Abstract
Yersinia pestis causes pneumonic plague, an exceptionally virulent disease for which we lack a safe and effective vaccine. Antibodies specific for the Y. pestis F1 and LcrV proteins can protect mice against pulmonary Y. pestis infection. We demonstrate that neutralizing tumor necrosis factor-alpha (TNFα) and gamma-interferon (IFNγ) abrogates this protection at sub-optimal levels of F1- or LcrV-specific antibody, but not at optimal levels. Moreover, we demonstrate that endogenous TNFα and IFNγ confer measurable protection in the complete absence of protective antibodies. These findings indicate that antibodies and cytokines independently protect against pneumonic plague and suggest that surrogate assays for plague vaccine efficacy should consider both the level of vaccine-induced antibody and the capacity of vaccine recipients to produce TNFα and IFNγ upon exposure to Y. pestis.
Keywords: Yersinia pestis, vaccine, antibody, cytokine
INTRODUCTION
Plague is one of the world’s most deadly infectious diseases. The causative agent, Yersinia pestis, is a gram-negative facultative bacterium naturally transmitted from rodent reservoirs to humans by fleas [1–5]. Upon transmission by fleabite, Y. pestis bacilli typically infect the nearest skin-draining lymph nodes, which swell to produce diagnostic buboes. This bubonic form of plague often leads to sepsis and occasionally progresses to secondary, pneumonic infection. Pneumonic plague is nearly always lethal in humans. Moreover, it can spread from person-to-person via infectious respiratory droplets [6,7].
There is substantial concern that pneumonic plague may be exploited as a weapon of terror: scientists developed the technology to purposefully aerosolize infectious Y. pestis during the Cold War, and extensively antibiotic-resistant Y. pestis strains are known to exist [5,6,8]. Accordingly, tremendous research effort and financial investment have been devoted to the development of plague vaccines. Candidate, subunit vaccines containing the Y. pestis F1 and LcrV proteins recently entered human clinical trials [9,10].
Since ethical considerations will prevent clinical trials from challenging humans with Y. pestis, the licensure of F1/LcrV-based vaccines, or any other pneumonic plague countermeasure, will be based on efficacy data in animal models and safety data in humans. Confidence that countermeasures licensed in this manner will protect humans must rely upon the identification of correlates of protection in animal models and the development of assays that can serve as surrogates for efficacy studies in humans. At present, we remain uncertain about our ability to predict whether the magnitude and quality of immunity evoked by experimental plague vaccines will suffice to protect immunized humans [11]. This deficiency certainly hampers efforts to optimize vaccine regimens and also may limit public acceptance of any licensed vaccine. A detailed understanding of the basic principles of immune defense against pneumonic plague should aid the identification of correlates of protection and the development of robust surrogate assays for efficacy.
Antibodies likely play critical roles in the protection mediated by F1/LcrV-based vaccines since passively immunizing with F1- and/or LcrV-specific monoclonal antibodies (mAb) can protect mice against pulmonary Y. pestis challenge [12–15]. Recent F1/LcrV vaccination studies in cynomolgus macaques demonstrated a robust immune response that protected against aerosolized Y. pestis. In addition, passive transfer of immune sera protected naïve mice against pneumonic plague (unpublished data). However, previous studies from the United States Army revealed that F1/LcrV-based vaccines fail to reliably protect African green monkeys, despite eliciting robust antibody responses [16,17]. One possible explanation is that some primate species may fail to produce antibodies with particular functions that are important for protection. Accordingly, substantial efforts are now aimed at improving the efficacy of F1/LcrV-based vaccines and identifying robust correlate assays for antibody-mediated protection [17–20]. Another possible explanation for the inconsistent efficacy of F1/LcrV-based vaccines in primates is that some species may be deficient in aspects of innate or cellular immunity that act in concert with antibodies to optimally defend against pneumonic plague.
Seminal studies by Meyer, Jawetz and colleagues demonstrated that serum from plague convalescents lacks measurable bactericidal activity on its own and is “unable to destroy or lyse [Y. pestis] organisms in vitro and in vivo in the absence of phagocytic cells” [21,22]. The antibacterial activities of phagocytes are dramatically upregulated by the cytokines TNFα and IFNγ, and recently we demonstrated that these cytokines contribute to serum-mediated protection against pneumonic plague [23]. Specifically, we observed that the resistance to pulmonary Y. pestis infection conferred by immune serum is significantly impaired in gene-targeted mice lacking the capacity to produce TNFα or respond to IFNγ.
Here, we provide new information about how immunity combats pneumonic plague that should advance efforts to devise surrogate assays for the efficacy of F1/LcrV-based vaccines. Consistent with our prior studies of protection mediated by unfractionated immune serum [23], we demonstrate that cytokines contribute to protection mediated by mAb specific for F1 or LcrV. Moreover, we demonstrate that cytokines and antibodies protect via separable, independent mechanisms, indicating that surrogate assays for efficacy may need to consider both the levels of vaccine-induced antibody and the vaccine recipients’ capacity to produce cytokines upon exposure to Y. pestis.
MATERIALS AND METHODS
Mice
Wild type C57BL/6 mice and B cell-deficient μMT mice on the C57BL/6 background were purchased from The Jackson Laboratory (Bar Harbor, ME) and then bred in the specific pathogen free Trudeau Institute Animal Breeding Facility after embryo rederivation. Mice were cared for according to Trudeau Institute Animal Care and Use Committee guidelines.
Bacteria
All in vivo challenge studies used pigmentation-negative Y. pestis strain KIM D27 [24], which was generously provided by Robert Brubaker (Michigan State University). Y. pestis bacilli from frozen glycerol stocks were grown overnight at 26°C with continuous shaking in Bacto heart infusion broth (Becton, Dickinson and Company) supplemented with 2.5 mM CaCl2. After dilution to an OD620nm of 0.1, they were re-grown for 3 hours at 26°C, washed with saline, and app lied in a volume of 30 μl saline to the nares of mice lightly anesthetized with isoflurane. The median lethal dose of strain KIM D27, as calculated by the method of Reed and Muench [25], is approximately 2×104 CFU when grown and administered as described above.
