Abstract
Previous studies indicate that schizophrenia patients draw decisions more hastily than controls. The aim of the present study was to obtain convergent evidence with a new paradigm, designed after the Who Wants to Be a Millionaire television game show. Thirty-two schizophrenia patients and 38 healthy subjects were administered 20 knowledge questions, along with 4 response alternatives. Participants were required to provide probability estimates for each alternative. Whenever a subject was confident that one of the alternatives was correct or was wrong, the subject was asked to indicate this via a decision or rejection rating. Thus, probability estimates and decisions were independently assessed, allowing determination of the point at which probability estimates translate into decisions. Patients and controls gave comparable probability estimates for all alternatives. However, patients committed more erroneous responses, owing to their making decisions in the face of low subjective probability ratings and rejecting alternatives despite rather high probability ratings. The results provide further evidence for the claim that schizophrenia patients make strong judgments based on little information. We propose that a lowered threshold for accepting alternatives provides a parsimonious explanation for the data-gathering bias reported in the literature.
Keywords: delusion, decision-making, probability threshold
Contrary to early claims by Jaspers1 that a proper delusion must defy understanding, a psychological understanding of paranoid schizophrenia has received increasing empirical support.2–4 Over the past decade, a number of attentional5 and reasoning biases6 have been observed in schizophrenia that may contribute to the emergence and maintenance of psychosis. Several studies whose claims are central to the present investigation suggest that schizophrenia patients are very hasty and incautious when drawing decisions.7–16 There is evidence that this so-called jumping to conclusions (JTC) bias stems from a liberal acceptance (LA) in schizophrenia.17 The LA account holds that fragmented and partial information is taken as sufficient evidence to accept a response option.
The preponderance of empirical evidence on the JTC bias has been gathered using the probabilistic reasoning task.4 For this paradigm, 2 jars containing colored beads in opposing ratios are displayed. The jars are then removed from the participant's view, and the participant is told that 1 bead at a time will be drawn from 1 jar only. The participant is required to identify the source of the beads.4 It has been repeatedly observed that 40–70% of schizophrenic patients, irrespective of delusional status, decide after only 1 bead (referred to as the JTC bias), whereas healthy subjects take more beads to decide. While impulsivity and poor motivation have been rendered unlikely by prior research,9,13 it has been objected that aberrant task performance is affected by low intelligence11 and poor task comprehension.13 Moreover, Maher has contended that it is counterintuitive to infer a dysfunctional bias from this task, as patients' performance is, in fact, superior to controls, according to optimal Bayesian reasoning.18
To strengthen the account, it is important to demonstrate the JTC bias with novel tasks. Such a convergent approach reduces the probability that the JTC pattern is bound to task-specific features of the beads paradigm. In addition, in order to link JTC with faulty reasoning, paradigms are needed for which such a reasoning style results in incorrect responses.
To meet this purpose, in the present study we administered a newly designed task, which was inspired by the Who Wants to Be a Millionaire television game show. For the present operationalization, the participant was required to answer knowledge questions with 4 possible alternatives. For each alternative, the participant was required to provide probability estimates between 0% and 100% and was then asked if he or she could decide in favor of 1 of the alternatives based on those estimates or could rule out 1 or more of the alternatives (optional). Thus, probability estimates and decisions were assessed independently, allowing determination of the point at which probability estimates translate into decisions.
Unlike for the draws-to-decision version of the beads task, premature decisions (ie, a decision based on a low probability estimate) in the present task cannot be explained by poor motivation or a preference to terminate the task prematurely because any decision or rejection rating for a given item, if anything, prolongs the task. Second, LA more easily leads to errors on this kind of task, and such a procedure may thus be more ecologically valid for tapping a mechanism that may contribute to reality distortion.
The independent assessment of probability estimates and decisions allows computation of the probabilities that correspond to the acceptance and rejection of alternatives, that is, the extent of subjective confidence required for decision-making. This approach is in accordance with recent research that posits that participants use an evidence-accrual strategy,19 whereby the decision is terminated once a sufficient amount of evidence has been collected.20,21
For the present study we expected that patients with schizophrenia would make decisions even in the face of low probability estimates, and that these same probability estimates would be deemed insufficient for healthy participants to make a decision. In line with the literature on the beads task,4 no differences were expected for probability assessment as such.
