Abstract
It is well known that exposure to one antigen can modulate the immune responses that develop following exposure to closely related antigens. It is also known that the composition of the repertoire can be skewed to favor epitopes shared between a current infection and a preceding one, a phenomenon referred to as “original antigenic sin.” It was of interest, therefore, to investigate the antibody response that develops following exposure to the malaria vaccine candidate homologue Plasmodium yoelii MSP119 in mice that had previously experienced malaria infection and vice versa. In this study, preexposure of mice to Plasmodium yoelii elicited native anti-MSP119 antibody responses, which could be boosted by vaccination with recombinant MSP119. Likewise, infection of MSP119-primed mice with P. yoelii led to an increase of anti-MSP119 antibodies. However, this increase was at the expense of antibodies to parasite determinants other than MSP119. This change in the balance of antibody specificities significantly affected the ability of mice to withstand a subsequent infection. These data have particular relevance to the possible outcome of malaria vaccination for those situations where the vaccine response is suboptimal and suggest that suboptimal vaccination may in fact render the ultimate acquisition of natural immunity more difficult.
The 19-kDa carboxyl-terminal fragment of merozoite surface protein 1 (MSP119) is a leading malaria vaccine candidate (reviewed in reference 6). Immunization of monkeys (11, 12) or mice (1, 8) with recombinant MSP119 confers protection against challenge infection. Studies using mouse models have clearly shown that immunity induced by MSP119 immunization is dependent on specific antibodies (Abs) present at the time of challenge (1, 7, 8) and requires an active immune response postchallenge involving B cells and CD4+ T cells (9).
An ideal malaria vaccine should effectively induce protective immunity in both naive individuals and those populations living in areas of endemicity. Therefore, immune responses generated in response to vaccination in both naive and exposed individuals should be considered in studies to develop a malaria vaccine. While MSP119 has been shown to be a promising malaria vaccine candidate, we have found that CD4+ T cells specific to a helper epitope on MSP119 are deleted via apoptosis during malaria infection (18). As a result, spleen cells from infected mice respond to parasite antigens significantly less than spleen cells from uninfected mice. This may reflect the situation in humans, where antigen-specific immune responses are suppressed during Plasmodium falciparum infection (10). It is important, therefore, to assess vaccine efficacy in individuals previously exposed.
Conversely, it is important to consider the impact of vaccination on the subsequent ability of the parasite to interact with the immune system and consequently generate both MSP119-specific Abs and Abs specific for other parasite antigens which may contribute in a significant way to the ultimate development of immunity. Francis (4) and Fazekas de St Groth (3) reported almost 50 years ago that prior exposure to one strain of an organism could skew the immune response to subsequent strains toward those antigenic determinants that are shared between the strains at the expense of novel determinants expressed on the new strain. The term “original antigenic sin” was coined to describe this phenomenon. We were interested to explore whether malaria subunit vaccination might prevent the development of protective Abs specific for those antigens other than the subunit vaccine, and if so, to determine the mechanism of the effect.
The experiments in this study were thus designed to model in the mouse those situations where malaria-preexposed individuals receive vaccination and also where vaccinated individuals from a nonmalaria area might travel to regions with malaria transmission.
MATERIALS AND METHODS
Experimental animals and parasites.
Six- to 8-week-old female BALB/c and B10.S mice were purchased from Animal Resources Center, Willeton, Australia. Plasmodium yoelii YM (lethal strain) and Plasmodium chabaudi were used.
Immunization protocol.
To investigate the effectiveness of MSP119 vaccination in malaria-preexposed animals, groups of BALB/c mice were infected with P. yoelii YM and were then treated daily 4 days later with three consecutive doses of 0.2 mg/ml pyrimethamine. This procedure is referred to as infection/cure. Three weeks later, all mice were vaccinated with phosphate-buffered saline (PBS) or 20 μg MSP119 formulated in complete Freund's adjuvant (CFA) (Sigma, St Louis, MO). Control groups consisted of mice that were not infected but were vaccinated with the same dose of antigens (Table 1). Five weeks after vaccination, mice were challenged intravenously with 104 P. yoelii YM-parasitized red blood cells (RBC). Vaccination of preexposed mice is hereafter referred to as protocol 1.