Protective Y. pestis-specific antibodies
Methods for preparing immune serum from plague convalescent mice were described previously [23,26]. Hybridomas F1-04-A-G1 and 7.3 producing F1- and LcrV-specific mAb, respectively, also were described previously [12,27]. The mAb produced by these hybridomas were purified using Protein G agarose. They contained endotoxin levels less than 2.2 units per mg as measured by Limulus Amebocyte Lysate assay. For passive immunotherapy, serum or mAb were diluted in phosphate buffered saline (PBS) and administered intraperitoneally.
Cytokine neutralization
When indicated, animals were treated with 1 mg neutralizing mAb specific for TNFα (clone XT3.11) and/or 600 μg neutralizing mAb specific for murine IFNγ (clone XMG1.2) diluted in PBS and administered intraperitoneally. In some studies, mice received equal quantities of isotype-matched control mAb (rat immunoglobulin G1, clone HRPN). Our prior studies have consistently found that treatment with control mAb does not impact survival or bacterial burden during Y. pestis challenge [23,26]. All these mAb were supplied by Bio X Cell (West Lebanon, NH) who reported endotoxin levels less than 1.7 units per mg.
Survival endpoints and bacterial burden
In all survival studies, recumbent animals were considered moribund and euthanized. For measurement of bacterial burden, mice were euthanized by carbon dioxide narcosis at the indicated day after initiating infection. Livers and lungs were harvested and plated for CFU determination as described previously [23,26].
Statistics
Survival data were analyzed by Log-rank tests and CFU data were analyzed by ANOVA or Student’s t-test, as indicated (Prism 4.0, GraphPad Software). For presentation and for assessments of statistical significance, CFU measurements that fell below the limit of our assays were assigned a value equal to the detection limit.
RESULTS
TNFα and IFNγ contribute to protection mediated by immune serum
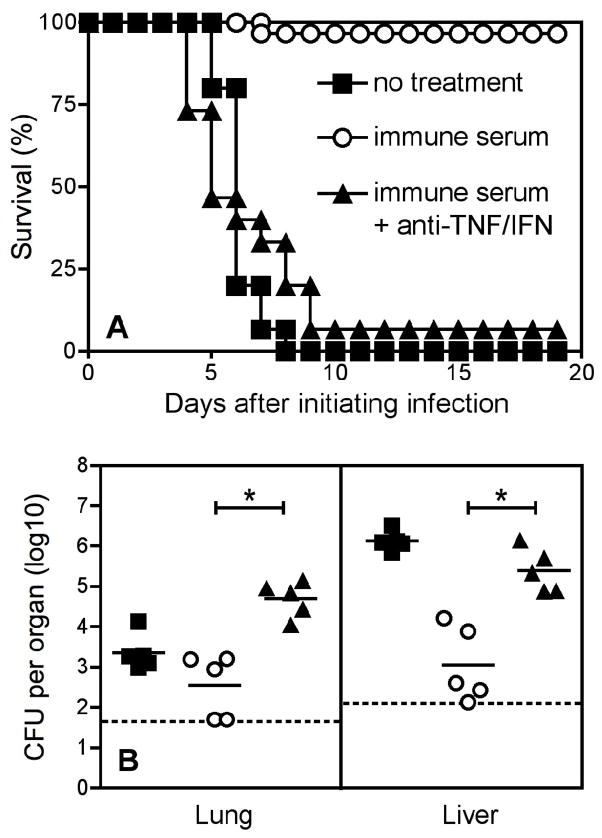
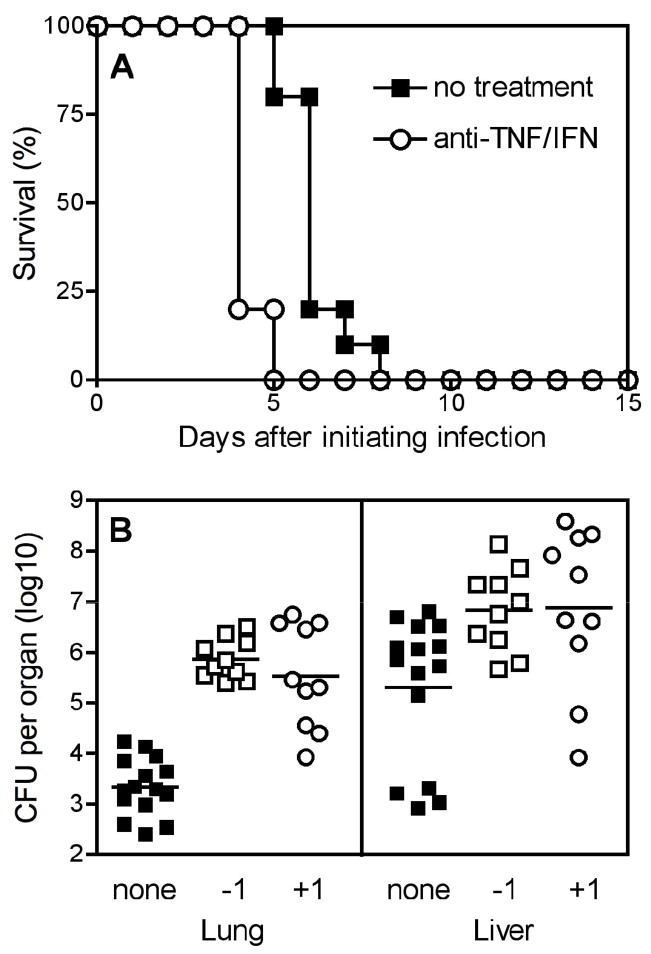
Figure 1 demonstrates that neutralizing the cytokines TNFα and IFNγ using specific mAb abrogates the protective efficacy of serotherapy. Wild type C57BL/6 mice infected intranasally with 10 LD-50 Y. pestis strain KIM D27 succumbed to plague between days 5 and 8 after the initiation of infection. Administration of 20 μl convalescent serum on day 1 post-infection significantly increased survival (p < 0.0001), but this protection was abrogated when mAb that neutralize TNFα and IFNγ were administered on day 1 post-infection (p < 0.0001). The data in Figure 1A is pooled from three independent experiments. In one experiment, we euthanized a parallel cohort of mice on day 3 after initiating infection and assessed bacterial burden. As shown in Figure 1B, serotherapy reduced the number of Y. pestis CFU, and co-administration of mAb that neutralize TNFα and IFNγ abrogated this serotherapy-mediated protection in the lung and liver (both p < 0.001).
