Abstract
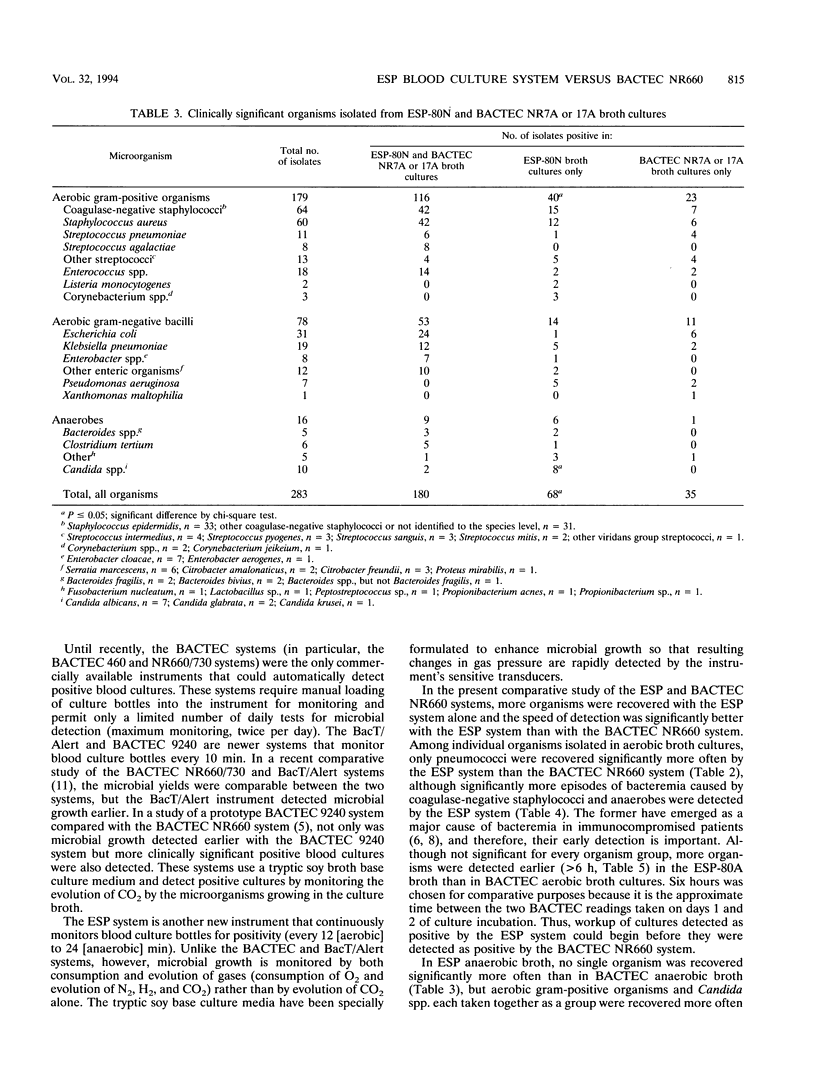
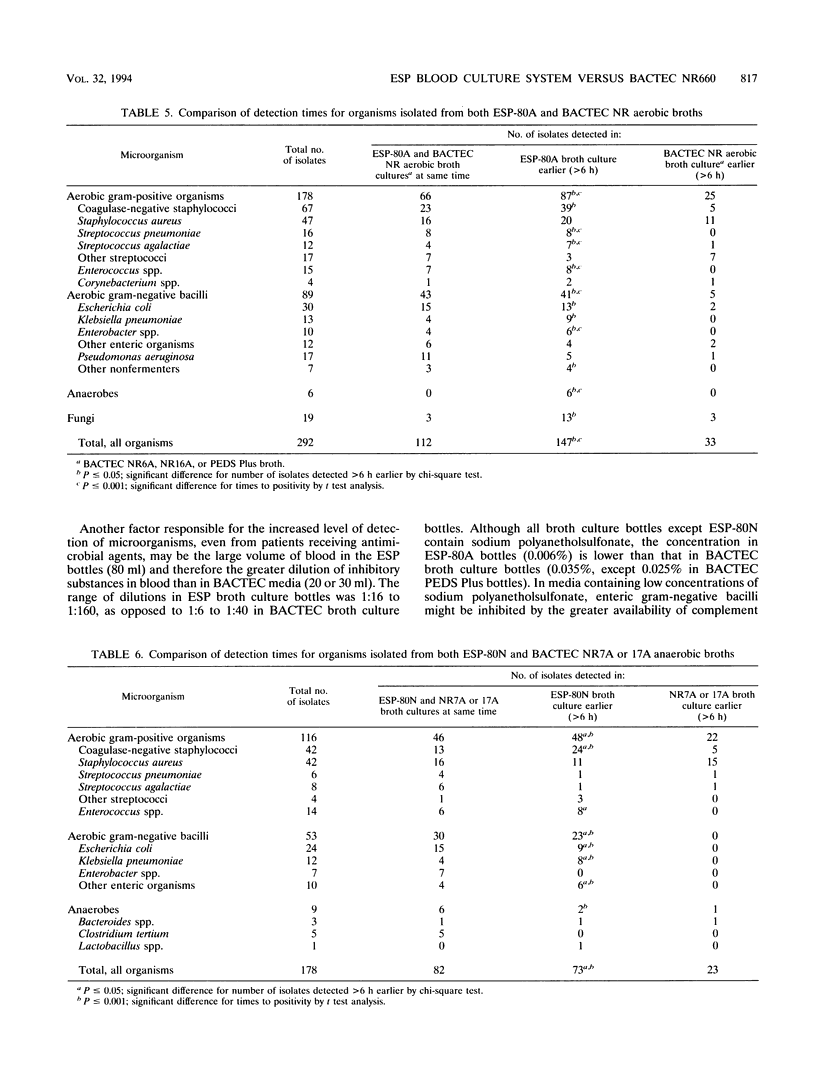
In a multicenter study, the Difco ESP blood culture system (Difco Laboratories, Detroit, Mich.) was compared with the BACTEC NR660 system (Becton Dickinson Diagnostic Instrument Systems, Sparks, Md.). The ESP system monitors each blood culture bottle every 12 to 24 min to detect changes in oxygen consumption and gas production by microbes. Equal volumes of blood were inoculated into aerobic ESP-80A and BACTEC 6A, 16A, or PEDS Plus broths and anaerobic ESP-80N and BACTEC 7A or 17A broths and were incubated for up to 7 days. ESP bottles contain supplemented tryptic soy broth without antimicrobial agent-adsorbing resins. From 7,532 aerobic compliant sets, the ESP system detected 356 clinically significant positive cultures and the BACTEC NR660 system detected 329. From 6,007 anaerobic cultures, the ESP system detected 234 clinically significant positive cultures and the BACTEC NR660 system detected 198. In aerobic broths, 292 organisms were isolated from both systems and 78 organisms were isolated from the ESP system alone, whereas 54 organisms were isolated from the BACTEC NR660 system alone (P < 0.05). Among individual organisms, pneumococci were isolated significantly more often in ESP aerobic broths. In anaerobic broths, 180 organisms were isolated from both systems and 68 organisms were isolated from the ESP system alone, whereas 35 organisms were isolated from the BACTEC NR660 system alone (P < 0.05). Aerobic gram-positive organisms as a group and Candida spp. were isolated significantly more often in ESP anaerobic broths. Both systems detected 207 clinically significant bacteremic episodes and the ESP system alone detected 63, whereas the BACTEC NR660 system alone detected 32 (P < 0.05). Significantly more episodes of bacteremia caused by Staphylococcus epidermidis and anaerobes were detected by the ESP system. The differences in the numbers of organisms detected >6h earlier in ESP broths compared with BACTNEC NR660 broths were significant, as were earlier times to detection. Although the total number of organisms detected was not significantly different, the ESP system alone detected more organisms in a shorter time than did the BACTEC NR660 system alone. The continuous monitoring capability of the ESP system makes it an attractive alternative to the BACTEC NR660 system.
Full text
PDF