TABLE 1.
Experimental protocol for malaria-preexposed mice (protocol 1)a
| Group | Exposure to P. yoelii YM | Vaccine |
|---|---|---|
| i | − | PBS |
| ii | − | MSP119 |
| iii | + | PBS |
| iv | + | MSP119 |
There were five mice in each group. All mice were treated with pyrimethamine and challenged with P. yoelii YM.
To examine the effect of malaria infection on vaccinated animals, groups of BALB/c mice were immunized with PBS or 20 μg MSP119 formulated in CFA. Three weeks later, mice were subjected to an infection/cure or were revaccinated with 20 μg MSP119 (Table 2). All mice, including control groups, were given the same curative dose of pyrimethamine. Five weeks after the last immunization, mice were challenged intravenously with 104 P. yoelii YM-parasitized RBC. Exposure of prevaccinated mice to an infection/cure or vaccination with MSP119 is hereafter referred to as protocol 2.
TABLE 2.
Experimental protocol for prevaccinated mice (protocol 2)a
| Group | Vaccine | Boost |
|---|---|---|
| v | PBS | Infection/cure |
| vi | MSP119 | Infection/cure |
| vii | MSP119 | MSP119 |
There were five mice in each group. All mice were treated with pyrimethamine and challenged with P. yoelii YM.
Determination of Ab responses.
Blood samples were taken from each individual mouse on the same day prior to each infection or vaccination. Levels of Abs in sera were determined by enzyme-linked immunosorbent assay (ELISA) as described previously (8). Briefly, Maxisorb immunoplates (Nalge Nunc International, NY) were coated overnight at 4°C with 100 μl of 0.3-μg/ml MSP119 or 10-μg/ml crude parasite antigens. After three washes with 0.05% Tween-PBS, wells were blocked with 200 μl of 1% bovine serum albumin (BSA) (Sigma, St. Louis, MO) in PBS and incubated for 1 h at 37°C. Supernatants were discarded, and 100 μl of serial dilutions of sera in 1% BSA in Tween-PBS was added. After incubation at 37°C for 1 h, wells were washed and 100 μl of a 1:3,000 dilution of horseradish peroxidase-conjugated sheep anti-mouse immunoglobulin G (Silenus, Australia) was added. After incubation at 37°C for 1 h, wells were washed, 100 μl of substrate solution (2,2-azino-di-[ethyl-benzithiozolin sulfonate]; Sigma) was added, and wells were incubated at room temperature for 30 min. The absorbance was read at 405 nm.
Statistical analysis.
Comparisons among experimental groups by Student's t test were performed using a statistical analysis program of Sigma Plot. The levels of peak parasitemia were compared among experimental groups. Significance was set at a P value of <0.05.
RESULTS
Ab responses following vaccination in P. yoelii-exposed mice.
The first set of experiments was performed to determine whether prior exposure to P. yoelii affected the ability of mice to respond to MSP119 vaccination. Sera were collected at different time points, and Ab responses to MSP119 or crude P. yoelii parasite antigens were determined. Sera taken prior to any experiments did not contain Abs specific to MSP119 or P. yoelii antigens (data not shown). Mice that had been exposed to P. yoelii infection/cure are referred to as P. yoelii exposed. Mice that had not received an infection followed by drug cure are referred to as nonexposed. Sera taken prior to MSP119 immunization or PBS immunization are referred to as preimmunization sera, whereas sera taken after immunization or after infection/cure are referred to as postimmunization or postinfection sera, respectively.