Figure 1. TNFα and IFNγ contribute to protection mediated by immune serum.
Wild-type C57BL/6 mice were infected intranasally with Y. pestis (10 LD-50; 2×105 CFU). The following day, they were left untreated (closed squares) or were treated with convalescent immune serum alone (open circles) or immune serum along with neutralizing mAb specific for TNFα and IFNγ (anti-TNF/IFN; closed triangles). (A) In comparison with mice treated with immune serum alone, mice treated with immune serum along with cytokine-neutralizing mAb exhibited significantly reduced survival (p < 0.0001 by Log rank test; n = 15 mice per group). Data are pooled from three independent experiments. (B) In parallel with (A), additional groups of mice were euthanized on day 3 after initiating infection and bacterial burden was measured in lung and liver. In comparison with mice treated with immune serum alone, mice treated with immune serum along with cytokine-neutralizing mAb exhibited significantly increased bacterial burden in lung and liver at day 3 after initiating infection (* p < 0.001 by ANOVA with Bonferroni’s post test; n = 5 mice per group). The bars depict the means and the dashed line depicts the limit of detection. Similar results were observed on day 4 after initiating infection in a second, independent, experiment.
TNFα and IFNγ contribute to protection mediated by mAb specific for F1 and LcrV in a dose dependent manner
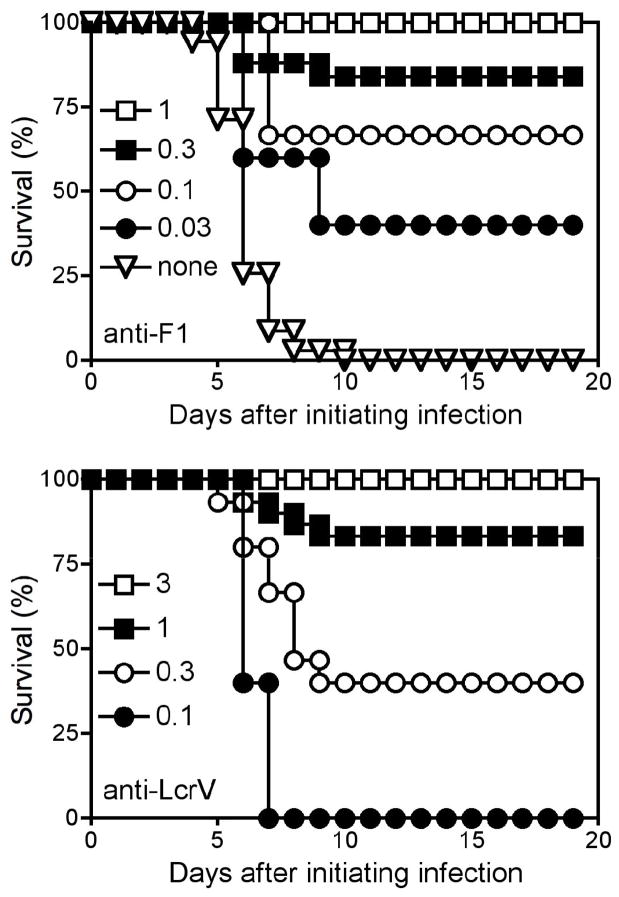
To investigate whether TNFα and IFNγ contribute to protection mediated by F1- and LcrV-specific antibodies, first we determined the doses of F1- and LcrV-specific mAb required to protect mice against intranasal infection with 10 LD-50 Y. pestis strain KIM D27. As for the serotherapy studies, we administered these mAb therapeutically on the day after initiating the infection. Figure 2 demonstrates that intraperitoneal administration of 1 μg F1-specific mAb (clone F1-04-A-G1) or 3 μg of LcrV-specific mAb (clone 7.3) sufficed to prevent lethality in wild type C57BL/6 experiencing pulmonary Y. pestis infection.
Figure 2. Determination of fully protective and sub-optimal doses of mAb specific for F1 or LcrV.
Wild-type C57BL/6 mice were infected intranasally with Y. pestis (10 LD-50; 2×105 CFU). The following day, mice were treated with the indicated doses of F1-specific mAb (top panel) or LcrV-specific mAb (bottom panel). Results depict percent survival over time post infection. Except for the lowest dose shown in each panel, which was only tested once, all data are pooled from 3 or more experiments using 5 mice/dose/experiment.