Method
Participants
Thirty-two patients with an established diagnosis of schizophrenia according to DSM-IV criteria took part in the experiment. Patients were recruited from the Psychiatry Department of the University Hospital of Hamburg. All patients underwent a thorough psychopathological assessment using a neuropsychiatric interview (MINI).22 Thirty-eight healthy controls were recruited for participation and screened with the MINI interview for absence of any psychiatric disorder and psychotic symptoms.
None of the schizophrenia participants had a known current or past history of brain damage, severe substance abuse, or an Axis I diagnosis other than schizophrenia, except for depression and dysthymia (n = 5), which were tolerated. All patients were stabilized with atypical neuroleptics.
Schizophrenic psychopathology was assessed with the Positive and Negative Syndrome Scale (PANSS).23 At the time of testing, 56% of the patients displayed at least mild paranoid symptoms (n = 18). After a complete description of the study was given to the participants, written informed consent was obtained. The research project was approved by the local ethics committee.
Experiment
Participants were presented 20 semantic knowledge questions in a fixed order. These questions were selected for moderate difficulty from a pilot study. Questions were carefully selected to avoid delusional themes. After each question (eg, “How many fingers does Mickey Mouse have?”), 4 alternatives were presented in fixed order (eg, 10, 12, 8, 6; correct answer: 8). For each of these possibilities the participant was requested to provide probability estimates in 10% steps from 0% to 100%. If the participant felt that an alternative could be clearly endorsed (decision) or rejected (rejection), this was marked in another column (decision or rejection). It was left up to the participant whether those inferences were made immediately following all the probability estimates or after each response alternative. In addition, ratings could be changed over the course of the response process. Even if a participant was entirely certain that an alternative was correct, the other alternatives nevertheless had to be rated in terms of their probability.
The present “quiz” was administered as an interview, and for every item participants were prompted whether their estimate would translate into a decision or rejection. No specific guidelines for participants were given as to a method for equating probability estimates to decisions. The participants were simply reminded for each item to consider these additional response options. Upon request, the experimenter repeated prior responses, and participants could take a look at the response sheet to minimize memory load. The experimenter was naive about the study hypotheses to avoid occurrence of a Pygmalion effect. The procedure was explained to participants with 1 practice trial. No feedback regarding correct or incorrect answers was provided.
Results
Sociodemographic Characteristics
As can be seen in table 1, the participant groups were not significantly different with respect to age, gender, school education and premorbid intelligence. Premorbid intelligence was tapped with a vocabulary/knowledge test.
Table 1.
Sociodemographic, Psychopathological, and Experimental Variables for the Schizophrenia and Healthy Participants
| Variable | Schizophrenia (S) (n = 32) | Healthy (H) (n = 38) | Statistics |
| Background Variables | |||
| Age in years | 36.72 (12.35) | 32.39 (10.20) | t = 1.60, p > .1 |
| Gender (male/female) | 18/14 | 18/20 | χ2 = 0.55, p > .4 |
| Formal education in years | 11.53 (1.83) | 11.41 (1.71) | t = 0.27, p > .7 |
| Premorbid IQ (vocabulary) | 107.84 (13.51) | 112.03 (12.76) | t = 1.30, p > .1 |
| PANSS total | 61.59 (15.52) | — | — |
| Number of hospitalizations | 3.65 (2.75) | — | — |
| “Millionaire” Test | |||
| Mean probability estimates for correct judgments in % | 49.08 (15.98) | 54.83 (15.75) | t = 1.51, p > .1 |
| Mean probability estimates for incorrect judgments in % | 20.45 (10.03) | 19.08 (10.04) | t = 0.57, p > .5 |
| Number of correct decisions | 7.78 (3.93) | 7.87 (3.90) | t = .09, p > .9 |
| Number of incorrect decisions | 6.47 (4.20) | 3.92 (3.35) | t = 2.82, p = .006 |
| Number of correct rejections | 28.37 (16.61) | 31.68 (11.97) | t = 1.00, p > .3 |
| Number of incorrect rejections | 4.22 (3.73) | 3.21 (2.44) | t = 1.36, p > .1 |
Note: PANSS = Positive and Negative Syndrome Scale.