The level of Abs against MSP119 or whole parasite antigens in P. yoelii-exposed mice did not change significantly after PBS immunization (Fig. 1C and G). P. yoelii-exposed mice had developed low levels of anti-MSP119 Abs before MSP119 boosting, and the levels of the Abs increased after boosting but did not differ from those for nonexposed animals that received MSP119 immunization (Fig. 1B versus D). Boosting with MSP119 had no effect on the level of anti-P. yoelii Abs in P. yoelii-exposed mice (Fig. 1H). There was no effect of treatment on the distribution of the isotype of the MSP119-specific Abs (Fig. 2).
FIG. 1.
Ab responses specific to MSP119 (A to D) or P. yoelii antigens (E to H). Nonexposed (A, B, E, and F) and P. yoelii-preexposed (C, D, G, and H) mice were immunized with PBS or 20 μg MSP119 as indicated. Sera taken 5 weeks after vaccination were compared with preboost sera by ELISA. The data show the means ± standard errors for five mice. O.D., optical density.
FIG. 2.

Isotypes of Abs specific to MSP119. Malaria-nonexposed or -preexposed mice were immunized with 20 μg MSP119. Pooled sera were diluted 1:5,000 before analysis by ELISA. O.D., optical density.
The data demonstrate that exposure to P. yoelii elicits an Ab response to MSP119 which could be boosted by MSP119 vaccination and that prior exposure to P. yoelii did not affect the Ab response to vaccination with MSP119.
Ab responses following infection of MSP119-vaccinated animals.
Mice were given a single injection of MSP119 or PBS in CFA as described in Materials and Methods (protocol 2). Infection/cure of PBS-immunized mice only slightly enhanced the levels of Abs against MSP119 (Fig. 3A). Sera from mice that had been primed with MSP119 contained Abs to the antigen, with levels of Abs increasing further following either an infection/cure (Fig. 3B) or MSP119 boosting (Fig. 3C). Levels of Ab against P. yoelii increased in all groups following infection/cure or MSP119 boosting (Fig. 3D to F). These data show that exposure to P. yoelii resulted in an increase in Ab response to MSP119.
FIG. 3.
Ab responses specific to MSP119 (A to C) or P. yoelii antigens (D to F). PBS-primed (A and D) and MSP119-primed (B, C, E, and F) mice were boosted with one episode of infection/cure or 20 μg MSP119 as indicated. Sera were analyzed by ELISA. The data show the means ± standard errors for five mice. O.D., optical density.
The distribution of the MSP119-specific Ab isotypes of MSP119-primed mice that were boosted by an infection/cure was similar to that for mice receiving a second MSP119 vaccination (Fig. 4).
FIG. 4.

Isotypes of Abs specific to MSP119. MSP119-primed mice were boosted by infection/cure or MSP119 vaccination. Pooled sera were diluted 1:5,000 before analysis by ELISA. O.D., optical density.
Protection against challenge infection.
Five weeks after the last immunization of the above groups, all mice were challenged with 104 P. yoelii YM-parasitized RBC. Parasitemia was then monitored. Figure 5 shows levels of parasitemia for mice that received the different protocols of immunization. Nonexposed mice that were given PBS succumbed to the infection within 7 days (Fig. 5A). All five nonexposed mice given a single immunization dose with MSP119 developed parasitemia; two animals died, and three were able to eliminate parasites (Fig. 5B). It should be noted, however, that mice given a full MSP119 vaccination schedule (four doses of MSP119) are completely protected (8); that protocol was not followed here so as to monitor and compare the effects of prior P. yoelii exposure and the impacts of suboptimal vaccination on the induction of immunity following parasite exposure.
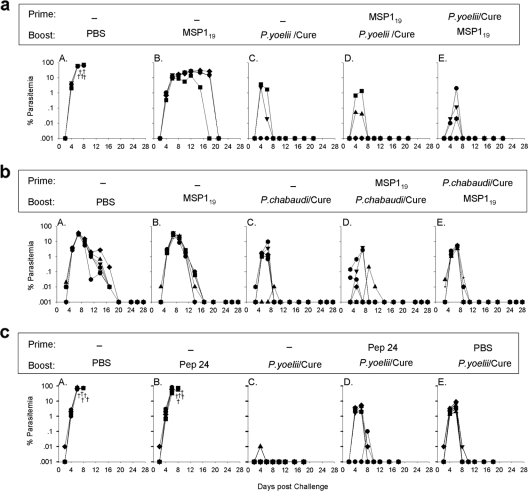
FIG. 5.