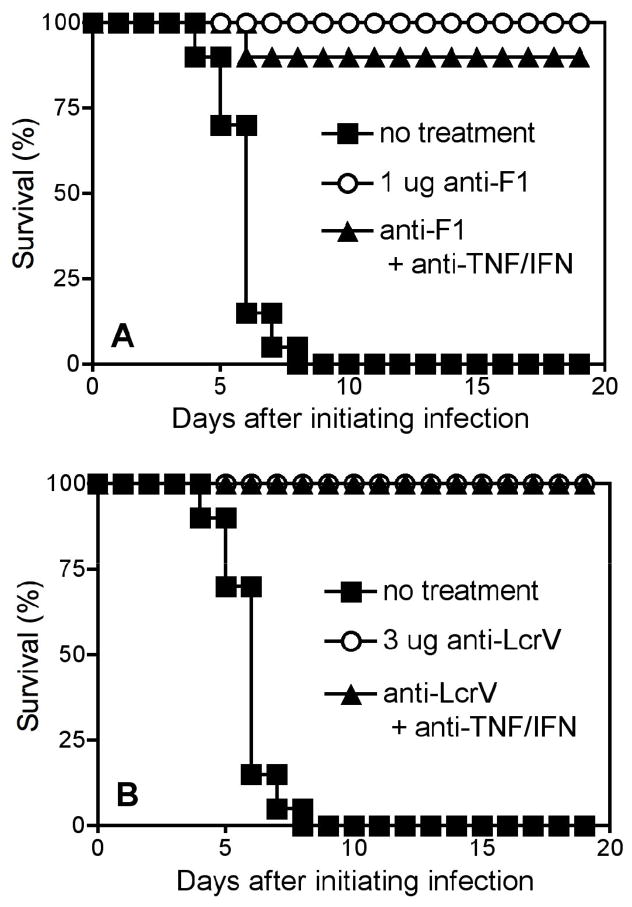
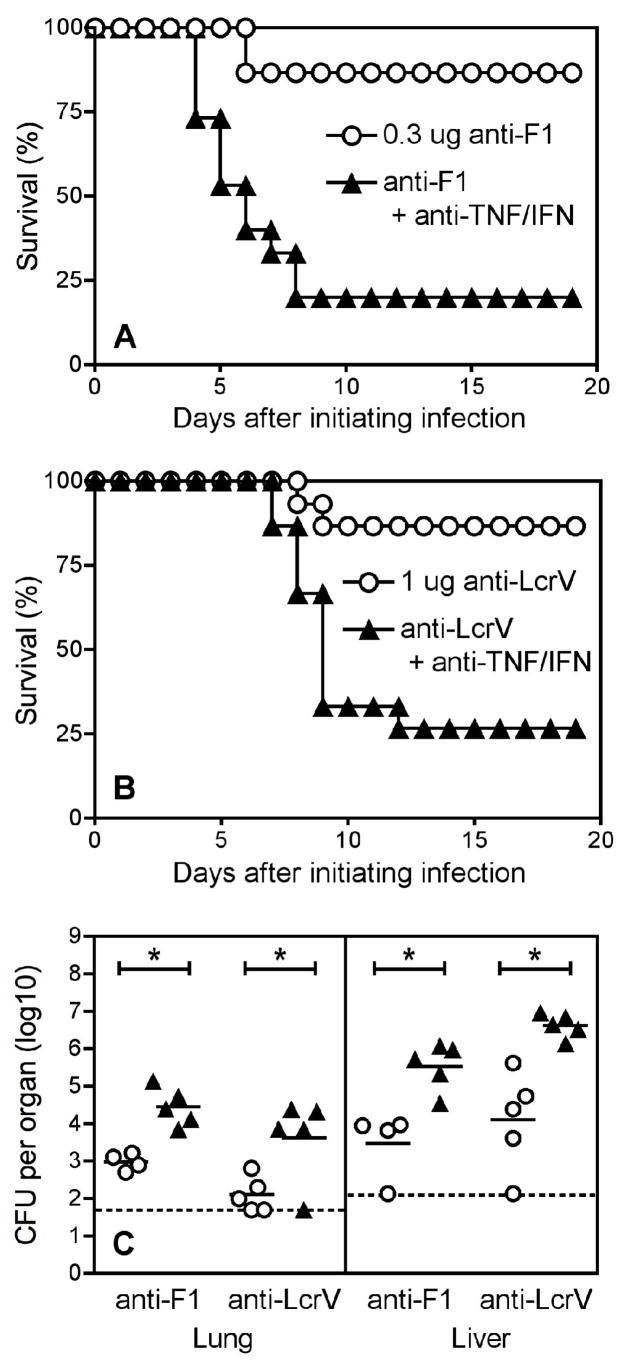
We next investigated roles for cytokines by co-administering F1- or LcrV-specific mAb along with mAb that neutralize TNFα and IFNγ. We performed these studies using two doses of F1- or LcrV-specific mAb: one that conferred full protection, and a second that conferred sub-optimal protection. Neutralizing TNFα and IFNγ in mice treated with fully protective doses of F1- (Figure 3A) or LcrV-specific antibody (Figure 3B) did not impact survival significantly. However, cytokine neutralization significantly reduced survival in mice treated with sub-optimal doses of F1- or LcrV-specific antibody (Figures 4A and 4B; p = 0.0002 for F1 and 0.001 for LcrV). This protective role for cytokines in mice treated with sub-optimal doses of F1- or LcrV-specific antibody also was documented by measurements of bacterial burden: Figure 4C demonstrates that neutralizing TNFα and IFNγ significantly increased the numbers of pulmonary and hepatic Y. pestis CFU at day 4 after initiating infection (all p < 0.05).
Figure 3. TNFα and IFNγ do not contribute significantly to protection mediated by optimal doses of mAb specific for F1 or LcrV.
Wild-type C57BL/6 mice were infected intranasally with Y. pestis (10 LD-50; 2×105 CFU). (A) The following day, they were left untreated (closed squares) or were treated with a fully protective dose of F1-specific mAb (1 μg; open circles) or that dose of F1-specific mAb along with neutralizing mAb specific for TNFα and IFNγ (anti-TNF/IFN; closed triangles). Cytokine neutralization did not significantly impact survival (n = 10 mice per group). Data are pooled from two independent experiments. (B) In parallel with (A), additional groups of mice were treated with a fully protective dose of LcrV-specific mAb (3 μg; open circles) or that dose of LcrV-specific mAb along with neutralizing mAb specific for TNFα and IFNγ (closed triangles). Cytokine neutralization did not significantly impact survival (n = 10 mice per group). Data are pooled from two independent experiments.
Figure 4. TNFα and IFNγ contribute to protection mediated by sub-optimal doses of mAb specific for F1 or LcrV.
