the methodology of recently completed and currently ongoing clinical trials in neuroprotection is vastly improved in many respects. This increased sophistication is likely to continue, and the field of clinical-trial design remains a dynamic, evolving one (Scott et al., 2007).
At the same time, there is a demonstrable need for improvements in the translational path that extends from drug-discovery through pre-clinical development to the clinical trials themselves. A recent thoughtful commentary (Feuerstein et al., 2007) has recommended that there be an in-depth exploration and validation of the molecular targets of compounds under development, including temporal expression and functional profile in relation to the pathophysiology of the disease; and that this include a closer definition of the “scope and time frames” of interaction of the compound with the target (Feuerstein et al., 2007). The implications for clincal-trial design would be a) improved patient selection to target those most susceptible to the treatment in question; and b) selection of more informative and specific clinical outcome measures (Feuerstein et al., 2007). This issue takes on added relevance in view of the fact that, in the case of most agents shown to be neuroprotective in experimental studies, no rigorous scientific evidence is provided to prove that the compound in question was in fact protecting solely (if at all) via its putative mechanism of action.
Combination therapies
Thrombolytic therapy with intravenous tPA is now a standard-of-care for ischemic stroke within the first 3 hours, and ongoing clinical trials are attempting to establish the efficacy of other thrombolytic approaches (Internet Stroke Center, 2007). As ischemic neuroprotection is also likely to be achievable only within a narrow time-window, it is inevitable that neuroprotectants must be evaluated clinically in combination with thrombolysis. This, in fact, is inherent in the design of several major ongoing trials reviewed above (albumin, hypothermia) (ClinicalTrials.gov website, 2007) and has received critical attention in recent reviews (Cheng et al., 2004).
Thinking “outside the box”
Other intriguing futuristic possibilities have received attention. Lipton has suggsted that, in order to have novel neuroprotective agents that are clinically well tolerated, drugs should be developed that are activated by the pathological state that they are intended to inhibit (Lipton, 2007). Others are directing attention to the nascent field of neurorestoration for stroke treatment – i.e., the stimulation of the brain’s endogenous repair mechanisms (Garber, 2007). In this era of increasing molecular and genetic sophistication, unexpected mechanistic breakthroughs are likely to occur.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Aarts MM, Tymianski M. Novel treatment of excitotoxicity: targeted disruption of intracellular signalling from glutamate receptors. Biochem. Pharmacol. 2003;66:877–886. doi: 10.1016/s0006-2952(03)00297-1. [DOI] [PubMed] [Google Scholar]
- 2.Adibhatla RM, Hatcher JF, Dempsey RJ. Phospholipase A2, hydroxyl radicals, and lipid peroxidation in transient cerebral ischemia. Antioxid. Redox. Signal. 2003;5:647–654. doi: 10.1089/152308603770310329. [DOI] [PubMed] [Google Scholar]
- 3.Adibhatla RM, Hatcher JF, Larsen EC, Chen X, Sun D, Tsao FH. CDP-choline significantly restores phosphatidylcholine levels by differentially affecting phospholipase A2 and CTP: phosphocholine cytidylyltransferase after stroke. J. Biol. Chem. 2006;281:6718–6725. doi: 10.1074/jbc.M512112200. [DOI] [PubMed] [Google Scholar]
- 4.Aichner FT, Fazekas F, Brainin M, Polz W, Mamoli B, Zeiler K. Hypervolemic hemodilution in acute ischemic stroke: the Multicenter Austrian Hemodilution Stroke Trial (MAHST) Stroke. 1998;29:743–749. doi: 10.1161/01.str.29.4.743. [DOI] [PubMed] [Google Scholar]
- 5.Albers GW, Atkinson RP, Kelley RE, Rosenbaum DM. Safety, tolerability, and pharmacokinetics of the N-methyl-D-aspartate antagonist dextrorphan in patients with acute stroke. Dextrorphan Study Group. Stroke. 1995;26:254–258. doi: 10.1161/01.str.26.2.254. [DOI] [PubMed] [Google Scholar]
- 6.Albers GW, Goldstein LB, Hall D, Lesko LM. Aptiganel hydrochloride in acute ischemic stroke: a randomized controlled trial. JAMA. 2001;286:2673–2682. doi: 10.1001/jama.286.21.2673. [DOI] [PubMed] [Google Scholar]
- 7.Allen GS, Ahn HS, Preziosi TJ, Battye R, Boone SC, Boone SC, Chou SN, Kelly DL, Weir BK, Crabbe RA, Lavik PJ, Rosenbloom SB, Dorsey FC, Ingram CR, Mellits DE, Bertsch LA, Boisvert DP, Hundley MB, Johnson RK, Strom JA, Transou CR. Cerebral arterial spasm--a controlled trial of nimodipine in patients with subarachnoid hemorrhage. N. Engl. J. Med. 1983;308:619–624. doi: 10.1056/NEJM198303173081103. [DOI] [PubMed] [Google Scholar]
- 8.Alonso de Lecinana M, Gutierrez M, Roda JM, Carceller F, Diez-Tejedor E. Effect of combined therapy with thrombolysis and citicoline in a rat model of embolic stroke. J. Neurol. Sci. 2006;247:121–129. doi: 10.1016/j.jns.2006.03.022. [DOI] [PubMed] [Google Scholar]
- 9.Amemiya S, Kamiya T, Nito C, Inaba T, Kato K, Ueda M, Shimazaki K, Katayama Y. Anti-apoptotic and neuroprotective effects of edaravone following transient focal ischemia in rats. Eur. J. Pharmacol. 2005;516:125–130. doi: 10.1016/j.ejphar.2005.04.036. [DOI] [PubMed] [Google Scholar]
- 10.American Nimodipine Study Group. Clinical trial of nimodipine in acute ischemic stroke. The American Nimodipine Study Group. Stroke. 1992;23:3–8. doi: 10.1161/01.str.23.1.3. [DOI] [PubMed] [Google Scholar]
- 11.Andersen M, Overgaard K, Meden P, Boysen G, Choi SC. Effects of citicoline combined with thrombolytic therapy in a rat embolic stroke model. Stroke. 1999;30:1464–1471. doi: 10.1161/01.str.30.7.1464. [DOI] [PubMed] [Google Scholar]
- 12.Argentino C, Sacchetti ML, Toni D, Savoini G, D'Arcangelo E, Erminio F, Federico F, Milone FF, Gallai V, Gambi D. GM1 ganglioside therapy in acute ischemic stroke. Italian Acute Stroke Study--Hemodilution + Drug. Stroke. 1989;20:1143–1149. doi: 10.1161/01.str.20.9.1143. [DOI] [PubMed] [Google Scholar]
- 13.Aronowski J, Strong R, Grotta JC. Citicoline for treatment of experimental focal ischemia: histologic and behavioral outcome. Neurol. Res. 1996a;18:570–574. doi: 10.1080/01616412.1996.11740473. [DOI] [PubMed] [Google Scholar]
- 14.Aronowski J, Strong R, Grotta JC. Treatment of experimental focal ischemia in rats with lubeluzole. Neuropharmacology. 1996b;35:689–693. doi: 10.1016/0028-3908(96)84640-5. [DOI] [PubMed] [Google Scholar]
- 15.Arundine M, Tymianski M. Molecular mechanisms of glutamate-dependent neurodegeneration in ischemia and traumatic brain injury. Cell Mol. Life Sci. 2004;61:657–668. doi: 10.1007/s00018-003-3319-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ashton D, Willems R, Wynants J, Van RJ, Marrannes R, Clincke G. Altered Na(+)-channel function as an in vitro model of the ischemic penumbra: action of lubeluzole and other neuroprotective drugs. Brain Res. 1997;745:210–221. doi: 10.1016/s0006-8993(96)01094-3. [DOI] [PubMed] [Google Scholar]
- 17.Asplund K. Haemodilution for acute ischaemic stroke. Cochrane. Database. Syst. Rev. 2002 doi: 10.1002/14651858.CD000103. CD000103. [DOI] [PubMed] [Google Scholar]
- 18.Back T. Pathophysiology of the ischemic penumbra--revision of a concept. Cell Mol. Neurobiol. 1998;18:621–638. doi: 10.1023/A:1020629818207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barone FC, Feuerstein GZ. Inflammatory mediators and stroke: new opportunities for novel therapeutics. J Cereb. Blood Flow Metab. 1999;19:819–834. doi: 10.1097/00004647-199908000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Barone FC, Feuerstein GZ, White RF. Brain cooling during transient focal ischemia provides complete neuroprotection. Neurosci. Biobehav. Rev. 1997b;21:31–44. doi: 10.1016/0149-7634(95)00080-1. [DOI] [PubMed] [Google Scholar]
- 21.Barone FC, Feuerstein GZ, White RF. Brain cooling during transient focal ischemia provides complete neuroprotection. Neurosci. Biobehav. Rev. 1997a;21:31–44. doi: 10.1016/0149-7634(95)00080-1. [DOI] [PubMed] [Google Scholar]
- 22.Bazan NG. Lipid signaling in neural plasticity, brain repair, and neuroprotection. Mol. Neurobiol. 2005;32:89–103. doi: 10.1385/MN:32:1:089. [DOI] [PubMed] [Google Scholar]
- 23.Becker DA, Ley JJ, Echegoyen L, Alvarado R. Stilbazulenyl nitrone (STAZN): a nitronyl-substituted hydrocarbon with the potency of classical phenolic chain-breaking antioxidants. J. Am. Chem. Soc. 2002;124:4678–4684. doi: 10.1021/ja011507s. [DOI] [PubMed] [Google Scholar]
- 24.Becker DA, Natero R, Echegoyen L, Lawson RC. Redox behavior of azulenyl nitrones: fully reversible one electron oxidation by cyclic voltammetry at potentials within the range of biological antioxidants. JCS Perkin Trans. 1998;2:1289–1291. [Google Scholar]
- 25.Belayev L, Alonso OF, Huh PW, Zhao W, Busto R, Ginsberg MD. Posttreatment with high-dose albumin reduces histopathological damage and improves neurological deficit following fluid percussion brain injury in rats. J Neurotrauma. 1999a;16:445–453. doi: 10.1089/neu.1999.16.445. [DOI] [PubMed] [Google Scholar]
- 26.Belayev L, Busto R, Zhao W, Clemens JA, Ginsberg MD. Effect of delayed albumin hemodilution on infarction volume and brain edema after transient middle cerebral artery occlusion in rats. J. Neurosurg. 1997a;87:595–601. doi: 10.3171/jns.1997.87.4.0595. [DOI] [PubMed] [Google Scholar]
- 27.Belayev L, Liu Y, Zhao W, Busto R, Ginsberg MD. Human albumin therapy of acute ischemic stroke: marked neuroprotective efficacy at moderate doses and with a broad therapeutic window. Stroke. 2001;32:553–560. doi: 10.1161/01.str.32.2.553. [DOI] [PubMed] [Google Scholar]
- 28.Belayev L, Pinard E, Nallet H, Seylaz J, Liu Y, Riyamongkol P, Zhao W, Busto R, Ginsberg MD. Albumin therapy of transient focal cerebral ischemia: in vivo analysis of dynamic microvascular responses. Stroke. 2002;33:1077–1084. doi: 10.1161/hs0402.105555. [DOI] [PubMed] [Google Scholar]
- 29.Belayev L, Saul I, Huh PW, Finotti N, Zhao W, Busto R, Ginsberg MD. Neuroprotective effect of high-dose albumin therapy against global ischemic brain injury in rats. Brain Res. 1999b;845:107–111. doi: 10.1016/s0006-8993(99)01952-6. [DOI] [PubMed] [Google Scholar]
- 30.Belayev L, Zhao W, Busto R, Ginsberg MD. Transient middle cerebral artery occlusion by intraluminal suture: I. Three-dimensional autoradiographic image-analysis of local cerebral glucose metabolism-blood flow interrelationships during ischemia and early recirculation. J. Cereb. Blood Flow Metab. 1997b;17:1266–1280. doi: 10.1097/00004647-199712000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Belayev L, Zhao W, Pattany PM, Weaver RG, Huh PW, Lin B, Busto R, Ginsberg MD. Diffusion-weighted magnetic resonance imaging confirms marked neuroprotective efficacy of albumin therapy in focal cerebral ischemia. Stroke. 1998;29:2587–2599. doi: 10.1161/01.str.29.12.2587. [DOI] [PubMed] [Google Scholar]