Parasitemia during challenge infection. Experimental treatments are indicated above each graph. Five weeks later all mice were challenged with 104 P. yoelii YM-parasitized RBC. The data show % parasitemia for five individual mice and represent one of five independent experiments with similar findings. Cross symbols indicate the days on which mice died.
P. yoelii-exposed mice that were immunized with PBS were able to control parasite growth, with only one animal showing a peak of 0.01% parasitemia on day 8 (Fig. 5C). Vaccination of P. yoelii-exposed animals with MSP119 also conferred protection, although two of five animals developed parasitemia with peaks of 0.02 and 3.8% (geometric mean peak parasitemia: 0.04%) (Fig. 5D).
PBS-immunized mice that were subsequently given an infection/cure developed patent parasitemia (geometric mean peak parasitemia: 0.21%) but were able to control parasite growth (Fig. 5E). All five MSP119-vaccinated mice that were given an infection/cure also showed patent parasitemia during the challenge infection (geometric mean peak parasitemia: 1.65%) (Fig. 5F). One of five mice that had been vaccinated with two doses of MSP119 died by day 9 postchallenge (Fig. 5G); one had no detectable parasitemia, and three animals showed patent parasitemia.
Mice which received MSP119 vaccination prior to infection/cure (protocol 2) (Fig. 5F) developed a mean peak parasitemia significantly higher than that developed by mice that received infection/cure prior to MSP119 vaccination (protocol 1) (geometric mean peak parasitemia of 1.65% versus 0.04%; P < 0.05).
Prior vaccination with MSP119 impeded the ability of mice to produce Abs to other determinants on the parasite.
We were concerned that prior exposure to MSP119-CFA or, to a lesser extent, PBS-CFA might alter the ability of parasite exposure to induce robust immunity. Since immunity induced by prior exposure to P. yoelii is believed to be mediated primarily by Abs (8), we asked whether prior vaccination with MSP119 impeded the ability of mice to generate an Ab response to other determinants on the parasite. Sera from MSP119-vaccinated P. yoelii-infected mice (from Fig. 5F) were tested in an inhibition ELISA in which free MSP119 was premixed with sera to absorb MSP119-specific Abs. The sera were then tested for their ability to recognize MSP119 and whole P yoelii parasites. The results (Fig. 6) demonstrate that free MSP119 can effectively block MSP119-specific Abs from recognizing MSP119 (Fig. 6B). However, there was also a significant reduction in the ability of the sera to respond to P. yoelii when the sera were blocked with free MSP119 (Fig. 6D). By comparison, MSP119-blocked sera from mice that had not been exposed to MSP119 but had been exposed to P. yoelii infection did not significantly affect Ab binding to P yoelii antigens at any of the serum dilutions tested (1/300 to 1/2,400) (Fig. 6C). These data are consistent with the reduced protection seen when P. yoelii-exposed mice were previously exposed to MSP119 (Fig. 5E versus F, geometric mean peak parasitemia of 0.21% versus 1.65% [P < 0.05]; Fig. 5F versus D, geometric mean peak parasitemia of 1.65% versus 0.04% [P < 0.05]), resulting in part from a reduced ability of MSP119-primed mice to generate an effective Ab response to P. yoelii antigens other than MSP119.
FIG. 6.
Ab specific to MSP119 and P. yoelii antigen in mouse sera detected by inhibition ELISA. Mice were primed with MSP119, followed by boost with infection/cure (C and D) or primed with infection/cure followed by boost with PBS (A and B). Anti-MSP119 Abs (A and C) and anti-P. yoelii Abs (B and D) were measured before and after blocking with excess free MSP119 antigen. O.D., optical density.