Wild-type C57BL/6 mice were infected intranasally with Y. pestis (10 LD-50; 2×105 CFU). (A) The following day, they were left untreated or were treated with a sub-optimal dose of F1-specific mAb (0.3 μg; open circles) or that dose of F1-specific mAb along with neutralizing mAb specific for TNFα and IFNγ (anti-TNF/IFN; closed triangles). All untreated mice succumbed by day 9 (not shown). In comparison with mice treated with F1-specific mAb alone, the mice treated with F1-specific mAb along with cytokine-neutralizing mAb exhibited significantly reduced survival (p = 0.0002; n = 15 mice per group). Data are pooled from three independent experiments. (B) In parallel with (A), additional groups of mice were treated with a sub-optimal dose of LcrV-specific mAb (1 μg; open circles) or that dose of LcrV-specific mAb along with neutralizing mAb specific for TNFα and IFNγ (closed triangles). In comparison with mice treated with LcrV-specific mAb alone, the mice treated with LcrV-specific mAb along with cytokine-neutralizing mAb exhibited significantly reduced survival (p = 0.001; n = 15 mice per group). Data are pooled from three independent experiments. (C) In parallel with (A) and (B), groups of mice were euthanized on day 4 after initiating infection and bacterial burden was measured. In comparison with mice treated with F1- or LcrV-specific mAb alone (open circles), mice treated with F1- or LcrV-specific mAb along with cytokine-neutralizing mAb (closed triangles) exhibited significantly increased bacterial burden in lung and liver (* p < 0.05 by ANOVA with Bonferroni’s post test; n = 4–5 mice per group). The bars depict the means and the dashed line depicts the limit of detection. Similar results were observed on day 3 after initiating infection in a second, independent, experiment.
TNFα and IFNγ contribute to protection in the absence of Y. pestis-specific antibodies
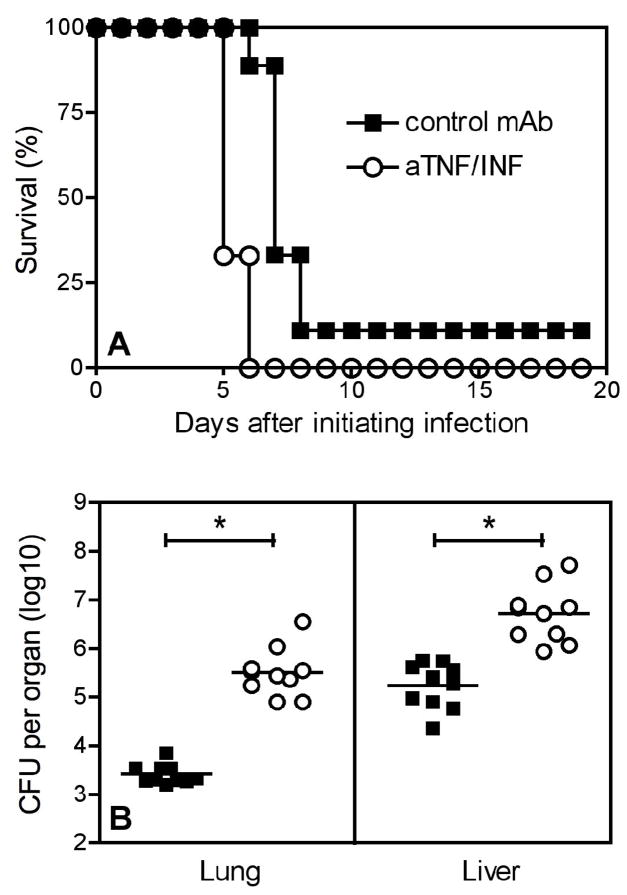
Figure 5 shows the consequences of neutralizing cytokines in wild type C57BL/6 mice in the absence of any therapeutic treatment with Y. pestis-specific antibodies. Administration of mAb that neutralize TNFα and IFNγ significantly shortened the time to morbidity in Y. pestis-infected wild type mice (Figure 5A; p < 0.0001). Consistent with the increased rate of morbidity, neutralization of TNFα and IFNγ also significant increased the number of Y. pestis CFU in the lung and liver at day 3 after initiating infection with 10 LD-50 Y. pestis (Figure 5B; all p < 0.05). Neutralizing TNFα and IFNγ on the day prior to infection or delaying neutralization until one day post-infection similarly impacted bacterial burden. Cytokine neutralization even increased bacterial burden significantly when the neutralization was delayed until day 2 post-infection and CFU were assayed on day 4 (not shown). Figure 6 shows that neutralization of TNFα and IFNγ one day after initiating pneumonic plague also significantly shortened the time to mortality (Figure 6A; p < 0.0001) and increased the bacterial burden (Figure 6B; p < 0.001 for both lung and liver) in μMT mice, which lack B cells and cannot produce antibody [28].
Figure 5. TNFα and IFNγ contribute to basal protection in wild type mice.
Wild-type C57BL/6 mice were infected intranasally with Y. pestis (10 LD-50; 2×105 CFU). (A) The following day, they were left untreated (closed squares) or were treated with neutralizing mAb specific for TNFα and IFNγ (anti-TNF/IFN; open circles). Mice treated with cytokine-neutralizing mAb exhibited significantly reduced survival (both p < 0.0001; n = 10 mice per group). Data are pooled from two independent experiments. (B) Groups of mice were treated with neutralizing mAb specific for TNFα and IFNγ one day prior (−1; open squares) or one day after (+1; open squares) initiating infection. Control animals were left untreated (closed squares). Bacterial burden was measured on day 3 after initiating infection. In comparison with controls, mice treated with TNFα- and IFNγ-specific mAb on either day −1 or day +1 exhibited significantly increased bacterial burden in lung and liver (p < 0.01 and p < 0.05 by ANOVA with Dunnett’s post test for lung and liver, respectively; n = 10–15 mice per group). The bars depict the means. Data are pooled from three independent experiments.
Figure 6. TNFα and IFNγ contribute to basal protection in B cell-deficient mice.
C57BL/6-backcrossed B cell-deficient μMT mice were infected intranasally with Y. pestis (10 LD-50; 2×105 CFU). On the day prior to infection, animals received control mAb (closed squares) or neutralizing mAb specific for TNFα and IFNγ (anti-TNF/IFN; open circles). (A) Treatment with cytokine-neutralizing mAb significantly increased the time to morbidity in naïve mice (p < 0.0001; n = 9 mice per group). (B) Treatment with cytokine-neutralizing mAb significantly increased the bacterial burden in lung and liver on day 3 after initiating infection (* p < 0.001 as determined by Student’s t-test; n = 9 mice per group). The bars depict the means. All data in this figure are pooled from two independent experiments.
