Abstract
Objectives
To compare nosologist coding of death certificate’s underlying cause of death with adjudicated cause of death for subjects age 65+ in the Cardiovascular Health Study (CHS).
Design
Observational study.
Setting
Four communities: Forsyth County North Carolina (Wake Forest University), Sacramento County California (University of California at Davis), Washington County Maryland (Johns Hopkins University), and Pittsburgh Pennsylvania (University of Pittsburgh).
Participants
Men and women ages 65 and over participating in CHS, a longitudinal study of coronary heart disease and stroke, and who died through June 2004.
Measurements
The CHS centrally adjudicated underlying cause of death for 3194 fatal events from 6/1989–6/2004 using medical records, death certificates, proxy interviews and autopsies, and results were compared with underlying cause of death assigned by a trained nosologist based on death certificate only.
Results
Comparison of 3194 CHS vs. nosologist underlying cause of death revealed moderate agreement except for cancer (kappa=0.91, 95% CI:0.89–0.93). Kappas varied by category: CHD=0.61 (95% CI:0.58–0.64), stroke=0.59 (95% CI:0.54–0.64), COPD=0.58 (95% CI:0.51–0.65), dementia=0.40 (95% CI:0.34–0.45), and pneumonia=0.35 (95% CI:0.29–0.42). Differences between CHS and nosologist coding of dementia were found especially in older ages in both sex and race categories. CHS classified 340 (10.6%) of deaths due to dementia, while nosologist coding classified only 113 (3.5%) with dementia as the underlying cause.
Conclusion
Studies that use only death certificates to determine cause of death may result in misclassification and potential bias. Changing trends in cause-specific mortality in older individuals may be a function of classification process rather than incidence and case fatality.
Keywords: death certificates, mortality, vital statistics
INTRODUCTION
Death certificates are the main data source for many mortality studies. These data are often used to identify public health problems, allocate funding, and set new goals. Previous studies suggest that death certificates, compared with other data sources, may misclassify the underlying cause of death, especially in older individuals with multiple comorbidities. This misclassification has been attributed, in part, to variations in coding, unrecognized limitations of the death certificate format, and changing trends in diagnostic technology, such as magnetic resonance imaging (MRI) and molecular pathology, in the diagnosis and classification of various diseases such as cancer and dementia (1,2). Additionally, physicians tend to overstate cardiovascular causes of death compared with subsequent autopsy or review of hospital discharge data (3).
Diseases such as Alzheimer’s disease (AD) represent a leading cause of death in the elderly. Beginning with mortality data for 1994, AD in the United States became common enough to become a major category of cause of death (4). In some populations only a quarter of deaths in demented patients had this disease on the death certificate (5). Similar underreporting of deaths related to vascular dementia takes place. In some studies, less than half of vascular dementia related deaths were correctly classified (6). Disparities on death certificates were found in coding of pulmonary, cardiac and cancer co-morbidities in demented versus non-demented patients.
Inaccuracy in reporting the underlying cause of death for elderly patients may therefore mask the growing impact of dementia as an important cause of death and associated comorbidities. Inaccurate death certificate causes of death data for older individuals may limit interpretations of time trends, geographic differences, variations by demographic characteristics and changing risk factors and medical care. All of these problems have drawn attention to the potential benefit of revised nosology coding structures. In this paper, we compare nosologist coding of death certificate diagnosis of underlying cause of death to adjudicated cause of death for all fatal events in the Cardiovascular Health Study (CHS) cohort for deaths in ages 65 and over occurring through June 2004.