- 32.Benveniste H. The excitotoxin hypothesis in relation to cerebral ischemia. Cerebrovasc Brain Metab Rev. 1991;3:213–245. [PubMed] [Google Scholar]
- 33.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N. Engl. J. Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 34.Billups B, Rossi D, Oshima T, Warr O, Takahashi M, Sarantis M, Szatkowski M, Attwell D. Physiological and pathological operation of glutamate transporters. Prog. Brain Res. 1998;116:45–57. doi: 10.1016/s0079-6123(08)60429-x. 45–57. [DOI] [PubMed] [Google Scholar]
- 35.Bogousslavsky J, Victor SJ, Salinas EO, Pallay A, Donnan GA, Fieschi C, Kaste M, Orgogozo JM, Chamorro A, Desmet A. Fiblast (trafermin) in acute stroke: results of the European-Australian phase II/III safety and efficacy trial. Cerebrovasc. Dis. 2002;14:239–251. doi: 10.1159/000065683. [DOI] [PubMed] [Google Scholar]
- 36.Bonvento G, MacKenzie ET, Edvinsson L. Serotonergic innervation of the cerebral vasculature: relevance to migraine and ischaemia. Brain Res Brain Res Rev. 1991;16:257–263. doi: 10.1016/0165-0173(91)90009-w. [DOI] [PubMed] [Google Scholar]
- 37.Bonventre JV. Roles of phospholipases A2 in brain cell and tissue injury associated with ischemia and excitotoxicity. J Lipid Mediat. Cell Signal. 1997;16:199–208. doi: 10.1016/s0929-7855(97)00014-x. [DOI] [PubMed] [Google Scholar]
- 38.Bordi F, Pietra C, Ziviani L, Reggiani A. The glycine antagonist GV150526 protects somatosensory evoked potentials and reduces the infarct area in the MCAo model of focal ischemia in the rat. Exp. Neurol. 1997;145:425–433. doi: 10.1006/exnr.1997.6442. [DOI] [PubMed] [Google Scholar]
- 39.Bordi F, Terron A, Reggiani A. The neuroprotective glycine receptor antagonist GV150526 does not produce neuronal vacuolization or cognitive deficits in rats. Eur. J. Pharmacol. 1999;378:153–160. doi: 10.1016/s0014-2999(99)00462-8. [DOI] [PubMed] [Google Scholar]
- 40.Bozzi Y, Borrelli E. Dopamine in neurotoxicity and neuroprotection: what do D2 receptors have to do with it? Trends Neurosci. 2006;29:167–174. doi: 10.1016/j.tins.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 41.Bruno V, Battaglia G, Copani A, D'Onofrio M, Di Iorio P, De Blasi A, Melchiorri D, Flor PJ, Nicoletti F. Metabotropic glutamate receptor subtypes as targets for neuroprotective drugs. J Cereb. Blood Flow Metab. 2001;21:1013–1033. doi: 10.1097/00004647-200109000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Buettner GR. The pecking order of free radicals and antioxidants: lipid peroxidation, alpha-tocopherol, and ascorbate. Arch. Biochem Biophys. 1993;300:535–543. doi: 10.1006/abbi.1993.1074. [DOI] [PubMed] [Google Scholar]
- 43.Busto R, Ginsberg MD. The influence of altered brain temperature in cerebral ischemia. 1998:287–307. [Google Scholar]
- 44.Candelise L, Ciccone A. Gangliosides for acute ischaemic stroke. Cochrane. Database. Syst. Rev. 2001 doi: 10.1002/14651858.CD000094. CD000094. [DOI] [PubMed] [Google Scholar]
- 45.Castillo J, Davalos A, Marrugat J, Noya M. Timing for fever-related brain damage in acute ischemic stroke. Stroke. 1998;29:2455–2460. doi: 10.1161/01.str.29.12.2455. [DOI] [PubMed] [Google Scholar]
- 46.Chan PH. Reactive oxygen radicals in signaling and damage in the ischemic brain. J Cereb. Blood Flow Metab. 2001;21:2–14. doi: 10.1097/00004647-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 47.Chan PH, Epstein CJ, Li Y, Huang TT, Carlson E, Kinouchi H, Yang G, Kamii H, Mikawa S, Kondo T. Transgenic mice and knockout mutants in the study of oxidative stress in brain injury. J Neurotrauma. 1995;12:815–824. doi: 10.1089/neu.1995.12.815. [DOI] [PubMed] [Google Scholar]
- 48.Charriaut-Marlangue C, Aggoun-Zouaoui D, Represa A, Ben Ari Y. Apoptotic features of selective neuronal death in ischemia, epilepsy and gp 120 toxicity. Trends Neurosci. 1996;19:109–114. doi: 10.1016/s0166-2236(96)80039-7. [DOI] [PubMed] [Google Scholar]
- 49.Chaulk D, Wells J, Evans S, Jackson D, Corbett D. Long-term effects of clomethiazole in a model of global ischemia. Exp. Neurol. 2003;182:476–482. doi: 10.1016/s0014-4886(03)00121-3. [DOI] [PubMed] [Google Scholar]
- 50.Chen Y, Swanson RA. Astrocytes and brain injury. J Cereb. Blood Flow Metab. 2003;23:137–149. doi: 10.1097/01.WCB.0000044631.80210.3C. [DOI] [PubMed] [Google Scholar]
- 51.Cheng YD, Al-Khoury L, Zivin JA. Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx. 2004;1:36–45. doi: 10.1602/neurorx.1.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chesler M. Failure and function of intracellular pH regulation in acute hypoxic-ischemic injury of astrocytes. Glia. 2005;50:398–406. doi: 10.1002/glia.20141. [DOI] [PubMed] [Google Scholar]
- 53.Choi DW. Calcium: still center-stage in hypoxic-ischemic neuronal death. Trends Neurosci. 1995;18:58–60. [PubMed] [Google Scholar]
- 54.Choi DW, Rothman SM. The role of glutamate neurotoxicity in hypoxic-ischemic neuronal death. Annu. Rev. Neurosci. 1990;13:171–182. doi: 10.1146/annurev.ne.13.030190.001131. 171–182. [DOI] [PubMed] [Google Scholar]
- 55.Clark W, Ertag W, Orecchio E, Raps E. Cervene in acute ischemic stroke: Results of a double-blind, placebo-controlled, dose-comparison study. J. Stroke Cerebrovasc. Dis. 1999a;8:224–230. doi: 10.1016/s1052-3057(99)80071-8. [DOI] [PubMed] [Google Scholar]
- 56.Clark WM, Raps EC, Tong DC, Kelly RE. Cervene (Nalmefene) in acute ischemic stroke : final results of a phase III efficacy study. The Cervene Stroke Study Investigators. Stroke. 2000;31:1234–1239. doi: 10.1161/01.str.31.6.1234. [DOI] [PubMed] [Google Scholar]
- 57.Clark WM, Warach SJ, Pettigrew LC, Gammans RE, Sabounjian LA. A randomized dose-response trial of citicoline in acute ischemic stroke patients. Citicoline Stroke Study Group. Neurology. 1997;49:671–678. doi: 10.1212/wnl.49.3.671. [DOI] [PubMed] [Google Scholar]
- 58.Clark WM, Wechsler LR, Sabounjian LA, Schwiderski UE. A phase III randomized efficacy trial of 2000 mg citicoline in acute ischemic stroke patients. Neurology. 2001;57:1595–1602. doi: 10.1212/wnl.57.9.1595. [DOI] [PubMed] [Google Scholar]
- 59.Clark WM, Williams BJ, Selzer KA, Zweifler RM, Sabounjian LA, Gammans RE. A randomized efficacy trial of citicoline in patients with acute ischemic stroke. Stroke. 1999b;30:2592–2597. doi: 10.1161/01.str.30.12.2592. [DOI] [PubMed] [Google Scholar]
- 60.ClinicalTrials.gov website. U.S. National Institutes of Health. 2007 http://clinicaltrials.gov.
- 61.Colbourne F, Li H, Buchan AM. Indefatigable CA1 sector neuroprotection with mild hypothermia induced 6 hours after severe forebrain ischemia in rats. J. Cereb. Blood Flow Metab. 1999;19:742–749. doi: 10.1097/00004647-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 62.Colbourne F, Sutherland G, Corbett D. Postischemic hypothermia. A critical appraisal with implications for clinical treatment. Mol. Neurobiol. 1997;14:171–201. doi: 10.1007/BF02740655. [DOI] [PubMed] [Google Scholar]
- 63.Corbett D, Thornhill J. Temperature modulation (hypothermic and hyperthermic conditions) and its influence on histological and behavioral outcomes following cerebral ischemia. Brain Pathol. 2000;10:145–152. doi: 10.1111/j.1750-3639.2000.tb00251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Culmsee C, Junker V, Wolz P, Semkova I, Krieglstein J. Lubeluzole protects hippocampal neurons from excitotoxicity in vitro and reduces brain damage caused by ischemia. Eur. J. Pharmacol. 1998;342:193–201. doi: 10.1016/s0014-2999(97)01499-4. [DOI] [PubMed] [Google Scholar]
- 65.Curry S, Mandelkow H, Brick P, Franks N. Crystal structure of human serum albumin complexed with fatty acid reveals an asymmetric distribution of binding sites. Nat. Struct. Biol. 1998;5:827–835. doi: 10.1038/1869. [DOI] [PubMed] [Google Scholar]
- 66.Dalkara T, Endres M, Moskowitz MA. Mechanisms of NO neurotoxicity. Prog. Brain Res. 1998;118:231–239. doi: 10.1016/s0079-6123(08)63211-2. 231–239. [DOI] [PubMed] [Google Scholar]
- 67.Davalos A, Castillo J, Varez-Sabin J, Secades JJ, Mercadal J, Lopez S, Cobo E, Warach S, Sherman D, Clark WM, Lozano R. Oral citicoline in acute ischemic stroke: an individual patient data pooling analysis of clinical trials. Stroke. 2002;33:2850–2857. doi: 10.1161/01.str.0000038691.03334.71. [DOI] [PubMed] [Google Scholar]
- 68.Davis SM, Albers GW, Diener HC, Lees KR, Norris J. Termination of Acute Stroke Studies Involving Selfotel Treatment. ASSIST Steering Committee. Lancet. 1997;349:32. doi: 10.1016/s0140-6736(05)62166-6. [DOI] [PubMed] [Google Scholar]
- 69.Davis SM, Lees KR, Albers GW, Diener HC, Markabi S, Karlsson G, Norris J. Selfotel in acute ischemic stroke : possible neurotoxic effects of an NMDA antagonist. Stroke. 2000;31:347–354. doi: 10.1161/01.str.31.2.347. [DOI] [PubMed] [Google Scholar]
- 70.Dawson DA, Wadsworth G, Palmer AM. A comparative assessment of the efficacy and side-effect liability of neuroprotective compounds inexperimental stroke. Brain Res. 2001;892:344–350. doi: 10.1016/s0006-8993(00)03269-8. [DOI] [PubMed] [Google Scholar]
- 71.De Deyn PP, Reuck JD, Deberdt W, Vlietinck R, Orgogozo JM. Treatment of acute ischemic stroke with piracetam. Members of the Piracetam in Acute Stroke Study (PASS) Group. Stroke. 1997;28:2347–2352. doi: 10.1161/01.str.28.12.2347. [DOI] [PubMed] [Google Scholar]
- 72.De Georgia MA, Krieger DW, bou-Chebl A, Devlin TG, Jauss M, Davis SM, Koroshetz WJ, Rordorf G, Warach S. Cooling for Acute Ischemic Brain Damage (COOL AID): a feasibility trial of endovascular cooling. Neurology. 2004;63:312–317. doi: 10.1212/01.wnl.0000129840.66938.75. [DOI] [PubMed] [Google Scholar]
- 73.De Ryck M, Keersmaekers R, Duytschaever H, Claes C, Clincke G, Janssen M, Van Reet G. Lubeluzole protects sensorimotor function and reduces infarct size in a photochemical stroke model in rats. J. Pharmacol. Exp. Ther. 1996;279:748–758. [PubMed] [Google Scholar]
- 74.De Ryck M, Verhoye M, Van der Linden AM. Diffusion-weighted MRI of infarct growth in a rat photochemical stroke model: effect of lubeluzole. Neuropharmacology. 2000;39:691–702. doi: 10.1016/s0028-3908(99)00176-8. [DOI] [PubMed] [Google Scholar]
- 75.DeGracia DJ, Kumar R, Owen CR, Krause GS, White BC. Molecular pathways of protein synthesis inhibition during brain reperfusion: implications for neuronal survival or death. J Cereb. Blood Flow Metab. 2002;22:127–141. doi: 10.1097/00004647-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 76.DeGracia DJ, Montie HL. Cerebral ischemia and the unfolded protein response. J Neurochem. 2004;91:1–8. doi: 10.1111/j.1471-4159.2004.02703.x. [DOI] [PubMed] [Google Scholar]