DISCUSSION
Subunit vaccines containing the Y. pestis F1 and LcrV proteins offer great promise for the development of a safe and effective countermeasures for pneumonic plague. Likewise, mAb specific for F1 or LcrV may constitute useful prophylactics or therapeutics. While F1/LcrV-based vaccines effectively protect mice against pulmonary Y. pestis challenge, recent studies indicate that other non-antibody contributions may be required for full protection in some species of non-human primates [16,17]. To facilitate the development of pneumonic plague countermeasures, we have been studying basic mechanisms of immune defense against pulmonary Y. pestis challenge.
Therapeutic administration of immune serum from convalescent mice protects naïve wild type mice against lethal pulmonary Y. pestis challenge. Previously, we demonstrated that this immune serum poorly protects gene-targeted mice lacking the capacity to produce TNFα or the receptor for IFNγ [23]. We concluded that TNFα-and IFNγ contribute to serotherapy-mediated protection against pneumonic plague. However, it remained possible that immunological abnormalities associated with congenital cytokine deficiency may have contributed to our prior observations. Here, we alleviated such concerns by using neutralizing mAb to assess the role of cytokines, rather than gene-targeted mice. Notably, the studies reported here also demonstrate that neutralizing TNFα and IFNγ either before or after initiating infection leads to similar outcomes (Figure 5), indicating that cytokines contribute to the clearance of established Y. pestis infection.
Our initial studies used immune serum from convalescent mice as a source of protective antibody. The use of convalescent serum left open the possibility that our findings may not extend to protection mediated by antibodies specific for the F1 and LcrV proteins included in the subunit plague vaccines now in human clinical trials. The studies reported here demonstrate directly that TNFα and IFNγ can augment protection conferred by F1- and LcrV-specific antibody (Figure 4). Interestingly, roles for cytokines are particularly evident at sub-optimal titers of F1- and LcrV-specific antibody. These findings are likely to be relevant to the development of human vaccines and therapeutics that rely upon F1- or LcrV-specific antibodies, particularly since vaccines rarely elicit optimal responses in all vaccinates, and since antibody titers inevitably wane with time.
While neutralizing TNFα and IFNγ abrogates protection at sub-optimal titers of F1- or LcrV-specific antibody, the protection conferred by optimal doses of those antibodies is impacted far less dramatically, if at all (Figure 3). This finding indicates that antibody-mediated protection does not absolutely require TNFα and IFNγ and strongly suggests that cytokines and antibodies protect via distinguishable, independent pathways. To further investigate that possibility, we assessed whether cytokines confer protection against pneumonic plague during experimental contexts that lack Y. pestis-specific antibody. Specifically, we examined naïve wild type mice that did not receive any treatment with F1- or LcrV-specific mAb. Remarkably, we discerned measurable protective roles for TNFα and IFNγ, as evidenced both by increased bacterial burden and shortened time to mortality upon cytokine neutralization (Figure 5). This protective role for TNFα and IFNγ may have reflected an impact of cytokines on antibody-mediated protection if the wild type mice used in these studies rapidly produced Y. pestis-specific antibody after the initiation of infection. However, we formally excluded that possibility by replicating the key observations in transgenic μMT mice, which cannot produce antibodies [28] (Figure 6). To our knowledge, these studies are the first to demonstrate measurable protective roles for endogenous TNFα or IFNγ in a model of untreated primary pneumonic plague.
While the data reported here demonstrate decisively that cytokine-mediated immunity can augment protection against lethal pulmonary Y. pestis challenge in the presence or absence of specific antibody, much remains to be learned about precisely how TNFα and IFNγ protect against pneumonic plague. Our findings are consistent with prior work indicating that injecting mice with exogenous TNFα and IFNγ protects against subsequent initiation of septicemic plague [29] and that vaccination with F1/LcrV poorly protects against bubonic plague in STAT4-deficient mice, which are impaired for production of IFNγ [30]. We find it particularly notable that pulmonary Y. pestis infection is characterized by a delayed inflammatory response [31–33], perhaps reflecting an evolutionary adaptation that serves to suppress cytokine-mediated host defense. Indeed, pre-treating macrophages with TNFα and IFNγ restricts the replication of Y. pestis within macrophages [34]. While the pathological significance of intracellular bacteria during plague remains to be established decisively, it is clear that Y. pestis can grow within phagocytes in vitro [35–40] and can be detected within phagocytes in vivo [34,41,42].
Together, the data reported here indicate that antibodies and cytokines independently contribute to defense against pneumonic plague. Our current working model [11] is that cytokines suppress the capacity of Y. pestis to replicate intracellularly [34], while antibodies neutralize Y. pestis virulence mechanisms and opsonize bacilli [17–20,43,44], thereby helping host cells survive interactions with Y. pestis bacilli and helping phagocytes to internalize and destroy the bacteria. Given these independent, overlapping and complementary activities, we anticipate that cytokines and antibodies will act additively, perhaps synergistically, during defense against pneumonic plague.
F1/LcrV-based vaccines elicit similar antibody titers, at least as measured by ELISA, in cynomolgus macaques and African green monkeys [16,17]. However, the vaccinated macaques are well protected against pneumonic plague whereas the African green monkeys are not [16,17]. The studies reported here may help to explain this variable efficacy of F1/LcrV-based vaccines in non-human primates. We found that F1- or LcrV-specific antibody protects mice against experimental pneumonic plague, but this protection is highly dependent on TNFα and IFNγ at suboptimal doses of antibody. Thus, it seems likely that animals with a capacity to efficiently produce and respond to TNFα and IFNγ will have a greater capacity to combat plague than animals that fail to utilize these cytokines efficiently. If cynomolgus macaques and African green monkeys differentially produce and/or respond to cytokines during Y. pestis infection, then this may explain why these two types of monkeys exhibit differential protection after vaccination despite harboring similar titers of F1/LcrV-specific antibody. Certainly there are other possible explanations for the variable efficacy of the F1/LcrV vaccine in non-human primates, such as the production of similar overall antibody titers but different levels of especially protective antibody sub-types. Future studies will need to address these distinguishable hypotheses.
