Abstract
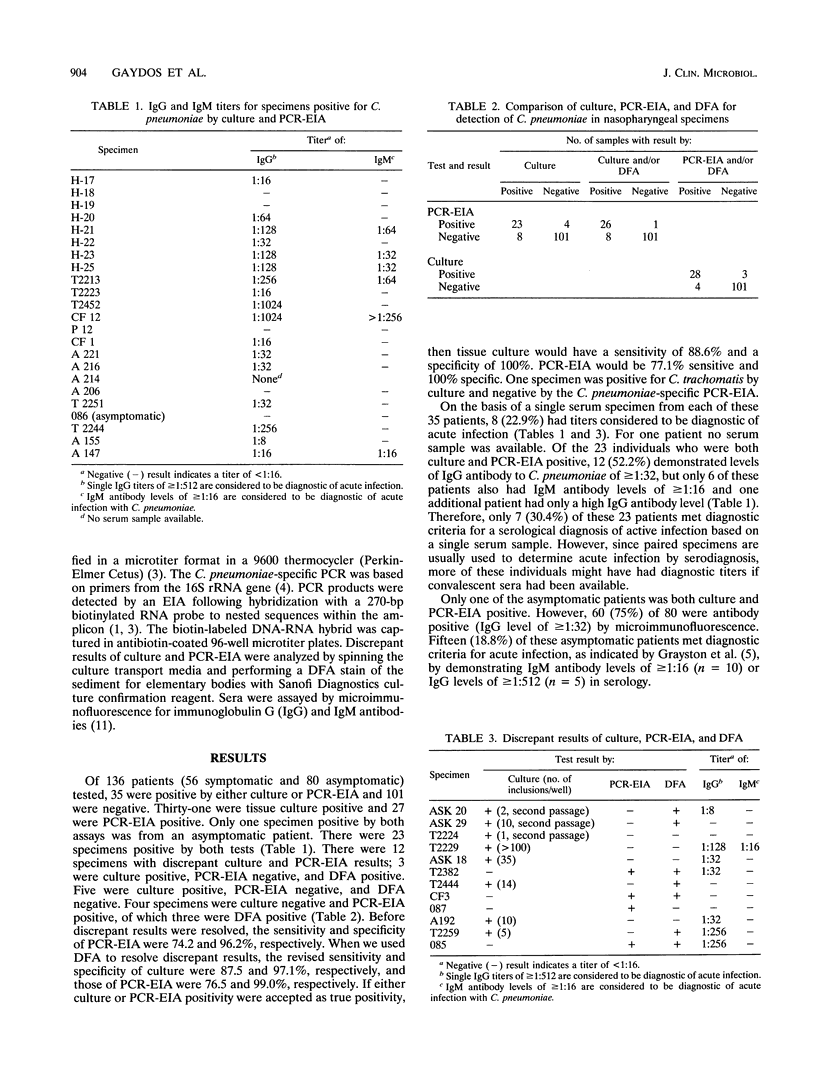
To assess the utility of PCR-enzyme immunoassay (EIA) for diagnosis of acute infection with Chlamydia pneumoniae, we compared tissue culture, PCR-EIA, direct fluorescent-antibody (DFA) stain, and serology in studies with 56 patients with respiratory symptoms and 80 asymptomatic persons. Thirty-five patients were positive by either culture or PCR-EIA, and 101 were negative by both assays. Thirty specimens from symptomatic patients and one from an asymptomatic patient were culture positive; 23 of these were also PCR-EIA positive. Of the eight culture-positive, PCR-EIA-negative specimens, five were DFA negative and three were DFA positive. Four additional specimens were culture negative and PCR-EIA positive; of these, three were DFA positive and one was DFA negative. When we used culture- and/or DFA-positive results as a reference or "gold standard," the sensitivity and specificity of PCR were 76.5 and 99.0%, respectively. When we used PCR- and/or DFA-positive results as the reference, the sensitivity of culture was 87.5%. On the basis of single acute serum specimens, only 8 of these 35 patients had diagnostic antibody titers. Of the asymptomatic patients, 75% had immunoglobulin G or immunoglobulin M antibody to C. pneumoniae; 15 (18.8%) of these had antibody levels considered to be diagnostic of acute infection. This multicenter study indicates that culture and/or PCR-EIA is more reliable for prompt diagnosis of C. pneumoniae infection than single-point serology alone.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bobo L., Coutlee F., Yolken R. H., Quinn T., Viscidi R. P. Diagnosis of Chlamydia trachomatis cervical infection by detection of amplified DNA with an enzyme immunoassay. J Clin Microbiol. 1990 Sep;28(9):1968–1973. doi: 10.1128/jcm.28.9.1968-1973.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang G. D., Fine M., Orloff J., Arisumi D., Yu V. L., Kapoor W., Grayston J. T., Wang S. P., Kohler R., Muder R. R. New and emerging etiologies for community-acquired pneumonia with implications for therapy. A prospective multicenter study of 359 cases. Medicine (Baltimore) 1990 Sep;69(5):307–316. doi: 10.1097/00005792-199009000-00004. [DOI] [PubMed] [Google Scholar]
