Abstract
Background
In 2005, following several years of declining efficacy of chloroquine, the Ministry of Health recommended the use of Amodiaquine/Artesunate combination therapy for the treatment of uncomplicated malaria. A system of continuous monitoring of therapeutic responses has been established in 10 district hospitals across the country. The data gathered will enable National Malaria Control Programme (NMCP) to respond to changes in the efficacy of the new treatment in a timely manner.
Objectives
To determine the 28 day therapeutic efficacy of Amodiaquine/Artesunate (AQ/AS) combination treatment in children with uncomplicated malaria in Ghana.
Methods
Children aged 6 – 59 months attending clinic with signs/symptoms of uncomplicated malaria at 9 district hospitals (3 in each of the 3 eco-epidemiological zones of the country) were eligible for enrolment. Enrolled children were followed up after treatment for a total of 28 days to record the clinical and parasitological resolution of their malaria episode as well as any adverse drug reactions.
Results
Treatment resulted in rapid and complete cure in almost all the children; 99.3% 14 days after treatment and 93.0%, 28 days after treatment. The majority of treatment failures on D28 were seen in the 3 sites located in the forest zones (Sunyani, Bekwai and Begoro). There was no case of Early Treatment Failure at both D14 and D28 assessments. Adverse events (AE's) were minimal, less than 4%, with the most common complaint being vomiting.
Conclusion
AQ/AS combination for uncomplicated malaria is efficacious and safe in children less than 5 years.
Keywords: Efficacy, Artemisinin-based Combination Therapy (ACTs), Uncomplicated malaria, Artesunate, Amodiaquine
Introduction
Malaria remains a major cause of morbidity and mortality in Ghana, accounting for approximately 50% of Out Patient attendances and 20% of deaths in children under 5 years.1 Malaria control in Ghana relies on early and prompt treatment of suspected cases (fevers), a strategy threatened by the emergence and spread of Plasmodium falciparum resistance to commonly used animalaria drugs such as chloroquine and sulfadoxine/pyrimethamine (first and second line antimalaria drugs prior to 2005). Such resistance has contributed to increase in child mortality in some countries.2
Chloroquine resistance was first reported in Ghana in 1986 and gradually increased3, 4, 5 so that by 2003 parasitological responses to chloroquine were less than 50% in some areas of the country.5 Similar studies on the efficacy of sulfadoxine/pyrimethamine (SP) have shown 0–36% of RII resistance and 0-9% of RIII resistance. 6,7 This pattern of P. falciparum resistance to chloroquine and other commonly used mono-therapies has become widespread in sub-Sahara Africa.8,9,10
The World Health Organization recently recommended the use of arteminisin-based combination therapy (ACT) for the treatment of uncomplicated P. falciparum malaria. It is believed that this will provide effective treatment against P. falciparum malaria and slow down the spread of drug resistance.11 Artemisinin compounds when used in combination with a longer acting antimalarial rapidly reduce parasite densities to low levels at a time when drug levels of the longer acting drug are still maximal, thereby reducing the likelihood of parasites being exposed to suboptimal levels of the longer acting drug and limiting the emergence of resistant strains.12
The National Malaria Control Programme, (NMCP) after a thorough examination of the available evidence and, in consultation with stake holders recommended the use of Amodiaquine/Artesunate (AQ/AS) for the treatment of uncomplicated malaria in the country beginning January 1st 2005. The new treatment was rolled out to the regions and districts during the first half of 2005. In order not to be caught unawares regarding changes in parasite susceptibility to the drug, the sentinel sites used in collecting data on the declining efficacy of chloroquine were maintained and increased to 10 to provide continuous data on the responses to treatment. In September 2005 a programme to monitor the new treatment at 9 out of the 10 sentinel sites across the country was instituted. The primary objective was to determine the therapeutic efficacy of the AQ/AS in the treatment of uncomplicated malaria in children less than 5 years of age and to set up a system of data collection on the efficacy of the new treatment to guide the NMCP in its continuous evaluation of the treatment policy. This report is a preliminary analysis of the data on therapeutic efficacy of AQ/AS obtained from the sentinel sites between September 2005 and December 2006.