- 77.Dehouck MP, Cecchelli R, Richard GA, Renftel M, Lundquist S. In vitro blood-brain barrier permeability and cerebral endothelial cell uptake of the neuroprotective nitrone compound NXY-059 in normoxic, hypoxic and ischemic conditions. Brain Res. 2002;955:229–235. doi: 10.1016/s0006-8993(02)03469-8. [DOI] [PubMed] [Google Scholar]
- 78.del Zoppo GJ, Mabuchi T. Cerebral microvessel responses to focal ischemia. J Cereb. Blood Flow Metab. 2003;23:879–894. doi: 10.1097/01.WCB.0000078322.96027.78. [DOI] [PubMed] [Google Scholar]
- 79.Dewar D, Underhill SM, Goldberg MP. Oligodendrocytes and ischemic brain injury. J Cereb. Blood Flow Metab. 2003;23:263–274. doi: 10.1097/01.WCB.0000053472.41007.F9. [DOI] [PubMed] [Google Scholar]
- 80.Diener HC. Multinational randomised controlled trial of lubeluzole in acute ischaemic stroke. European and Australian Lubeluzole Ischaemic Stroke Study Group. Cerebrovasc. Dis. 1998;8:172–181. doi: 10.1159/000015847. [DOI] [PubMed] [Google Scholar]
- 81.Diener HC, Cortens M, Ford G, Grotta J, Hacke W, Kaste M, Koudstaal PJ, Wessel T. Lubeluzole in acute ischemic stroke treatment: A double-blind study with an 8-hour inclusion window comparing a 10-mg daily dose of lubeluzole with placebo. Stroke. 2000;31:2543–2551. doi: 10.1161/01.str.31.11.2543. [DOI] [PubMed] [Google Scholar]
- 82.Diener HC, Hacke W, Hennerici M, Radberg J, Hantson L, De KJ. Lubeluzole in acute ischemic stroke. A double-blind, placebo-controlled phase II trial. Lubeluzole International Study Group. Stroke. 1996;27:76–81. doi: 10.1161/01.str.27.1.76. [DOI] [PubMed] [Google Scholar]
- 83.Diringer MN. Treatment of fever in the neurologic intensive care unit with a catheter-based heat exchange system. Crit Care Med. 2004;32:559–564. doi: 10.1097/01.CCM.0000108868.97433.3F. [DOI] [PubMed] [Google Scholar]
- 84.Dirnagl U. Bench to bedside: the quest for quality in experimental stroke research. J. Cereb. Blood Flow Metab. 2006;26:1465–1478. doi: 10.1038/sj.jcbfm.9600298. [DOI] [PubMed] [Google Scholar]
- 85.Dirnagl U, Simon RP, Hallenbeck JM. Ischemic tolerance and endogenous neuroprotection. Trends Neurosci. 2003;26:248–254. doi: 10.1016/S0166-2236(03)00071-7. [DOI] [PubMed] [Google Scholar]
- 86.Dixon SR, Whitbourn RJ, Dae MW, Grube E, Sherman W, Schaer GL, Jenkins JS, Baim DS, Gibbons RJ, Kuntz RE, Popma JJ, Nguyen TT, O'Neill WW. Induction of mild systemic hypothermia with endovascular cooling during primary percutaneous coronary intervention for acute myocardial infarction. J. Am. Coll. Cardiol. 2002;40:1928–1934. doi: 10.1016/s0735-1097(02)02567-6. [DOI] [PubMed] [Google Scholar]
- 87.Dorman PJ, Counsell C, Sandercock P. Reports of randomized trials in acute stroke, 1955 to 1995. What proportions were commercially sponsored? Stroke. 1999;30:1995–1998. doi: 10.1161/01.str.30.10.1995. [DOI] [PubMed] [Google Scholar]
- 88.Doufas AG, Sessler DI. Physiology and clinical relevance of induced hypothermia. Neurocrit. Care. 2004;1:489–498. doi: 10.1385/NCC:1:4:489. [DOI] [PubMed] [Google Scholar]
- 89.Duley L, Gulmezoglu AM, Henderson-Smart DJ. Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane. Database. Syst. Rev. 2003 doi: 10.1002/14651858.CD000025. CD000025. [DOI] [PubMed] [Google Scholar]
- 90.Dyker AG, Lees KR. Safety and tolerability of GV150526 (a glycine site antagonist at the N-methyl-D-aspartate receptor) in patients with acute stroke. Stroke. 1999;30:986–992. doi: 10.1161/01.str.30.5.986. [DOI] [PubMed] [Google Scholar]
- 91.EAST Trial. Use of anti-ICAM-1 therapy in ischemic stroke: results of the Enlimomab Acute Stroke Trial. Neurology. 2001;57:1428–1434. doi: 10.1212/wnl.57.8.1428. [DOI] [PubMed] [Google Scholar]
- 92.Edaravone Acute Infarction Study. Effect of a novel free radical scavenger, edaravone (MCI-186), on acute brain infarction. Randomized, placebo controlled, double-blind study at multicenters. Cerebrovasc. Dis. 2003;15:222–229. doi: 10.1159/000069318. [DOI] [PubMed] [Google Scholar]
- 93.Elting JW, Sulter GA, Kaste M, Lees KR, Diener HC, Hommel M, Versavel M, Teelken AW, De KJ. AMPA antagonist ZK200775 in patients with acute ischemic stroke: possible glial cell toxicity detected by monitoring of S-100B serum levels. Stroke. 2002;33:2813–2818. doi: 10.1161/01.str.0000043823.37955.fb. [DOI] [PubMed] [Google Scholar]
- 94.Endres M, Dirnagl U. Ischemia and stroke. Adv. Exp. Med. Biol. 2002;513:455–473. doi: 10.1007/978-1-4615-0123-7_17. 455–473. [DOI] [PubMed] [Google Scholar]
- 95.Endres M, Laufs U, Liao JK, Moskowitz MA. Targeting eNOS for stroke protection. Trends Neurosci. 2004;27:283–289. doi: 10.1016/j.tins.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 96.Erecinska M, Silver IA. Calcium handling by hippocampal neurons under physiologic and pathologic conditions. Adv. Neurol. 1996;71:119–136. 119–136. [PubMed] [Google Scholar]
- 97.Erecinska M, Thoresen M, Silver IA. Effects of hypothermia on energy metabolism in Mammalian central nervous system. J Cereb. Blood Flow Metab. 2003;23:513–530. doi: 10.1097/01.WCB.0000066287.21705.21. [DOI] [PubMed] [Google Scholar]
- 98.Faraci FM, Heistad DD. Regulation of the cerebral circulation: role of endothelium and potassium channels. Physiol Rev. 1998;78:53–97. doi: 10.1152/physrev.1998.78.1.53. [DOI] [PubMed] [Google Scholar]
- 99.FAST-MAG Trial website. 2007 http://www.fastmag.info/p_summ.htm.
- 100.Ferrer I, Planas AM. Signaling of cell death and cell survival following focal cerebral ischemia: life and death struggle in the penumbra. J Neuropathol. Exp. Neurol. 2003;62:329–339. doi: 10.1093/jnen/62.4.329. [DOI] [PubMed] [Google Scholar]
- 101.Feuerstein GZ, Zaleska MM, Krams M, Wang X, Day M, Rutkowski JL, Finklestein SP, Pangalos MN, Poole M, Stiles GL, Ruffolo RR, Walsh FL. Missing steps in the STAIR case: a Translational Medicine perspective on the development of NXY-059 for treatment of acute ischemic stroke. J. Cereb. Blood Flow Metab. 2007:1–3. doi: 10.1038/sj.jcbfm.9600516. online. [DOI] [PubMed] [Google Scholar]
- 102.Fiskum G. Mitochondrial participation in ischemic and traumatic neural cell death. J Neurotrauma. 2000;17:843–855. doi: 10.1089/neu.2000.17.843. [DOI] [PubMed] [Google Scholar]
- 103.Franke CL, Palm R, Dalby M, Schoonderwaldt HC, Hantson L, Eriksson B, Lang-Jenssen L, Smakman J. Flunarizine in stroke treatment (FIST): a double-blind, placebo-controlled trial in Scandinavia and the Netherlands. Acta Neurol. Scand. 1996;93:56–60. doi: 10.1111/j.1600-0404.1996.tb00171.x. [DOI] [PubMed] [Google Scholar]
- 104.Friberg H, Wieloch T. Mitochondrial permeability transition in acute neurodegeneration. Biochimie. 2002;84:241–250. doi: 10.1016/s0300-9084(02)01381-0. [DOI] [PubMed] [Google Scholar]
- 105.Fukunaga K, Kawano T. Akt is a molecular target for signal transduction therapy in brain ischemic insult. J Pharmacol. Sci. 2003;92:317–327. doi: 10.1254/jphs.92.317. [DOI] [PubMed] [Google Scholar]
- 106.Furuya K, Takeda H, Azhar S, McCarron RM, Chen Y, Ruetzler CA, Wolcott KM, DeGraba TJ, Rothlein R, Hugli TE, del Zoppo GJ, Hallenbeck JM. Examination of several potential mechanisms for the negative outcome in a clinical stroke trial of enlimomab, a murine anti-human intercellular adhesion molecule-1 antibody: a bedside-to-bench study. Stroke. 2001;32:2665–2674. doi: 10.1161/hs3211.098535. [DOI] [PubMed] [Google Scholar]
- 107.Gandolfo C, Sandercock P, Conti M. Lubeluzole for acute ischaemic stroke. Cochrane. Database. Syst. Rev. 2002 doi: 10.1002/14651858.CD001924. CD001924- [DOI] [PubMed] [Google Scholar]
- 108.Garber K. Stroke treatment--light at the end of the tunnel? Nat. Biotechnol. 2007;25:838–840. doi: 10.1038/nbt0807-838. [DOI] [PubMed] [Google Scholar]
- 109.Gasche Y, Soccal PM, Kanemitsu M, Copin JC. Matrix metalloproteinases and diseases of the central nervous system with a special emphasis on ischemic brain. Front Biosci. 2006;11:1289–1301. doi: 10.2741/1883. 1289–1301. [DOI] [PubMed] [Google Scholar]
- 110.Gelmers HJ, Gorter K, de Weerdt CJ, Wiezer HJ. A controlled trial of nimodipine in acute ischemic stroke. N. Engl. J. Med. 1988;318:203–207. doi: 10.1056/NEJM198801283180402. [DOI] [PubMed] [Google Scholar]
- 111.Gibson CL, Gray LJ, Murphy SP, Bath PM. Estrogens and experimental ischemic stroke: a systematic review. J Cereb. Blood Flow Metab. 2006;26:1103–1113. doi: 10.1038/sj.jcbfm.9600270. [DOI] [PubMed] [Google Scholar]
- 112.Gidday JM. Cerebral preconditioning and ischaemic tolerance. Nat. Rev. Neurosci. 2006;7:437–448. doi: 10.1038/nrn1927. [DOI] [PubMed] [Google Scholar]
- 113.Gill R. The pharmacology of alpha-amino-3-hydroxy-5-methyl-4-isoxazole propionate (AMPA)/kainate antagonists and their role in cerebral ischaemia. Cerebrovasc Brain Metab Rev. 1994;6:225–256. [PubMed] [Google Scholar]
- 114.Ginsberg MD. Local metabolic responses to cerebral ischemia. Cerebrovasc. Brain Metab. Rev. 1990;2:58–93. [PubMed] [Google Scholar]
- 115.Ginsberg MD. Neuroprotection in brain ischemia -- an update -- Parts I and II. Neuroscientist. 1995;1:95, 164–103. [Google Scholar]
- 116.Ginsberg MD. Life after Cerovive: a personal perspective on ischemic neuroprotection in the post-NXY-059 era. Stroke. 2007;38:1967–1972. doi: 10.1161/STROKEAHA.106.479170. [DOI] [PubMed] [Google Scholar]
- 117.Ginsberg MD, Becker DA, Busto R, Belayev A, Zhang Y, Khoutorova L, Ley JJ, Zhao W, Belayev L. Stilbazulenyl nitrone, a novel antioxidant, is highly neuroprotective in focal ischemia. Ann Neurol. 2003;54:330–342. doi: 10.1002/ana.10659. [DOI] [PubMed] [Google Scholar]
- 118.Ginsberg MD, Belayev L. Biological and molecular mechanisms of hypothermic neuroprotection. 2005:85–140. [Google Scholar]
- 119.Ginsberg MD, Belayev L, Bazan NG, Marcheselli VL, Hill MD, Palesch YY, Khoutorova L, Rodriguez de Turco EB, Ryckborst K, Tamariz D, Busto R. Albumin-based neurotherapeutics for acute ischemic stroke: from bench to bedside. 2004:421–433. [Google Scholar]
- 120.Ginsberg MD, Busto R. Combating hyperthermia in acute stroke: a significant clinical concern. Stroke. 1998a;29:529–534. doi: 10.1161/01.str.29.2.529. [DOI] [PubMed] [Google Scholar]
- 121.Ginsberg MD, Busto R. Small-animal models of global and focal cerebral ischemia. 1998b:14–35. [Google Scholar]
- 122.Ginsberg MD, Hill MD, Palesch YY, Ryckborst KJ, Tamariz D. The ALIAS Pilot Trial: a dose-escalation and safety study of albumin therapy for acute ischemic stroke. I. Physiological responses and safety results. Stroke. 2006a;37:2100–2106. doi: 10.1161/01.STR.0000231388.72646.05. [DOI] [PubMed] [Google Scholar]
