Summary
Rudimentary horn pregnancy is a rare obstetric entity and the diagnosis and management may pose some problems especially in a low-resource center. We report our experience in diagnosing and managing a case of fetal death in a rudimentary horn.
Keywords: rudimentary horn, pre-rupture, pregnancy, tourniquet
Case Report
Madam CA was a 28 years old gravida 6 para 5. She presented to Korle Bu Teaching hospital with a complaint of vaginal bleeding of two days duration. She did not remember the exact date of her last menstrual period but she believed she was six months pregnant. The vaginal bleeding was associated with lower abdominal pain. She had not booked for antenatal care in this pregnancy. All her previous deliveries were spontaneous vaginal deliveries at term.
On examination, she looked well with a pulse rate of 88 beats per minute and a blood pressure of 130/70mmHg. There was a mass arising from the pelvis corresponding to the size of a 16-week pregnancy. The surface was smooth, mildly tender and not mobile. The cervix was firm, 2.5cm long, posterior and the os was closed. There were no adnexal masses felt and the mass was not displaced to either side. There was no active vaginal bleeding. A speculum examination did not reveal any cervical or vaginal pathology. A clinical impression of threatened abortion was formed.
A transabdominal ultrasound scan was performed and the findings were as follows: single intrauterine pregnancy, no fetal heart activity, reduced liquor volume, femur length 2.2cm and gestation age 16weeks. Her haemoglobin was 11.2g/dl, platelet count was 320 × 109/L, and the clotting profile was normal.
Labour was induced with 200mcg of misoprostol in the posterior vaginal fornix, 6 hourly for a total of four doses. This was however, unsuccessful on two different occasions, 48 hours apart. There were no complications associated with the attempts at induction of labour. Based on the two failed attempts at induction of labour, extrauterine pregnancy was suspected. A repeat trans-abdominal ultrasound scan could not conclusively confirm or rule out an extrauterine pregnancy. Transvaginal ultrasound scan, MRI and CT scan were not readily available for further investigation of the patient. A size 18 Foley catheter was passed into the uterine cavity and the balloon inflated with 10mls of normal saline. The bladder was also filled with about 250mls of normal saline. Trans-abdominal ultrasound scan examination was then repeated. On this occasion, the fetus was seen to be outside the uterine cavity and the diagnosis of extrauterine pregnancy was confirmed. Madam CA was counselled and prepared for laparotomy which was performed under general anaesthesia.
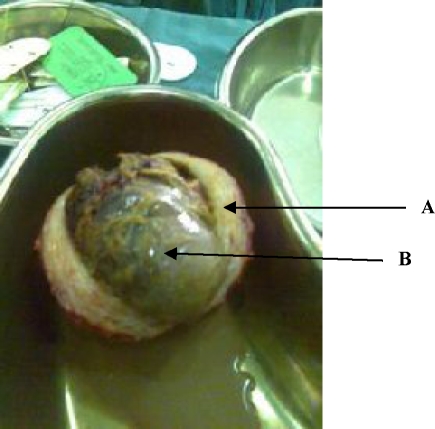
The findings at surgery were: a slightly bulky uterus, a pregnant left rudimentary horn which was attached to the whole length of the body of the uterus, both tubes and ovarieswere normal (figure 1). On palpation, both kidneys were in their normal positions and were of normal size.
Figure 1.
Pregnant rudimentary horn (in the hand of the assistant) still attached to the main horn. The left ovarian ligament and tube have been clamped and cut from the rudimentary horn. (A) Pregnant rudimentary horn (B) Left ovary (C) Uterus
The left tube, ovarian ligament, and round ligament were clamped cut and transfixed. A size 18 Foley catheter (used as a tourniquet) was then placed around the uterus at the level of the isthmus, pulled tightly and clamped with a medium-size artery forceps. On the right the catheter passed over the infundibulo-pelvic ligament but below the tube. On the left, it passed through the defect in the broad ligament and below the lowest part of the rudimentary horn. The rudimentary horn was then excised from the main uterus with a scalpel. There was no communication between the rudimentary horn and the main uterus. The defect on the uterus was repaired in two layers. The tourniquet was then removed. Ipsilateral salpingectomy was performed. The estimated blood loss was 200ml.
The postoperative recovery was uneventful. Her hemoglobin on postoperative day five was 11g/dl. She was counseled on family planning and given a referral to the family planning clinic. She was also educated on the need for antenatal care and elective caesarean section for any future pregnancy. The stitches were removed and she was discharged on the ninth postoperative day. Intravenous urography was requested and she was to bring the report during her follow-up visit. She was scheduled for review in two weeks but she defaulted and did not come for follow-up.
Histopathology report
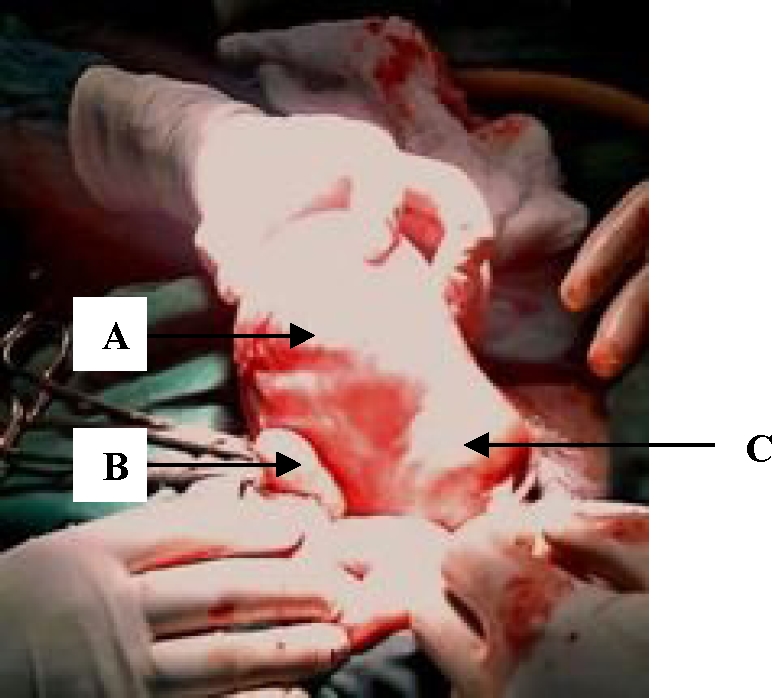
The gross specimen measured 110×90×50mm. Sectioning showed a fetus with a crown-rump length of 120mm. Sections showed normal villi within a thickened smooth muscle cavity. Few endometrial glands and stroma were seen within the muscle layer. The findings were consistent with ectopic (uterine horn) gestation.