Subjects and Methods
Study sites and population
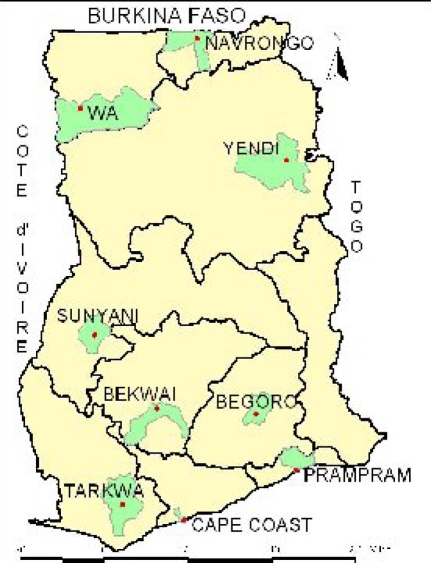
The study was conducted at nine district hospitals across the country namely, Begoro, Bekwai, Cape Coast, Navrongo, Prampram, Sunyani, Tarkwa, Wa and. Yendi (Figure 1).
Figure 1.
Map of Ghana showing the 9 study districts (shaded green)
A tenth site, Hohoe, did not provide data because of an ongoing randomized trial in the district. These sites were chosen in order that we obtained data from all 3 eco-epidemiological zones of the country.
Children aged 6–59 months presenting at the Out-Patient Department (OPD) of a study site clinic with symptoms and signs suggestive of malaria were reviewed by the study nurse. Once a clinical diagnosis of malaria was made, a blood sample was drawn for smear for malaria parasites and to determine the haemoglobin level. Children meeting the inclusion criteria, detailed below, were recruited into the study and followed up for a minimum of 14 days and a maximum of 28 days.
Inclusion Criteria
Axillary temperature >= 37.5°C
Mono infection with P. falciparum
Parasite count ranging between 2×103 and 200×103 per µl
Haemoglobin level > 5g/dl
No severe malaria
Parental informed consent
Malaria was diagnosed by light microscopy of thick and thin blood smears. The thick and thin blood smears were stained with 3% Giemsa for 30 minutes. Parasite density was determined by counting the number of asexual parasites per 200 white blood cells, and calculated per µL assuming a white blood cell count of 8000 cells per µL. Sexual parasite count was done per 1,000 white blood cells. A smear was declared negative when the examination of 100 thick-film fields did not reveal the presence of asexual parasites. Quality control checks were performed on a random 10% sample of blood films, examined at an independent site.
Children received 10mg/kg body weight of AQ daily and 4mg/kg of AS daily (given as a single dose) over 3 days. All treatments were given under direct observation and children were observed for 30minutes after drug administration to ensure that they retained the medication. Children who vomited within the 30 minute observation period received a repeated full dose of the medication. Patients with repeated vomiting were excluded from the study. All patients were allowed use of antipyretics. The rescue drug used was Quinine given orally according to national treatment guidelines. Patients who showed signs/symptoms of severe malaria, had serious adverse events or required blood transfusion were withdrawn.
Children were followed up at the OPD on days 1, 2, 3, 7, 14, 21, and 28 after treatment (day of treatment was counted as Day 0) with a morbidity questionnaire as well as a physical examination. Information on symptoms, temperature, and pulse rate were recorded on the Case Record Form (CRF). Parasitaemia levels (asexual and sexual) were assessed on each follow-up day and on any day the child had fever. Filter paper blood blots were obtained on day 0, and at recurrence of parasitaemia for PCR genotyping, and using merozoite surface proteins 1 and 2 (MSP1, MSP2), and glutamate-rich protein (GLURP) to distinguish between re-infection and recrudescence (To be analysed and reported in final paper).
Data Analysis
Clinical responses on Day 14 and Day 28 were classified based on the WHO 2002 criteria, as : Early Treatment Failure (ETF), Late Clinical Failure (LCF), Late Parasitological Failure (LPF) or Adequate Clinical and Parasitological Response (ACPR).13 Trends for fever and parasite clearance, as well as haematological responses, were also analysed.
Ethics
The Institutional Review Board of the Noguchi Memorial Institute for Medical Research, University of Ghana, reviewed and approved the study. Each mother/care giver was informed of the objectives, methods, anticipated benefits and potential hazards of the study. They were also informed that they were at liberty to withdraw their children from the study at any time without penalty. In particular, mothers/care givers were informed that the treatment the child would receive was not dependent on whether or not the child participated in the study.
Results
Baseline characteristics
Of the 1193 children screened, 545 (45.7%) qualified to be enrolled into the study, of whom 540 (99.1%) reached a study endpoint. Five hundred and six (92.8%) were assessed on Day 14 and 498 (91.4%) on Day 28 days. The majority of children who did not complete study procedures had travelled out of the study area (73%) and in substantial number of these; this prevented them from completing the full course of treatment. The median age of study children was 26 months and the male: female ratio was 1:1. The geometric mean parasite density (min, max) at enrolment was 35,793/µl (167: 881,765).