“Millionaire” Test
Table 1 shows that patients and healthy controls could not be differentiated in terms of probability estimates for correct and incorrect response options (ie, at least p > .1): patients as well as controls expressed higher probability judgments for alternatives that turned out to be correct. However, a different picture emerges when looking at decision ratings. Whereas correct decisions were made comparably often in both groups (see Table 1), patients made significantly more incorrect decisions than controls. From the top panel of Figure 1, it becomes clear that this is due to incautious decision-making in patients: patients endorsed decisions even in the face of rather low subjective probability estimates, especially for incorrect alternatives, while healthy participants based decisions on higher probability estimates (mean rating: 92.7% versus 85.9%, p < .01). Even stronger results emerged when the minimum probability for a decision was calculated: while healthy participants did not decide for probabilities lower than 70%, the corresponding result in patients was 54.4% (collapsed for both correct and incorrect ratings; p = .01). Again, the difference was most pronounced for incorrect decisions (see the top panel of Figure 1). An inverted picture emerged for rejections (the bottom panel of Figure 1): patients discarded response alternatives that were assigned rather high probability estimates (mean ratings, schizophrenia: 6.0%, controls: 0.7%, p < .001). The mean sum probability estimates across the 4 alternatives for each item (correct: 100%) did not differ between healthy subjects (104.8%) and schizophrenic participants (105.1%; p > .9).
Fig. 1.
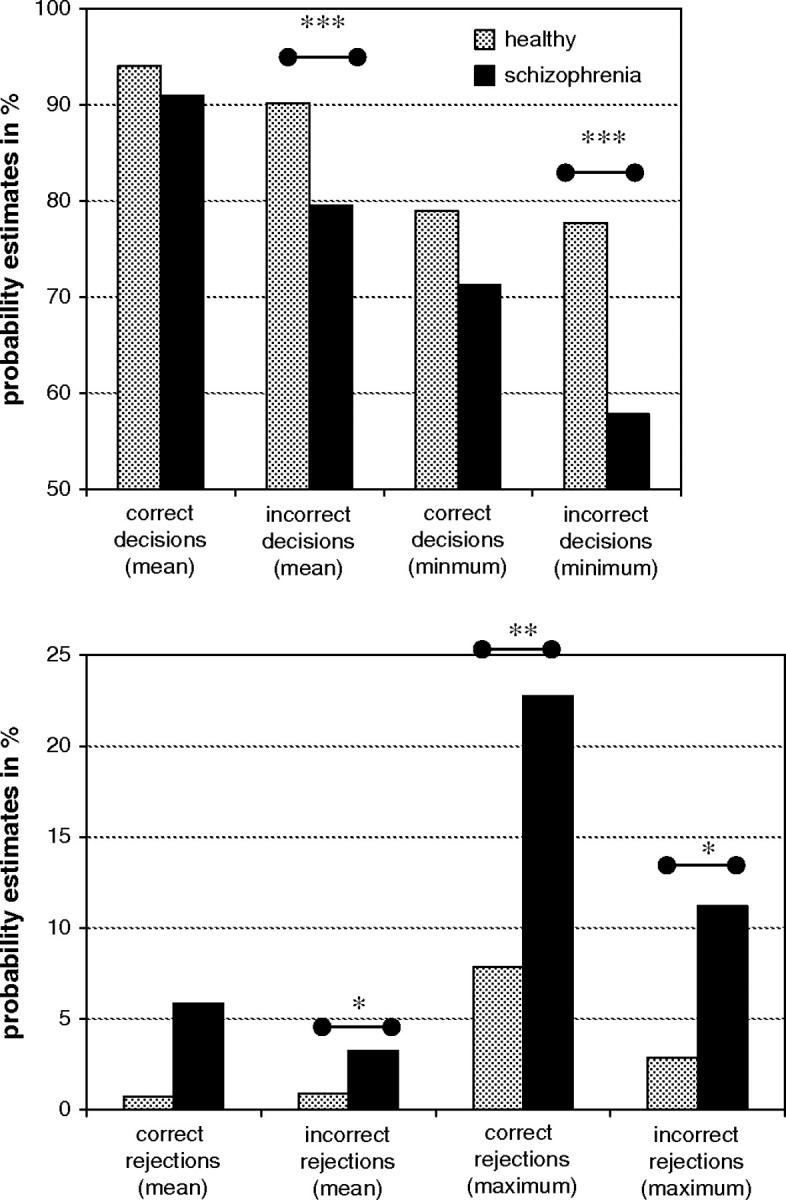
Correspondence Between Subjective Probabilities and Decisions Versus Rejections. For most parameters, schizophrenia patients decided and rejected response alternatives more hastily than controls (ie, decisions despite rather low probability estimates; rejections despite rather high probability estimates). * p ≤ .05; ** p ≤ .01; *** p ≤.001.