Discussion
Unicornuate uterus with a rudimentary horn is a mullerian duct malformation. The incidence of mullerian duct malformations in the general population is estimated to be 4.3% while that of unicornuate uterus is about 0.4%.1 Rudimentary horn pregnancy occurs in approximately 1/76 000 to 1/150 000 pregnancies.2,3 The literature is replete with case reports on pregnancy in the rudimentary horn with different outcomes. However, a search of the literature did not yield any such reports from West Africa. In the past, majority of cases were diagnosed after rupture of the rudimentary horn. However, with the advent of investigative methods such as ultrasound scan, CT scan, MRI, and laparoscopy, the diagnosis is more often being made before rupture. There have even been reports of first trimester prerupture diagnosis of rudimentary horn pregnancy.4
In the case of Madam CA, the diagnosis was not suspected on ultrasound scan therefore induction of labour was attempted. Even when the diagnosis was suspected clinically, other methods of confirmation such as CT scan and MRI could not be used because they were not readily available.
The placement of a Foley catheter into the uterine cavity prior to performing a transabdominal ultrasound scan is obviously not a preferred method of diagnosing an extrauterine pregnancy but it has proved to be a useful and cheap way of excluding an intrauterine pregnancy. This method has been used by others to confirm an extrauterine pregnancy which proved to be a rudimentary horn pregnancy at laparotomy.5
Although the incidence of rudimentary horn pregnancy is relatively small, the risk of serious maternal morbidity and mortality is high. Early prerupture diagnosis is therefore very important. The following criteria have been suggested by Tsafri et al for sonographic diagnosis of rudimentary horn pregnancy4: (1) pseudopattern of an asymmetrical bicornuate uterus, (2) absent visual continuity between the cervical canal and the lumen of the pregnant horn, and (3) the presence of myometrial tissue surrounding the gestational sac.
Additionally, hypervascularization typical to placenta accreta may support the diagnosis of rudimentary horn pregnancy. This feature can be diagnosed with colour flow Doppler and power Doppler sonography.
The attachment of the rudimentary horn to the main uterus varies from a fibro-muscular band to an extensive fusion between the two horns where there is no external separation between them. The latter was the type of attachment found in the case of Madam CA. Resecting the rudimentary horn from the main horn in this case was bound to provoke significant blood loss. It was for this reason that a tourniquet was applied at the level of the uterine isthmus in such a way that the contra lateral ovarian vessels as well as the uterine vessels were compressed by the tourniquet. When the rudimentary horn pregnancy is small and facilities exist, it may be possible to resect it laparoscopically.4 Others have described the administration of methotrexate for termination of an early pregnancy in a rudimentary horn followed by elective laparoscopic resection.6
In conclusion, this case report has highlighted the need for high level of suspicion for this rare but very important complication of pregnancy. It has also shown that in low-resource centers, placement of a Foley catheter into the uterine cavity and performing a transabdominal ultrasound scan can conclusively exclude an intrauterine pregnancy. Lastly, we suggest the use of a tourniquet in selected cases of rudimentary horn pregnancy where there is extensive fusion between the two horns. This approach can prevent excessive blood loss and avert the need for blood transfusion.
Figure 2.
Sectioned rudimentary horn showing conceptus in intact membranes. (A) Sectioned rudimentary horn (B) Fetus in intact membranes
References
- 1.Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update. 2001;7:161–174. doi: 10.1093/humupd/7.2.161. [DOI] [PubMed] [Google Scholar]
- 2.Ural SH, Artal R. Third-trimester rudimentary horn pregnancy. A case report. J Reprod Med. 1998;37:919–921. [PubMed] [Google Scholar]
- 3.Nahum GG. Rudimentary uterine horn pregnancy. A case report on surviving twins delivered eight days apart. J Reprod Med. 1997;42:525–532. [PubMed] [Google Scholar]
- 4.Tsafrir A, Rojansky N, Sela HY, Gomori JM, Nadjari M. Rudimentary horn pregnancy: first-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med. 2005;(2):219–223. doi: 10.7863/jum.2005.24.2.219. [DOI] [PubMed] [Google Scholar]
- 5.Chopra S, Suri V, Aggarwal N. Rudimentary horn pregnancy: Prerupture diagnosis and management. Indian J Med Sci. 2007;61:28–29. [PubMed] [Google Scholar]
- 6.Edelman AB, Jensen JT, Lee DM, Nichols MD. Successful medical abortion of a Pregnancy within a noncommunicating rudimentary uterine horn. Am J Obstet Gynecol. 2003;189(3):886–887. doi: 10.1067/s0002-9378(03)00121-2. [DOI] [PubMed] [Google Scholar]