Primary outcomes
Amodiaquine/Artesunate combination gave good clinical and parasitological cure rates at all the study sites. Adequate Clinical and Parasitological Response (ACPR) (95% CI) on Day 28 was 92.8% (90.1, 94.9) and varied from 87% in Begoro to 100% in Tarkwa. There was no case of Early Treatment Failure (ETF). Late Clinical Failure (LCF) and Late Parasitological Failure (LPF) accounted for 2.7% (1.5, 4.6) and 4.5% (2.9, 6.8), respectively, of all the treatment outcomes (Table 1). There was no difference in the cure rates between young children (less than 24 months) and those older than 24 months or among males and females. Assessed at 14 days post treatment, only 1% of children failed treatment (1 case of LCF and 3 cases of LPF seen at Bekwai, Cape Coast and Wa) (Table 2).
Table 1.
Clinical and Parasitological Responses 28 days post treatment
| District | Clinical and Parasitological Responses | Total | |||||
| ACPR | LCF | LPF | |||||
| N | (%) | N | (%) | N | (%) | ||
| Begoro | 60 | (87.0%) | 4 | (5.8%) | 5 | (7.2%) | 69 |
| Bekwai | 62 | (87.4%) | 5 | (7.0%) | 4 | (5.6%) | 71 |
| Cape Coast | 73 | (96.1%) | 1 | (1.3%) | 2 | (2.6%) | 76 |
| Navrongo | 79 | (98.7%) | 0 | (0%) | 1 | (1.3%) | 80 |
| Prampram | 10 | (100%) | 0 | (0%) | 0 | (0%) | 10 |
| Sunyani | 37 | (97.4%) | 0 | (0%) | 1 | (2.6%) | 38 |
| Tarkwa | 4 | (100%) | 0 | (0%) | 0 | (0%) | 4 |
| Wa | 66 | (88.0%) | 4 | (5.3%) | 5 | (6.7%) | 75 |
| Yendi | 72 | (96.1%) | 1 | (1.3%) | 2 | (2.6%) | 75 |
| Total | 463 | (93.0%) | 15 | (3.0%) | 20 | (4.0%) | 498 |
Table 2.
Clinical and Parasitological Responses 14 days post treatment
| District | Clinical and Parasitological Responses | Total | |||||
| ACPR | LCF | LPF | |||||
| N | (%) | N | (%) | N | (%) | ||
| Begoro | 69 | (98.6%) | 1 | (1.4%) | 0 | (0%) | 70 |
| Bekwai | 71 | (98.6%) | 1 | (1.4%) | 0 | (0%) | 72 |
| Cape Coast | 77 | (98.7%) | 1 | (1.3%) | 0 | (0%) | 78 |
| Navrongo | 80 | (100%) | 0 | (0%) | 0 | (0%) | 80 |
| Prampram | 11 | (100%) | 0 | (0%) | 0 | (0%) | 11 |
| Sunyani | 40 | (100%) | 0 | (0%) | 0 | (0%) | 40 |
| Tarkwa | 4 | 100.0%) | 0 | (0%) | 0 | (0%) | 4 |
| Wa | 73 | (97.3%) | 2 | (2.7%) | 0 | (0%) | 75 |
| Yendi | 76 | (100%) | 0 | (0%) | 0 | (0%) | 76 |
| Total | 501 | (99.0%) | 5 | (1.0%) | 0 | (0%) | 506 |
Secondary outcomes
The resolution of fever was rapid after commencement of treatment with only 2% being febrile at Day 2. Parasite clearance was also rapid, and rates of clearance remained high after treatment. Only 4.2% of children were found to have asexual parasites 28 days after commencement of treatment. Both fever resolution and parasite clearance rates did not differ by study site or gender.
There were significant improvements in the mean haemoglobin (Hb) concentration 14 and 28 days post treatment over the enrolment mean Hb. Overall, the mean Hb at enrolment, 9.58 (9.41, 9.75) improved to 10.15 (10.0, 10.3) on Day 14 (p < 0.01), and to 10.96 (10.82, 11.09) on Day 28 (p < 0.001) among study subjects. This improvement was also seen among the various treatment outcome groups, with the greatest improvement seen in those who had Adequate Clinical and Parasitological Response. However, at each follow up visit, there were no significant differences in the mean Hb concentrations between the various treatment outcome groups (Table 3).
Table 3.