METHODS
The CHS is an observational study of the incidence and natural history of coronary heart disease (CHD) and stroke in men and women ages 65 and over. (7) Recruitment, design and methods have previously been described (8). Briefly, Medicare beneficiaries were recruited in four communities: Forsyth County North Carolina (Wake Forest University), Sacramento County California (University of California at Davis), Washington County Maryland (Johns Hopkins University), and Pittsburgh Pennsylvania (University of Pittsburgh). Initial recruitment of 5201 subjects was completed in 1989–1990, and a supplemental cohort of 687 African-Americans was recruited in 1992–93 resulting in a total recruitment yield of 5888. (8) The study underwent Institutional Review Board review and approval. All subjects provided informed consent to participate in the study. Annual assessments including various risk factor measurements and medical/personal history were completed through 1998–99 (Study Year 11), and again in 2005–2006 (Study Year 18).
Morbidity and mortality surveillance was conducted at every six-month interval after the baseline visit during each annual in-person assessment and semi-annual telephone surveillance call. Methods for ascertainment, investigation and adjudication of all clinical events, both morbid and fatal, have been previously described (9,10). In summary, deaths were ascertained at the field centers by proxy report, local obituaries, Social Security Death Index searches, searches of Medicare claims data, and other means. All staff and adjudicators were trained according to CHS protocol and procedures. Field center data collection included hospital, physician’s office and/or nursing home records, death certificates, autopsies, and narrative interviews from proxies providing circumstances of the death especially when it was out of the hospital. Abstracted data included hospital diagnostic and procedure codes with associated text fields, death certificate diagnoses, and other information pertaining to the study criteria for underlying cause of death categories. All deaths were locally classified and centrally adjudicated by a group of physicians representing each field center and the data coordinating center to determine underlying cause of death. A local physician adjudicator reviewed all the supporting documentation and assigned an underlying cause of death. Abstracted and adjudicated data were electronically transmitted, and copies of the abstraction forms and sterilized source documents were mailed to the data coordinating center in Seattle. Deaths packets from the four sites were compiled and distributed to the physician adjudicators for review at face-to-face central adjudications. Prior hospitalization codes, diagnoses, and adjudication results for all morbid events during the study were summarized to provide historical information leading to the death. Medicare data were used to identify unreported clinical events. Classification of each underlying cause of death was proposed using standardized criteria, with discussion being critical to the adjudication process. Both the cardiac and stroke committees’ adjudicators have remained stable throughout the study, and are strongly represented by geriatricians and other physicians experienced in the clinical syndromes and treatment of the elderly.
The CHS classification categories and definitions for underlying cause of death are shown in Table 1. Group 5 (Non-cardiovascular) provides the adjudication committee a text field for underlying cause of death, which is the condition that sets in motion the train of events leading to death. The text field list of causes is later grouped into subcategories. The adjudicators are not informed about the cause of death coding by the nosologist. Quality control efforts by readjudication for approximately 300 events, including of a sample of deaths (N=94), revealed good agreement, Kappa=0.78.
Table 1.
CHS Classification Definitions and Nosologist ICD Categories for Underlying Cause of Death
| Category/ICD Code | CHS Underlying Cause of Death Categories |
|---|---|
| 1 | Atherosclerotic coronary heart disease, includes: definite fatal MI (no known non-atherosclerotic cause, and definite MI within 4 weeks of death, definite fatal CHD (no known non-atherosclerotic cause, and one or both of the following: chest pain within 72 hours of death or a history of chronic ischemic heart disease in the absence of valvular heart disease or noischemic cardiomyopathy) and possible fatal CHD (no known non- atherosclerotic cause, and death certificate consistent with underlying cause) |
| 2 | Cerebrovascular (includes acute and late effect of stroke) |
| 3 | Atherosclerotic disease other than coronary or Cerebrovascular disease (includes ruptured abdominal aortic aneurysm and peripheral vascular disease) |
| 4 | Other cardiovascular disease, not codable as 1–3 (includes valvular heart disease, hypertensive renal disease, pulmonary embolism and endocarditis) |
| 5 | Non-cardiovascular disease (includes all other causes of death not codable as 1–4, natural, accidental, homicide and suicide |
| Nosologist Underlying Cause of Death ICD Code Categories