It is important to identify robust correlates of protection in animals that can be used as surrogate assays for plague vaccine efficacy in humans. Recent studies have advanced the development of surrogate assays [17–20] but none have yet to adequately explain the variable efficacy of F1/LcrV-based vaccines in the two types of non-human primates studied to date. Our observations that cytokines contribute to antibody-mediated defense against pneumonic plague suggest that surrogate assays for plague vaccine efficacy in humans should consider both the levels of vaccine-induced antibody and the capacity of vaccine recipients to produce cytokines upon exposure to Y. pestis. Our findings also suggest that supplementing F1/LcrV-based vaccines with adjuvants and/or antigens that prime memory T cells with the capacity to rapidly produce cytokines in response to Y. pestis infection should improve efficacy against pneumonic plague.
Acknowledgments
This research was supported by funding from the Trudeau Institute and PHS grants R01-AI061577 (Smiley) and U54-AI057158 (Lipkin). We thank Debbie Duso for technical assistance and the employees of the Trudeau Institute animal facilities for dedicated care and breeding of the mice used in these studies. We also thank Dr. Robert Brubaker for generously providing access to the KIM D27 Y. pestis strain.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Perry RD, Fetherston JD. Yersinia pestis-etiologic agent of plague. Clin Microbiol Rev. 1997;10(1):35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brubaker RR. Yersinia pestis and bubonic plague. In: Dworkin M, Falkow S, Rosenberg E, Schleifer K-H, Stackebrandte E, editors. The prokaryotes, an evolving electronic resource for the microbiological community. Springer-Verlag; New York: 2000. [Google Scholar]
- 3.Pollitzer R. Plague. Geneva: 1954. [Google Scholar]
- 4.Dennis DT, Gage KL, Gratz N, Poland JD, Tikhomirov E. Plague Manual: Epidemiology, Distribution, Surveillance and Control WHO/CDS/CSR/EDC/99.2. World Health Organization; 1999. [Google Scholar]
- 5.Prentice MB, Rahalison L. Plague. Lancet. 2007;369(9568):1196–1207. doi: 10.1016/S0140-6736(07)60566-2. [DOI] [PubMed] [Google Scholar]
- 6.Inglesby TV, Dennis DT, Henderson DA, et al. Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. Jama. 2000;283(17):2281–2290. doi: 10.1001/jama.283.17.2281. [DOI] [PubMed] [Google Scholar]
- 7.Kool JL. Risk of person-to-person transmission of pneumonic plague. Clin Infect Dis. 2005;40(8):1166–1172. doi: 10.1086/428617. [DOI] [PubMed] [Google Scholar]
- 8.Dennis DT. Plague as a biological weapon. In: Fong IW, Alibek K, editors. Bioterrorism and infectious agents: a new dilemma for the 21st century. Springer Science; 2005. pp. 37–64. [Google Scholar]
- 9.Williamson ED, Flick-Smith HC, Lebutt C, et al. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect Immun. 2005;73(6):3598–3608. doi: 10.1128/IAI.73.6.3598-3608.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris SR. Development of a recombinant vaccine against aerosolized plague. Vaccine. 2007;25(16):3115–3117. doi: 10.1016/j.vaccine.2007.01.071. [DOI] [PubMed] [Google Scholar]
- 11.Smiley ST. Current challenges in the development of vaccines for pneumonic plague. Expert Rev Vaccines. 2008;7(2):209–221. doi: 10.1586/14760584.7.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson GW, Jr, Worsham PL, Bolt CR, et al. Protection of mice from fatal bubonic and pneumonic plague by passive immunization with monoclonal antibodies against the F1 protein of Yersinia pestis. Am J Trop Med Hyg. 1997;56(4):471–473. doi: 10.4269/ajtmh.1997.56.471. [DOI] [PubMed] [Google Scholar]
- 13.Green M, Rogers D, Russell P, et al. The SCID/Beige mouse as a model to investigate protection against Yersinia pestis. FEMS Immunol Med Microbiol. 1999;23(2):107–113. doi: 10.1111/j.1574-695X.1999.tb01229.x. [DOI] [PubMed] [Google Scholar]
- 14.Hill J, Copse C, Leary S, Stagg AJ, Williamson ED, Titball RW. Synergistic protection of mice against plague with monoclonal antibodies specific for the F1 and V antigens of Yersinia pestis. Infect Immun. 2003;71(4):2234–2238. doi: 10.1128/IAI.71.4.2234-2238.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hill J, Eyles JE, Elvin SJ, Healey GD, Lukaszewski RA, Titball RW. Administration of antibody to the lung protects mice against pneumonic plague. Infect Immun. 2006;74(5):3068–3070. doi: 10.1128/IAI.74.5.3068-3070.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pitt ML. Animals Models and Correlates of Protection for Plague Vaccines Workshop. Gaithersburg, MD: 2004. Non-human primates as a model for pneumonic plague. http://www.fda.gov/cber/minutes/plague101304t.pdf. [Google Scholar]
- 17.Bashaw J, Norris S, Weeks S, Trevino S, Adamovicz JJ, Welkos S. Development of in vitro correlate assays of immunity to infection with Yersinia pestis. Clin Vaccine Immunol. 2007;14(5):605–616. doi: 10.1128/CVI.00398-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williamson ED, Flick-Smith HC, Waters E, et al. Immunogenicity of the rF1+rV vaccine for plague with identification of potential immune correlates. Microb Pathog. 2007;42(1):11–21. doi: 10.1016/j.micpath.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Zauberman A, Cohen S, Levy Y, et al. Neutralization of Yersinia pestis-mediated macrophage cytotoxicity by anti-LcrV antibodies and its correlation with protective immunity in a mouse model of bubonic plague. Vaccine. 2008;26(13):1616–1625. doi: 10.1016/j.vaccine.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 20.Welkos S, Norris S, Adamovicz J. Modified caspase-3 assay indicates correlation of caspase-3 activity with immunity of nonhuman primates to Yersinia pestis infection. Clin Vaccine Immunol. 2008;15(7):1134–1137. doi: 10.1128/CVI.00091-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jawetz E, Meyer KF. Studies on plague immunity in experimental animals. II. Some factors of the immunity mechanism in bubonic plague. J Immunol. 1944;49:15–30. [Google Scholar]