- 123.Ginsberg MD, Palesch YY, Hill MD. The ALIAS (ALbumin In Acute Stroke) Phase III randomized multicentre clinical trial: design and progress report. Biochem Soc Trans. 2006b;34:1323–1326. doi: 10.1042/BST0341323. [DOI] [PubMed] [Google Scholar]
- 124.Ginsberg MD, Sternau LL, Globus MY, Dietrich WD, Busto R. Therapeutic modulation of brain temperature: relevance to ischemic brain injury. Cerebrovasc. Brain Metab. Rev. 1992;4:189–225. [PubMed] [Google Scholar]
- 125.Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, Polin RA, Robertson CM, Thoresen M, Whitelaw A, Gunn AJ. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet. 2005;365:663–670. doi: 10.1016/S0140-6736(05)17946-X. [DOI] [PubMed] [Google Scholar]
- 126.Goldstein LB, Brott TG, Kothari RU, Smith WS. Clinical stroke trials: guarding against bias. Stroke. 1999;30:1165–1166. doi: 10.1161/01.str.30.6.1165. [DOI] [PubMed] [Google Scholar]
- 127.Gorelick PB. Neuroprotection in acute ischaemic stroke: a tale of forwhom the bell tolls? Lancet. 2000;355:1925–1926. doi: 10.1016/S0140-6736(00)02318-7. [DOI] [PubMed] [Google Scholar]
- 128.Goslinga H, Eijzenbach V, Heuvelmans JH, van der Laan de Vries, Melis VM, Schmid-Schonbein H, Bezemer PD. Custom-tailored hemodilution with albumin and crystalloids in acute ischemic stroke. Stroke. 1992;23:181–188. doi: 10.1161/01.str.23.2.181. [DOI] [PubMed] [Google Scholar]
- 129.Graham DI. Chapter 4. Hypoxia and vascular disorders. In: Adams JH, Duchen LW, editors. Greenfield's Neuropathology. New York: Oxford University Press; 1992. pp. 153–268. [Google Scholar]
- 130.Graham SH, Chen J. Programmed cell death in cerebral ischemia. J Cereb. Blood Flow Metab. 2001;21:99–109. doi: 10.1097/00004647-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 131.Green AR, Ashwood T, Odergren T, Jackson DM. Nitrones as neuroprotective agents in cerebral ischemia, with particular reference to NXY-059. Pharmacol. Ther. 2003;100:195–214. doi: 10.1016/j.pharmthera.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 132.Greenberg DA, Jin K. Growth factors and stroke. NeuroRx. 2006;3:458–465. doi: 10.1016/j.nurx.2006.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gribkoff VK, Starrett JE, Jr, Dworetzky SI, Hewawasam P, Boissard CG, Cook DA, Frantz SW, Heman K, Hibbard JR, Huston K, Johnson G, Krishnan BS, Kinney GG, Lombardo LA, Meanwell NA, Molinoff PB, Myers RA, Moon SL, Ortiz A, Pajor L, Pieschl RL, Post-Munson DJ, Signor LJ, Srinivas N, Taber MT, Thalody G, Trojnacki JT, Wiener H, Yeleswaram K, Yeola SW. Targeting acute ischemic stroke with a calcium-sensitive opener of maxi-K potassium channels. Nat. Med. 2001;7:471–477. doi: 10.1038/86546. [DOI] [PubMed] [Google Scholar]
- 134.Grotta J. Lubeluzole treatment of acute ischemic stroke. The US and Canadian Lubeluzole Ischemic Stroke Study Group. Stroke. 1997;28:2338–2346. doi: 10.1161/01.str.28.12.2338. [DOI] [PubMed] [Google Scholar]
- 135.Grotta J, Clark W, Coull B, Pettigrew LC, Mackay B, Goldstein LB, Meissner I, Murphy D, LaRue L. Safety and tolerability of the glutamate antagonist CGS 19755 (Selfotel) in patients with acute ischemic stroke. Results of a phase IIa randomized trial. Stroke. 1995;26:602–605. doi: 10.1161/01.str.26.4.602. [DOI] [PubMed] [Google Scholar]
- 136.Guluma KZ, Hemmen TM, Olsen SE, Rapp KS, Lyden PD. A trial of therapeutic hypothermia via endovascular approach in awake patients with acute ischemic stroke: methodology. Acad. Emerg. Med. 2006;13:820–827. doi: 10.1197/j.aem.2006.03.559. [DOI] [PubMed] [Google Scholar]
- 137.Gunn AJ, Battin M, Gluckman PD, Gunn TR, Bennet L. Therapeutic hypothermia: from lab to NICU. J. Perinat. Med. 2005;33:340–346. doi: 10.1515/JPM.2005.061. [DOI] [PubMed] [Google Scholar]
- 138.Gunn AJ, Thoresen M. Hypothermic neuroprotection. NeuroRx. 2006;3:154–169. doi: 10.1016/j.nurx.2006.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Haass A, Kroemer H, Jager H, Muller K, Decker I, Wagner EM, Schimrigk K. [Dextran 40 or HES 200/0.5? Hemorheology of the long-term treatment of ischemic cerebral attacks] Dtsch. Med. Wochenschr. 1986;111:1681–1686. doi: 10.1055/s-2008-1068692. [DOI] [PubMed] [Google Scholar]
- 140.Haley EC, Jr, Thompson JL, Levin B, Davis S, Lees KR, Pittman JG, DeRosa JT, Ordronneau P, Brown DL, Sacco RL. Gavestinel does not improve outcome after acute intracerebral hemorrhage: an analysis from the GAIN International and GAIN Americas studies. Stroke. 2005;36:1006–1010. doi: 10.1161/01.STR.0000163053.77982.8d. [DOI] [PubMed] [Google Scholar]
- 141.Halliwell B. Albumin -- an important extracellular antioxidant? Biochem Pharmacol. 1988;37:569–571. doi: 10.1016/0006-2952(88)90126-8. [DOI] [PubMed] [Google Scholar]
- 142.Hansen AJ. The importance of glutamate receptors in brain ischemia. Adv. Exp. Med. Biol. 1995;363:123–131. doi: 10.1007/978-1-4615-1857-0_14. 123-131. [DOI] [PubMed] [Google Scholar]
- 143.Hartl R, Schurer L, Schmid-Schonbein GW, del Zoppo GJ. Experimental antileukocyte interventions in cerebral ischemia. J Cereb. Blood Flow Metab. 1996;16:1108–1119. doi: 10.1097/00004647-199611000-00004. [DOI] [PubMed] [Google Scholar]
- 144.Haseldonckx M, Van RJ, Van, d V, Wouters L, Borgers M. Protection with lubeluzole against delayed ischemic brain damage in rats. A quantitative histopathologic study. Stroke. 1997;28:428–432. doi: 10.1161/01.str.28.2.428. [DOI] [PubMed] [Google Scholar]
- 145.He P, Curry FE. Albumin modulation of capillary permeability: role of endothelial cell [Ca2+]i. Am. J. Physiol. 1993;265:H74–H82. doi: 10.1152/ajpheart.1993.265.1.H74. [DOI] [PubMed] [Google Scholar]
- 146.Heiss WD. Ischemic penumbra: evidence from functional imaging in man. J Cereb. Blood Flow Metab. 2000;20:1276–1293. doi: 10.1097/00004647-200009000-00002. [DOI] [PubMed] [Google Scholar]
- 147.Heiss WD, Rosner G. Functional recovery of cortical neurons as related to degree and duration of ischemia. Ann. Neurol. 1983;14:294–301. doi: 10.1002/ana.410140307. [DOI] [PubMed] [Google Scholar]
- 148.Hemmen TM, Lyden PD. Induced hypothermia for acute stroke. Stroke. 2007;38:794–799. doi: 10.1161/01.STR.0000247920.15708.fa. [DOI] [PubMed] [Google Scholar]
- 149.Hertz L. Features of astrocytic function apparently involved in the response of central nervous tissue to ischemia-hypoxia. J Cereb. Blood Flow Metab. 1981;1:143–153. doi: 10.1038/jcbfm.1981.17. [DOI] [PubMed] [Google Scholar]
- 150.Horn J, de Haan RJ, Vermeulen M, Limburg M. Very Early Nimodipine Use in Stroke (VENUS): a randomized, double-blind, placebo-controlled trial. Stroke. 2001a;32:461–465. doi: 10.1161/01.str.32.2.461. [DOI] [PubMed] [Google Scholar]
- 151.Horn J, de Haan RJ, Vermeulen M, Luiten PG, Limburg M. Nimodipine in animal model experiments of focal cerebral ischemia: a systematic review. Stroke. 2001b;32:2433–2438. doi: 10.1161/hs1001.096009. [DOI] [PubMed] [Google Scholar]
- 152.Horn J, Limburg M. Calcium antagonists for acute ischemic stroke. Cochrane. Database. Syst. Rev. 2000 doi: 10.1002/14651858.CD001928. CD001928- [DOI] [PubMed] [Google Scholar]
- 153.Hossmann KA. Glutamate-mediated injury in focal cerebral ischemia: the excitotoxin hypothesis revised. Brain Pathol. 1994a;4:23–36. doi: 10.1111/j.1750-3639.1994.tb00808.x. [DOI] [PubMed] [Google Scholar]
- 154.Hossmann KA. Viability thresholds and the penumbra of focal ischemia. Ann. Neurol. 1994b;36:557–565. doi: 10.1002/ana.410360404. [DOI] [PubMed] [Google Scholar]
- 155.Hou ST, MacManus JP. Molecular mechanisms of cerebral ischemia-induced neuronal death. Int. Rev. Cytol. 2002;221:93–148. doi: 10.1016/s0074-7696(02)21011-6. 93–148. [DOI] [PubMed] [Google Scholar]
- 156.Hoyte L, Barber PA, Buchan AM, Hill MD. The rise and fall of NMDA antagonists for ischemic stroke. Curr. Mol. Med. 2004;4:131–136. doi: 10.2174/1566524043479248. [DOI] [PubMed] [Google Scholar]
- 157.Hsu CY, Norris JW, Hogan EL, Bladin P, Dinsdale HB, Yatsu FM, Earnest MP, Scheinberg P, Caplan LR, Karp HR. Pentoxifylline in acute nonhemorrhagic stroke. A randomized, placebo-controlled double-blind trial. Stroke. 1988;19:716–722. doi: 10.1161/01.str.19.6.716. [DOI] [PubMed] [Google Scholar]
- 158.Hudetz AG. Blood flow in the cerebral capillary network: a review emphasizing observations with intravital microscopy. Microcirculation. 1997;4:233–252. doi: 10.3109/10739689709146787. [DOI] [PubMed] [Google Scholar]
- 159.Huh PW, Belayev L, Zhao W, Busto R, Saul I, Ginsberg MD. The effect of high-dose albumin therapy on local cerebral perfusion after transient focal cerebral ischemia in rats. Brain Res. 1998;804:105–113. doi: 10.1016/s0006-8993(98)00674-x. [DOI] [PubMed] [Google Scholar]
- 160.Huh PW, Belayev L, Zhao W, Koch S, Busto R, Ginsberg MD. Comparative neuroprotective efficacy of prolonged moderate intraischemic and postischemic hypothermia in focal cerebral ischemia. J Neurosurg. 2000;92:91–99. doi: 10.3171/jns.2000.92.1.0091. [DOI] [PubMed] [Google Scholar]
- 161.Hurn PD, Macrae IM. Estrogen as a neuroprotectant in stroke. J Cereb. Blood Flow Metab. 2000;20:631–652. doi: 10.1097/00004647-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 162.Hurtado O, Cardenas A, Pradillo JM, Morales JR, Ortego F, Sobrino T, Castillo J, Moro MA, Lizasoain I. A chronic treatment with CDP-choline improves functional recovery and increases neuronal plasticity after experimental stroke. Neurobiol. Dis. 2007;26:105–111. doi: 10.1016/j.nbd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 163.Hurtado O, Moro MA, Cardenas A, Sanchez V, Fernandez-Tome P, Leza JC, Lorenzo P, Secades JJ, Lozano R, Davalos A, Castillo J, Lizasoain I. Neuroprotection afforded by prior citicoline administration in experimental brain ischemia: effects on glutamate transport. Neurobiol. Dis. 2005;18:336–345. doi: 10.1016/j.nbd.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 164.Hypothermia After Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N. Engl. J. Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 165.Iadecola C. Bright and dark sides of nitric oxide in ischemic brain injury. Trends Neurosci. 1997;20:132–139. doi: 10.1016/s0166-2236(96)10074-6. [DOI] [PubMed] [Google Scholar]
- 166.Iadecola C, Pelligrino DA, Moskowitz MA, Lassen NA. Nitric oxide synthase inhibition and cerebrovascular regulation. J Cereb. Blood Flow Metab. 1994;14:175–192. doi: 10.1038/jcbfm.1994.25. [DOI] [PubMed] [Google Scholar]
- 167.Imai H, Masayasu H, Dewar D, Graham DI, Macrae IM. Ebselen protects both gray and white matter in a rodent model of focal cerebral ischemia. Stroke. 2001;32:2149–2154. doi: 10.1161/hs0901.095725. [DOI] [PubMed] [Google Scholar]
- 168.Internet Stroke Center. Stroke Trials Registry. 2007 http://www.strokecenter.org/trials/index.aspx.