|
|
| 410–411,413– 414,429 | Coronary heart disease |
| 428 | Congestive heart failure |
| 434,436–438 | Cerebrovascular disease |
| 440–444,557 | Other atherosclerotic disease |
| 390–398,415–427 | Other cardiac disease |
| 290,294,331 | Dementia |
| 332 | Parkinson’s disease |
| 140–208 | Cancer |
| 490–496, 518–519 | Chronic pulmonary disease |
| 480–486, 507 | Pneumonia |
| 038, 599 | Sepsis, Urosepsis |
| 580–593 | Renal Failure |
| 570–579 | Liver Disease |
| 530–540, 555–569 | Gastrointestinal disease |
| 250–279 | Diabetes |
| 783 | Failure to thrive |
| 280–289 | Blood disease |
| Other | Assigned an underlying cause of death other than above |
CHS=Cardiovascular Health Study, ICD=International Classification of Diseases, MI=myocardial infarction, CHD=coronary heart disease
There were a very small number of deaths (n=74) for which no other documentation pertaining to the fatal event was available except for the death certificate. In these cases, other sources of information were used to assist in the CHS adjudication process including medical record data from prior morbid events, and data collected at the clinic visits or surveillance calls such as medical history and medications. These additional data collected over the duration of the study provided supplemental information above and beyond the death certificate alone, and therefore these cases were included in the analysis.
The CHS does not classify any deaths as due to an underlying cause of congestive heart failure. The CHS classification focuses on the etiology of the heart failure, which is considered a mechanism of death rather than an underlying cause. CHS classifies deaths as being from CHD or valvular disease most commonly when the mechanism is congestive heart failure (CHF). In this analysis, the CHF deaths classified by the nosologist were combined with the nosologist CHD deaths in an effort to harmonize the two classification systems for analysis.
In a patient who had a stroke with a persistent aspiration and who later died of pneumonia, even if this pneumonia occurred years after the stroke, CHS classified the death due to stroke (‘late effects of stroke’). Nosologist coding would reflect the pneumonia as the underlying cause in this case where the stroke was remote and may not have even been mentioned on the death certificate.
The CHS identified dementia as the underlying cause of death in many older individuals, and the subsequent immediate causes of death such as pneumonia and septicemia that occurs at the time of the death were secondary to the dementia. Other CHS coding rules include rarely classifying risk factors such as diabetes, hypertension and hyperlipidemia as an underlying cause of death. The CHS focuses on the specific organ system leading to the death such as CHD, peripheral vascular disease, associated diabetes-related infection, and renal failure with refusal or withdrawal of dialysis.
All death certificates were also coded for underlying cause of death by a trained and experienced nosologist without any other supporting information about the circumstances of death or any knowledge of the central adjudication committees’ classification. All nosologists coding death certificates are trained to code underlying cause of death using standardized general principles and selection rules based on the listed causes of death on the certificates. Interpretations are made on the probability of the sequence of the conditions using detailed algorithms and tables with instructions for determining causal relationships and modifications for complex co-morbidities. These principles and rules were established by the World Health Organization to be used internationally, and the National Center for Health Statistics enhanced the documentation based on the Automated Classification of Medical Entities (ACME) selection system using the International Classification of Diseases (ICD). (11) Once the nosologist determined the underlying cause of death, these ICD codes were grouped into categories, also shown in Table 1. The ninth revision of the codes was used in order to maintain consistency over the duration of the study (12). Nosologist coding only included a 3-digit integer code without any digits to the right of decimal.
Statistical analyses were conducted using SPSS and SAS Statistical Packages. Frequency distribution and descriptives were run prior to the analysis on both nosologist coded data and the mortality review form completed at the death adjudication. SPSS Chi-square test was used to compare nosologist coding with CHS mortality review coding. P-values of <0.05 were considered statistically significant. SAS was used to determine measures of agreement (Kappa) for individual events classified by the two groups. Although neither the CHS nor nosologist coding are considered a ‘gold standard’, sensitivity and specificity are reported to reflect the comparison of the two methods, based on the additional data in CHS used to supplement the death certificate alone. The analyses presented here represent all centrally adjudicated deaths through June 2004 with an associated nosologist ICD-9 code for underlying cause of death.