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Jungkind D., Millan J., Allen S., Dyke J., Hill E. Clinical comparison of a new automated infrared blood culture system with the BACTEC 460 system. J Clin Microbiol. 1986 Feb;23(2):262–266. doi: 10.1128/jcm.23.2.262-266.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin J. C., Evers J. L., Officer J. L. Lack of requirement for blind subcultures of BACTEC blood culture media. J Clin Microbiol. 1981 Nov;14(5):567–570. doi: 10.1128/jcm.14.5.567-570.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolte F. S., Williams J. M., Jerris R. C., Morello J. A., Leitch C. D., Matushek S., Schwabe L. D., Dorigan F., Kocka F. E. Multicenter clinical evaluation of a continuous monitoring blood culture system using fluorescent-sensor technology (BACTEC 9240). J Clin Microbiol. 1993 Mar;31(3):552–557. doi: 10.1128/jcm.31.3.552-557.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaller M. A., Herwaldt L. A. Laboratory, clinical, and epidemiological aspects of coagulase-negative staphylococci. Clin Microbiol Rev. 1988 Jul;1(3):281–299. doi: 10.1128/cmr.1.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R. L., Meixler S. M., Simberkoff M. S. Excess mortality in critically ill patients with nosocomial bloodstream infections. Chest. 1991 Jul;100(1):164–167. doi: 10.1378/chest.100.1.164. [DOI] [PubMed] [Google Scholar]
- Stillman R. I., Wenzel R. P., Donowitz L. C. Emergence of coagulase negative staphylococci as major nosocomial bloodstream pathogens. Infect Control. 1987 Mar;8(3):108–112. doi: 10.1017/s0195941700067278. [DOI] [PubMed] [Google Scholar]
- Stratton C. W., Weinstein M. P., Mirrett S., Paisley J., Lauer B. A., Reller L. B. Controlled evaluation of blood culture medium containing gelatin and V-factor-analog for detection of septicemia in children. J Clin Microbiol. 1988 Apr;26(4):747–749. doi: 10.1128/jcm.26.4.747-749.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington J. A., 2nd, Ilstrup D. M. Blood cultures: issues and controversies. Rev Infect Dis. 1986 Sep-Oct;8(5):792–802. doi: 10.1093/clinids/8.5.792. [DOI] [PubMed] [Google Scholar]
- Wilson M. L., Weinstein M. P., Reimer L. G., Mirrett S., Reller L. B. Controlled comparison of the BacT/Alert and BACTEC 660/730 nonradiometric blood culture systems. J Clin Microbiol. 1992 Feb;30(2):323–329. doi: 10.1128/jcm.30.2.323-329.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]