No relationship emerged between psychopathological symptoms and syndromes that would have survived a Bonferroni-correction.
Discussion
The main motivation for the current study was to gain insight into the nature of biased reasoning in schizophrenia with a new paradigm, designed after the Who Wants to Be a Millionaire television game show. The results demonstrated that schizophrenia patients did not perform differently from controls when estimating the likelihood of correct and incorrect alternatives in a multiple-choice knowledge task. Thus, in line with prior research,4,13 patients did not display a disturbance in probability judgment as such. However, patients committed more erroneous decisions than controls, reflecting a facilitated readiness to translate probability estimates into decisions, particularly for incorrect decisions. In addition, the minimum probability estimate deemed sufficient for drawing a decision was significantly lower. Interestingly, such a lax response threshold operates for both decisions and rejections. Thus, patients also rejected alternatives more easily.
The present results fit nicely with the literature on JTC in schizophrenia: patients are hastier in their decision-making, that is, they base strong judgments on little evidence. What may appear on the surface to be a deficit in semantic knowledge may in fact be more adequately described as a greater incautiousness for decisions. As noted, the present set of results cannot parsimoniously be explained as a result of poor motivation or the urge to terminate the task quickly. Moreover, comprehension problems are very unlikely since the patients performed equal to healthy participants in terms of overall probability estimates and sum probability estimate per item.
From the available evidence on reasoning in schizophrenia, we propose that JTC emerges when (a) only a limited number of response alternatives is available, (b) the strongest option is very discrepant in terms of probability relative to other options, and (c) rejection of an alternative is fostered thereby narrowing the pool of available candidates. While such conditions may also prompt earlier decisions in healthy subjects, healthy subjects, as shown, will nevertheless collect more evidence to substantiate their reasoning. Prior research by our group has demonstrated that, in line with the LA account, JTC in schizophrenia does not occur when ambiguity is high, particularly with multiple “tempting” alternatives (eg, multiple jars in the beads task with less discrepant ratios).
It is important to consider the potential behavioral consequences of a lower acceptance threshold. As has been shown, risky decision-making renders a participant prone to errors made with high confidence. This, in turn, may promote the development of a set of false ideas that, by means of heightened incorrigibility in schizophrenia,24,25 a confirmation bias,26 and various other “safety behaviors,”27 may eventually trigger a full-blown delusion. Further maintenance factors may be a gain in self-esteem as a consequence of paranoid and grandiose belief systems28 and the relief that is accompanied with the decrement of uncertainty once an alleged delusional conspiracy, for example, has been uncovered.29 In healthy people, a rather strict threshold makes it unlikely that many firmly held false ideas are established. In order to address delusion-related metacognitive biases, including LA, we have recently devised a metacognitive skill training program.30
Whereas the proposed mechanism may be instructive in explaining the emergence of delusions, it is also important to test whether it applies to hallucinatory experiences. When a healthy person has a hallucination, which is by no means a rare experience,31 he or she acknowledges that the voice has arisen from his or her own mind because a number of characteristics are likely checked before a hallucination is considered a percept. For a schizophrenia patient, on the other hand, a limited set of voicelike characteristics may suffice to mistake self-generated cognitions as real voices (eg, content is not representing normal thinking) while ignoring others (eg, no overt source).