RESULTS
A total of 3209 deaths were adjudicated in CHS covering the period through June 30, 2004. After removing any deaths without a nosologist code, the total number of deaths for this analysis is 3194; virtually all deaths in the cohort through this period. The agreement between categorical causes of death for the CHS classification and nosologist codes are shown in Table 2.
Table 2.
Agreement between Nosologist Underlying Cause of Death using CHS Adjudication as the Reference, with 95% Confidence Interval, Deaths through June 2004
| Nosologist ICD | Nosol=yes | Nosol=yesCH | Nosol=no | Nosol=no | Sensitivity | Specificity | Kappa | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Disease Category | Codes | CHS=yes | S=no | CHS=yes | CHS=no | % | 95%CI | % | 95%CI | 95% | CI |
| Coronary Heart Disease & Congestive Heart | 410–411, 413– | ||||||||||
| Failure | 414, 428, 429 | 612 | 265 | 220 | 2097 | 74 | 70, 77 | 89 | 87, 90 | 0.61 | 0.58,0.64 |
| Cerebrovascular Disease Other | 430–434, 436– 438, 557 | 195 | 137 | 90 | 2772 | 68 | 63, 74 | 95 | 94, 96 | 0.59 | 0.55,0.64 |
| Atherosclerosis Other | 440–444, 557 | 34 | 45 | 39 | 3076 | 47 | 35, 59 | 99 | 98, 99 | 0.43 | 0.33,0.53 |
| Cardiovascular | 390–398, 415–427 | 41 | 101 | 50 | 3002 | 45 | 35, 56 | 97 | 96, 97 | 0.33 | 0.25,0.41 |
| Cancer | 140–208 | 692 | 35 | 68 | 2399 | 91 | 89, 93 | 99 | 98, 99 | 0.91 | 0.89,0.93 |
| Dementia | 290, 294, 331 | 97 | 16 | 243 | 2854 | 29 | 24, 34 | 99 | 99,99 | 0.40 | 0.34,0.45 |
| Pneumonia | 480–486, 507 | 67 | 118 | 94 | 2915 | 42 | 34, 50 | 96 | 95, 97 | 0.35 | 0.29,0.42 |
| Chronic Respiratory | 490–496, 518–519 | 95 | 40 | 87 | 2972 | 52 | 45, 60 | 98 | 98, 99 | 0.58 | 0.51,0.65 |
CHS=Cardiovascular Health Study, ICD=International Classification of Diseases
Based on the CHS adjudication, 26.1% of overall deaths were attributed to CHD, 23.8% to cancer, 10.6% to dementia, 8.9% to cerebrovascular disease, 5.7% to chronic pulmonary disease, 5% to pneumonia, and the remaining to other causes. Based on the nosologist coding, 27.5% were from CHD/CHF, 22.8% were due to cancer, 10.4% to cerebrovascular disease, 5.8% to pneumonia, and 4.2% to chronic pulmonary disease. Of the 760 CHS cancer and 727 nosologist cancer deaths, both classified 692 of the deaths as cancer (Kappa =0.91, 95% CI: 0.89–0.93), and both sensitivity and specificity were high at 91% and 99%, respectively. Although specificity remained high in all other categories, sensitivity varied greatly ranging from only 29% for dementia to 74% in the combined CHD/CHF category. Of the 832 CHS CHD deaths and 877 nosologist CHD/CHF deaths, both matched 612 as CHD (Kappa =0.61, 95% CI: 0.58–0.64). Unlike cancer and CHD, other causes of death were found to have similar overall totals; however the actual cases classified by both adjudications were different. For example, cerebrovascular disease was the cause of death for 285 CHS cases and 332 nosologist cases yet both agreed on cerebrovascular disease as the cause of death for only 195 (Kappa =0.59, 95% CI: 0.54–0.64). Similarly, for chronic pulmonary disease CHS classified 182 deaths versus 135 by the nosologist yet only 95 were classified as chronic pulmonary disease by both (Kappa =0.58, 95% CI: 0.51–0.65). Pneumonia was classified by CHS in 161 cases, 185 by the nosologist, but only 67 were classified by both (Kappa=0.35, 95% CI: 0.29–0.42). In contrast to the 10.6% of cases classified as dementia by CHS, only 3.5% of the nosologist coded deaths were attributed to dementia. CHS classified 340 deaths from dementia while the nosologist classified only 113 dementia deaths, and 97 deaths were considered to be from dementia by both (Kappa =0.40, 95% CI: 0.34–0.45). The remaining figures focus on the causes of death with the greatest number of cases.