Impaired protective immunity was exclusively induced by the suboptimal vaccination of a particular antigen.
To confirm that the impaired protective immunity in MSP119-primed mice (Fig. 5F) was indeed induced by prior exposure to MSP119 antigen, a similar experimental approach was performed with B10.S mice. Because B10.S mice do not respond to MSP119 (14, 16), we expected that this approach would not affect the protective immunity following MSP119 priming and boosting by infection/cure. As shown in Fig. 7a, similar to the mice that were exposed to an infection/cure and boosted with MSP119 (7a, E), MSP119-primed B10.S mice that were boosted with an infection/cure were completely protected against parasite challenge (7a, D). We have previously reported the immune response to MSP119 in B10.S mice in extensive detail (14). These mice were unable to produce anti-MSP119 Abs and developed high parasitemia after infection.
FIG. 7.
Parasitemia during challenge infection. Experimental treatments are indicated above each graph. Five weeks later all mice were challenged with 104 P. yoelii YM-parasitized RBC (a and c) or P. chabaudi (b). The data show % parasitemia for five individual mice and represent one of three independent experiments with similar findings. Cross symbols indicate the days on which mice died.
Because MSP119 used in this experiment was derived from P. yoelii, this suboptimal vaccination should not affect the protective immunity induced by exposure to other species of parasites. As expected, the MSP119-primed BALB/c mice that had been given an infection/cure with P. chabaudi parasites had a level of parasitemia following challenge similar to that of mice that received an infection/cure followed by boosting with MSP119 when challenged with P. chabaudi (Fig. 7b, D versus E). To further confirm that the impaired protective immunity induced by the suboptimal vaccination was exclusively due to the immune responses to antibody production, a T-cell epitope (18) from MSP119 (peptide 24 [p24], EPTPNAYYEGVFCSSS) (18) was also used in this study. p24 priming had no ability to alter the level of protection, as shown in Fig. 7c, D. Collectively, the data demonstrate that an impaired protective immune response was induced by the suboptimal vaccination with MSP119.
DISCUSSION
The benefit of a malaria vaccine is dependent on its effectiveness in preventing disease and death. In developing a malaria vaccine for universal use, it is important to understand the regulation of immunity induced by vaccination in both malaria-naive and preexposed or semi-immune individuals.
The aims of this study were to investigate the immune responses that develop following MSP119 vaccination in malaria-preexposed animals and vice versa. Anti-MSP119 Abs could be detected in prevaccination sera from malaria-preexposed mice (Fig. 1 C and D), indicating that P. yoelii infection elicits a natural albeit limited Ab response to MSP119. MSP119 vaccination of these preexposed mice resulted in a boosting of the MSP119-specific Ab response (Fig. 1D), but this increase of anti-MSP119 Abs was not accompanied by an increase of anti-whole-parasite Abs (Fig. 1H). We have previously reported that malaria infection results in deletion of adoptively transferred MSP119-specific Th1 cells (18) and memory B cells (19). The increase in MSP119-specific antibodies seen in this study suggests that infection had not resulted in deletion of MSP119-specific helper cells to such an extent as to ablate helper activity. We also observed that infection of MSP119-primed mice with P. yoelii led to an increase of anti-MSP119 Abs (Fig. 3B). Boosting of P. yoelii-exposed mice with MSP119 or infection/cure of MSP119-primed mice boosted Ab responses to MSP119 in both groups to comparable levels (Fig. 1D versus 3B).
However, MSP119 boosting of malaria-preexposed mice (Fig. 5D) and infection/cure of MSP119-primed mice (Fig. 5F) induced different degrees of protective immunity against P. yoelii challenge. The levels of anti-MSP119 Abs in these groups were equivalent (Fig. 1D versus 3B). This suggested that immune responses other than MSP119-specific Abs were responsible for the differences in protection. This conclusion was confirmed from the study of the malaria-preexposed, PBS-vaccinated group. This group demonstrated the highest degree of protection (Fig. 5C), but they had low levels of anti-MSP119-specific Abs (Fig. 1C); although they had levels of whole-parasite-specific Abs comparable to those in the poorly protected malaria-preexposed, MSP119-boosted mice (Fig. 1G and 3E), the component of those Abs that were not directed against MSP119 was significantly greater in the malaria-preexposed, PBS-vaccinated group than in the malaria-preexposed, MSP119-boosted group, as shown by ELISA inhibition studies using free MSP119 (Fig. 6).