- 169.Irving EA, Bamford M. Role of mitogen- and stress-activated kinases in ischemic injury. J Cereb. Blood Flow Metab. 2002;22:631–647. doi: 10.1097/00004647-200206000-00001. [DOI] [PubMed] [Google Scholar]
- 170.Italian Acute Stroke Study Group. Haemodilution in acute stroke: results of the Italian haemodilution trial. Italian Acute Stroke Study Group. Lancet. 1988;1:318–321. [PubMed] [Google Scholar]
- 171.Izumi Y, Roussel S, Pinard E, Seylaz J. Reduction of infarct volume by magnesium after middle cerebral artery occlusion in rats. J. Cereb. Blood Flow Metab. 1991;11:1025–1030. doi: 10.1038/jcbfm.1991.170. [DOI] [PubMed] [Google Scholar]
- 172.Jian LK, Rosenberg GA. Matrix metalloproteinases and free radicals in cerebral ischemia. Free Radic. Biol. Med. 2005;39:71–80. doi: 10.1016/j.freeradbiomed.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 173.Johansson BB. Regeneration and plasticity in the brain and spinal cord. J Cereb. Blood Flow Metab. 2007;27:1417–1430. doi: 10.1038/sj.jcbfm.9600486. [DOI] [PubMed] [Google Scholar]
- 174.Johnson EM, Jr, Greenlund LJ, Akins PT, Hsu CY. Neuronal apoptosis: current understanding of molecular mechanisms and potential role in ischemic brain injury. J Neurotrauma. 1995;12:843–852. doi: 10.1089/neu.1995.12.843. [DOI] [PubMed] [Google Scholar]
- 175.Kammersgaard LP, Rasmussen BH, Jorgensen HS, Reith J, Weber U, Olsen TS. Feasibility and safety of inducing modest hypothermia in awake patients with acute stroke through surface cooling: A case-control study: the Copenhagen Stroke Study. Stroke. 2000;31:2251–2256. doi: 10.1161/01.str.31.9.2251. [DOI] [PubMed] [Google Scholar]
- 176.Kaste M, Fogelholm R, Erila T, Palomaki H, Murros K, Rissanen A, Sarna S. A randomized, double-blind, placebo-controlled trial of nimodipine in acute ischemic hemispheric stroke. Stroke. 1994;25:1348–1353. doi: 10.1161/01.str.25.7.1348. [DOI] [PubMed] [Google Scholar]
- 177.Kazda S, Towart R. Nimodipine: a new calcium antagonistic drug with a preferential cerebrovascular action. Acta Neurochir. (Wien.) 1982;63:259–265. doi: 10.1007/BF01728880. [DOI] [PubMed] [Google Scholar]
- 178.Keaney JFJ, Simon DI, Stamler JS, Jaraki O, Scharfstein J, Vita JA, Loscalzo J. NO forms an adduct with serum albumin that has endothelium-derived relaxing factor-like properties. J Clin Invest. 1993;91:1582–1589. doi: 10.1172/JCI116364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kilpatrick MM, Lowry DW, Firlik AD, Yonas H, Marion DW. Hyperthermia in the neurosurgical intensive care unit. Neurosurgery. 2000;47:850–855. doi: 10.1097/00006123-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 180.Kimberger O, Ali SZ, Markstaller M, Zmoos S, Lauber R, Hunkeler C, Kurz A. Meperidine and skin surface warming additively reduce the shivering threshold: a volunteer study. Crit Care. 2007;11:R29. doi: 10.1186/cc5709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Kirino T. Delayed neuronal death. Neuropathology. 2000;20 Suppl:S95–S97. doi: 10.1046/j.1440-1789.2000.00306.x. [DOI] [PubMed] [Google Scholar]
- 182.Kirino T. Ischemic tolerance. J Cereb. Blood Flow Metab. 2002;22:1283–1296. doi: 10.1097/01.WCB.0000040942.89393.88. [DOI] [PubMed] [Google Scholar]
- 183.Kitano H, Kirsch JR, Hurn PD, Murphy SJ. Inhalational anesthetics as neuroprotectants or chemical preconditioning agents in ischemic brain. J Cereb. Blood Flow Metab. 2007;27:1108–1128. doi: 10.1038/sj.jcbfm.9600410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Koehler RC. Large-animal models of focal and global cerebral ischemia. 1998:36–51. [Google Scholar]
- 185.Kong RS, Butterworth J, Aveling W, Stump DA, Harrison MJ, Hammon J, Stygall J, Rorie KD, Newman SP. Clinical trial of the neuroprotectant clomethiazole in coronary artery bypass graft surgery: a randomized controlled trial. Anesthesiology. 2002;97:585–591. doi: 10.1097/00000542-200209000-00011. [DOI] [PubMed] [Google Scholar]
- 186.Koziol JA, Feng AC. On the analysis and interpretation of outcome measures in stroke clinical trials: lessons from the SAINT I study of NXY-059 for acute ischemic stroke. Stroke. 2006;37:2644–2647. doi: 10.1161/01.STR.0000241106.81293.2b. [DOI] [PubMed] [Google Scholar]
- 187.Krams M, Lees KR, Hacke W, Grieve AP, Orgogozo JM, Ford GA. Acute Stroke Therapy by Inhibition of Neutrophils (ASTIN): an adaptive dose-response study of UK-279,276 in acute ischemic stroke. Stroke. 2003;34:2543–2548. doi: 10.1161/01.STR.0000092527.33910.89. [DOI] [PubMed] [Google Scholar]
- 188.Krieger DW. Radiant Medical Reprieve Endovascular Temperature Therapy System. Neurocrit. Care. 2004;1:205–208. doi: 10.1385/ncc:1:2:205. [DOI] [PubMed] [Google Scholar]
- 189.Kuroda S, Tsuchidate R, Smith ML, Maples KR, Siesjo BK. Neuroprotective effects of a novel nitrone, NXY-059, after transient focal cerebral ischemia in the rat. J. Cereb. Blood Flow Metab. 1999;19:778–787. doi: 10.1097/00004647-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 190.Labiche LA, Grotta JC. Clinical trials for cytoprotection in stroke. NeuroRx. 2004;1:46–70. doi: 10.1602/neurorx.1.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Lapchak PA, Araujo DM, Song D, Wei J, Purdy R, Zivin JA. Effects of the spin trap agent disodium- [(tert-butylimino)methyl]benzene-1,3-disulfonate N-oxide (generic NXY-059) on intracerebral hemorrhage in a rabbit Large clot embolic stroke model: combination studies with tissue plasminogen activator. Stroke. 2002a;33:1665–1670. doi: 10.1161/01.str.0000017145.22806.aa. [DOI] [PubMed] [Google Scholar]
- 192.Lapchak PA, Araujo DM, Song D, Wei J, Zivin JA. Neuroprotective effects of the spin trap agent disodium-[(tert-butylimino)methyl]benzene-1,3-disulfonate N-oxide (generic NXY-059) in a rabbit small clot embolic stroke model: combination studies with the thrombolytic tissue plasminogen activator. Stroke. 2002b;33:1411–1415. doi: 10.1161/01.str.0000015346.00054.8b. [DOI] [PubMed] [Google Scholar]
- 193.Lascola C, Kraig RP. Astroglial acid-base dynamics in hyperglycemic and normoglycemic global ischemia. Neurosci. Biobehav. Rev. 1997;21:143–150. doi: 10.1016/s0149-7634(96)00004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Lees GJ. Pharmacology of AMPA/kainate receptor ligands and their therapeutic potential in neurological and psychiatric disorders. Drugs. 2000;59:33–78. doi: 10.2165/00003495-200059010-00004. [DOI] [PubMed] [Google Scholar]
- 195.Lees KR, Asplund K, Carolei A, Davis SM, Diener HC, Kaste M, Orgogozo JM, Whitehead J. Glycine antagonist (gavestinel) in neuroprotection (GAIN International) in patients with acute stroke: a randomised controlled trial. GAIN International Investigators. Lancet. 2000;355:1949–1954. doi: 10.1016/s0140-6736(00)02326-6. [DOI] [PubMed] [Google Scholar]
- 196.Lees KR, Zivin JA, Ashwood T, Davalos A, Davis SM, Diener HC, Grotta J, Lyden P, Shuaib A, Hardemark HG, Wasiewski WW. NXY-059 for acute ischemic stroke. N. Engl. J. Med. 2006;354:588–600. doi: 10.1056/NEJMoa052980. [DOI] [PubMed] [Google Scholar]
- 197.Leis JA, Bekar LK, Walz W. Potassium homeostasis in the ischemic brain. Glia. 2005;50:407–416. doi: 10.1002/glia.20145. [DOI] [PubMed] [Google Scholar]
- 198.Lenzi GL, Grigoletto F, Gent M, Roberts RS, Walker MD, Easton JD, Carolei A, Dorsey FC, Rocca WA, Bruno R. Early treatment of stroke with monosialoganglioside GM-1. Efficacy and safety results of the Early Stroke Trial. Stroke. 1994;25:1552–1558. doi: 10.1161/01.str.25.8.1552. [DOI] [PubMed] [Google Scholar]
- 199.Lesage AS, Peeters L, Leysen JE. Lubeluzole, a novel long-term neuroprotectant, inhibits the glutamate-activated nitric oxide synthase pathway. J. Pharmacol. Exp. Ther. 1996;279:759–766. [PubMed] [Google Scholar]
- 200.Li H, Buchan AM. Treatment with an AMPA antagonist 12 hours following severe normothermic forebrain ischemia prevents CA1 neuronal injury. J Cereb Blood Flow Metab. 1993;13:933–939. doi: 10.1038/jcbfm.1993.116. [DOI] [PubMed] [Google Scholar]
- 201.Liang D, Dawson TM, Dawson VL. What have genetically engineered mice taught us about ischemic injury? Curr. Mol. Med. 2004;4:207–225. doi: 10.2174/1566524043479194. [DOI] [PubMed] [Google Scholar]
- 202.Lichtenwalner RJ, Parent JM. Adult neurogenesis and the ischemic forebrain. J Cereb. Blood Flow Metab. 2006;26:1–20. doi: 10.1038/sj.jcbfm.9600170. [DOI] [PubMed] [Google Scholar]
- 203.Lipton SA. Pathologically activated therapeutics for neuroprotection. Nat. Rev. Neurosci. 2007;8:803–808. doi: 10.1038/nrn2229. [DOI] [PubMed] [Google Scholar]
- 204.Liu Y, Belayev L, Zhao W, Busto R, Belayev A, Ginsberg MD. Neuroprotective effect of treatment with human albumin in permanent focal cerebral ischemia: histopathology and cortical perfusion studies. Eur. J Pharmacol. 2001;428:193–201. doi: 10.1016/s0014-2999(01)01255-9. [DOI] [PubMed] [Google Scholar]
- 205.Lodder J, van RL, Hilton A, Hardy E, Kessels A. Diazepam to improve acute stroke outcome: results of the early GABA-Ergic activation study in stroke trial. a randomized double-blind placebo-controlled trial. Cerebrovasc. Dis. 2006;21:120–127. doi: 10.1159/000090210. [DOI] [PubMed] [Google Scholar]
- 206.Lyden P, Jacoby M, Schim J, Albers G, Mazzeo P, Ashwood T, Nordlund A, Odergren T. The Clomethiazole Acute Stroke Study in tissue-type plasminogen activator-treated stroke (CLASS-T): final results. Neurology. 2001;57:1199–1205. doi: 10.1212/wnl.57.7.1199. [DOI] [PubMed] [Google Scholar]
- 207.Lyden P, Shuaib A, Ng K, Levin K, Atkinson RP, Rajput A, Wechsler L, Ashwood T, Claesson L, Odergren T, Salazar-Grueso E. Clomethiazole Acute Stroke Study in ischemic stroke (CLASS-I): final results. Stroke. 2002;33:122–128. doi: 10.1161/hs0102.101478. [DOI] [PubMed] [Google Scholar]
- 208.MacKenzie ET, Scatton B. Cerebral circulatory and metabolic effects of perivascular neurotransmitters. CRC Crit Rev. Clin. Neurobiol. 1987;2:357–419. [PubMed] [Google Scholar]
- 209.MacManus JP, Linnik MD. Gene expression induced by cerebral ischemia: an apoptotic perspective. J Cereb. Blood Flow Metab. 1997;17:815–832. doi: 10.1038/aj.jcbfm.9590266. [DOI] [PubMed] [Google Scholar]
- 210.Maiese K, TenBroeke M, Kue I. Neuroprotection of lubeluzole is mediated through the signal transduction pathways of nitric oxide. J. Neurochem. 1997;68:710–714. doi: 10.1046/j.1471-4159.1997.68020710.x. [DOI] [PubMed] [Google Scholar]
- 211.Manley GT, Binder DK, Papadopoulos MC, Verkman AS. New insights into water transport and edema in the central nervous system from phenotype analysis of aquaporin-4 null mice. Neuroscience. 2004;129:983–991. doi: 10.1016/j.neuroscience.2004.06.088. [DOI] [PubMed] [Google Scholar]
- 212.Marinov MB, Harbaugh KS, Hoopes PJ, Pikus HJ, Harbaugh RE. Neuroprotective effects of preischemia intraarterial magnesium sulfate in reversible focal cerebral ischemia. J. Neurosurg. 1996;85:117–124. doi: 10.3171/jns.1996.85.1.0117. [DOI] [PubMed] [Google Scholar]
- 213.Marshall JW, Cross AJ, Jackson DM, Green AR, Baker HF, Ridley RM. Clomethiazole protects against hemineglect in a primate model of stroke. Brain Res. Bull. 2000;52:21–29. doi: 10.1016/s0361-9230(99)00275-0. [DOI] [PubMed] [Google Scholar]