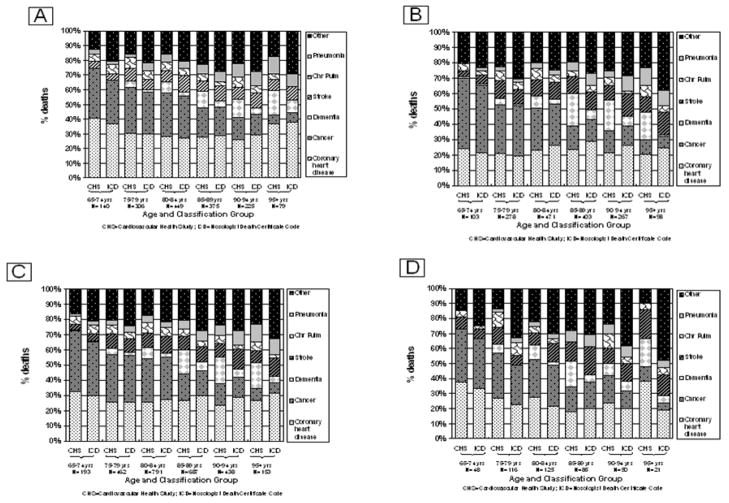
Underlying cause of death as coded by CHS compared to the nosologist by both gender and age are shown in Figure 1A and B.
Figure 1.
Figure 1A. CHS and Nosologist Underlying Cause of Death by Age, Men (N=1574)
Figure 1B. CHS and Nosologist Underlying Cause of Death by Age, Women (N=1620)
Figure 1C. CHS and Nosologist Underlying Cause of Death by Age, White (N=2724)
Figure 1D. CHS and Nosologist Underlying Cause of Death by Age, Black (N=445)
For both genders in the youngest age group, cancer and CHD comprised the majority of deaths (66–75% of deaths in men and 65–70% of deaths in women), and remained the leading underlying causes of death up to the oldest age group. In the three oldest age groups for men, the CHS classified dementia as the third leading underlying cause of death compared with stroke by the nosologist. In the oldest men, cancer was no longer among the top three leading causes of death, and dementia became the second leading cause of death by CHS coding. Dementia became the second leading underlying cause of death in women 85 and over in CHS as compared to stroke for nosologist coding.
Cause of death by age and race are shown in Figure 1C and D. Cancer and CHD were the two leading underlying causes of death in both whites and blacks for 65–94 year olds. In 85–89 year old whites, dementia was the third leading underlying cause of death by CHS while stroke remained the third leading underlying cause by the nosologist. In 90–94 and 95 plus year old whites, dementia was to the second leading underlying cause of death by CHS. The nosologist continued to classify stroke as the third leading underlying cause of death in the oldest whites. Stroke was the third leading underlying cause of death in the youngest group by both classifications, and remained either second or third by the nosologist coding in all age groups. However, CHS classified dementia at the same proportion as CHD as the second leading underlying cause of death in 80–84 year old blacks, second in 85–89 year olds and tied for second with stroke in the oldest age group.