- Gaydos C. A., Fowler C. L., Gill V. J., Eiden J. J., Quinn T. C. Detection of Chlamydia pneumoniae by polymerase chain reaction-enzyme immunoassay in an immunocompromised population. Clin Infect Dis. 1993 Oct;17(4):718–723. doi: 10.1093/clinids/17.4.718. [DOI] [PubMed] [Google Scholar]
- Gaydos C. A., Quinn T. C., Eiden J. J. Identification of Chlamydia pneumoniae by DNA amplification of the 16S rRNA gene. J Clin Microbiol. 1992 Apr;30(4):796–800. doi: 10.1128/jcm.30.4.796-800.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grayston J. T., Campbell L. A., Kuo C. C., Mordhorst C. H., Saikku P., Thom D. H., Wang S. P. A new respiratory tract pathogen: Chlamydia pneumoniae strain TWAR. J Infect Dis. 1990 Apr;161(4):618–625. doi: 10.1093/infdis/161.4.618. [DOI] [PubMed] [Google Scholar]
- Hahn D. L., Dodge R. W., Golubjatnikov R. Association of Chlamydia pneumoniae (strain TWAR) infection with wheezing, asthmatic bronchitis, and adult-onset asthma. JAMA. 1991 Jul 10;266(2):225–230. [PubMed] [Google Scholar]
- Marrie T. J., Grayston J. T., Wang S. P., Kuo C. C. Pneumonia associated with the TWAR strain of Chlamydia. Ann Intern Med. 1987 Apr;106(4):507–511. doi: 10.7326/0003-4819-106-4-507. [DOI] [PubMed] [Google Scholar]
- Miller S. T., Hammerschlag M. R., Chirgwin K., Rao S. P., Roblin P., Gelling M., Stilerman T., Schachter J., Cassell G. Role of Chlamydia pneumoniae in acute chest syndrome of sickle cell disease. J Pediatr. 1991 Jan;118(1):30–33. doi: 10.1016/s0022-3476(05)81839-6. [DOI] [PubMed] [Google Scholar]
- Roblin P. M., Dumornay W., Hammerschlag M. R. Use of HEp-2 cells for improved isolation and passage of Chlamydia pneumoniae. J Clin Microbiol. 1992 Aug;30(8):1968–1971. doi: 10.1128/jcm.30.8.1968-1971.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saikku P., Leinonen M., Tenkanen L., Linnanmäki E., Ekman M. R., Manninen V., Mänttäri M., Frick M. H., Huttunen J. K. Chronic Chlamydia pneumoniae infection as a risk factor for coronary heart disease in the Helsinki Heart Study. Ann Intern Med. 1992 Feb 15;116(4):273–278. doi: 10.7326/0003-4819-116-4-273. [DOI] [PubMed] [Google Scholar]
- Wang S. P., Kuo C. C., Grayston J. T. Formalinized Chlamydia trachomatis organisms as antigen in the micro-immunofluorescence test. J Clin Microbiol. 1979 Aug;10(2):259–261. doi: 10.1128/jcm.10.2.259-261.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]