- 214.Marshall JW, Cross AJ, Ridley RM. Functional benefit from clomethiazole treatment after focal cerebral ischemia in a nonhuman primate species. Exp. Neurol. 1999;156:121–129. doi: 10.1006/exnr.1998.6994. [DOI] [PubMed] [Google Scholar]
- 215.Marshall JW, Cummings RM, Bowes LJ, Ridley RM, Green AR. Functional and histological evidence for the protective effect of NXY-059 in a primate model of stroke when given 4 hours after occlusion. Stroke. 2003;34:2228–2233. doi: 10.1161/01.STR.0000087790.79851.A8. [DOI] [PubMed] [Google Scholar]
- 216.Marshall JW, Duffin KJ, Green AR, Ridley RM. NXY-059, a free radical--trapping agent, substantially lessens the functional disability resulting from cerebral ischemia in a primate species. Stroke. 2001;32:190–198. doi: 10.1161/01.str.32.1.190. [DOI] [PubMed] [Google Scholar]
- 217.Mattson MP. Neuroprotective signal transduction: relevance to stroke. Neurosci. Biobehav. Rev. 1997b;21:193–206. doi: 10.1016/s0149-7634(96)00010-3. [DOI] [PubMed] [Google Scholar]
- 218.Mattson MP. Neuroprotective signal transduction: relevance to stroke. Neurosci. Biobehav. Rev. 1997a;21:193–206. doi: 10.1016/s0149-7634(96)00010-3. [DOI] [PubMed] [Google Scholar]
- 219.Mayer SA, Kowalski RG, Presciutti M, Ostapkovich ND, McGann E, Fitzsimmons BF, Yavagal DR, Du YE, Naidech AM, Janjua NA, Claassen J, Kreiter KT, Parra A, Commichau C. Clinical trial of a novel surface cooling system for fever control in neurocritical care patients. Crit Care Med. 2004;32:2508–2515. doi: 10.1097/01.ccm.0000147441.39670.37. [DOI] [PubMed] [Google Scholar]
- 220.Mehta SL, Manhas N, Raghubir R. Molecular targets in cerebral ischemia for developing novel therapeutics. Brain Res Rev. 2007;54:34–66. doi: 10.1016/j.brainresrev.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 221.Meloni BP, Zhu H, Knuckey NW. Is magnesium neuroprotective following global and focal cerebral ischaemia? A review of published studies. Magnes. Res. 2006;19:123–137. [PubMed] [Google Scholar]
- 222.Mergenthaler P, Dirnagl U, Meisel A. Pathophysiology of stroke: lessons from animal models. Metab Brain Dis. 2004;19:151–167. doi: 10.1023/b:mebr.0000043966.46964.e6. [DOI] [PubMed] [Google Scholar]
- 223.Mies G. Autoradiographic and biochemical imaging in cerebral ischemia. Adv. Exp. Med. Biol. 1993;333:273–285. doi: 10.1007/978-1-4899-2468-1_25. 273–285. [DOI] [PubMed] [Google Scholar]
- 224.Minematsu K, Fisher M, Li L, Sotak CH. Diffusion and perfusion magnetic resonance imaging studies to evaluate a noncompetitive N-methyl-D-aspartate antagonist and reperfusion in experimental stroke in rats. Stroke. 1993;24:2074–2081. doi: 10.1161/01.str.24.12.2074. [DOI] [PubMed] [Google Scholar]
- 225.Mir C, Clotet J, Aledo R, Durany N, Argemi J, Lozano R, Cervos-Navarro J, Casals N. CDP-choline prevents glutamate-mediated cell death in cerebellar granule neurons. J. Mol. Neurosci. 2003;20:53–60. doi: 10.1385/JMN:20:1:53. [DOI] [PubMed] [Google Scholar]
- 226.Miyabe M, Kirsch JR, Nishikawa T, Koehler RC, Traystman RJ. Comparative analysis of brain protection by N-methyl-D-aspartate receptor antagonists after transient focal ischemia in cats. Crit Care Med. 1997;25:1037–1043. doi: 10.1097/00003246-199706000-00022. [DOI] [PubMed] [Google Scholar]
- 227.Moher D, Jones A, Lepage L. Use of the CONSORT statement and quality of reports of randomized trials: a comparative before-and-after evaluation. JAMA. 2001a;285:1992–1995. doi: 10.1001/jama.285.15.1992. [DOI] [PubMed] [Google Scholar]
- 228.Moher D, Schulz KF, Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001b;285:1987–1991. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- 229.Mohr JP, Orgogozo JM, Harrison MJG, Hennerici M, Wahlgren NG, Gelmers HJ, Martinez-Vila E, Dycka J, Tettenborn D. Meta-analysis of oral nimodipine trials in acute ischemic stroke. Cerebrovasc. Dis. 1994;4:197–203. [Google Scholar]
- 230.Mokhtarani M, Mahgoub AN, Morioka N, Doufas AG, Dae M, Shaughnessy TE, Bjorksten AR, Sessler DI. Buspirone and meperidine synergistically reduce the shivering threshold. Anesth. Analg. 2001;93:1233–1239. doi: 10.1097/00000539-200111000-00038. [DOI] [PubMed] [Google Scholar]
- 231.Muir KW, Grosset DG, Gamzu E, Lees KR. Pharmacological effects of the non-competitive NMDA antagonist CNS 1102 in normal volunteers. Br. J. Clin. Pharmacol. 1994;38:33–38. doi: 10.1111/j.1365-2125.1994.tb04318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Muir KW, Grosset DG, Lees KR. Clinical pharmacology of CNS 1102 in volunteers. Ann. N. Y. Acad. Sci. 1995;765:279–289. doi: 10.1111/j.1749-6632.1995.tb16585.x. [DOI] [PubMed] [Google Scholar]
- 233.Muir KW, Lees KR, Ford I, Davis S. Magnesium for acute stroke (Intravenous Magnesium Efficacy in Stroke trial): randomised controlled trial. Lancet. 2004;363:439–445. doi: 10.1016/S0140-6736(04)15490-1. [DOI] [PubMed] [Google Scholar]
- 234.Muller WE, Eckert GP, Eckert A. Piracetam: novelty in a unique mode of action. Pharmacopsychiatry. 1999;32 Suppl 1:2–9. doi: 10.1055/s-2007-979230. [DOI] [PubMed] [Google Scholar]
- 235.Mun-Bryce S, Rosenberg GA. Matrix metalloproteinases in cerebrovascular disease. J Cereb. Blood Flow Metab. 1998;18:1163–1172. doi: 10.1097/00004647-199811000-00001. [DOI] [PubMed] [Google Scholar]
- 236.Nakajima H, Kakui N, Ohkuma K, Ishikawa M, Hasegawa T. A newly synthesized poly(ADP-ribose) polymerase inhibitor, DR2313 [2-methyl-3,5,7,8-tetrahydrothiopyrano[4,3-d]-pyrimidine-4-one]: pharmacological profiles, neuroprotective effects, and therapeutic time window in cerebral ischemia in rats. J. Pharmacol. Exp. Ther. 2005;312:472–481. doi: 10.1124/jpet.104.075465. [DOI] [PubMed] [Google Scholar]
- 237.Namura S, Nagata I, Takami S, Masayasu H, Kikuchi H. Ebselen reduces cytochrome c release from mitochondria and subsequent DNA fragmentation after transient focal cerebral ischemia in mice. Stroke. 2001;32:1906–1911. doi: 10.1161/01.str.32.8.1906. [DOI] [PubMed] [Google Scholar]
- 238.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N. Engl. J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 239.Nedergaard M, Dirnagl U. Role of glial cells in cerebral ischemia. Glia. 2005;50:281–286. doi: 10.1002/glia.20205. [DOI] [PubMed] [Google Scholar]
- 240.Nimmagadda A, Park H-P, Prado R, Ginsberg MD. Albumin therapy improves local vascular dynamics in a rat model of primary microvascular thrombosis: a two-photon laser-scanning microscopy study. Stroke. 2007 doi: 10.1161/STROKEAHA.107.495598. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Noraberg J, Poulsen FR, Blaabjerg M, Kristensen BW, Bonde C, Montero M, Meyer M, Gramsbergen JB, Zimmer J. Organotypic hippocampal slice cultures for studies of brain damage, neuroprotection and neurorepair. Curr. Drug Targets. CNS. Neurol. Disord. 2005;4:435–452. doi: 10.2174/1568007054546108. [DOI] [PubMed] [Google Scholar]
- 242.North American GAIN Investigators. Phase II studies of the glycine antagonist GV150526 in acute stroke : the North American experience. The North American Glycine Antagonist in Neuroprotection (GAIN) Investigators. Stroke. 2000;31:358–365. doi: 10.1161/01.str.31.2.358. [DOI] [PubMed] [Google Scholar]
- 243.O'Collins VE, Macleod MR, Donnan GA, Horky LL, van der Worp BH, Howells DW. 1,026 experimental treatments in acute stroke. Ann. Neurol. 2006;59:467–477. doi: 10.1002/ana.20741. [DOI] [PubMed] [Google Scholar]
- 244.Olney JW. Neurotoxicity of NMDA receptor antagonists: an overview. Psychopharmacol. Bull. 1994;30:533–540. [PubMed] [Google Scholar]
- 245.Ovbiagele B, Kidwell CS, Starkman S, Saver JL. Neuroprotective agents for the treatment of acute ischemic stroke. Curr. Neurol. Neurosci. Rep. 2003;3:9–20. doi: 10.1007/s11910-003-0031-z. [DOI] [PubMed] [Google Scholar]
- 246.Palesch YY, Hill MD, Ryckborst KJ, Tamariz D, Ginsberg MD. The ALIAS Pilot Trial: a dose-escalation and safety study of albumin therapy for acute ischemic stroke. II. Neurological outcome and efficacy-analysis. Stroke. 2006;37:2107–2114. doi: 10.1161/01.STR.0000231389.34701.b5. [DOI] [PubMed] [Google Scholar]
- 247.Parnham M, Sies H. Ebselen: prospective therapy for cerebral ischaemia. Expert. Opin. Investig. Drugs. 2000;9:607–619. doi: 10.1517/13543784.9.3.607. [DOI] [PubMed] [Google Scholar]
- 248.Paschen W. Endoplasmic reticulum dysfunction in brain pathology: critical role of protein synthesis. Curr. Neurovasc. Res. 2004;1:173–181. doi: 10.2174/1567202043480125. [DOI] [PubMed] [Google Scholar]
- 249.Paschen W, Doutheil J. Disturbances of the functioning of endoplasmic reticulum: a key mechanism underlying neuronal cell injury? J Cereb. Blood Flow Metab. 1999;19:1–18. doi: 10.1097/00004647-199901000-00001. [DOI] [PubMed] [Google Scholar]
- 250.Pedersen SF, O'Donnell ME, Anderson SE, Cala PM. Physiology and pathophysiology of Na+/H+ exchange and Na+ -K+ -2Cl- cotransport in the heart, brain, and blood. Am. J Physiol Regul. Integr. Comp Physiol. 2006;291:R1–R25. doi: 10.1152/ajpregu.00782.2005. [DOI] [PubMed] [Google Scholar]
- 251.Pellegrini-Giampietro DE, Gorter JA, Bennett MV, Zukin RS. The GluR2 (GluR-B) hypothesis: Ca(2+)-permeable AMPA receptors in neurological disorders. Trends Neurosci. 1997;20:464–470. doi: 10.1016/s0166-2236(97)01100-4. [DOI] [PubMed] [Google Scholar]
- 252.Perez-Pinzon MA. Mechanisms of neuroprotection during ischemic preconditioning: lessons from anoxic tolerance. Comp Biochem. Physiol A Mol. Integr. Physiol. 2007;147:291–299. doi: 10.1016/j.cbpa.2006.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Perez-Pinzon MA, Dave KR, Raval AP. Role of reactive oxygen species and protein kinase C in ischemic tolerance in the brain. Antioxid. Redox. Signal. 2005;7:1150–1157. doi: 10.1089/ars.2005.7.1150. [DOI] [PubMed] [Google Scholar]
- 254.Phillis JW, Horrocks LA, Farooqui AA. Cyclooxygenases, lipoxygenases, and epoxygenases in CNS: their role and involvement in neurological disorders. Brain Res Rev. 2006;52:201–243. doi: 10.1016/j.brainresrev.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 255.Phillis JW, O'Regan MH. The role of phospholipases, cyclooxygenases, and lipoxygenases in cerebral ischemic/traumatic injuries. Crit Rev. Neurobiol. 2003;15:61–90. doi: 10.1615/critrevneurobiol.v15.i1.30. [DOI] [PubMed] [Google Scholar]
- 256.Phillis JW, O'Regan MH. A potentially critical role of phospholipases in central nervous system ischemic, traumatic, and neurodegenerative disorders. Brain Res Brain Res Rev. 2004;44:13–47. doi: 10.1016/j.brainresrev.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 257.Piaggio G, Elbourne DR, Altman DG, Pocock SJ, Evans SJ. Reporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statement. JAMA. 2006;295:1152–1160. doi: 10.1001/jama.295.10.1152. [DOI] [PubMed] [Google Scholar]
- 258.Planas AM, Gorina R, Chamorro A. Signalling pathways mediating inflammatory responses in brain ischaemia. Biochem. Soc. Trans. 2006;34:1267–1270. doi: 10.1042/BST0341267. [DOI] [PubMed] [Google Scholar]
- 259.Polderman KH, Callaghan J. Equipment review: cooling catheters to induce therapeutic hypothermia? Crit Care. 2006;10:234. doi: 10.1186/cc5023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.PubMed. Search string: (neuroprotection [ti] OR neuroprotective [ti]) AND (stroke OR ischemia) 2007 http://www.ncbi.nlm.nih.gov/sites/entrez.