DISCUSSION
Comparison of the adjudicated CHS underlying cause of death with the nosologist coding of death certificates resulted in some important differences. The generally accepted leading causes of death in older people, including coronary heart disease, cancer and stroke, were well represented in both classifications (2). However, although the total number of deaths by both CHS and the nosologist for CHD and stroke was similar, the actual deaths classified by each method were often different, and the agreement was only modest.
Differences in the classification findings were primarily related to dementia as the underlying cause of death. By age 75, dementia emerged as a prominent cause of death only in CHS. The CHS adjudication placed dementia as the second or third leading cause of death in the two older age groups for both genders and races. This was not consistent with nosologist coding. The nosologist coding of CHS dementia cases often reflected coding by the more immediate causes of death such as pneumonia (N=50) and sepsis (N=10) that were available on the death certificate, when information on underlying dementia was not documented on the certificate. In other instances, the nosologist coded deaths as cardiovascular (N=46). Underreporting of dementia on death certificates has been observed in other studies (5,13).
The CHD and stroke mortality rates were similar for the CHS and the nosologist classification. However, the agreement between the two methods was only modest, and a large number of individuals classified as deaths from one cause by the nosologist could be considered misclassified from the point of view of CHS. In studies of older adults, methods used to classify causes of death should be clearly explained (10). It is possible that variations among studies in association of risk factors and fatal outcomes may be a function of the classification system for causes of death.
The lack of physician training in completing cause of death information on certificates has contributed to the problems associated with using death certificates as the sole source of mortality tracking (3). Especially in nursing homes where deaths in elderly are common, physicians are expected to complete death certificates on patients with whom they may have had little or no contact, have limited clinical documentation, and may have little knowledge of the actual events immediately preceding the death. The underlying cause of death is sometimes omitted from the certificate entirely, which may include only the immediate cause or a list of comorbid conditions not necessarily interconnected but possibly contributing to the death. Training of physicians should include capture of the underlying, not just immediate or primary cause. Death certificates with the only cause of death as ‘cardiorespiratory arrest’ are still being accepted, despite evidence suggesting better training at completion of certificates results in a reduction of the overuse of cardiac causes (14). Twelve such cases listing only ‘cardiorespiratory arrest’ were noted in CHS.
CHS classified only an underlying cause of death without classifying any immediate or secondary causes. The nosologist was charged with coding only an underlying cause as well. Limiting the classification system in this way may have led to biases forcing the selection of one single cause when the deaths were multifactorial due to other contributing conditions. A coding scheme to capture multiple causes or comorbid conditions could have increased the agreement between the two classifications. The CHS physician adjudicators were primarily geriatricians, potentially leading to another bias towards classifying underlying causes of death more common to geriatric syndromes such as dementia. This may have resulted in another explanation for the large differences in agreement with the nosologist, who may classify cases in a different manner.
The CHS methods to classify cause of death used very detailed and comprehensive collection and review of documentation. Mortality statistics still remain the only easily accessible complete ascertainment of the comparative health of populations over time, across and within populations. Most of the deaths in the United States occur in older individuals. The many comorbid conditions common in older adults sometimes make it difficult to attribute death to a single specific underlying cause of death. One study following Alzheimer’s disease cases from initial diagnosis to death revealed impairment of cognition may decrease patients’ ability to recognize and report medical symptoms, and thus impact their clinical course. (15) The growing epidemic of dementia-related deaths is masked by the current vital statistics. The critical question is whether these older individuals die with dementia or because of their dementia.
CONCLUSION
There is no national database of incident chronic disease such as CHD in the United States except in certain areas and states that have cancer registries. Medicare provides counts of hospitalizations but does not distinguish between prevalent and incident events. There is also no national database that measures case fatality, the other component of determination of mortality rates. The measure of public health, therefore, depends on quality mortality statistics (16,17).