Treatment responses and changes in mean Haemoglobin concentration
| Day of Observation | Therapeutic Response | |||
| LCF N = 12 |
LPF N = 20 |
ACPR N = 446 |
P value | |
| D0 Mean (95% CI) | 9.35 (8.20, 10.50) | 9.77 (9.07, 10.47) | 9.58 (9.40, 9.75) | NS |
| D14 Mean (95% CI) | 10.0 (9.07, 10.93) | 10.13 (9.44, 10.81) | 10.16 (10.0, 10.31) | NS |
| D28 Mean (95% CI) | 10.7 (9.37, 12.03) | 10.92 (10.13, 11.71) | 10.96 (10.82, 11.10) | NS |
Safety of treatment regimen
There were 21 episodes of vomiting seen in 12 children within 72 hours after any treatment. All episodes occurred outside the 30 minute observation period after treatment and therefore did not warrant removal of the children from the study. No other adverse events were reported.
Discussion
Following the reports and documentation of reduced efficacy of chloroquine in the treatment of uncomplicated malaria in the late 1990's and the first half of this decade3,5, the National Malaria Control Programme (NMCP), recommended the use of AQ/AS combination therapy for the treatment of uncomplicated malaria in 2005.
We show in this preliminary report that AQ/AS combination therapy, resulted in rapid, high clinical and parasitological cure rates in children in the first full year of implementation. Almost all children monitored (99.8%) had cleared their parasites by Day 3 and the cure rates remained at more than 90% throughout the 28 days of follow up. The treatment was effective at all the study sites and did not differ by gender. The reported treatment responses compares very well with previous reports on the use of AQ/AS combination therapy in several clinical trials conducted on the continent before the introduction of the treatment regime in Ghana.14, 15
This report shows that the improved efficacies reported in those trials still persist and the current regimen should provide improved outcomes following treatment of uncomplicated malaria. Haematological recovery was significantly improved in all children following treatment. This may be attributed to the rapid clearance of parasites, and thus, relieving the pressure on both red blood cells and the bone marrow resulting from the infection.16 The relatively quick action of the combination, complete clearance of parasitaemia in more than 99% of children treated, if combined with a programme of judicious use of the treatment regimen, should slow the emergence of resistance parasites overall.
There is the need for the continued monitoring of treatment responses in the country in order to detect early cases of treatment failure. The 28 day monitoring is laborious and difficult to interpret in high transmission areas such as Ghana. Consideration should therefore be given to developing simplified surveillance protocols to enable the NMCP obtain good but credible data from routine reports from the clinics. A systematic reading of smears on D3 for example should be able to quickly inform the programme of problems if responses fall substantially below the current rate of 99%. Indeed such abbreviated protocol has recently been proposed for the malaria control programme in Colombia.17
In conclusion, there is evidence to show that a year after the roll out of the new treatment programme, the response to treatment is very good, the drug effects quick parasite clearance and provides improved haematological recovery, and the safety profile remains good among children. Since more than 90% of clinical cases occur in children, the choice of AQ/AS for the treatment of uncomplicated malaria is well grounded.
Acknowledgements
The authors acknowledge the contributions of Dr. George Amofa (Director of Public Health, Ghana Health Service), Dr. Constance Bart Plange (National Malaria Control Programme Manager), and project staff at all the district hospitals in following up children and collecting the data. We also wish to thank Messrs John Fenteng, Daniel Ahulu, Charles Attiogbe, and Maxwell Christian Osei-Bonsu of the Epidemiology Department, Noguchi Memorial Institute for technical assistance. The monitoring of treatment responses is supported by the National Malaria Control Programme with funds from the Global Fund for Tuberculosis, AIDS and Malaria and a grant from the IAEA, Project RAF 6025.