Finally, we would like to note some limitations of the present study. In future studies psychiatric control subjects should to be recruited to verify the specificity of LA to schizophrenia. Moreover, our claim that LA is a traitlike feature of schizophrenia needs to be directly addressed in a longitudinal study, which is currently being performed. Finally, the role of affect and the impact of stress induction on JTC in schizophrenia deserve thorough attention.
References
- 1.Jaspers K. Berlin: Springer; 1973. Allgemeine Psychopathologie [General psychopathology] [Google Scholar]
- 2.Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. 2001;21:1143–1192. doi: 10.1016/s0272-7358(01)00106-4. [DOI] [PubMed] [Google Scholar]
- 3.Blackwood NJ, Howard RJ, Bentall RP, Murray RM. Cognitive neuropsychiatric models of persecutory delusions. Am J Psychiatry. 2001;158:527–539. doi: 10.1176/appi.ajp.158.4.527. [DOI] [PubMed] [Google Scholar]
- 4.Garety PA, Freeman D. Cognitive approaches to delusions: a critical review of theories and evidence. Br J Clin Psychol. 1999;38:113–154. doi: 10.1348/014466599162700. [DOI] [PubMed] [Google Scholar]
- 5.Green MJ, Phillips ML. Social threat perception and the evolution of paranoia. Neurosci Biobehav Rev. 2004;28:333–342. doi: 10.1016/j.neubiorev.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Dudley REJ, Over DE. People with delusions jump to conclusions: a theoretical account of research findings on the reasoning of people with delusions. Clin Psychol Psychother. In press. [Google Scholar]
- 7.Colbert SM, Peters ER. Need for closure and jumping-to-conclusions in delusion-prone individuals. J Nerv Ment Dis. 2002;190:27–31. doi: 10.1097/00005053-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Freeman D, Garety PA, Fowler D, Kuipers E, Bebbington PE, Dunn G. Why do people with delusions fail to choose more realistic explanations for their experiences? An empirical investigation. J Consult Clin Psychol. 2004;72:671–680. doi: 10.1037/0022-006X.72.4.671. [DOI] [PubMed] [Google Scholar]
- 9.Dudley REJ, John CH, Young AW, Over DE. Normal and abnormal reasoning in people with delusions. Br J Clin Psychol. 1997;36:243–258. doi: 10.1111/j.2044-8260.1997.tb01410.x. [DOI] [PubMed] [Google Scholar]
- 10.Fear CF, Healy D. Probabilistic reasoning in obsessive-compulsive and delusional disorders. Psychol Med. 1997;27:199–208. doi: 10.1017/s0033291796004175. [DOI] [PubMed] [Google Scholar]
- 11.Garety PA, Hemsley DR, Wessely S. Reasoning in deluded schizophrenic and paranoid patients: biases in performance on a probabilistic inference task. J Nerv Ment Dis. 1991;179:194–201. doi: 10.1097/00005053-199104000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Huq SF, Garety PA, Hemsley DR. Probabilistic judgements in deluded and non-deluded subjects. Q J Exp Psychol A. 1988;40:801–812. doi: 10.1080/14640748808402300. [DOI] [PubMed] [Google Scholar]
- 13.Moritz S, Woodward TS. Jumping to conclusions in delusional and non-delusional schizophrenic patients. Br J Clin Psychol. 2005;44:193–207. doi: 10.1348/014466505X35678. [DOI] [PubMed] [Google Scholar]
- 14.Menon M, Pomarol-Clotet E, McCarthy RA, McKenna PJ. Probabilistic reasoning bias is a function of having schizophrenia, not of being deluded. Schizophr Res. 2002;53(suppl):133. [Google Scholar]