Unfortunately, without high quality cause-specific mortality data, variation in disease rates by geographic area, by demographic characteristics and, most important, by time are difficult to interpret (18–21). Some of these include determining whether the reported rising age-specific death rate due to dementia is simply a change in certificate practices and better diagnosis or whether it is an increased incidence; possibly a function of better survival to older ages of at-risk populations with vascular disease, hypertension, diabetes, etc., which may be risk determinants for vascular brain pathology of dementia. Similarly, it is difficult to determine if the apparent increase in septicemia death is just a function of death certificate coding practices, and if the growing interest in diabetes mellitus will result in an increase in diabetes listed as the underlying cause of death and an “epidemic” of diabetes mortality. The results of this analysis comparing detailed adjudication of fatal events to death certificate coding is not evidence that one approach is superior, but rather to illustrate that the differences between the approaches do impact trends and geographic variation in mortality statistics.
Supplementary Material
Acknowledgments
The research reported in this article was supported by contracts N01-HC-85079 through N01-HC-85086, N01-HC-35129, N01 HC-15103, N01 HC-55222, and U01 HL080295 from the National Heart, Lung, and Blood Institute, with additional contribution from the National Institute of Neurological Disorders and Stroke. A full list of participating CHS investigators and institutions can be found at http://www.chs-nhlbi.org.
Participating CHS Investigators and Institutions
Steering Committee Chairman: Curt D. Furberg, MD PhD, Wake Forest University School of Medicine.
NHLBI Project Office: Jean Olson, MD MPH.
Wake Forest University School of Medicine: Gregory L. Burke, MD.
Wake Forest University — ECG Reading Center: Pentti Rautaharju, MD PhD, Ronald Prineas, MD PhD.
University of California, Davis: John Robbins, MD MHS.
The Johns Hopkins University: Linda P. Fried, MD MPH.
The Johns Hopkins University — MRI Reading Center: Nick Bryan, MD, PhD; Norman Beauchamp, MD, MHS; David Yousem, MD MBA.
University of Pittsburgh: Lewis H. Kuller, MD DrPH.
University of Pittsburgh - MRI Archive: James T. Becker, PhD.
University of California, Irvine — Echocardiography Reading Center (baseline): Julius M. Gardin, MD.
Georgetown Medical Center — Echocardiography Reading Center (follow-up): John S. Gottdiener, MD.
New England Medical Center, Boston — Ultrasound Reading Center: Daniel H. O’Leary, MD.
University of Vermont — Central Blood Analysis Laboratory: Russell P. Tracy, PhD.
University of Arizona, Tucson — Pulmonary Reading Center: Paul Enright, MD.
Retinal Reading Center - University of Wisconsin: Ronald Klein, MD.
University of Washington — Coordinating Center: Richard A. Kronmal, PhD
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Diane Ives developed the concept, design, collection and interpretation of data, and preparation of manuscript. Paulraj Samuel contributed to the preparation of the manuscript. Bruce Psaty contributed to the design, interpretation of results and preparation of the manuscript. Lewis Kuller was the principal investigator of the Pittsburgh field center and contributed to the data collection, interpretation of results and preparation of the manuscript. All authors reviewed and approved the last version of the manuscript.