- 261.Read SJ, Parsons AA, Harrison DC, Philpott K, Kabnick K, O'Brien S, Clark S, Brawner M, Bates S, Gloger I, Legos JJ, Barone FC. Stroke genomics: approaches to identify, validate, and understand ischemic stroke gene expression. J Cereb. Blood Flow Metab. 2001;21:755–778. doi: 10.1097/00004647-200107000-00001. [DOI] [PubMed] [Google Scholar]
- 262.Reggiani A, Pietra C, Arban R, Marzola P, Guerrini U, Ziviani L, Boicelli A, Sbarbati A, Osculati F. The neuroprotective activity of the glycine receptor antagonist GV150526: an in vivo study by magnetic resonance imaging. Eur. J. Pharmacol. 2001;419:147–153. doi: 10.1016/s0014-2999(01)00948-7. [DOI] [PubMed] [Google Scholar]
- 263.Reinhart WH, Nagy C. Albumin affects erythrocyte aggregation and sedimentation. Eur. J Clin. Invest. 1995;25:523–528. doi: 10.1111/j.1365-2362.1995.tb01739.x. [DOI] [PubMed] [Google Scholar]
- 264.Reith J, Jorgensen HS, Pedersen PM, Nakayama H, Raaschou HO, Jeppesen LL, Olsen TS. Body temperature in acute stroke: relation to stroke severity, infarct size, mortality, and outcome. Lancet. 1996;347:422–425. doi: 10.1016/s0140-6736(96)90008-2. [DOI] [PubMed] [Google Scholar]
- 265.Rodriguez de Turco EB, Belayev L, Liu Y, Busto R, Parkins N, Bazan NG, Ginsberg MD. Systemic fatty acid responses to transient focal cerebral ischemia: influence of neuroprotectant therapy with human albumin. J. Neurochem. 2002;83:515–524. doi: 10.1046/j.1471-4159.2002.01121.x. [DOI] [PubMed] [Google Scholar]
- 266.Rosenberg GA. Ischemic brain edema. Prog. Cardiovasc. Dis. 1999;42:209–216. doi: 10.1016/s0033-0620(99)70003-4. [DOI] [PubMed] [Google Scholar]
- 267.Rothman SM, Olney JW. Glutamate and the pathophysiology of hypoxic--ischemic brain damage. Ann. Neurol. 1986;19:105–111. doi: 10.1002/ana.410190202. [DOI] [PubMed] [Google Scholar]
- 268.Rutherford MA, Azzopardi D, Whitelaw A, Cowan F, Renowden S, Edwards AD, Thoresen M. Mild hypothermia and the distribution of cerebral lesions in neonates with hypoxic-ischemic encephalopathy. Pediatrics. 2005;116:1001–1006. doi: 10.1542/peds.2005-0328. [DOI] [PubMed] [Google Scholar]
- 269.Sacco RL, DeRosa JT, Haley EC, Jr, Levin B, Ordronneau P, Phillips SJ, Rundek T, Snipes RG, Thompson JL. Glycine antagonist in neuroprotection for patients with acute stroke: GAIN Americas: a randomized controlled trial. JAMA. 2001;285:1719–1728. doi: 10.1001/jama.285.13.1719. [DOI] [PubMed] [Google Scholar]
- 270.Salom JB, Perez-Asensio FJ, Burguete MC, Marin N, Pitarch C, Torregrosa G, Romero FJ, Alborch E. Single-dose ebselen does not afford sustained neuroprotection to rats subjected to severe focal cerebral ischemia. Eur. J. Pharmacol. 2004;495:55–62. doi: 10.1016/j.ejphar.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 271.SASS Trial. Ganglioside GM1 in acute ischemic stroke. The SASS Trial. Stroke. 1994;25:1141–1148. doi: 10.1161/01.str.25.6.1141. [DOI] [PubMed] [Google Scholar]
- 272.Saver JL. Clinical impact of NXY-059 demonstrated in the SAINT I trial: derivation of number needed to treat for benefit over entire range of functional disability. Stroke. 2007;38:1515–1518. doi: 10.1161/01.STR.0000263135.47779.9e. [DOI] [PubMed] [Google Scholar]
- 273.Saver JL, Kidwell C, Eckstein M, Ovbiagele B, Starkman S. Physician-investigator phone elicitation of consent in the field: a novel method to obtain explicit informed consent for prehospital clinical research. Prehosp. Emerg. Care. 2006;10:182–185. doi: 10.1080/10903120500541035. [DOI] [PubMed] [Google Scholar]
- 274.Saver JL, Kidwell C, Eckstein M, Starkman S. Prehospital neuroprotective therapy for acute stroke: results of the Field Administration of Stroke Therapy-Magnesium (FAST-MAG) pilot trial. Stroke. 2004;35:e106–e108. doi: 10.1161/01.STR.0000124458.98123.52. [DOI] [PubMed] [Google Scholar]
- 275.Savitz SI. A critical appraisal of the NXY-059 neuroprotection studies for acute stroke: a need for more rigorous testing of neuroprotective agents in animal models of stroke. Exp. Neurol. 2007;205:20–25. doi: 10.1016/j.expneurol.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 276.Savitz SI, Dinsmore JH, Wechsler LR, Rosenbaum DM, Caplan LR. Cell therapy for stroke. NeuroRx. 2004;1:406–414. doi: 10.1602/neurorx.1.4.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Savitz SI, Fisher M. Future of neuroprotection for acute stroke: in the aftermath of the SAINT trials. Ann. Neurol. 2007;61:396–402. doi: 10.1002/ana.21127. [DOI] [PubMed] [Google Scholar]
- 278.Scandinavian Stroke Study Group. Multicenter trial of hemodilution in acute ischemic stroke. I. Results in the total patient population. Scandinavian Stroke Study Group. Stroke. 1987;18:691–699. doi: 10.1161/01.str.18.4.691. [DOI] [PubMed] [Google Scholar]
- 279.Scandinavian Stroke Study Group. Multicenter trial of hemodilution in acute ischemic stroke. Results of subgroup analyses. Scandinavian Stroke Study Group. Stroke. 1988;19:464–471. doi: 10.1161/01.str.19.4.464. [DOI] [PubMed] [Google Scholar]
- 280.Schabitz WR, Li F, Fisher M. The N-methyl-D-aspartate antagonist CNS 1102 protects cerebral gray and white matter from ischemic injury following temporary focal ischemia in rats. Stroke. 2000;31:1709–1714. doi: 10.1161/01.str.31.7.1709. [DOI] [PubMed] [Google Scholar]
- 281.Schabitz WR, Weber J, Takano K, Sandage BW, Locke KW, Fisher M. The effects of prolonged treatment with citicoline in temporary experimental focal ischemia. J. Neurol. Sci. 1996;138:21–25. doi: 10.1016/0022-510x(95)00341-x. [DOI] [PubMed] [Google Scholar]
- 282.Scheller DK, De Ryck M, Kolb J, Szathmary S, Van Reempts J, Clincke G, Tegtmeier F. Lubeluzole blocks increases in extracellular glutamate and taurine in the peri-infarct zone in rats. Eur. J. Pharmacol. 1997;338:243–251. doi: 10.1016/s0014-2999(97)81927-9. [DOI] [PubMed] [Google Scholar]
- 283.Schilling L, Wahl M. Mediators of cerebral edema. Adv. Exp. Med. Biol. 1999;474:123–141. doi: 10.1007/978-1-4615-4711-2_11. 123–141. [DOI] [PubMed] [Google Scholar]
- 284.Schmidt-Kastner R, Freund TF. Selective vulnerability of the hippocampus in brain ischemia. Neuroscience. 1991;40:599–636. doi: 10.1016/0306-4522(91)90001-5. [DOI] [PubMed] [Google Scholar]
- 285.Schurr A. Neuroprotection against ischemic/hypoxic brain damage: blockers of ionotropic glutamate receptor and voltage sensitive calcium channels. Curr. Drug Targets. 2004;5:603–618. doi: 10.2174/1389450043345209. [DOI] [PubMed] [Google Scholar]
- 286.Scott CT, Baker M. Overhauling clinical trials. Nat. Biotechnol. 2007;25:287–292. doi: 10.1038/nbt0307-287. [DOI] [PubMed] [Google Scholar]
- 287.Scriabine A, Schuurman T, Traber J. Pharmacological basis for the use of nimodipine in central nervous system disorders. FASEB J. 1989;3:1799–1806. [PubMed] [Google Scholar]
- 288.Secades JJ, Frontera G. CDP-choline: pharmacological and clinical review. Methods Find. Exp. Clin. Pharmacol. 1995;17 Suppl B:1–54. [PubMed] [Google Scholar]
- 289.Sena E, Wheble P, Sandercock P, Macleod M. Systematic review and meta-analysis of the efficacy of tirilazad in experimental stroke. Stroke. 2007;38:388–394. doi: 10.1161/01.STR.0000254462.75851.22. [DOI] [PubMed] [Google Scholar]
- 290.Serebruany VL. Hypokalemia, cardiac failure, and reporting NXY-059 safety for acute stroke. J. Cardiovasc. Pharmacol. Ther. 2006;11:229–231. doi: 10.1177/1074248406297311. [DOI] [PubMed] [Google Scholar]
- 291.Sharp FR, Liu J, Bernabeu R. Neurogenesis following brain ischemia. Brain Res Dev. Brain Res. 2002;134:23–30. doi: 10.1016/s0165-3806(01)00286-3. [DOI] [PubMed] [Google Scholar]
- 292.Sharp FR, Lu A, Tang Y, Millhorn DE. Multiple molecular penumbras after focal cerebral ischemia. J Cereb. Blood Flow Metab. 2000;20:1011–1032. doi: 10.1097/00004647-200007000-00001. [DOI] [PubMed] [Google Scholar]
- 293.Sharp FR, Massa SM, Swanson RA. Heat-shock protein protection. Trends Neurosci. 1999;22:97–99. doi: 10.1016/s0166-2236(98)01392-7. [DOI] [PubMed] [Google Scholar]
- 294.Shuaib A, Lees KR, Lyden P, Grotta J, Davalos A, Davis SM, Diener HC, Ashwood T, Wasiewski WW, Emeribe U. NXY-059 for the treatment of acute ischemic stroke. N. Engl. J. Med. 2007;357:562–571. doi: 10.1056/NEJMoa070240. [DOI] [PubMed] [Google Scholar]
- 295.Siesjo BK. Brain Energy Metabolism. Chichester: John Wiley and Sons; 1978. [Google Scholar]
- 296.Siesjo BK. Cell damage in the brain: a speculative synthesis. J Cereb. Blood Flow Metab. 1981;1:155–185. doi: 10.1038/jcbfm.1981.18. [DOI] [PubMed] [Google Scholar]
- 297.Siesjo BK. Pathophysiology and treatment of focal cerebral ischemia. Part I: Pathophysiology. J Neurosurg. 1992;77:169–184. doi: 10.3171/jns.1992.77.2.0169. [DOI] [PubMed] [Google Scholar]
- 298.Siesjo BK, Bengtsson F. Calcium fluxes, calcium antagonists, and calcium-related pathology in brain ischemia, hypoglycemia, and spreading depression: a unifying hypothesis. J Cereb. Blood Flow Metab. 1989;9:127–140. doi: 10.1038/jcbfm.1989.20. [DOI] [PubMed] [Google Scholar]
- 299.Simard JM, Kent TA, Chen M, Tarasov KV, Gerzanich V. Brain oedema in focal ischaemia: molecular pathophysiology and theoretical implications. Lancet Neurol. 2007;6:258–268. doi: 10.1016/S1474-4422(07)70055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Simon R, Shiraishi K. N-methyl-D-aspartate antagonist reduces stroke size and regional glucose metabolism. Ann. Neurol. 1990;27:606–611. doi: 10.1002/ana.410270604. [DOI] [PubMed] [Google Scholar]
- 301.STAIR. Recommendations for standards regarding preclinical neuroprotective and restorative drug development. Stroke. 1999;30:2752–2758. doi: 10.1161/01.str.30.12.2752. [DOI] [PubMed] [Google Scholar]
- 302.Stenzel-Poore MP, Stevens SL, King JS, Simon RP. Preconditioning reprograms the response to ischemic injury and primes the emergence of unique endogenous neuroprotective phenotypes: a speculative synthesis. Stroke. 2007;38:680–685. doi: 10.1161/01.STR.0000251444.56487.4c. [DOI] [PubMed] [Google Scholar]
- 303.Stewart D, Marder VJ, Starkman S, Saver JL. Magnesium sulfate neither potentiates nor inhibits tissue plasminogen activator-induced thrombolysis. J. Thromb. Haemost. 2006;4:1575–1579. doi: 10.1111/j.1538-7836.2006.01999.x. [DOI] [PubMed] [Google Scholar]
- 304.Strijbos PJ. Nitric oxide in cerebral ischemic neurodegeneration and excitotoxicity. Crit Rev. Neurobiol. 1998;12:223–243. doi: 10.1615/critrevneurobiol.v12.i3.40. [DOI] [PubMed] [Google Scholar]
- 305.Stys PK. Anoxic and ischemic injury of myelinated axons in CNS white matter: from mechanistic concepts to therapeutics. J Cereb. Blood Flow Metab. 1998;18:2–25. doi: 10.1097/00004647-199801000-00002. [DOI] [PubMed] [Google Scholar]
- 306.Sugawara T, Chan PH. Reactive oxygen radicals and pathogenesis of neuronal death after cerebral ischemia. Antioxid. Redox. Signal. 2003;5:597–607. doi: 10.1089/152308603770310266. [DOI] [PubMed] [Google Scholar]
- 307.Sughrue ME, Connolly ES., Jr Effectively bridging the preclinical/clinical gap: the results of the ASTIN trial. Stroke. 2004;35:e81–e82. doi: 10.1161/01.STR.0000121164.29117.44. [DOI] [PubMed] [Google Scholar]
- 308.Swanson RA, Ying W, Kauppinen TM. Astrocyte influences on ischemic neuronal death. Curr. Mol. Med. 2004;4:193–205. doi: 10.2174/1566524043479185. [DOI] [PubMed] [Google Scholar]
- 309.Sydserff SG, Borelli AR, Green AR, Cross AJ. Effect of NXY-059 on infarct volume after transient or permanent middle cerebral artery occlusion in the rat; studies on dose, plasma concentration and therapeutic time window. Br. J. Pharmacol. 2002;135:103–112. doi: 10.1038/sj.bjp.0704449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Sydserff SG, Cross AJ, Green AR. The neuroprotective effect of chlormethiazole on ischaemic neuronal damage following permanent middle cerebral artery ischaemia in the rat. Neurodegeneration. 1995a;4:323–328. doi: 10.1016/1055-8330(95)90022-5. [DOI] [PubMed] [Google Scholar]