- 22.Meyer KF. Immunity in plague: a critical consideration of some recent studies. J Immunol. 1950;64:139–163. [PubMed] [Google Scholar]
- 23.Parent MA, Wilhelm LB, Kummer LW, Szaba FM, Mullarky IK, Smiley ST. Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect Immun. 2006;74(6):3381–3386. doi: 10.1128/IAI.00185-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lahteenmaki K, Virkola R, Saren A, Emody L, Korhonen TK. Expression of plasminogen activator pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect Immun. 1998;66(12):5755–5762. doi: 10.1128/iai.66.12.5755-5762.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reed LJ, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 26.Parent MA, Berggren KN, Kummer LW, et al. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect Immun. 2005;73(11):7304–7310. doi: 10.1128/IAI.73.11.7304-7310.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hill J, Leary SE, Griffin KF, Williamson ED, Titball RW. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect Immun. 1997;65(11):4476–4482. doi: 10.1128/iai.65.11.4476-4482.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kitamura D, Roes J, Kuhn R, Rajewsky K. A B cell-deficient mouse by targeted disruption of the membrane exon of the immunoglobulin mu chain gene. Nature. 1991;350(6317):423–426. doi: 10.1038/350423a0. [DOI] [PubMed] [Google Scholar]
- 29.Nakajima R, Brubaker RR. Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect Immun. 1993;61(1):23–31. doi: 10.1128/iai.61.1.23-31.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elvin SJ, Williamson ED. Stat 4 but not Stat 6 mediated immune mechanisms are essential in protection against plague. Microb Pathog. 2004;37(4):177–184. doi: 10.1016/j.micpath.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 31.Lathem WW, Crosby SD, Miller VL, Goldman WE. Progression of primary pneumonic plague: a mouse model of infection, pathology, and bacterial transcriptional activity. Proc Natl Acad Sci U S A. 2005;102(49):17786–17791. doi: 10.1073/pnas.0506840102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lathem WW, Price PA, Miller VL, Goldman WE. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science. 2007;315(5811):509–513. doi: 10.1126/science.1137195. [DOI] [PubMed] [Google Scholar]
- 33.Bubeck SS, Cantwell AM, Dube PH. Delayed inflammatory response to primary pneumonic plague occurs in both outbred and inbred mice. Infect Immun. 2007;75(2):697–705. doi: 10.1128/IAI.00403-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lukaszewski RA, Kenny DJ, Taylor R, Rees DG, Hartley MG, Oyston PC. Pathogenesis of Yersinia pestis infection in BALB/c mice: effects on host macrophages and neutrophils. Infect Immun. 2005;73(11):7142–7150. doi: 10.1128/IAI.73.11.7142-7150.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cavanaugh DC, Randall R. The role of multiplication of Pasteurella pestis in mononuclear phagocytes in the pathogenesis of flea-borne plague. J Immunol. 1959;83:348–363. [PubMed] [Google Scholar]
- 36.Janssen WA, Lawton WD, Fukui GM, Surgalla MJ. The pathogenesis of plague. I. A study of the correlation between virulence and relative phagocytosis resistance of some strains of Pasteurella pestis. J Infect Dis. 1963;113:139–143. doi: 10.1093/infdis/113.2.139. [DOI] [PubMed] [Google Scholar]
- 37.Janssen WA, Surgalla MJ. Plague bacillus: survival within host phagocytes. Science. 1969;163:950–952. doi: 10.1126/science.163.3870.950. [DOI] [PubMed] [Google Scholar]
- 38.Straley SC, Harmon PA. Yersinia pestis grows within phagolysosomes in mouse peritoneal macrophages. Infect Immun. 1984;45(3):655–659. doi: 10.1128/iai.45.3.655-659.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pujol C, Bliska JB. The ability to replicate in macrophages is conserved between Yersinia pestis and Yersinia pseudotuberculosis. Infect Immun. 2003;71(10):5892–5899. doi: 10.1128/IAI.71.10.5892-5899.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pujol C, Grabenstein JP, Perry RD, Bliska JB. Replication of Yersinia pestis in interferon gamma-activated macrophages requires ripA, a gene encoded in the pigmentation locus. Proc Natl Acad Sci U S A. 2005;102(36):12909–12914. doi: 10.1073/pnas.0502849102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Finegold MJ. Pneumonic plague in monkeys. An electron microscopic study. Am J Pathol. 1969;54(2):167–185. [PMC free article] [PubMed] [Google Scholar]
- 42.Davis KJ, Fritz DL, Pitt ML, Welkos SL, Worsham PL, Friedlander AM. Pathology of experimental pneumonic plague produced by fraction 1-positive and fraction 1-negative Yersinia pestis in African green monkeys (Cercopithecus aethiops) Arch Pathol Lab Med. 1996;120(2):156–163. [PubMed] [Google Scholar]
- 43.Cowan C, Philipovskiy AV, Wulff-Strobel CR, Ye Z, Straley SC. Anti-LcrV antibody inhibits delivery of Yops by Yersinia pestis KIM5 by directly promoting phagocytosis. Infect Immun. 2005;73(9):6127–6137. doi: 10.1128/IAI.73.9.6127-6137.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weeks S, Hill J, Friedlander A, Welkos S. Anti-V antigen antibody protects macrophages from Yersinia pestis-induced cell death and promotes phagocytosis. Microb Pathog. 2002;32(5):227–237. doi: 10.1006/mpat.2002.0498. [DOI] [PubMed] [Google Scholar]