Significantly, in this study, we have shown that the impaired protective immunity in the MSP119-primed mice was at least in part induced by suboptimal vaccination with this antigen. The evidence comes from three separate sets of experiments. First, MSP119-nonresponding B10.S mice were used to test whether the MSP119 suboptimal vaccine affects immunity induced by homologous parasite infection/cure. We could demonstrate no such effect in MSP119-nonresponding mice, as the data showed that MSP119-primed B10.S mice that were boosted with an infection/cure had the same level of protection to parasite challenge (7a, D) as mice that were primed with infection/cure and boosted with MSP119 (7a, E). Second, we tested whether P. yoelii- derived-MSP119 priming affects immunity induced by a different species of parasite. As shown in Fig. 7b, D and E, the P. yoelii-derived-MSP119-primed BALB/c mice given an infection/cure with P. chabaudi parasites had the same level of protective immunity to P. chabaudi as mice that had been primed with infection/cure and boosted with P. yoelii-derived MSP119. Finally, a single P. yoelii-derived-MSP119 T-cell epitope was used to prime BALB/c mice. We showed that p24 priming had no ability to skew the immune response (Fig. 7c). Taken together, these experiments suggested that the impaired protective immunity that follows suboptimal vaccination was induced by the immune responses to P. yoelii-derived MSP119. These results have profound implications for a human vaccine program in a situation where the vaccine response may be suboptimal for a variety of reasons. Suboptimal vaccination may render the ultimate acquisition of immunity that follows parasite exposure more difficult.
This study shows that a single injection of MSP119 impedes the development of natural immunity that arises following parasite infection. The MSP119 vaccination regimen in this study was deliberately suboptimal in order to more clearly reflect the likely situation in humans, where some will respond well to vaccination but others less well. Exposure of MSP119-primed mice to P. yoelii resulted in an increase of anti-MSP119 Abs, suggesting that MSP119 is a dominant B-cell epitope and that malaria infection induces the boosting of a preexisting Ab response. However, the increase of anti-MSP119 Abs observed in these mice did not confer protection at the same level as that observed in mice exposed to malaria parasites before MSP119 vaccination. It is well known that in rodent systems a very high titer of anti-MSP119 antibodies is required for protection and that in these situations no mice demonstrate a patent parasitemia following challenge (8). However, when the immune response to vaccination is suboptimal, mice are not protected (8). This study now demonstrates that not only are mice not protected by a low-titer Ab response but also that they can be inhibited from developing an otherwise protective immune response to the parasite. This “original antigenic sin” phenomenon has also been observed in humans, in which malaria infection selectively induces existing Ab responses to immunodominant epitopes (5, 15, 17), but its contribution to protection remains to be investigated.
Similar to the findings in this study, a previous study has shown that immunization of preimmune Saimiri sciureus monkeys with recombinant proteins associated with the membranes of trophozoite- and schizont-infected erythrocytes results in an enhancement of Ab responses and better protective immunity (13). In another study (2), prior exposure of Aotus vociferans monkeys to P. falciparum primes the production of anti-native MSP119 Abs, which are further boosted by vaccination with recombinant MSP119. This monkey demonstrated better protection than a vaccinated malaria-naive monkey (2), analogous to the results of this study (Fig. 5). However, the effect of prior exposure to MSP119 on the ability to induce immunity following parasite exposure has been studied to only a very limited degree. In the study referred to above (2) six of six monkeys that were vaccinated with MSP119 and infected were protected against a second challenge infection. However, the MSP119 vaccine regimen was highly efficacious by itself in that seven of nine monkeys in total were protected from high parasitemia during their initial challenge. Our study was designed to assess the effect of suboptimal vaccination.