References
- 1.Anti Malaria Drug Treatment Policy. National Malaria Control Programme (GHS/MOH) 2004
- 2.Trape JF, Pison G, Preziosi MP, Enel C, Desgrees du Lou A, Delaunay V. Impact of chloroquine resistance on malaria mortality. Comptes Rendus Acad Sci III. 1998;321:689–697. doi: 10.1016/s0764-4469(98)80009-7. [DOI] [PubMed] [Google Scholar]
- 3.Neequaye J. In vivo chloroquine-resistant falciparum in western Africa. Lancet. 1986;I:153. [PubMed] [Google Scholar]
- 4.Afari EA, Akanmori BD, Nankano T, Ofori-Adjei D. Plasmodium falciparum: sensitivity to chloroquine in-vivo in three ecological zones in Ghana. Trans R Soc Trop Med Hyg. 1992;86:231–232. doi: 10.1016/0035-9203(92)90285-k. [DOI] [PubMed] [Google Scholar]
- 5.Koram KA, Abuaku B, Duah N, Quashie N. Comparative efficacy of antimalarial drugs including ACTs in the treatment of uncomplicated malaria among children under 5 years in Ghana. Acta Tropica. 1994;95:194–203. doi: 10.1016/j.actatropica.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 6.Landgraf B, Kollaritsch H, Wiedermann G, Wernsdorfer H. Plasmodium falciparum: susceptibility in vitro and in vivo to chloroquine and sulfadoxine-pyrimethamine in Ghanaian school children. Trans R Soc Trop Med Hyg. 1994;88:440–442. doi: 10.1016/0035-9203(94)90424-3. [DOI] [PubMed] [Google Scholar]
- 7.Driessen GJ, van Kerkhpven S, Schouwenberg BJ, Bonsu G, Verhave JP. Sulphadoxine/pyrimethamine: an appropriate first-line alternative for the treatment of uncomplicated falciparum malaria in Ghanaian children under 5 years of age. Tropical Medicine and International Health. 2002;7:577–583. doi: 10.1046/j.1365-3156.2002.00910.x. [DOI] [PubMed] [Google Scholar]
- 8.Spencer HC, Watkins WW, Sixsmith DG, Koech DK. Response of Plasmodium falciparum to dihydrofolate reductase inhibitors in Malindi, Kenya. Trans R Soc Trop Med Hyg. 1986;80(2):201–203. doi: 10.1016/0035-9203(86)90009-x. [DOI] [PubMed] [Google Scholar]
- 9.Amukoye E, Winstanley PA, Watkins WM, Snow RW, Hatcher J, Mosobo M, Ngumbao E, Lowe B, Ton M, Minyiri G, Marsh K. Chlorproguanil-dapsone: effective treatment for uncomplicated falciparum malaria. Antimicrob Agents Chemother. 1997;41(10):2261–2264. doi: 10.1128/aac.41.10.2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sowunmi A, Ayede AI, Falade AG, Ndikum VN, Sowunmi CO, Adedeji AA, Falade CO, Happi TC, Oduola AMJ. Randomized comparison of chloroquine and amodiaquine in the treatment of acute, uncomplicated, Plasmodium falciparum malaria in children. Ann Trop Med Parasitol. 2001;95(6):549–558. doi: 10.1080/00034980120092507. [DOI] [PubMed] [Google Scholar]
- 11.WHO, author. Antimalarial Drug Combination Therapy: Report of a WHO Technical Consultation. Geneva: WHO; 2001. 4–5 April 2001. [Google Scholar]
- 12.White NJ. Delaying antimalarial drug resistance with combination chemotherapy. Parasitologia. 1999;44:301–308. [PubMed] [Google Scholar]
- 13.WHO, author. Monitoring Antimalarial Drug Resistance: Report of a WHO Consultation. Geneva: WHO; 2002. 3–5 December 2001. [Google Scholar]
- 14.Adjuik M, Agnamey P, Babiker A, Borrmann S, Brasseur P, Cisse M, Cobelens F, Diallo S, Faucher JF, Garner P, Gikunda S, Kremsner PG, Krishna S, Lell B, Loolpapit M, Matsiegui P-B, Missinou MA, Mwanza J, Ntoumi F, Olliaro P, Osimbo P, Rezbach P, Some E, Taylor WRJ. Amodiaquine-artesunate versus amodiaquine for uncomplicated Plasmodium falciparum malaria in African children: a randomized, multi-centre trial. Lancet. 2002;359:1365–1371. doi: 10.1016/s0140-6736(02)08348-4. [DOI] [PubMed] [Google Scholar]
- 15.Barenness H, Nagot N, Valea I, Koussoubé-Balma T, Ouedraogo A, Sanou T, Yé S. A randomized trial of amodiaquine and artesunate alone and in combination for the treatment of uncomplicated falciparum malaria in children from Burkina Faso. Trop Med Int Health. 2004;9(4):438–444. doi: 10.1111/j.1365-3156.2004.01224.x. [DOI] [PubMed] [Google Scholar]
- 16.Helleberg M, Goka BQ, Akanmori BD, Obeng-Adjei G, Rodrigues O, Kurtzals JA. Bone marrow suppression and severe anaemia associated with persistent plasmodium falciparum infection in African children with microscopical undetectable parasitaemia. Malar J. 2005 Dec 1;4(1):56. doi: 10.1186/1475-2875-4-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blair Silvia, Carmona-Fonseca Jaime, Piñeros Juan G, Ríos Alexandra, Álvarez Tania, Álvarez Gonzalo, Tobón Alberto. Therapeutic efficacy test in malaria falciparum in Antioquia, Colombia. Malaria Journal. 2006;5:14. doi: 10.1186/1475-2875-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]