- 311.Sydserff SG, Cross AJ, West KJ, Green AR. The effect of chlormethiazole on neuronal damage in a model of transient focal ischaemia. Br. J. Pharmacol. 1995b;114:1631–1635. doi: 10.1111/j.1476-5381.1995.tb14950.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Takahashi M, Kohara A, Shishikura J, Kawasaki-Yatsugi S, Ni JW, Yatsugi S, Sakamoto S, Okada M, Shimizu-Sasamata M, Yamaguchi T. YM872: a selective, potent and highly water-soluble alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptor antagonist. CNS. Drug Rev. 2002;8:337–352. doi: 10.1111/j.1527-3458.2002.tb00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Takasago T, Peters EE, Graham DI, Masayasu H, Macrae IM. Neuroprotective efficacy of ebselen, an anti-oxidant with anti-inflammatory actions, in a rodent model of permanent middle cerebral artery occlusion. Br. J. Pharmacol. 1997;122:1251–1256. doi: 10.1038/sj.bjp.0701426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Tazaki Y, Sakai F, Otomo E, Kutsuzawa T, Kameyama M, Omae T, Fujishima M, Sakuma A. Treatment of acute cerebral infarction with a choline precursor in a multicenter double-blind placebo-controlled study. Stroke. 1988;19:211–216. doi: 10.1161/01.str.19.2.211. [DOI] [PubMed] [Google Scholar]
- 315.The RANTTAS Investigators. A randomized trial of tirilazad mesylate in patients with acute stroke (RANTTAS). The RANTTAS Investigators. Stroke. 1996;27:1453–1458. doi: 10.1161/01.str.27.9.1453. [DOI] [PubMed] [Google Scholar]
- 316.Tirilazad International Steering Committee. Tirilazad mesylate in acute ischemic stroke: A systematic review. Tirilazad International Steering Committee. Stroke. 2000;31:2257–2265. doi: 10.1161/01.str.31.9.2257. [DOI] [PubMed] [Google Scholar]
- 317.Trendelenburg G, Dirnagl U. Neuroprotective role of astrocytes in cerebral ischemia: focus on ischemic preconditioning. Glia. 2005;50:307–320. doi: 10.1002/glia.20204. [DOI] [PubMed] [Google Scholar]
- 318.TRUST Study Group. Randomised, double-blind, placebo-controlled trial of nimodipine in acute stroke. Trust Study Group. Lancet. 1990;336:1205–1209. [PubMed] [Google Scholar]
- 319.Turner AJ, Nalivaeva NN. New insights into the roles of metalloproteinases in neurodegeneration and neuroprotection. Int. Rev. Neurobiol. 2007;82:113–135. doi: 10.1016/S0074-7742(07)82006-X. 113–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Tymianski M, Tator CH. Normal and abnormal calcium homeostasis in neurons: a basis for the pathophysiology of traumatic and ischemic central nervous system injury. Neurosurgery. 1996;38:1176–1195. doi: 10.1097/00006123-199606000-00028. [DOI] [PubMed] [Google Scholar]
- 321.van der Worp HB, de Haan P, Morrema E, Kalkman CJ. Methodological quality of animal studies on neuroprotection in focal cerebral ischaemia. J Neurol. 2005;252:1108–1114. doi: 10.1007/s00415-005-0802-3. [DOI] [PubMed] [Google Scholar]
- 322.van der Worp HB, Kappelle LJ, Algra A, Bar PR, Orgogozo JM, Ringelstein EB, Bath PM, van GJ. The effect of tirilazad mesylate on infarct volume of patients with acute ischemic stroke. Neurology. 2002;58:133–135. doi: 10.1212/wnl.58.1.133. [DOI] [PubMed] [Google Scholar]
- 323.Wahlgren NG, MacMahon DG, DeKeyser J, Indredavik B, Ryman T. Intravenous Nimodipine West European Stroke Trial (INWEST) of nimodipine in the treatment of acute ischaemic stroke. Cerebrovasc. Dis. 1994;4:204–210. [Google Scholar]
- 324.Wahlgren NG, Ranasinha KW, Rosolacci T, Franke CL, van Erven PM, Ashwood T, Claesson L. Clomethiazole acute stroke study (CLASS): results of a randomized, controlled trial of clomethiazole versus placebo in 1360 acute stroke patients. Stroke. 1999;30:21–28. doi: 10.1161/01.str.30.1.21. [DOI] [PubMed] [Google Scholar]
- 325.Wang Q, Tang XN, Yenari MA. The inflammatory response in stroke. J Neuroimmunol. 2007;184:53–68. doi: 10.1016/j.jneuroim.2006.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Wang Y, Lim LL, Levi C, Heller RF, Fisher J. Influence of admission body temperature on stroke mortality. Stroke. 2000;31:404–409. doi: 10.1161/01.str.31.2.404. [DOI] [PubMed] [Google Scholar]
- 327.Warach S, Kaufman D, Chiu D, Devlin T, Luby M, Rashid A, Clayton L, Kaste M, Lees KR, Sacco R, Fisher M. Effect of the Glycine Antagonist Gavestinel on cerebral infarcts in acute stroke patients, a randomized placebo-controlled trial: The GAIN MRI Substudy. Cerebrovasc. Dis. 2006;21:106–111. doi: 10.1159/000090208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Warach S, Pettigrew LC, Dashe JF, Pullicino P, Lefkowitz DM, Sabounjian L, Harnett K, Schwiderski U, Gammans R. Effect of citicoline on ischemic lesions as measured by diffusion-weighted magnetic resonance imaging. Citicoline 010 Investigators. Ann. Neurol. 2000;48:713–722. [PubMed] [Google Scholar]
- 329.Warner DS, Sheng H, Batinic-Haberle I. Oxidants, antioxidants and the ischemic brain. J Exp. Biol. 2004;207:3221–3231. doi: 10.1242/jeb.01022. [DOI] [PubMed] [Google Scholar]
- 330.Wass CT, Lanier WL. Glucose modulation of ischemic brain injury: review and clinical recommendations. Mayo Clin. Proc. 1996;71:801–812. doi: 10.1016/S0025-6196(11)64847-7. [DOI] [PubMed] [Google Scholar]
- 331.Watanabe T, Yuki S, Egawa M, Nishi H. Protective effects of MCI-186 on cerebral ischemia: possible involvement of free radical scavenging and antioxidant actions. J. Pharmacol. Exp. Ther. 1994;268:1597–1604. [PubMed] [Google Scholar]
- 332.Waxman SG, Ransom BR, Stys PK. Non-synaptic mechanisms of Ca(2+)-mediated injury in CNS white matter. Trends Neurosci. 1991;14:461–468. doi: 10.1016/0166-2236(91)90046-w. [DOI] [PubMed] [Google Scholar]
- 333.Wayner DD, Burton GW, Ingold KU, Locke S. Quantitative measurement of the total, peroxyl radical-trapping antioxidant capability of human blood plasma by controlled peroxidation. The important contribution made by plasma proteins. FEBS Lett. 1985;187:33–37. doi: 10.1016/0014-5793(85)81208-4. [DOI] [PubMed] [Google Scholar]
- 334.Weiss GB. Metabolism and actions of CDP-choline as an endogenous compound and administered exogenously as citicoline. Life Sci. 1995;56:637–660. doi: 10.1016/0024-3205(94)00427-t. [DOI] [PubMed] [Google Scholar]
- 335.Westermaier T, Zausinger S, Baethmann A, Schmid-Elsaesser R. Dose finding study of intravenous magnesium sulphate in transient focal cerebral ischemia in rats. Acta Neurochir. (Wien. ) 2005;147:525–532. doi: 10.1007/s00701-005-0496-4. [DOI] [PubMed] [Google Scholar]
- 336.Wieloch T. Neurochemical correlates to selective neuronal vulnerability. Prog. Brain Res. 1985;63:69–85. doi: 10.1016/S0079-6123(08)61976-7. 69–85. [DOI] [PubMed] [Google Scholar]
- 337.Wieloch T, Bergstedt K, Hu BR. Protein phosphorylation and the regulation of mRNA translation following cerebral ischemia. Prog. Brain Res. 1993;96:179–191. doi: 10.1016/s0079-6123(08)63266-5. 179–191. [DOI] [PubMed] [Google Scholar]
- 338.Wilby MJ, Hutchinson PJ. The pharmacology of chlormethiazole: a potential neuroprotective agent? CNS. Drug Rev. 2004;10:281–294. doi: 10.1111/j.1527-3458.2004.tb00028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Winblad B. Piracetam: a review of pharmacological properties and clinical uses. CNS. Drug Rev. 2005;11:169–182. doi: 10.1111/j.1527-3458.2005.tb00268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Witlin AG, Sibai BM. Magnesium sulfate therapy in preeclampsia and eclampsia. Obstet. Gynecol. 1998;92:883–889. doi: 10.1016/s0029-7844(98)00277-4. [DOI] [PubMed] [Google Scholar]
- 341.Wu D. Neuroprotection in experimental stroke with targeted neurotrophins. NeuroRx. 2005;2:120–128. doi: 10.1602/neurorx.2.1.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Xiong ZG, Chu XP, Simon RP. Acid sensing ion channels--novel therapeutic targets for ischemic brain injury. Front Biosci. 2007;12:1376–1386. doi: 10.2741/2154. [DOI] [PubMed] [Google Scholar]
- 343.Xue D, Huang ZG, Barnes K, Lesiuk HJ, Smith KE, Buchan AM. Delayed treatment with AMPA, but not NMDA, antagonists reduces neocortical infarction. J Cereb Blood Flow Metab. 1994;14:251–261. doi: 10.1038/jcbfm.1994.32. [DOI] [PubMed] [Google Scholar]
- 344.Yamaguchi T, Sano K, Takakura K, Saito I, Shinohara Y, Asano T, Yasuhara H. Ebselen in acute ischemic stroke: a placebo-controlled, double-blind clinical trial. Ebselen Study Group. Stroke. 1998;29:12–17. doi: 10.1161/01.str.29.1.12. [DOI] [PubMed] [Google Scholar]
- 345.Yang Y, Li Q, Ahmad F, Shuaib A. Survival and histological evaluation of therapeutic window of post-ischemia treatment with magnesium sulfate in embolic stroke model of rat. Neurosci. Lett. 2000;285:119–122. doi: 10.1016/s0304-3940(00)01048-x. [DOI] [PubMed] [Google Scholar]
- 346.Yon S, Magers M, Dobak J, Klos B. A novel system for mild hypothermia. Biomed. Instrum. Technol. 2004;38:241–246. doi: 10.2345/0899-8205(2004)38[241:ANSFMH]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 347.Young C, Tenkova T, Dikranian K, Olney JW. Excitotoxic versus apoptotic mechanisms of neuronal cell death in perinatal hypoxia/ischemia. Curr. Mol. Med. 2004;4:77–85. doi: 10.2174/1566524043479158. [DOI] [PubMed] [Google Scholar]
- 348.Yrjanheikki J, Keinanen R, Pellikka M, Hokfelt T, Koistinaho J. Tetracyclines inhibit microglial activation and are neuroprotective in global brain ischemia. Proc. Natl. Acad. Sci. U. S. A. 1998;95:15769–15774. doi: 10.1073/pnas.95.26.15769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Zhang F, Yin W, Chen J. Apoptosis in cerebral ischemia: executional and regulatory signaling mechanisms. Neurol. Res. 2004;26:835–845. doi: 10.1179/016164104X3824. [DOI] [PubMed] [Google Scholar]
- 350.Zhang N, Komine-Kobayashi M, Tanaka R, Liu M, Mizuno Y, Urabe T. Edaravone reduces early accumulation of oxidative products and sequential inflammatory responses after transient focal ischemia in mice brain. Stroke. 2005a;36:2220–2225. doi: 10.1161/01.STR.0000182241.07096.06. [DOI] [PubMed] [Google Scholar]
- 351.Zhang RL, Chopp M, Jiang N, Tang WX, Prostak J, Manning AM, Anderson DC. Anti-intercellular adhesion molecule-1 antibody reduces ischemic cell damage after transient but not permanent middle cerebral artery occlusion in the Wistar rat. Stroke. 1995;26:1438–1442. doi: 10.1161/01.str.26.8.1438. [DOI] [PubMed] [Google Scholar]
- 352.Zhang RL, Zhang ZG, Chopp M. Neurogenesis in the adult ischemic brain: generation, migration, survival, and restorative therapy. Neuroscientist. 2005b;11:408–416. doi: 10.1177/1073858405278865. [DOI] [PubMed] [Google Scholar]
- 353.Zhao H, Sapolsky RM, Steinberg GK. Phosphoinositide-3-kinase/akt survival signal pathways are implicated in neuronal survival after stroke. Mol. Neurobiol. 2006;34:249–270. doi: 10.1385/MN:34:3:249. [DOI] [PubMed] [Google Scholar]
- 354.Zhao W, Belayev L, Ginsberg MD. Transient middle cerebral artery occlusion by intraluminal suture: II. Neurological deficits, and pixel-based correlation of histopathology with local blood flow and glucose utilization. J. Cereb. Blood Flow Metab. 1997;17:1281–1290. doi: 10.1097/00004647-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 355.Zhao Z, Cheng M, Maples KR, Ma JY, Buchan AM. NXY-059, a novel free radical trapping compound, reduces cortical infarction after permanent focal cerebral ischemia in the rat. Brain Res. 2001;909:46–50. doi: 10.1016/s0006-8993(01)02618-x. [DOI] [PubMed] [Google Scholar]
- 356.Zweifler RM, Voorhees ME, Mahmood MA, Parnell M. Rectal temperature reflects tympanic temperature during mild induced hypothermia in nonintubated subjects. J. Neurosurg. Anesthesiol. 2004;16:232–235. doi: 10.1097/00008506-200407000-00008. [DOI] [PubMed] [Google Scholar]