In conclusion, this study demonstrates that (i) prior exposure to malaria does not seem to have negative effect on the response to subunit vaccination and (ii) vaccination with a partially effective subunit vaccine may impair subsequent development of immunity following malaria infection. Potential differences in response to vaccines between naive and semi-immune or preexposed individuals should be taken into consideration when planning malaria vaccine trials, and the consequences of a less-than-optimal vaccination in naive individuals should be considered. The need for optimal vaccine-induced Ab responses should be considered with respect to the overall development of malaria immunity.
Acknowledgments
We thank Salenna Elliott for significant input into these studies and critical review of the manuscript. We also acknowledge statistical assistance from Kanitta Thaikla.
Research in the authors' laboratories is supported by the Australian National Health and Medical Research Council and the UNDP/World Bank/WHO Special Program for Research and Training in Tropical Diseases (TDR). H.X. is an Australian NHMRC RD Wright fellow, and his research is also supported by China MOST 973 CB513100 and NNSF30610103103.
Editor: W. A. Petri, Jr.
Footnotes
Published ahead of print on 17 November 2008.
REFERENCES
- 1.Daly, T. M., and C. A. Long. 1995. Humoral response to a carboxyl-terminal region of the merozoite surface protein-1 plays a predominant role in controlling blood-stage infection in rodent malaria. J. Immunol. 155236-243. [PubMed] [Google Scholar]
- 2.Egan, A. F., M. J. Blackman, and D. C. Kaslow. 2000. Vaccine efficacy of recombinant Plasmodium falciparum merozoite surface protein 1 in malaria-naive, -exposed, and/or -rechallenged Aotus vociferans monkeys. Infect. Immun. 681418-1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fazekas de St Groth, S. 1967. Cross recognition and cross reactivity. Cold Spring Harbor Symp. Quant. Biol. 32525. [Google Scholar]
- 4.Francis, T., Jr. 1953. Influenza: the new acquayantance. Ann. Intern. Med. 39203-221. [DOI] [PubMed] [Google Scholar]
- 5.Franks, S., L. Baton, K. Tetteh, E. Tongren, D. Dewin, B. D. Akanmori, K. A. Koram, L. Ranford-Cartwright, and E. M. Riley. 2003. Genetic diversity and antigenic polymorphism in Plasmodium falciparum: extensive serological cross-reactivity between allelic variants of merozoite surface protein 2. Infect. Immun. 713485-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Good, M. F., D. C. Kaslow, and L. H. Miller. 1998. Pathways and strategies for developing a malaria blood-stage vaccine. Annu. Rev. Immunol. 1657-87. [DOI] [PubMed] [Google Scholar]
- 7.Hirunpetcharat, C., D. Stanisic, X. Q. Liu, J. Vadolas, R. A. Strugnell, R. Lee, L. H. Miller, D. C. Kaslow, and M. F. Good. 1998. Intranasal immunization with yeast-expressed 19 kD carboxyl-terminal fragment of Plasmodium yoelii merozoite surface protein-1 (yMSP119) induces protective immunity to blood stage malaria infection in mice. Parasite Immunol. 20413-420. [DOI] [PubMed] [Google Scholar]
- 8.Hirunpetcharat, C., J. H. Tian, D. C. Kaslow, N. van Rooijen, S. Kumar, J. A. Berzofsky, L. H. Miller, and M. F. Good. 1997. Complete protective immunity induced in mice by immunization with the 19-kilodalton carboxyl-terminal fragment of the merozoite surface protein-1 (MSP1[19]) of Plasmodium yoelii expressed in Saccharomyces cerevisiae: correlation of protection with antigen-specific antibody titer, but not with effector CD4+ T cells. J. Immunol. 1593400-3411. [PubMed] [Google Scholar]