References
- 1.Johansson LA, Westerling R. Comparing hospital discharge records with death certificates: Can the differences be explained? J Epidemiol Community Health. 2002;56:301–308. doi: 10.1136/jech.56.4.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shayoun NR, Lentzer H, Hoyert D, et al. Trends in causes of death among the elderly. Aging Trends. 2001;1:1–10. doi: 10.1037/e620692007-001. [DOI] [PubMed] [Google Scholar]
- 3.Lakkireddy DR, Gowda MS, Murray CW, et al. Death certificate completion: how well are physicians trained and are cardiovascular causes overstated? Am J Med. 2004;117:492–498. doi: 10.1016/j.amjmed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Hoyert DL, Rosenberg HM. Alzheimer’s Disease as a cause of death in the United States. Public Health Rep. 1997;112:497–505. [PMC free article] [PubMed] [Google Scholar]
- 5.Ganguli M, Rodriguez EG. Reporting of dementia on death certificates: A community study. J Am Geriatr So. 1999;47:842–849. doi: 10.1111/j.1532-5415.1999.tb03842.x. [DOI] [PubMed] [Google Scholar]
- 6.Thomas BM, Starr JM, Whalley LJ. Death certification in treated cases of presenile Alzheimer’s disease and vascular dementia in Scotland. Age Ageing. 1997;26:401–406. doi: 10.1093/ageing/26.5.401. [DOI] [PubMed] [Google Scholar]
- 7.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 8.Tell GS, Fried LP, Hermanson B, et al. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:358–366. doi: 10.1016/1047-2797(93)90062-9. [DOI] [PubMed] [Google Scholar]
- 9.Psaty BM, Kuller LH, Bild D, et al. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–277. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- 10.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 11.National Vital Statistics System Instruction Manual. National Center for Health Statistics Web Site. [Updated January 16, 2008. Accessed June 30, 2008]; http://www.cdc.gov/nchs/about/major/dvs/im.htm.
- 12.International Classification of Diseases 9th Revision Clinical Modification. 5. Salt Lake City, UT: Medicode Publications; 1996. [Google Scholar]
- 13.Macera CA, Sun RKP, Yeager KY, et al. Sensitivity and specificity of death certificate diagnoses for dementing illnesses, 1988–1990. J Am Geriatr Soc. 1992;40:479–481. doi: 10.1111/j.1532-5415.1992.tb02015.x. [DOI] [PubMed] [Google Scholar]
- 14.Lakkireddy DR, Vasarakodu KR, Vacek JL, et al. Improving death certificate completion: A trial of two training interventions. J Gen Intern Med. 2007;22:544–548. doi: 10.1007/s11606-006-0071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kukull WA, Brenner DE, Speck CE, et al. Causes of death associated with Alzheimer disease: Variation by level of cognitive impairment before death. J Am Geriatr Soc. 1994;42:723–726. doi: 10.1111/j.1532-5415.1994.tb06531.x. [DOI] [PubMed] [Google Scholar]
- 16.Lopez AD, AbouZahr C, Shibuya K, et al. Keeping count: births, deaths, and causes of death. Lancet. 2007;370:1744–1746. doi: 10.1016/S0140-6736(07)61419-6. [DOI] [PubMed] [Google Scholar]
- 17.AbouZahr C, Cleland J, Coullare F, et al. The way forward. Lancet. 2007;370:1791–1799. doi: 10.1016/S0140-6736(07)61310-5. [DOI] [PubMed] [Google Scholar]
- 18.Nolte E, Martin McKee CM. Measuring the health of nations: Updating an earlier analysis. Health Aff. 2008;27:58–71. doi: 10.1377/hlthaff.27.1.58. [DOI] [PubMed] [Google Scholar]
- 19.Ruzicka LT, Lopez AD. The use of cause-of-death statistics for health situation assessment: National and international experiences. World Health Stat Q. 1990;43:249–258. [PubMed] [Google Scholar]
- 20.Kelson M, Farebrother M. The effect of inaccuracies in death certification and coding practices in the European Economic Community (EEC) on international cancer mortality statistics. Int J Epidemiol. 1987;16:411–414. doi: 10.1093/ije/16.3.411. [DOI] [PubMed] [Google Scholar]
- 21.Tobias M, Jackson G. Avoidable mortality in New Zealand, 1981–97. Aust N Z J Public Health. 2001;25:12–20. doi: 10.1111/j.1467-842x.2001.tb00543.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.