- 15.Mortimer AM, Bentham P, McKay AP, et al. Delusions in schizophrenia: a phenomenological and psychological exploration. Cogn Neuropsychiatry. 1996;1:289–303. doi: 10.1080/135468096396451. [DOI] [PubMed] [Google Scholar]
- 16.Peters E, Day S, Garety PA. A longitudinal study of cognitive abnormalities in delusions at different levels of information processing. Schizophr Res. 1999;36:180. [Google Scholar]
- 17.Moritz S, Woodward TS. Plausibility judgment in schizophrenic patients: evidence for a liberal acceptance bias. Germ J Psychiatry. 2004;7:66–74. [Google Scholar]
- 18.Maher BA. Anomalous experience in everyday life: its significance for psychopathology. Monist. 1999;82:547–570. [Google Scholar]
- 19.Newell BR. Re-visions of rationality? Trends Cogn Sci. 2005;9:11–15. doi: 10.1016/j.tics.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Lee MD, Cummins TD. Evidence accumulation in decision making: unifying the “take the best” and the “rational” models. Psychol Bull Rev. 2004;11:343–352. doi: 10.3758/bf03196581. [DOI] [PubMed] [Google Scholar]
- 21.Hausmann D, Läge D. How the desired level of confidence influences the stopping rule of information search. In: Opwis K, Penner I-K, editors. Proceedings of KogWis05: The German Cognitive Science Conference 2005. Basel: Schwabe; 2005. pp. 71–76. [Google Scholar]
- 22.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview. J Clin Psychiatry. 1998;59(suppl 20):22–33. [PubMed] [Google Scholar]
- 23.Kay SR, Opler LA, Lindenmayer J-P. The Positive and Negative Syndrome Scale (PANSS): rationale and standardisation. Br J Psychiatry. 1989;155(suppl 7):59–65. [PubMed] [Google Scholar]
- 24.Woodward TS, Moritz S, Cuttler C, Whitman JC. Contribution of a cognitive bias against disconfirmatory evidence to delusions in schizophrenia. J Clin Exp Neuropsychol. doi: 10.1080/13803390590949511. In press. [DOI] [PubMed] [Google Scholar]
- 25.Moritz S, Woodward TS. A generalized bias against disconfirmatory evidence (BADE) in schizophrenia. Psychiatry Res. doi: 10.1016/j.psychres.2005.08.016. In press. [DOI] [PubMed] [Google Scholar]
- 26.Jonas E, Schulz-Hardt S, Frey D, Thelen N. Confirmation bias in sequential information search after preliminary decisions: an expansion of dissonance theoretical research on selective exposure to information. J Pers Soc Psychol. 2001;80:557–571. doi: 10.1037//0022-3514.80.4.557. [DOI] [PubMed] [Google Scholar]
- 27.Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41:331–347. doi: 10.1348/014466502760387461. [DOI] [PubMed] [Google Scholar]
- 28.Moritz S, Werner R, von Collani G. The inferiority complex in paranoia re-addressed: a study with the Implicit Association Test. Cogn Neuropsychiatry. doi: 10.1080/13546800444000263. In press. [DOI] [PubMed] [Google Scholar]
- 29.Klosterkotter J. Wie entsteht das schizophrene Kernsyndrom? Ergebnisse der Bonner Übergangsreihenstudie und angloamerikanische modellvorstellungen-ein vergleich [How does the schizophrenic nuclear syndrome arise? Results of the Bonn transition series study and Anglo-American models—a comparison] Nervenarzt. 1992;63:675–682. [PubMed] [Google Scholar]
- 30.Moritz S, Burlon M, Woodward TS. Metacognitive Skill Training for Patients With Schizophrenia: Manual. Hamburg: VanHam Campus Verlag; 2005. [Google Scholar]
- 31.David AS. Auditory hallucinations: phenomenology, neuropsychology, and neuroimaging update. Acta Psychiatr Scand. 1999;99(suppl 395):95–104. doi: 10.1111/j.1600-0447.1999.tb05988.x. [DOI] [PubMed] [Google Scholar]