- 9.Hirunpetcharat, C., P. Vukovic, X. Q. Liu, D. C. Kaslow, L. H. Miller, and M. F. Good. 1999. Absolute requirement for an active immune response involving B cells and Th cells in immunity to Plasmodium yoelii passively acquired with antibodies to the 19-kDa carboxyl-terminal fragment of merozoite surface protein-1. J. Immunol. 1627309-7314. [PubMed] [Google Scholar]
- 10.Ho, M., H. K. Webster, S. Looareesuwan, W. Supanaranond, R. E. Phillips, P. Chanthavanich, and D. A. Warrell. 1986. Antigen-specific immunosuppression in human malaria due to Plasmodium falciparum. J. Infect. Dis. 153763-771. [DOI] [PubMed] [Google Scholar]
- 11.Kumar, S., W. Collins, A. Egan, A. Yadava, O. Garraud, M. J. Blackman, J. A. Guevara Patino, C. Diggs, and D. C. Kaslow. 2000. Immunogenicity and efficacy in aotus monkeys of four recombinant Plasmodium falciparum vaccines in multiple adjuvant formulations based on the 19-kilodalton C terminus of merozoite surface protein 1. Infect. Immun. 682215-2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar, S., A. Yadava, D. B. Keister, J. H. Tian, M. Ohl, K. A. Perdue-Greenfield, L. H. Miller, and D. C. Kaslow. 1995. Immunogenicity and in vivo efficacy of recombinant Plasmodium falciparum merozoite surface protein-1 in Aotus monkeys. Mol. Med. 1325-332. [PMC free article] [PubMed] [Google Scholar]
- 13.Perraut, R., O. Mercereau-Puijalon, D. Mattei, E. Bourreau, O. Garraud, B. Bonnemains, L. Pereia de Silva, and J. C. Michel. 1995. Induction of opsonizing antibodies after injection of recombinant Plasmodium falciparum vaccine candidate antigens in preimmune Saimiri sciureus monkeys. Infect. Immun. 63554-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stanisic, D. I., L. B. Martin, X. Q. Liu, D. Jackson, J. Cooper, and M. F. Good. 2003. Analysis of immunological nonresponsiveness to the 19-kilodalton fragment of merozoite surface protein 1 of Plasmodium yoelii: rescue by chemical conjugation to diphtheria toxoid (DT) and enhancement of immunogenicity by prior DT vaccination. Infect. Immun. 715700-5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor, R. R., A. Egan, D. McGuinness, A. Jepson, R. Adair, C. Drakely, and E. Riley. 1996. Selective recognition of malaria antigens by human serum antibodies is not genetically determined but demonstrates some features of clonal imprinting. Int. Immunol. 8905-915. [DOI] [PubMed] [Google Scholar]
- 16.Tian, J. H., L. H. Miller, D. C. Kaslow, J. Ahlers, M. F. Good, D. W. Alling, J. A. Berzofsky, and S. Kumar. 1996. Genetic regulation of protective immune response in congenic strains of mice vaccinated with a subunit malaria vaccine. J. Immunol. 1571176-1183. [PubMed] [Google Scholar]
- 17.Weisman, S., L. Wang, H. Billman-Jacobe, D. H. Nhan, T. L. Richie, and R. L. Coppel. 2001. Antibody responses to infections with strains of Plasmodium falciparum expressing diverse forms of merozoite surface protein 2. Infect. Immun. 69959-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wipasa, J., H. Xu, A. Stowers, and M. F. Good. 2001. Apoptotic deletion of Th cells specific for the 19-kDa carboxyl-terminal fragment of merozoite surface protein 1 during malaria infection. J. Immunol. 1673903-3909. [DOI] [PubMed] [Google Scholar]
- 19.Wykes, M. N., Y. H. Zhou, X. Q. Liu, and M. F. Good. 2005. Plasmodium yoelii can ablate vaccine-induced long-term protection in mice. J. Immunol. 1752510-2516. [DOI] [PubMed] [Google Scholar]